middle adult development
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
stages of adulthood
- early adulthood: 21 to 34/40 (depends on source)
- middle adulthood: 40 to 65
- late adulthood: 65+

central development tasks of middle adulthood
- expressing love through more than sexual contact
- being proud of accomplishments
- maintain a standard of living
- adjusting to the physiologic changes of middle ages

body functions and structures of middle adulthood: cognitive change
- changes are typically mild
` link between physical health conditions (diabetes, hypertension, hypercholesterolemia)
` can reduce cognitive decline with healthy lifestyle choices
` can improve with cognitive training

do people care more about doing every day things or mobility
most people care more about doing everyday things cognitively than not being able to get around mobile
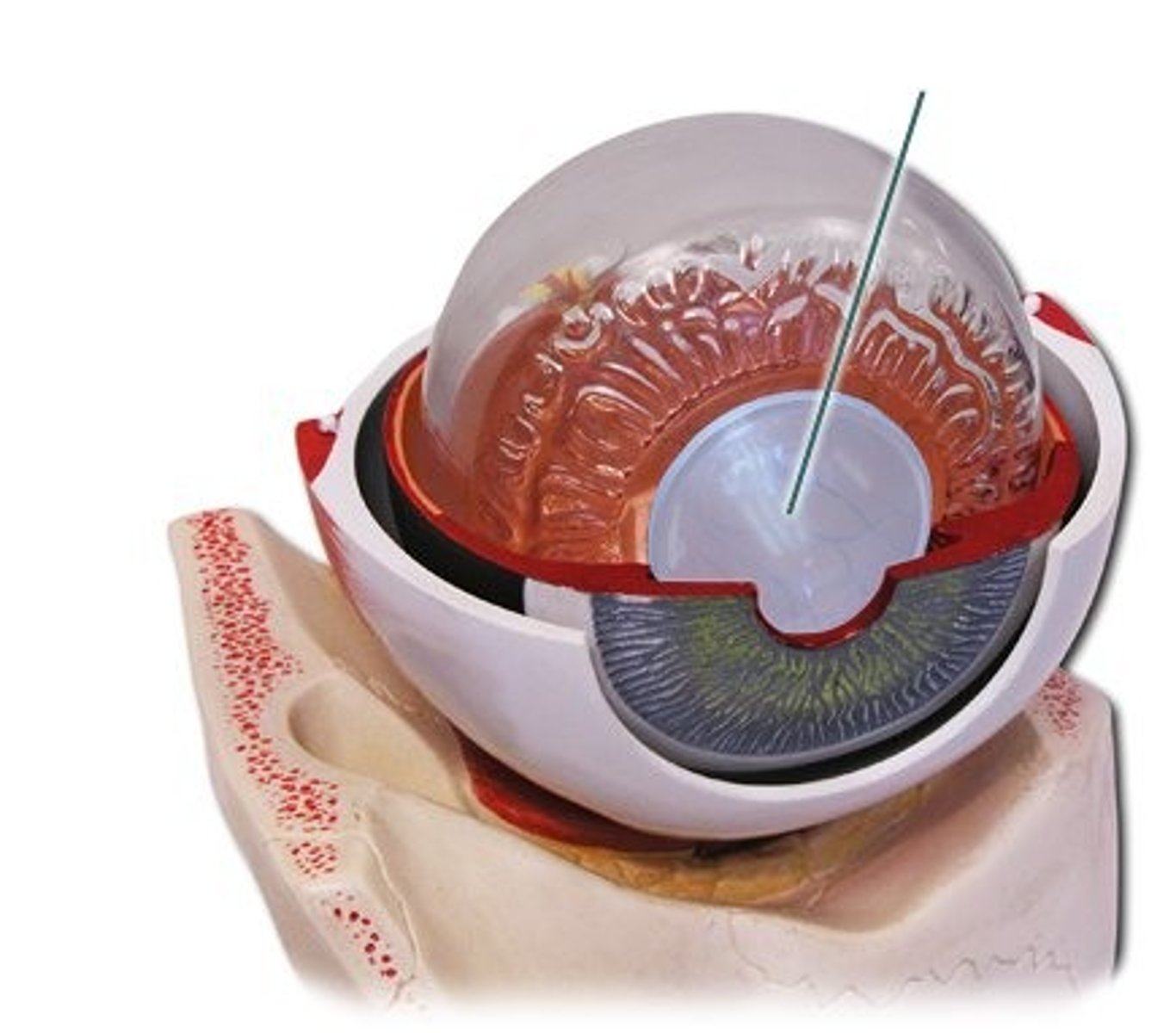
body functions and structures of middle adulthood: vision
- mostly stable, normal age related decline starts around 50
- visual accommodation worsens with age, likely requiring reading glasses or changes to pre-existing correction (ex bifocals)
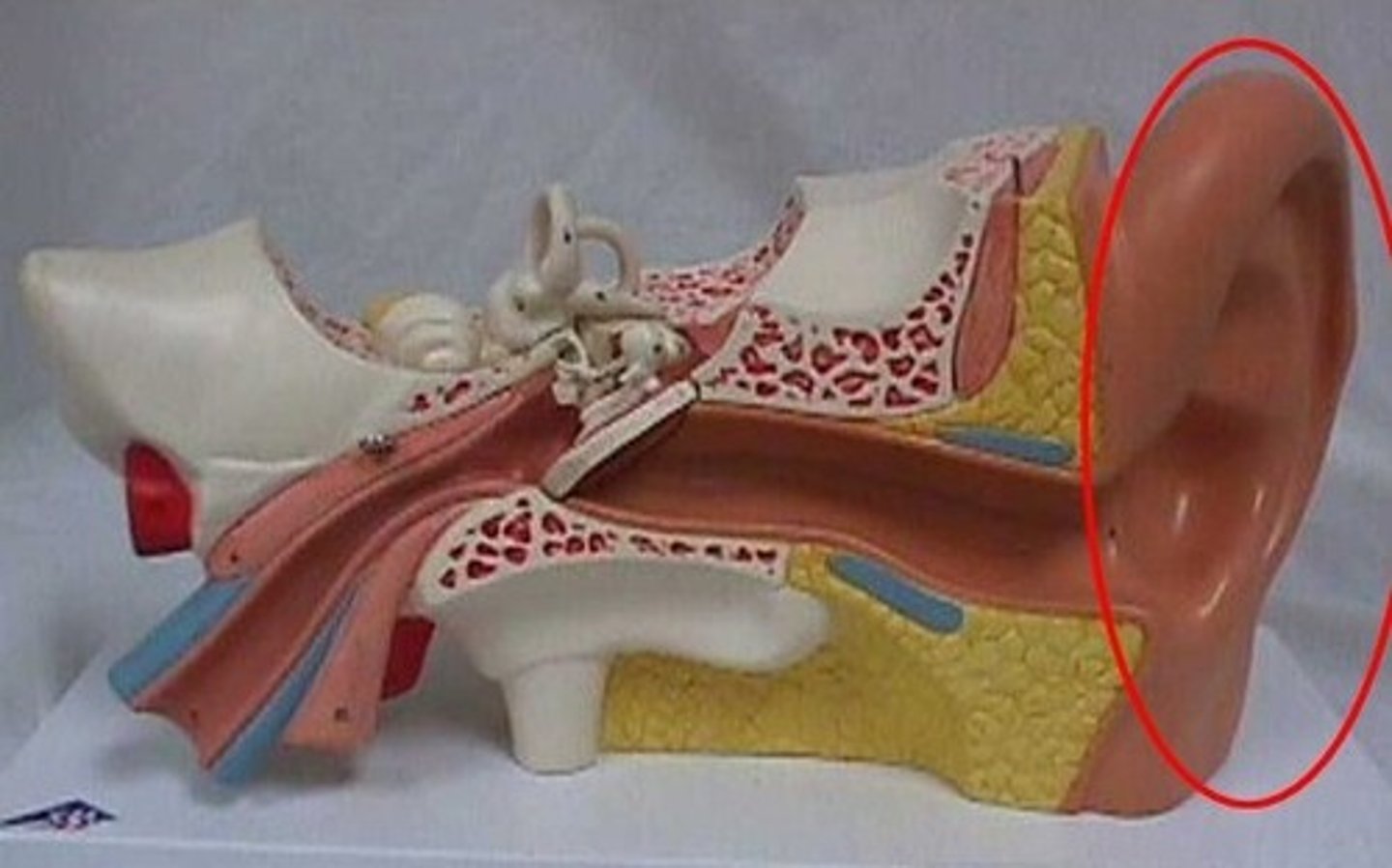
body functions and structures of middle adulthood: hearing
- Sensorineural hearing loss caused by prolonged exposure to loud noises
- Age related hearing loss
body functions and structures of middle adulthood: physical
- Changes to bones (ex: osteoporosis, osteopenia (fails to form new bones)
- Loss of lean body mass
- Decreased muscle force (slight between 40-65)
- Decreased flexibility
- Decreased cardiovascular fitness

activities and participation in middle adulthood
- Competence in a diverse array of activity demands, occupations, and roles
- Typically, no decline in ability to participate in various areas of occupation
- Potential role strain, feelings of anxiety/tension associated with all of the roles
- Expectation of having a refined process with a multitude of skills (e.g. home management, community mobility, finances, health management, etc.)
body functions and structures that change in late adulthood
- Age related declines become more noticeable
- Cognitive changes
- Sensory changes
- physical
cognitive changes in late adulthood
- Impaired working memory and inhibitory control
- Slower processing speed
- Age associated memory impairments
- Benign senescent forgetfulness (senior moments, can't recall that name of that one actor)

sensory changes in late adulthood
- Decreased acuity with increased contrast needs
- Decreased dynamic visual acuity (i.e. ability to see clearly when person and/or object is moving)
- Impaired ability to see color
- Decreased peripheral vision
- Decreased hearing, taste, and smell (taste you might not know something is spoiled, for smell you might have decreased appetite)
- Decreased vestibular system functioning

physical changes in late adulthood
- Continued loss of lean body mass and increase in body fat
- Continued incidence of osteoarthritis, osteoporosis, decreased range of motion and flexibility
- High incidence of kyphosis
- Impaired balance, slower walking, impaired stair climbing, shorter reach, impaired adls
- Cardiovascular changes (htn, orthostatic hypotension, etc.)
- Thinning skin and easily bruised

defining death
- part of the life cycle
- What are your beliefs about death? What feelings are often associated with death?
- How may your beliefs and/or feelings impact the therapeutic relationship?
during the grieving process what does occupational accommodation refer to?
transformation of occupational patterns in response to changing reality
`assimilation involves fitting loss into one's current occupational patterns
people who lost a loved one often do what to be close to the deceased
engaging in occupations that were meaningful or closely related to the deceased.
principles of palliative care
- Respects the goals, likes and choices of the dying person
- Looks after the medical, emotional, social and spiritual needs of the dying person
- Supports the needs of the family
- Helps gain access to needed health care providers and appropriate care settings
- Builds ways to provide excellent care at the end of life

ot and hospice
- Philosophy AND system of care that embodies an individualized, humanistic approach for people who are dying
- Provides end of life care
- Focus on living and dying
the team of hospice includes what professionals
headed by physician and under them is:
- nurse
- ot
- pt
- speech
- social work
- home care aides
- counselors
- pastoral support
- psychologists
what services are provided with hospice
- drugs for pain relief/symptom control
- medical supplies and equipment
- respite care for family caregivers
- bereavement support
*normally used when 6 months of is estimated
areas of process in otpf
- evaluation
- intervention
- outcome

overview of process
- service delivery approaches
- practice within organization and systems
- occupational and activity analysis
- therapeutic use of self
- clinical and professional reasoning
service delivery approaches: direct
working directly with client
service delivery approach: indirect
- consultations
- part of a multidisciplinary team, telehealth
therapeutic use of self considers what
- an intervention approach that is inherent to the OT practice
- requires a conscious effort to optimize client interaction
why is collaboration essential in person centered care
- Providing choices
- Allowing for decision making
- Encourages active contribution when setting goals for therapy process
therapeutic use of self asks how therapists
- connect with their clients
- accommodate OTP interactions to a client need
- build relationships
- motivate
- ensure mutual participation in the OT process
model of skill acquisition
- stage 1: novice
- stage 2: advanced beginner
- stage 3: competence
- stage 4: proficient
- stage 5 expert
stage 1: novice
- concrete thought process, leaves no room for negotiation
- "when this happens, I do this"
stage 2: advanced beginner
- clinician keeps other people or past experiences in mind when making decisions
- "I've seen this before and this worked best
stage 3: competence
- it depends
- "when this happens, i consider several options and choose the best one for this situation"
stage 4: proficient
- less break down of information
- looking at the client as a whole, more intuition that comes with this stage
- "when this happens, i intuitively sense what is most important and respond accordingly"
stage 5: expert
- don't know how to explain the decisions they made
- intuition
- "i just know what to do"
Mrs. Jones is a 45 y/o right-hand dominant nurse who sustained a right distal radius fracture after a fall off her bike. She is coming to you for OPOT 3- weeks after her cast was removed. She presents with: decreased wrist ROM and grip strength, pain with daily tasks (brushing teeth, combing hair, lifting items) Client goal: "Get back to work and right hand to be back to normal"
response: Working on the injury, range of motion exercises, strengthening exercises
novice
Mrs. Jones is a 45 y/o right-hand dominant nurse who sustained a right distal radius fracture after a fall off her bike. She is coming to you for OPOT 3- weeks after her cast was removed. She presents with: decreased wrist ROM and grip strength, pain with daily tasks (brushing teeth, combing hair, lifting items) Client goal: "Get back to work and right hand to be back to normal"
response: Working on the injury, range of motion exercises, strengthening exercises but also drawing on past experiences like using a hot pack to begin session
advanced beginner
Mrs. Jones is a 45 y/o right-hand dominant nurse who sustained a right distal radius fracture after a fall off her bike. She is coming to you for OPOT 3- weeks after her cast was removed. She presents with: decreased wrist ROM and grip strength, pain with daily tasks (brushing teeth, combing hair, lifting items) Client goal: "Get back to work and right hand to be back to normal"
response: taking into consideration what the client does regularly
competent
Mrs. Jones is a 45 y/o right-hand dominant nurse who sustained a right distal radius fracture after a fall off her bike. She is coming to you for OPOT 3- weeks after her cast was removed. She presents with: decreased wrist ROM and grip strength, pain with daily tasks (brushing teeth, combing hair, lifting items) Client goal: "Get back to work and right hand to be back to normal"
response: making decisions in real time to meet client's needs and where they are
proficient
Mrs. Jones is a 45 y/o right-hand dominant nurse who sustained a right distal radius fracture after a fall off her bike. She is coming to you for OPOT 3- weeks after her cast was removed. She presents with: decreased wrist ROM and grip strength, pain with daily tasks (brushing teeth, combing hair, lifting items) Client goal: "Get back to work and right hand to be back to normal"
response: intuitive, understanding the goal for that day isn't what should take priority in that moment
expert
types of clinical reasoning (how we make these decisions)
- ethical
- narrative
- pragmatic
- diagnostic
- interactive
- procedural/scientific
- conditional
scientific reasoning: Use of applied logical and scientific methods
- Hypothesis testing
- Theory-based decision making
What is looks like
- Impersonal and focused on diagnosis, condition
- What "typically" happens with "clients like this"
- novice
- gives you comprehensive guide to follow
diagnostic reasoning: - Investigative reasoning and analysis of cause or nature of conditions
what it looks like: Uses both personal and impersonal information to explain WHY the client is having difficulty
advanced beginner
procedural reasoning: What activities can be used to help with the functional issue
What it looks like: Use of activities which are typically helpful with a specific condition (diagnosis driven)
novice and or expert
narrative reasoning: what is the clients story
what it looks like: Understanding past, present, and future with consideration of cultural factors
competent
pragmatic reasoning: Practical reasoning based on external factors (e.g. environment, insurance) and personal situation of therapist
what it looks like: Focus on what the therapist is able to do for the patient based on external circumstances (e.g. scheduling, equipment availability
proficient
what is the main difference between a COTA and a OT
selecting outcome measures to assist with determining how progress will be measured toward goals of treatment
intervention
- Created by information from the evaluation process
- Guided by theoretical principles
- Consideration of intervention types
- Consideration of intervention approaches
intervention process
- intervention plan
- intervention implementation
- intervention review
intervention plan
- selection of objective and measurable occupation based goals and related time frames
- choose appropriate intervention approach/approaches
methods for service delivery
- consideration of potential discharge needs and plan
- recommendations/referrals to other professionals as needed
consideration of potential discharge needs and plan
- collective influences of contexts
- occupation and activity demands
- what do we see in terms of performance patterns and skills
- understanding what context of service delivery is being used
intervention types
- occupations and activities
- interventions to support occupations
- education and training
- advocacy
- group interventions
- virtual intervention
occupations and activities
- Occupations and activities selected as interventions for specific clients
- designed to meet therapeutic goals and address the underlying needs of the client's mind, body, and spirit.
- the practitioner considers activity demands and client factors in relation to the client's therapeutic goals and contexts
intervention to support occupations
- Methods/tasks that prepare the client for occupational performance used as part of a treatment session in preparation for or concurrently with occupations and activities or provided to a client as a home based engagement to support daily occupational performance
- ex: PAM, electrical stim, ultrasound, orthotics/prosthetics
education and training
- education: imparting knowledge or information about occupation, health, well being, and participation
- training: facilitation of concrete skills to meet specific goals in real life
advocacy
promoting occupational justice and empowering clients to seek and obtain resources to support health, well-being, and occupational participation.
group intervention
Use of distinct knowledge of the dynamics of group and social interaction and leadership techniques to facilitate learning and skill acquisition across the lifespan. Groups are used as a method of service delivery
virtual intervention
Use of simulated, real-time, and near-time technologies for service delivery absent of physical contact, such as telehealth or mHealth
approaches to intervention
- create, promote
- establish, restore
- maintain
- modify (compensation/adaptation)
- prevent
create, promote
- enhances performance for ALL individuals
- does not assume a disability is present or that any aspect would interfere with performance
establish, restore
- establish new skill or restore skill that had been inhibited
- designed to change client variables to establish a skill or ability that has not yet developed or to restore a skill or ability that has been impaired
maintain
- preserve their functional ability to maintain quality of life
- provide supports that will allow clients to preserve the performance capabilities that they have regained and that continue to meet their occupational needs
- The assumption is that without continued maintenance intervention, performance would decrease
modify
- revising current context of activity demand to support performance in a natural environment
- finding ways to revise the current context or activity demands to support performance in the natural setting
` compensatory techniques
` enhancing or reducing features
prevent
- for people with or without disability at risk for problems with occupational performance
- s designed to prevent the occurrence or evolution of barriers to performance in context
Intervention implementation
- select and carry out intervention(s)
- monitor response to intervention(s)
` wincing
` asking what the pain levels are for the day
` see how well or not client is progressing in therapy
intervention review, questions to consider
- are the interventions effective
- is this service delivery effective
- is there progression towards desired goals/outcome
what to consider in the intervention review
the feasibility of the plan and how interventions are implemented to achieve desired outcomes