Labor and Delivery Complications and High-Risk Pregnancies
1/112
Earn XP
Description and Tags
These flashcards encapsulate key concepts and management strategies related to labor and delivery complications and high-risk pregnancies, providing a succinct review for exam preparation.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
What is the definition of multi-gestation pregnancies?
Multi-gestation pregnancies involve one or more eggs fertilized, leading to twins, triplets, or more, with increasing incidences due to fertility treatments and advanced maternal age.
What are the maternal risks associated with multi-gestation pregnancies?
Increased risk of preterm labor, hydramnios, anemia, preeclampsia, and antepartum hemorrhage.
What are some fetal risks linked with multi-gestation pregnancies?
Increased risk for respiratory distress syndrome (RDS), congenital anomalies, prematurity, birth asphyxia, twin-to-twin transfusion, and intrauterine growth restriction (IUGR).
Define the Bishop Score and its significance.
The Bishop Score evaluates cervical readiness for labor; a score of less than 5 suggests that labor will not start without induction, while a score of 9 or higher indicates labor will likely begin spontaneously.
What is the function of Prostaglandin E1 in labor management?
Prostaglandin E1 (Cytotec) is used for cervical ripening to stimulate labor that may lead to delivery.
What should be done if there are signs of fetal distress during labor induced with Pitocin?
Turn off Pitocin, turn the mother to her side, provide oxygen via face mask, and notify the primary care provider.
What is shoulder dystocia and its associated risks?
Shoulder dystocia is the failure to deliver fetal shoulders by the usual cardinal movements after the head has been born, increasing risks for maternal trauma, PPH, and fetal complications like fractured clavicle and hypoxia.
What emergency management steps should be taken for umbilical cord prolapse?
Maintain a knee-chest or Trendelenburg position to alleviate pressure on the cord, lift the presenting part off the cord without removing your hand, and prepare for an immediate cesarean section.
What are the signs and symptoms of preterm labor?
Regular uterine contractions (6 or more in an hour), lower abdomen cramping, low back pain, changes in vaginal discharge, and pelvic pressure.
What is the initial management for a patient experiencing preterm labor?
Hydrate, rest, and consider medications like magnesium sulfate, beta-mimetics, or corticosteroids, while avoiding vaginal exams or speculum exams.
Why does managing multiple pregnancies put the mother at risk for PPH?
Managing multiple pregnancies increases the risk of postpartum hemorrhage (PPH) due to factors like increased uterine distension, fatigue of uterine muscle, higher likelihood of placenta issues (like placenta previa or abruption), and higher blood volume that complicates bleeding management.
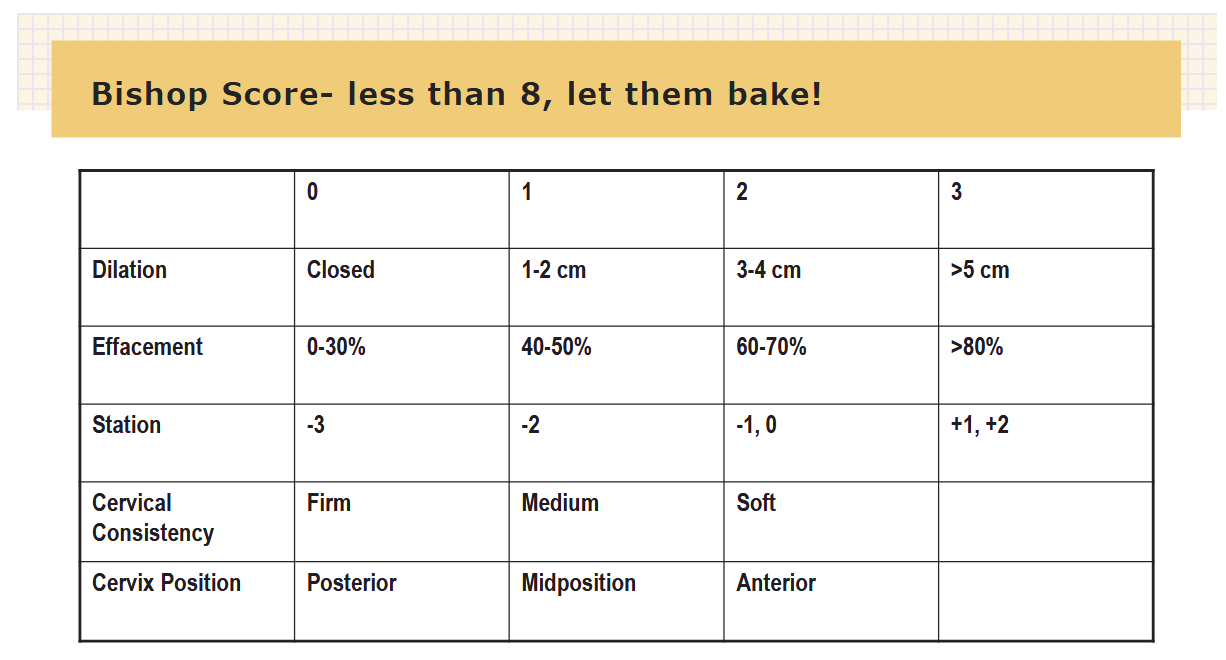
What is the purpose of Bishop scoring?
The Bishop score is used to assess the readiness of the cervix for labor by evaluating factors such as cervical dilation, effacement, station of the fetus, consistency, and position of the cervix. A higher score indicates a greater likelihood of successful induction of labor.
How is the readiness for labor evaluated?
Readiness for labor is evaluated through the Bishop score, which assesses cervical dilation, effacement, fetal station, consistency, and position.
Nulliparas – 9 or more
Multiparas – 5 or more
Less than 5 = suggests labor will not start without induction
Score 9 and ^ =indicates labor will likely begin spontaneously
Score 3 and lower = indicates induction would not be successful.
What is cervical ripening?
Is the process by which the cervix softens, thins (effacement), and dilates in preparation for labor, making it more favorable for vaginal delivery. This process can occur naturally or be induced through medical interventions:
Prostaglandin E1 - Cytotec (misoprostol) 25-50mcg sublingual/PV q4hr (6 dose max)
Prostaglandin E2 – Cervidil, Prepidil (dinoprostone)- controlled release of 0.3mg/ hr for 12 hours.
Balloon catheters- foley balloon, Cooks balloon- assess q4, w ill come out at 4 -5cm dilated
Amniotomy- AROM
Stripping/sw eeping membranes
When is pitocin contraindicated?
Pitocin is contraindicated in situations such as fetal distress, uterine hyperstimulation (tachysystole), and when there are contraindications to vaginal delivery, such as a previous cesarean with a classic incision or placenta previa. Tumultuous labor with teteanic contractions, placental abruption, uterine rupture, cervical lacerations, PP hemorrhage, consequent fetal effects. Basically in cases where vaginal delivery is inadvisable - non reassuring pattern- IV, O2, TURN OFF PITOCIN!!
How is pitocin administered?
Administration – titrated IV drip via pump piggybacked in most proximal port of IV line
Dosage – 1-3 mU/minute, increased by 1-3 mU q 30-40 minutes
What should you monitor for pitocin?
Monitor – CTX frequency, duration, intensity, and uterine resting tone; FHR pattern, maternal VS, labor progress. AWHONN says q15
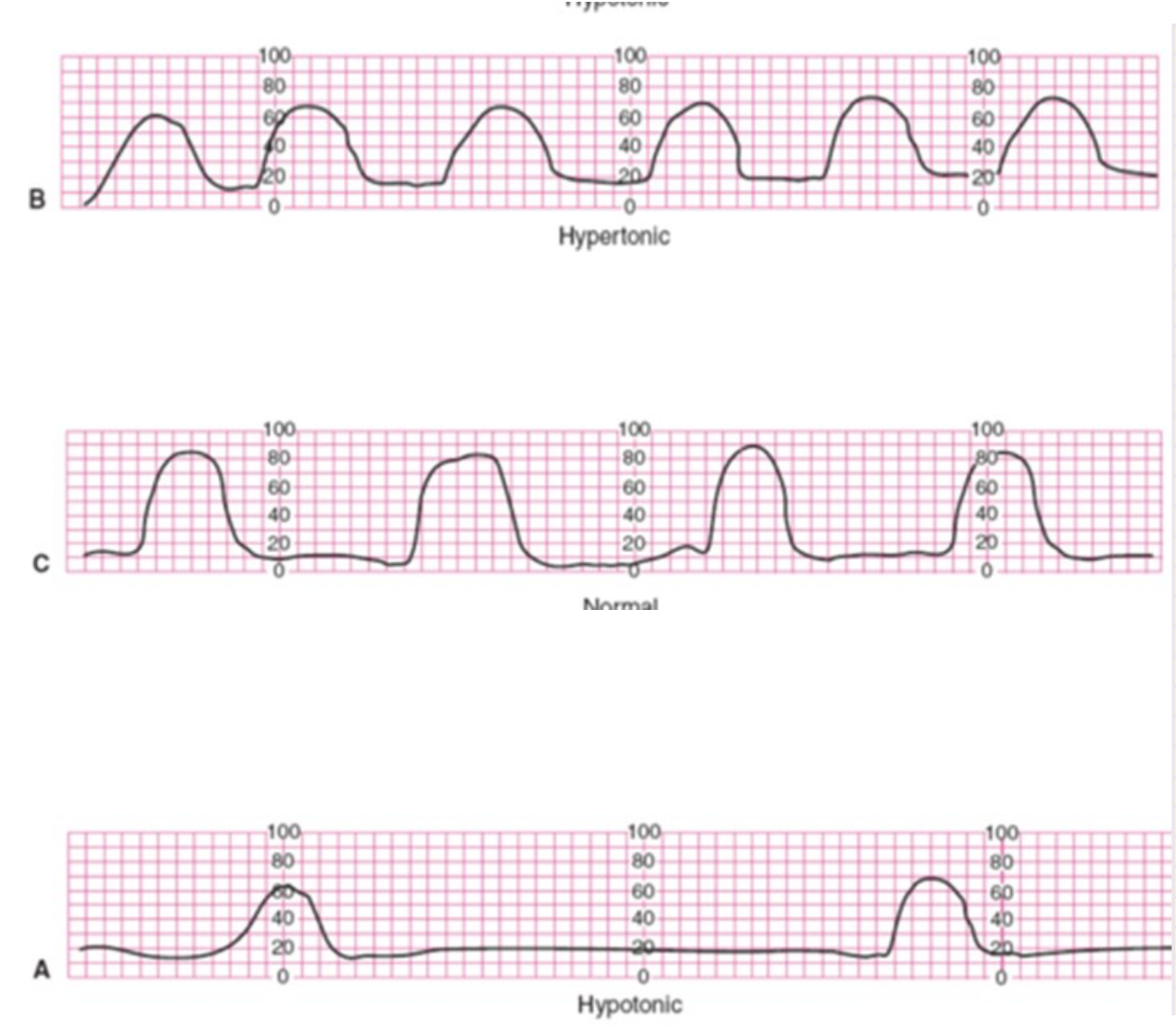
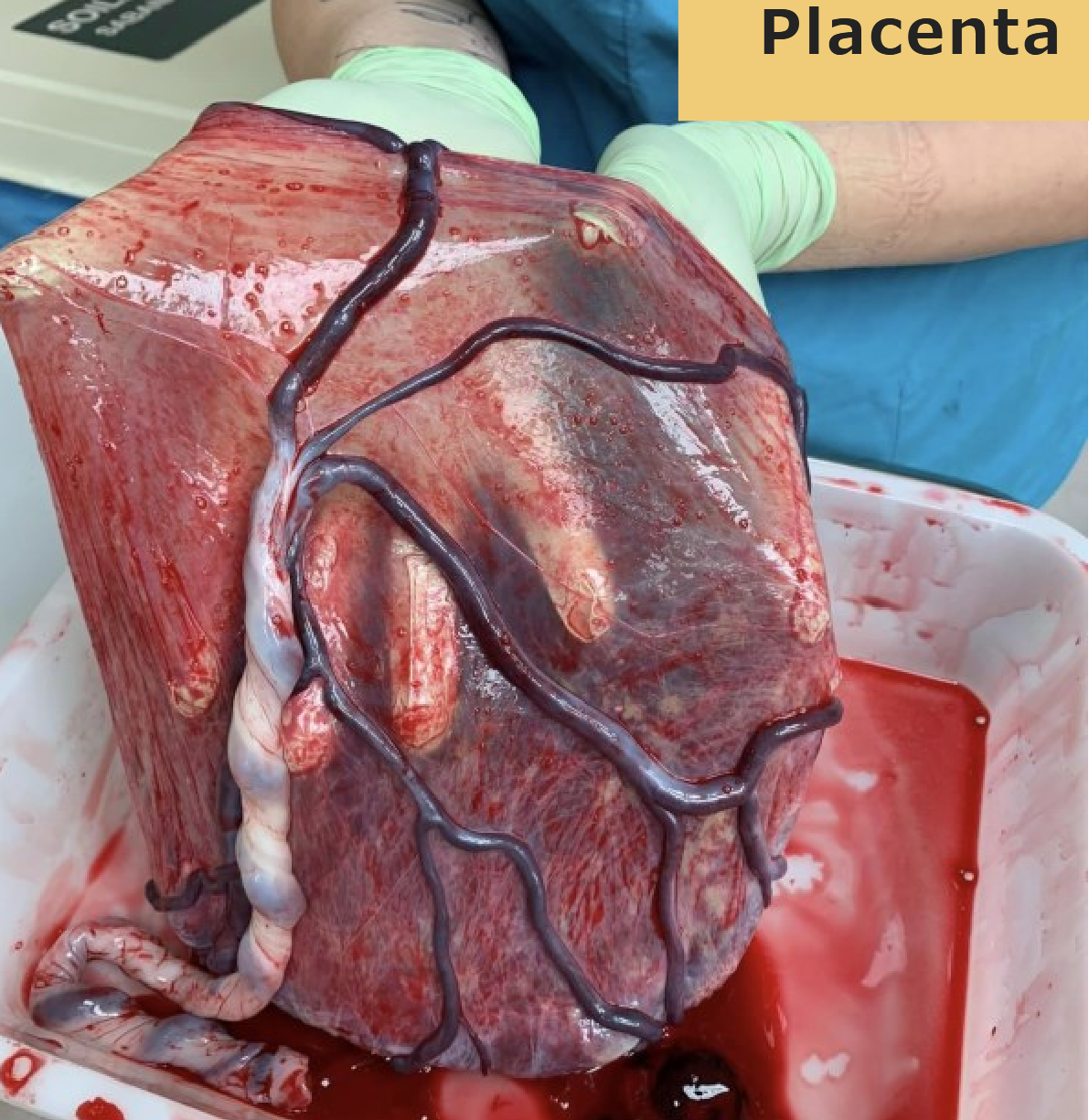
What is this?
Uterine Tachysystole -
s/s: CTX frequency < q2minutes, duration > 90seconds, uterine resting tone > 20mmhg; non-reasuring FHR tracing.
What are interventions for uterine tachysystole?
Turn off infusion , turn Mom to side, O2 via face mask, IV fluid bolus, notify primary care provider, may need to give Terbutaline; document fetal responses to actions
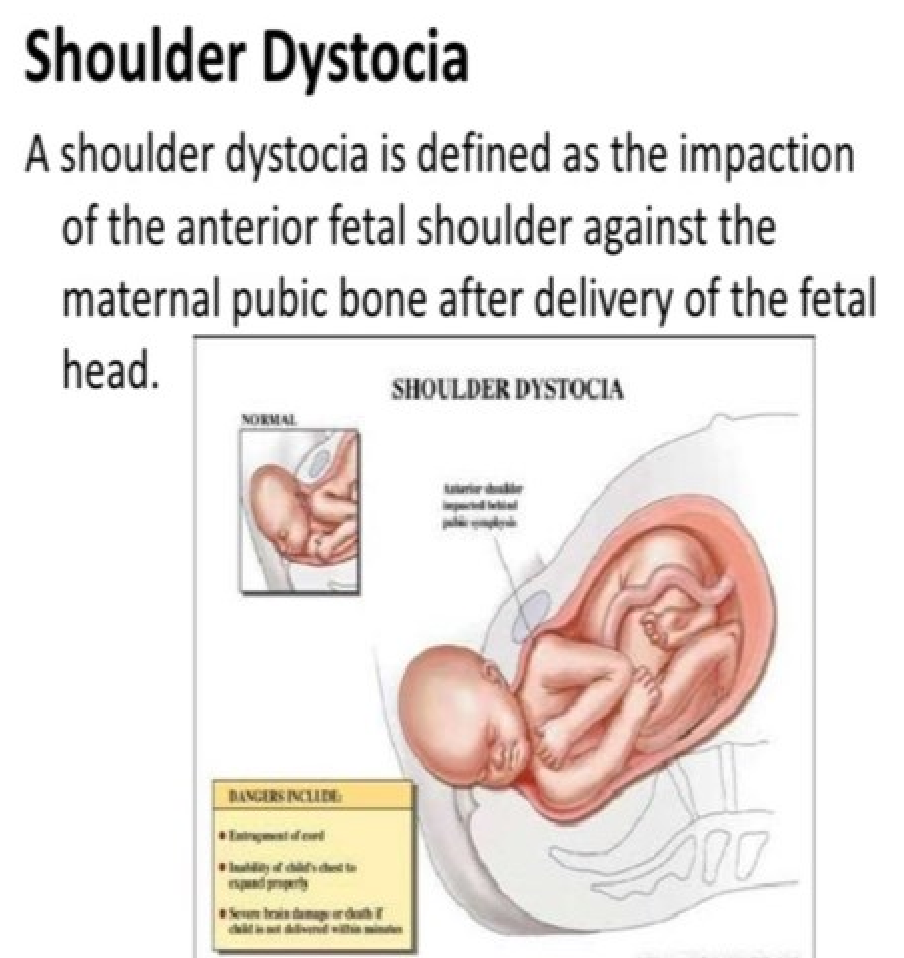
What is shoulder dystocia?
Failure to deliver the fetal shoulders by the usual cardinal movements after the head has been born. Time of head delivery to time of body delivery is >60 seconds or if any maneuvers are used
What are risk factors of should dystocia?
@ 5mins, neonatal acidemia risk is high
Risk factors - increased size of fetus, maternal obesity, excessive maternal weight gain, short stature, contracted pelvic outlet, protracted labor, male fetus, gestational diabetes
What are maternal and fetal complications of shoulder dystocia?
Maternal complications - trauma to pelvis, tissue, birth canal, PPH
Fetal complications - fractured clavicle, brachial plexus palsy (erb’s palsy), hypoxia, death
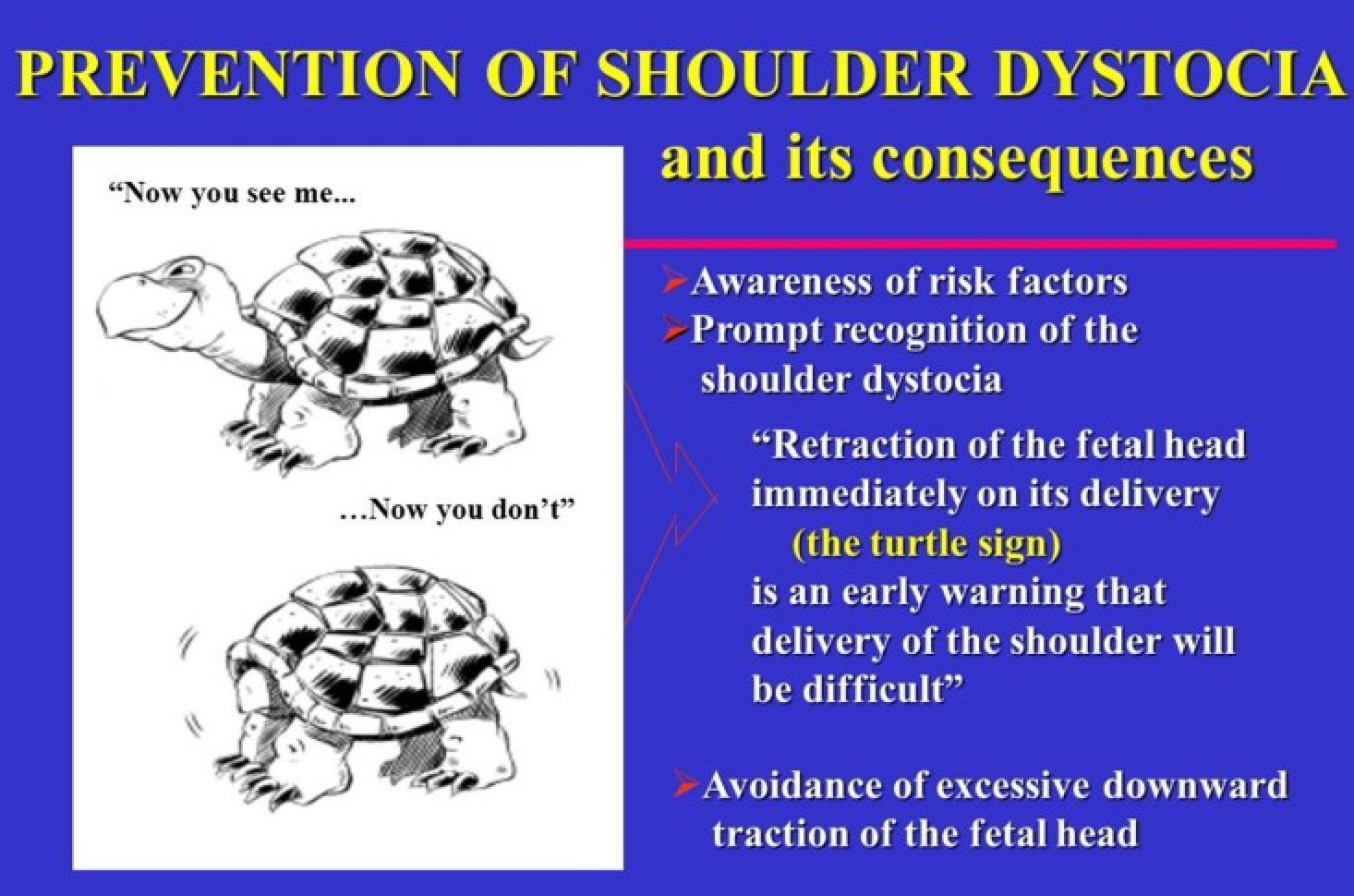
What are S/S of shoulder dystocia?
delay in delivery of shoulders following delivery of the head, “Turtle sign”
What should you do when there is a risk for shoulder dystocia?
Do’s:
Call for help (NICU)
McRoberts maneuver
Suprapubic pressure (these 2 relieve about 70% of
shoulders)
Reposition to all hand and knees (Gaskins)
Empty bladder
What should you not do when there is a risk for shoulder dystocia?
Don’t:
Fundal pressure
Vacuum delivery once the shoulder is called.
C-section is a last resort (Zavanelli maneuver)
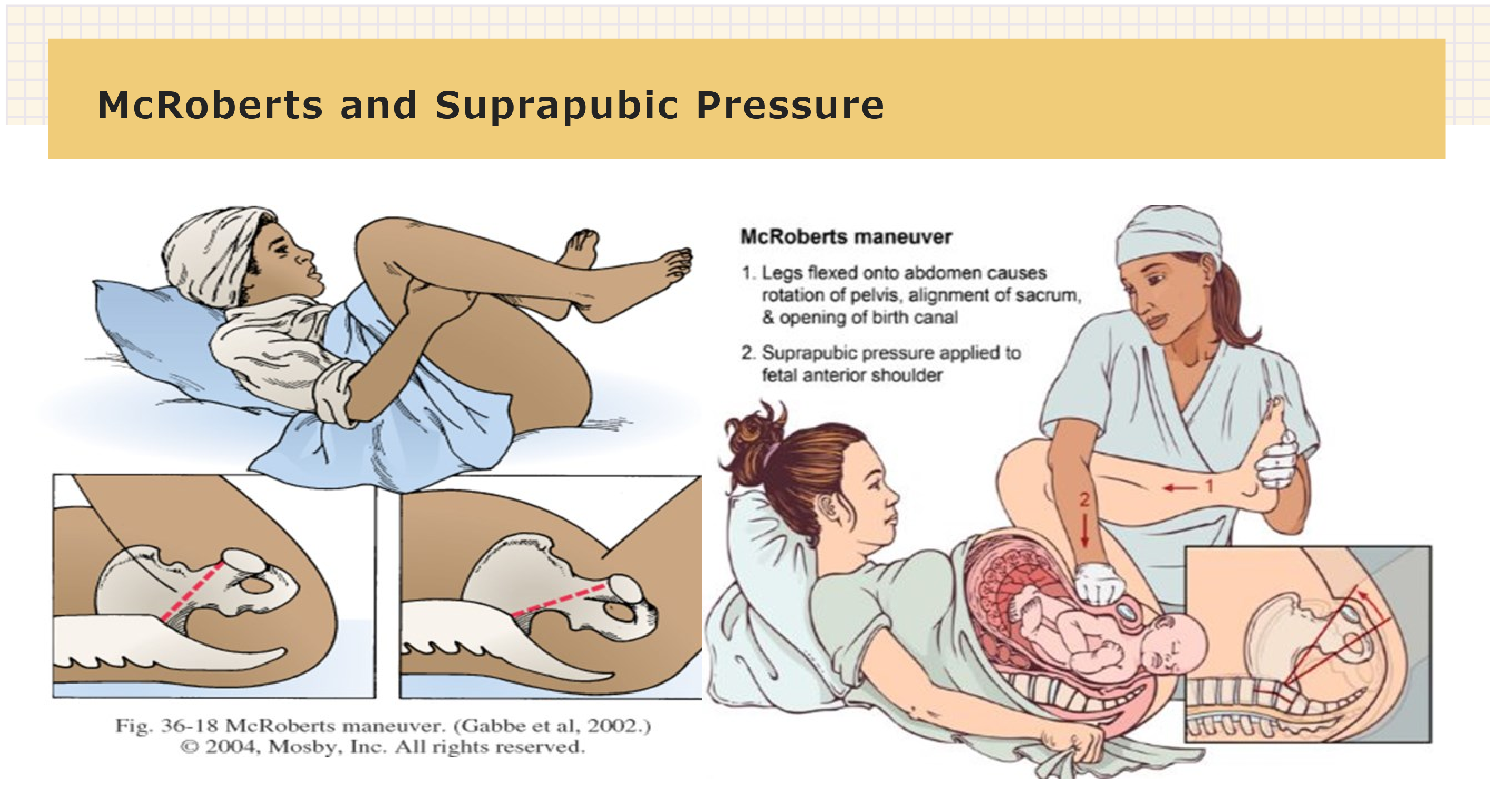
What is the purpose of McRoberts and suprapubic pressure?
To facilitate the delivery of shoulders by relieving shoulder dystocia during childbirth.
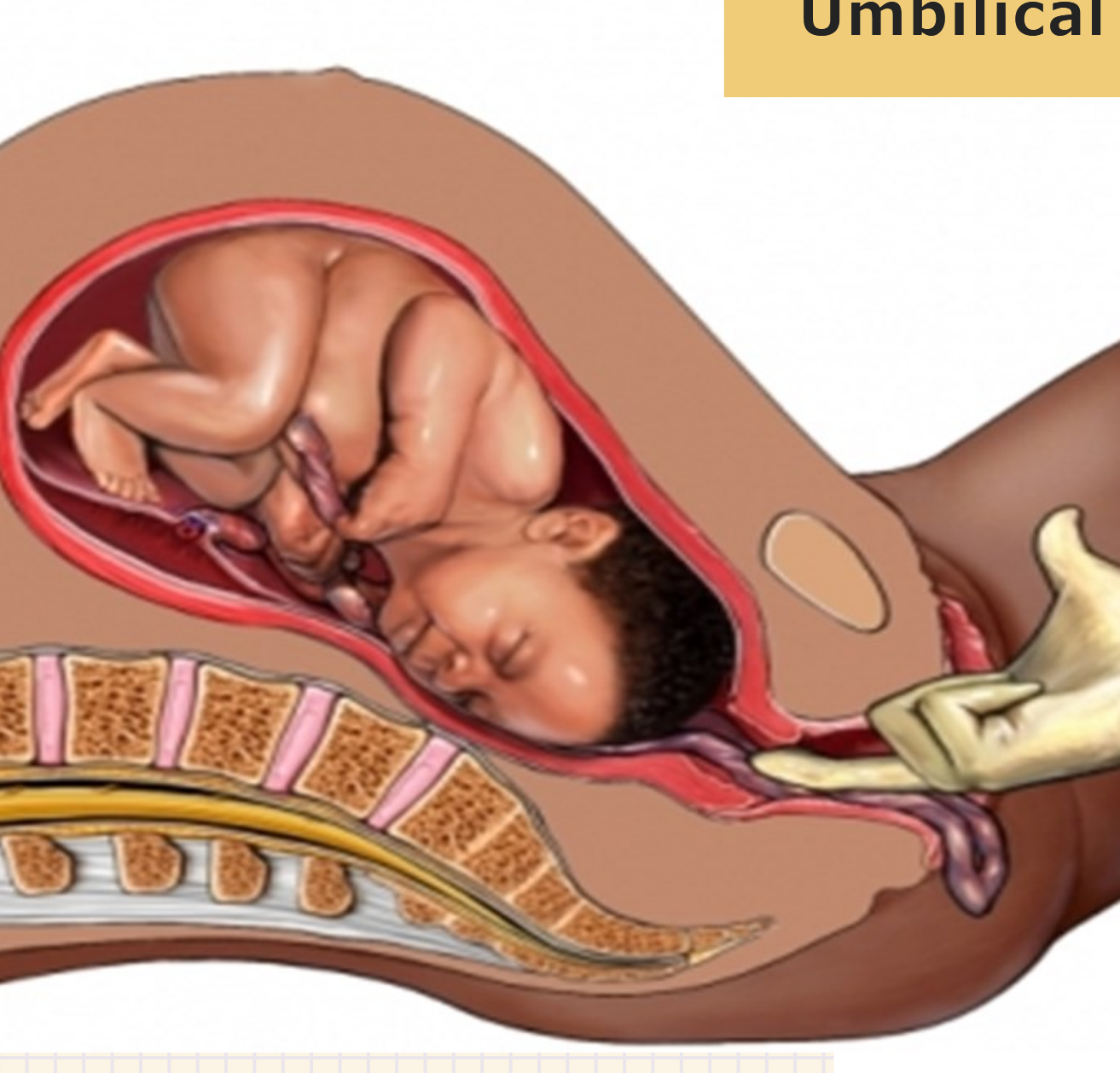
What is umbilical cord prolapse?
A condition where the umbilical cord slips ahead of the presenting part of the fetus, potentially leading to fetal distress due to reduced blood flow.
What are risk factors related to umbilical cord prolapse?
Risk factors - long cord, anything that prevents engagement of the fetal head in the cervix (malpresentation, CPD, multiple gestation, polyhydramnios, congenital anomalies) Amniotomy should be delayed until head engages in cervix.

What are fetal consequences of cord prolapse?
Compression of cord leading to asphyxia or death
What are S/S of cord prolapse?
S/S - visualization of the cord at the vaginal introitus, palpation of pulsing cord on vaginal examination, profound bradycardia on monitor tracing

What is are management efforts for cord prolapse?
Management: “rodeo delivery” do not remove your hand!! Knee-chest or Trendelenburg position, lift presenting part off cord, STAT c-sectionto relieve cord compression and deliver the baby.
Why are hemorrhagic disorders a priority?
Hemorrhagic disorders are a priority due to the potential for significant maternal and fetal morbidity or mortality, as they can lead to rapid blood loss and complicate the delivery process. Any bleeding in pregnancy = medical emergencies; Significant cause of maternal death. Blood loss may reach 40% before hypovolemic shock occurs. 15% of maternal cardiac output (1 L/min) flows through the placental bed at term. Unchecked bleeding can result in complete exsanguination in 8 -10 minutes
What are maternal and fetal risks during a hemorrhagic disorder?
Maternal risks include: hypovolemia, anemia, infection, preterm labor/birth
Fetal risks include: blood loss /anemia, hypoxemia, hypoxia, anoxia, preterm birth
Any bleeding is associated with increased maternal &/or fetal morbidity & mortality
What is the incidence of pregnancies complicated by bleeding?
1 in 5 pregnancies complicated by bleeding (20%); varies by trimester
Most bleeding in 1st trimester related to spontaneous abortion, gestational trophoblastic disease and cervical insufficiency (Incompetency). Most hemorrhagic deaths are related to ectopic rupture. Most bleeding in 2 nd & 3 rd trimester related to placenta previa
How does hemorrhage affect blood levels in terms of lab values?
Hemorrhage: a 10% decrease in hematocrit OR a need for a transfusion
Hemoglobin will decrease 1 -1.5 g /dl & Hematocrit will decrease 2 -4% for each 450-500 cc of blood loss
Hemorrhage in Vaginal deliveries = 3.9%
Cesarean deliveries = 6.4%
What is a miscarriage?
A miscarriage, also known as spontaneous abortion, is the loss of a fetus before the 20th week of pregnancy. It is often characterized by vaginal bleeding, cramping, and tissue passing. (SAB, threatened, inevitable, incomplete, Missed, Habitual). Can’ t cause or prevent
What is a ectopic pregnancy?
An ectopic pregnancy occurs when a fertilized egg implants outside the uterus, most commonly in a fallopian tube. This can lead to serious complications and is a medical emergency. Pregnancy in wrong place. 3rd most common pregnancy related death
in US
What is cervical insufficiency? Treatment?
(cervical incompetence) painless cervical dilation, cervical weakness – TX: Cervical Cerclage, a surgical treatment to support the cervix during pregnancy, preventing premature birth.
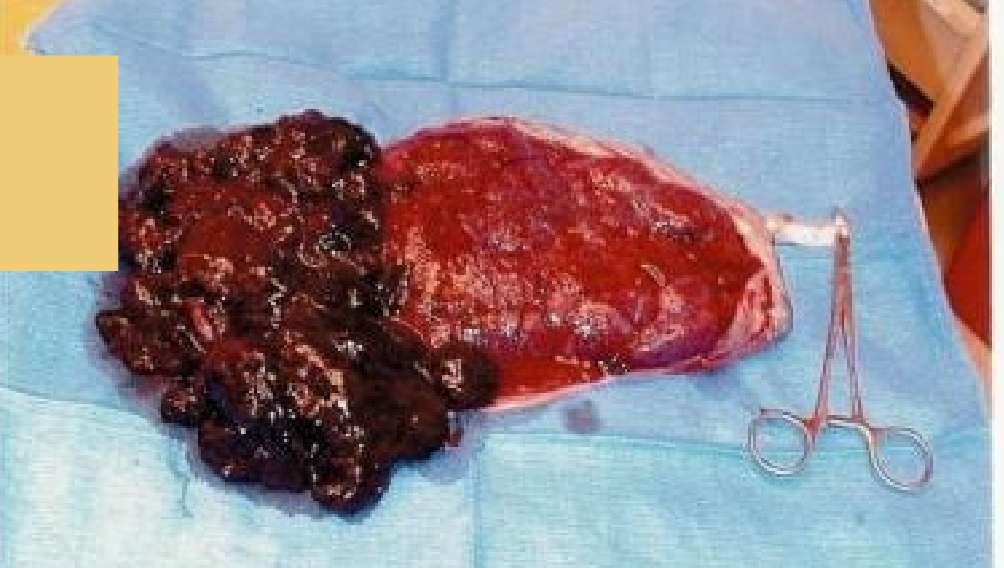
What is hydatiform mole (molar pregnancy)?
A hydatiform mole is a rare condition characterized by the abnormal growth of trophoblastic tissue in the uterus, which can lead to a non-viable pregnancy. It occurs when the sperm fertilizes an empty egg, resulting in an overgrowth of placental tissue instead of a developing embryo.
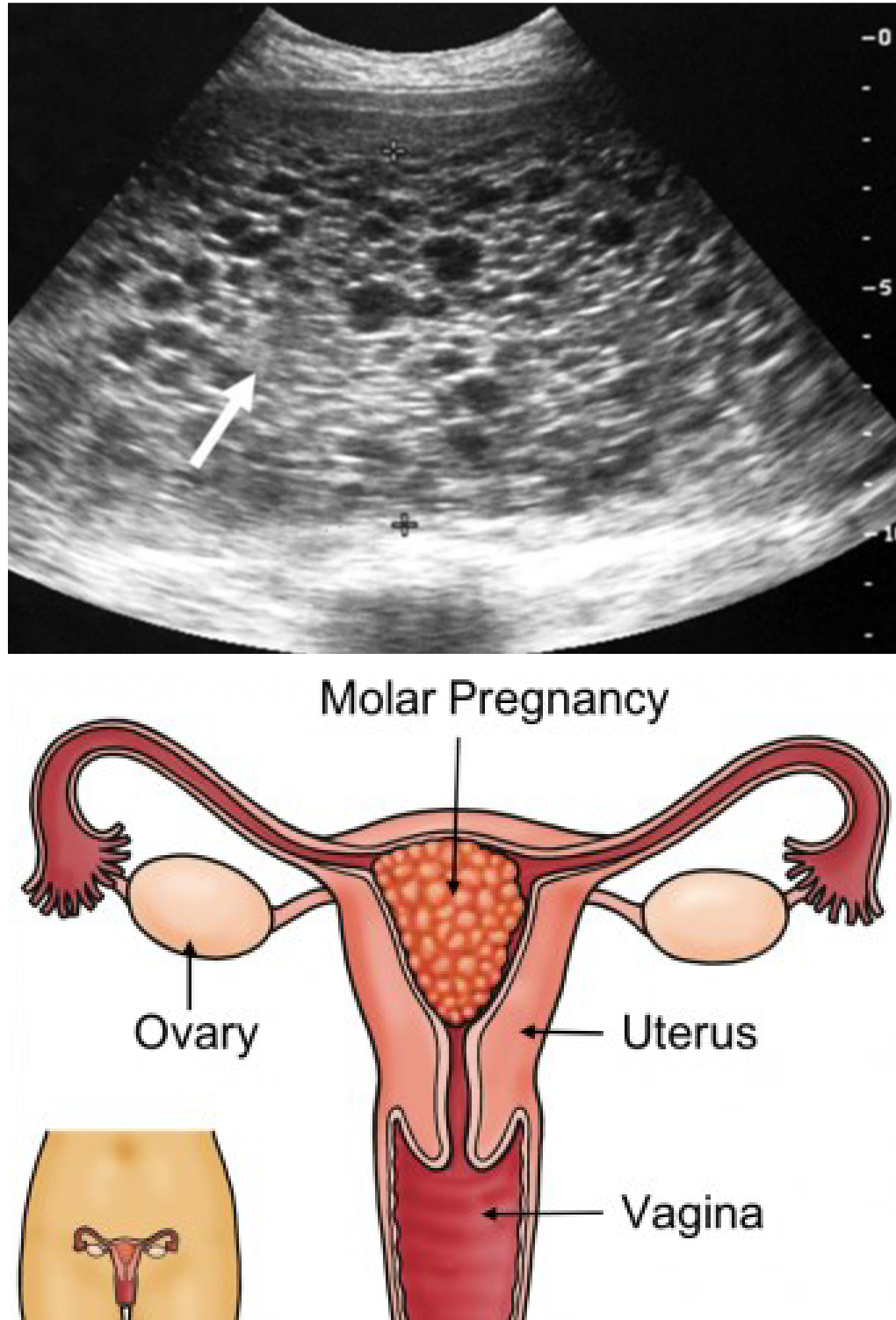
What is a consequence of molar pregnancy? Treatment?
Proliferation of rapid dividing cells that invade wall of uterus = forming cancer
TX: evacuate uterus, Methotrexate ( Chemotx), follow with serial hCG levels, avoid pregnancy X’s 1 year
What are placental abnormalities such as placenta previa?
Placental abnormalities are conditions where the placenta is improperly positioned in the uterus, potentially leading to complications during pregnancy and delivery, such as bleeding or premature birth. One common type is placenta previa, where the placenta covers the cervix.
What are S/S of placenta previa?
S/S: PAINLESS BRIGHT RED BLEEDING, intermittent or continuous starting in the 2nd trimester
What are risk factors of placenta previa?
Risk factors: AMA, smoking, Multiple gestation, fibroids, uterine scarring.
How are placental abnormalities like placenta previa diagnosed?
Diagnostics: ultrasound, may be asymptomatic until first bleeding episode
What are some patient education/management for placental abnormalities?
Patient education /management: pelvic rest, avoid speculums and vag exams, steroids, scheduled c -section around 36-37 weeks
What is cretas?
A condition where the placenta abnormally adheres to the uterine wall, potentially leading to severe complications during delivery. This condition includes types like placenta accreta, increta, and percreta, which vary based on the depth of invasion into the uterine wall.
What is accreta?
growth into the myometrium (most common, caused by scar tissue from previous c-sections)
What is increta?
deeper into the myometrium where the placenta invades the muscular layer of the uterus, increasing the risk of complications during delivery.
What is percreta?
through the uterine wall and out (might attach to bladder or bowel) - mush have hysterectomy due to risk of hemorrhage.
What are treatments for cretas?
High risk for hemorrhage. Betamethasone, scheduled c -section, blood on hold /in OR and potential hysterectomy after delivery if necessary.
What is placental abruption?
The placenta separates from the uterine wall prematurely. Partial or complete, concealed or free flowing hemorrhage.
What are S/S of placental abruption?
Sudden, intense pain , high frequency / low amplitude ctx, rigid board like palpation of abdomen, may or may not have vaginal bleeding
What are risk factors for placental abruption?
HTN, trauma (most common), infection, Smoking, Drugs, IUPC placement, fibroids (highly vascular, competing or blood supply)
What is nursing management for placental abruption?
O2, IV’s, Massive blood transfusion protocol, Stat c -section
What is valamentous cord insertion?
A condition where the umbilical cord inserts into the placenta at the fetal membranes rather than directly into the placenta, increasing the risk of vessel rupture and hemorrhage. Risk- massive fetal hemorrhage with ROM >50% death rate with ROM.
What is management efforts for velamentous cord insertion?
Management: scheduled c -section (97% survival rate)
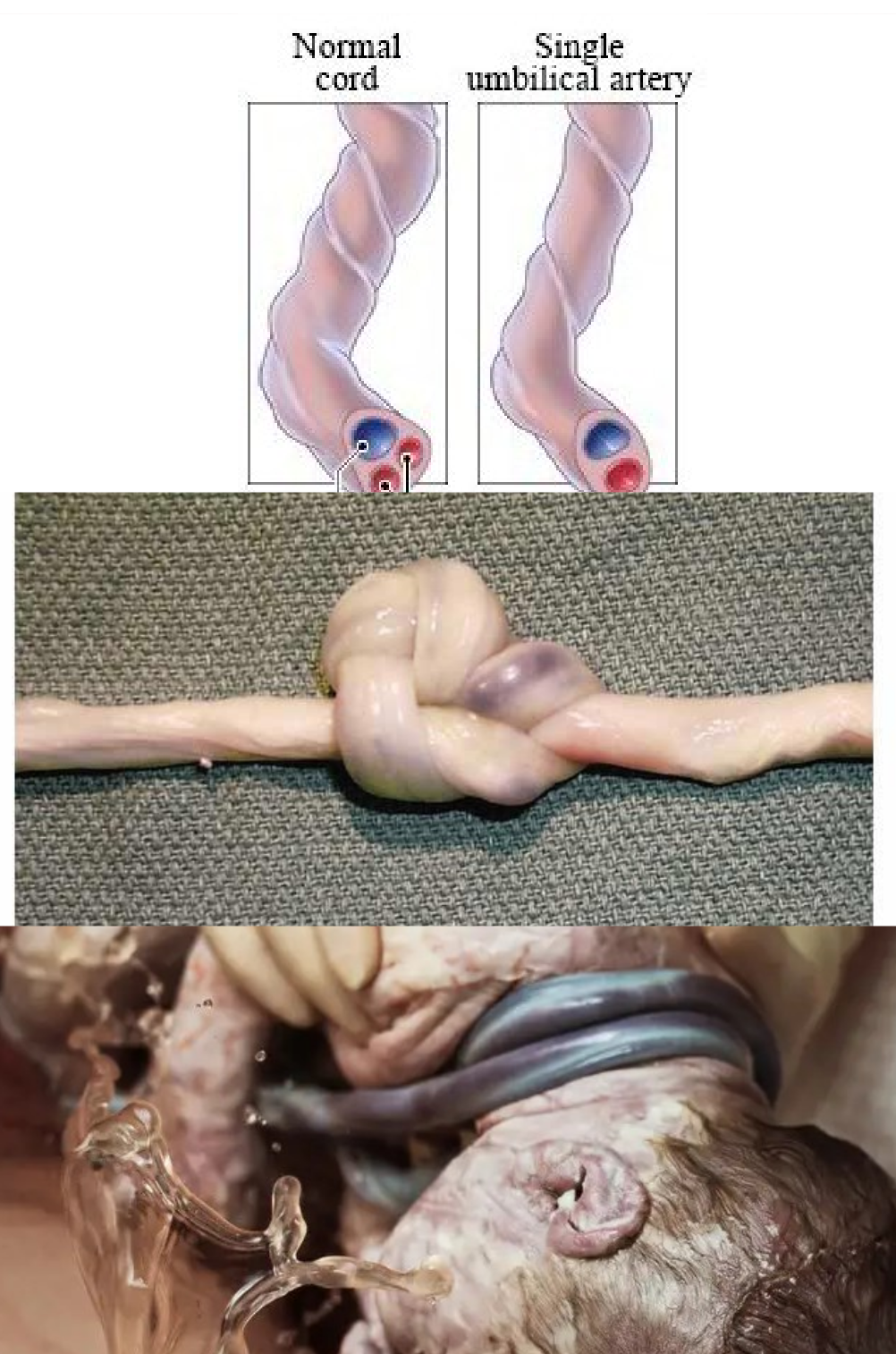
What are true knots, nuchal cord, and 2 vessel cords?
Types of cord abnormalities during pregnancy that can complicate labor and delivery. True knots can constrict blood flow, nuchal cords wrap around the fetus's neck, and two vessel cords indicate a potential risk for congenital anomalies. Associated with variable decelerations, fetal intolerance of labor. SUA- signal umbilical artery
What is the nursing management for cord abnormalities?
low and slow with Pitocin management. Potential for CO2 and lactic acid build up in fetus. Causes - can be benign but can be an indicator or other abnormalities (renal, GI, spinal and cardiac)
What is uterine rupture?
Tearing or opening of the uterus into the abdominal cavity, usually at the site of a scar from previous uterine surgery. This serious complication can lead to severe maternal and fetal morbidity and mortality, necessitating immediate surgical intervention.
What are risk factors for uterine rupture?
Risk factors - previous uterine surgery (cesarean section, myomectomy), tumultuous
labor, multiparity combined with Pitocin administration, obstructed labor, excessive
fundal pressure, use of forceps, violent pushing, shoulder dystocia, trauma, LGA or
Polyhydramnios
What are S/S for uterine rupture?
abdominal pain (irritated diaphragm or shoulder pain, loss of fetal station, palpable fetal parts on Leopold’s maneuvers, fetal intolerance (what kind of strip would you suspect?), sudden loss of uterine tone to palpation or on monitor, may or may not have vaginal bleeding, shock
What are maternal and fetal complications of uterine rupture?
Maternal complications - pain, hemorrhage, DIC, death
Fetal complications - hemorrhage, death
What are nursing care for uterine rupture?
O2, stat c-section, IVF, labs (coags), Massive blood transfusion policy
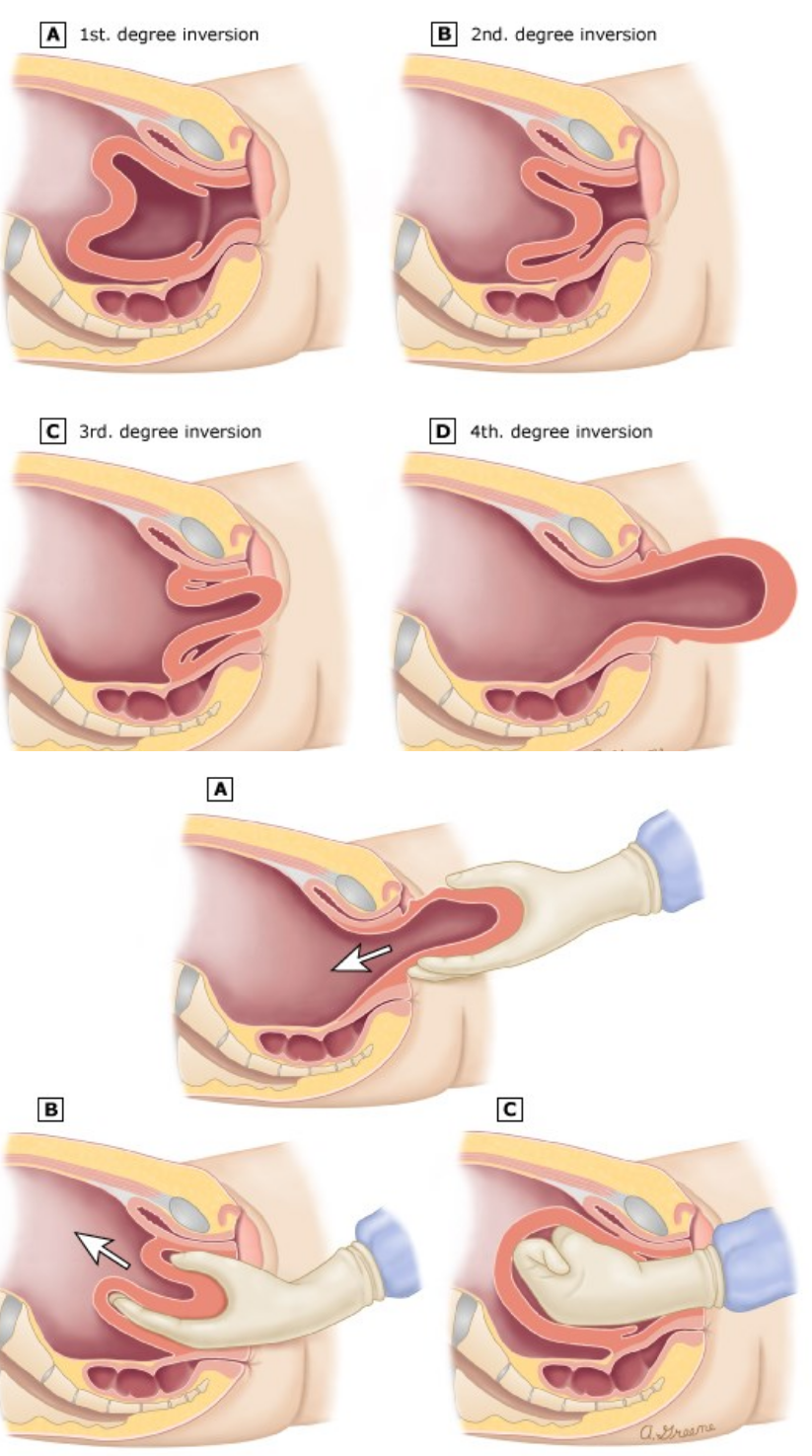
What is prolapsed or inverted uterus?
Uterus turns inside out and prolapses out of the body cavity. Most commonly happens with delivery of the placenta.
What are causes of prolapsed or inverted uterus?
fundal pressure, too firm traction on umbilical cord during 3rd stage of labor, uterine atony
What are S/S of prolapsed or inverted uterus?
mass palpated or observed below cervix, pain, bleeding
What are nursing management efforts for prolapsed or inverted uterus?
O2, fluids, blood, antibiotics. The uterus must manually be replaced. MUST HAVE OTHER HAND ON LOWER UTERINE SEGMENT BEFORE FUNDAL MASSAGE.
What is anaphylactoid syndrome of pregnancy (amniotic fluid embolism)?
A rare but serious condition that occurs when amniotic fluid enters the mother's bloodstream, triggering a severe allergic reaction. This can lead to respiratory and cardiovascular collapse.
What is the level of incidence for anaphylactoid syndrome of pregnancy?
Amniotic fluid containing particles of debris enters maternal circulation causing
cardiac and reparatory collapse. Occurs at the point of separation of the placenta
from the uterine wall.
-1 in 60-80k deliveries (70% in labor, 20% in c /s, 10% PP)
-IF they make it to ICU, 25% death rate
-IF patient survives, 80% have neuro dama
What is the risk factors for anaphylactoid syndrome of pregnancy?
multiparity, AMA, macrosomia, rapid labor, meconium, IUFD, abruption
What are S/S for anaphylactoid syndrome of pregnancy?
PROFOUND shock: sudden dyspnea, cough, tachycardia, fetal bradycardia, PE, DIC (bleeding /bruising), hypotension, cardiac arrest, Death (mortality rates as high as 86%)
What is treatment for anaphylactoid syndrome of pregnancy?
Anecdotal treatment ( A O-K for AFE) Atropine 1mg, Ondansetron (Zofran) 8mg, Ketorolac (Toradol) 30mg
What is preterm labor?
The onset of labor before 37 weeks of gestation, leading to the potential for premature birth. Affects 1 in 10 births in the U.S. Causes at least 75% of neonatal deaths not due to congenital malformations. Rate of preterm births has not changed over the past 40 years
What are the consequences of preterm labor?
Infants born weighing less than 1,500 g (3.3 pounds) are approximately 200 times more likely to die in the first year of life than those weighing more than 2,500 g (5.5 pounds).
10 times more likely to be neurologically impaired.
Preterm births disproportionately contributes to developmental delay, visual and hearing impairment, chronic lung disease, and cerebral palsy
Preterm labor risk factors
Multiples only 1.1% of all pregnancies result in 10% of
preterm births.
Previous PTD
Uterine or cervical anomalies (incompetent cervix)
Infection (UTI, chorioamnionitis, STI, toxoplasmosis,
CMV, varicella, ect.)- the earlier the PTL starts, the more
likely an infection was the cause)
Polyhydramnios
PROM
Placental hemorrhage,
Maternal age extremes (younger than 16, older than 40)
1 or more spontaneous 2nd trimester abortions
PTL other risks
Obesity
DM
HTN
Trauma
Smoking=IUGR
Etoh
Drugs
PPROM
Stress
Low socioeconomic
Short intervals between pregnancies (<18months)
Family history
Poor prenatal care
S/S of PTL
Regular uterine contractions (6 or more in an hour)
Lower abd cramping (may be mistaken for gas)
Low back pain/discomfort – similar to menstrual cramps
Change in vaginal discharge/ROM
Pelvic pressure
What is positive fetal fibronectin?
A test used to measure fetal fibronectin levels in vaginal secretions, which can indicate the likelihood of preterm labor. A positive result suggests a higher risk of delivering within the next few days to weeks. If present between 22 -34 may indicate she is at risk for PTD with in 2 weeks average. More predictive that she WILL NOT deliver within next 2 week if FFN test is negative. (less than 1% chance of delivery with in 2 weeks)
What are preterm labor management efforts?
NO sterile vaginal examination (SVE) nor a transvaginal ultrasound (vaginal US) will be performed
HYDRATE and REST/Sedate!!!!!!!
Magnesium sulfate (Fetal neuro protection for <32weeks - decreased risk of
CP- vasodilates vessels to brain-increases blood flow)
Beta-mimetic agents- off label use Terbutaline- can delay PTD by 48-72hours.
Side effects- increase HR, anxiety, n/v arrhythmias, pulmonary edema
Indomethacin- (prostaglandin inhibitor/NSAID)
Nifedipine- CA channel blocker-decreases contractility of smooth muscles
Corticosteroid Therapy (effects within 48hrs of administration, repeat every 7 days)
Bedrest: not been proven to be effective. Loss of CA, muscle tone, weight loss, financial and emotional damage
What are magnesium sulfate management efforts?
IV, M gSO4
Monitor DTRs/VS/I&O
Monitor serum mag levels: Serum magnesium levels ranging from 1.5-2.5 is a normal value outside of OB.
However, 4 to 6 mEq/L are considered therapeutic in OB when treating hypertension or preterm labor, whereas levels more than 8 mEq/dL are generally considered toxic.
@ 8-10mEq/l: loss of DTRs
@ 12-17 mEq/l: respiratory depression
@ 15-17 mEq/L: paralysis
@ 25-30 mEq/l: cardiac arrest
Mg is administered to prevent preterm labor and provide fetal neuroprotection. It requires monitoring of deep tendon reflexes, vital signs, and intake/output, while also checking serum magnesium levels to ensure they remain within therapeutic range.
What is the level of survivability of preterm delivery at varying gestations?
22 weeks- rare (usually with larger infants)
23 weeks- 0-8%
24 weeks- 15-20%
25 weeks- 50-60%
26-28 wks- up to 85%
29 weeks- > 90%
Preterm delivery
Delivery at a facility capable of providing the highest quality of care for the infant is
imperative for achieving an optimal perinatal outcome.
Aggressive obstetrical and neonatal interventions have had minimal effects on the
survival of infants born at 22-23 weeks
gestation.
Criteria for current viability threshold is 24 weeks gestation or 600 g weight.
What is post term delivery?
Delivery that occurs after 42 weeks of gestation, which can increase risks for both the mother and the baby, including potential complications such as meconium aspiration and decreased amniotic fluid.
What is the consequence of post term delivery?
>42 weeks
Peak amniotic fluid is 36-37weeks, slow gradual decline after that
Neonate have dry, peeling skin; New study shows higher c /section rates with spontaneous labor at 4 1 weeks + in comparison to IOL at 39-40weeks
What is pregestational?
Pregestational - When the woman is known to have diabetes prior to becoming pregnant
Maternal type 1 and type 2
at risk for: congenital abnormalities - cardiac and neural tube. If A1C >8.5 - 40% chance ofcardiac defect.
What is gestational diabetes?
When the woman develops diabetes during the pregnancy, or it is first recognized during pregnancy
Diet controlled - A1 or PO meds, or insulin- A2
What are maternal risk for GDM?
Maternal risk: UTI, operative deliver y, SAB/Stillbir th /IUFD, preterm delivery, healing/infection
At risk for: newborn hypoglycemia, asphyxia, macrosomia/LGA, fetal acidosis, miscarriage, fetal death, vascular flow problems, shoulder dystocia, newborn RDS from delayed surfactant caused by excess glucose***
GDM pathophysiology
Gestational diabetes mellitus (GDM) occurs when the body's inability to produce enough insulin leads to elevated blood glucose levels during pregnancy. This condition is often related to increased insulin resistance and hormonal changes associated with pregnancy. Goes in hand with per-ecclampsia.
What is the treatment for GDM?
The treatment for gestational diabetes mellitus (GDM) involves dietary modifications, blood glucose monitoring, and, if necessary, medication such as insulin or oral hypoglycemic agents to maintain normal blood sugar levels during pregnancy.
1st trimester: insulin needs decrease
2nd/3rd trimester: insulin emands increase (more placental mass)
Postpartum/lactation: insulin demands at its lowest!
What are risk factors of GDM?
Risk factors for gestational diabetes mellitus (GDM) include obesity, a history of GDM in previous pregnancies, advanced maternal age, family history of diabetes, and certain ethnic backgrounds. Additionally, women with polycystic ovary syndrome (PCOS) or those who have had large babies in the past are at greater risk.
GDM screening
Screening Test at 24-28 weeks (earlier if risk factors present)
1 hr gluconla: 75gm oral glucola
1 hr > 140mg/dl … 3hr GTT needed
3hr glucola: 75 gm glucola after 3 day high carb diet at least 150 g/d
Should be:
Fasting < 95
One hour < 180
Two hour <155
Three hour < 140
If 2 or more above = gestational diabetes
What are patient management efforts for GDM?
Will require more frequent follow up (More OB appointments, labs, NST’s, U/S, BPP, Fetal echocardiograms, EFM)
May require more medication changes /adjustments
Multi-disciplinary management team
BGFS q2hr with labor. Target is to keep bs
>120mg /dl while in labor- decreases risk for
hypoglycemia in NB
If on insulin drip during labor - 2nd IV required.
What are hypertensive disorders of pregnancy?
Second leading cause of maternal death and is related to other complications associated with the hypertension:
•stroke, abruption, hepatic failure /rupture, eclampsia and acute renal failure
Hypertensive disorder risk factors
◦Primigravida (6-8 times the risk)
◦Age extremes (<17 or >40)
◦Diabetes
◦Pre-existing hypertensive, vascular, collagen vascular or renal disease
◦Multiple gestation
◦Hydatiform mole
◦Preeclampsia in previous pregnancy, family history
◦First pregnancy with current partner (immune response
◦Obesity
How do you classify between two types of hypertension?
Chronic Hypertension: hypertension before 20 weeks or remains elevated for 12 week PP 140/90
Hypertensive disorders of pregnancy: Gestational Hypertension, Chronic Hypertension with superimposed preeclampsia, Preeclampsia/Eclampsia, HELLP
What are risk factors for chronic HTN?
High Risk for abruption, and /or stroke- intercranial bleeds due to prolonged endothelial damage.
What are chronic HTN treatments?
Ace inhibitors /ARB’s are fetotoxic to kidney development.
Beta blockers /calcium channel blockers /Thiazides are preferred
(labetalol)
What is gestational HTN?
Elevated B/P after 20w eeks or 1st 24 hours postpartum with out signs of Preeclampsia
Elevation to 140/90 on 2 occasions 6 hours apart
Proteinuria under 300mg/dl
No previous history of HTN – return to normal within
6 wks PP If hypertension persists for longer than 12 weeks PP = chronic HTN
Chronic HTN with superimposed Pre-E
Chronic hypertension increase risk of Preeclampsia by 25%
Morbidity is 25-35% higher than with “just” Hypertension
New onset of proteinuria
Hypertension + baseline proteinuria before 20 weeks that gets worse throughout pregnancy
Sudden spike in BP that was previously well controlled
High risk for stroke and abruption