L2: Airway resistance, pulmonary circulation, fluid movement
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
Resistance within the respiratory system
change in pressure per unit flow
in cmH2O per litre per second
Resistance of respiratory system comes from a combination of factors
Main one→ resistance from air flow friction
Airway resistance (R)
the force that impedes airflow along the respiratory passages
Airway resistance is primarily affected by
airway diameter→ (resistance greater in narrower airways)
If there is turbulent or laminar air flow
resistance greater with turbulent flow
Type of flow in respiratory tres
Turbulent air flow
Laminar air flow
Transitional flow
Turbulent air flow
WHERE occurs in the large airways
trachea and the large bronchi→ especially at high flow rates
WHAT air flows in disorganised patterns
sounds that can be heard when breathing deeply
under stethoscope during normal respiration
Laminar flow
WHAT streamlined flow of air that runs parallel to the sides of the airways
silent
WHERE: small airways
where flow is very slow
Transitional flow
WHAT: mix between the two
WHERE: mostly in lower airways of the lung
where conditions for true laminar flow (essentially flow through long straight tubes) are not met
How does turbulent flow affect resistance?
creates greater resistance to flow
Airway diameter:
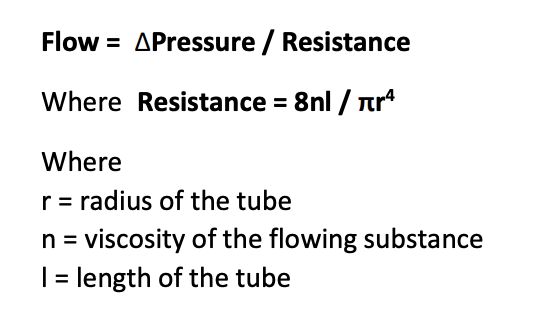
Importance of the tube diameter to resistance:
Small reductions in radius→
dramatically increase the resistance
→ reduce flow
(unless grater work is applied to generate a steeper pressure gradient)
Under normal respiratory conditions…
air flows through the respiratory passageways easily
as little as 1 cmH2O pressure gradient is sufficient for eupnea
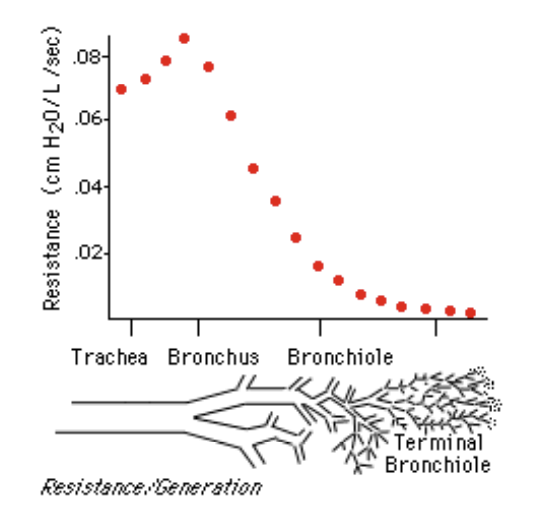
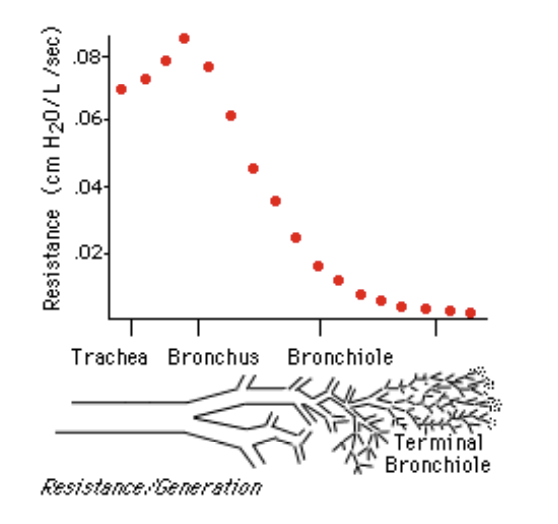
Where is the greatest resistance to air flow?
Upper respiratory tract:
although the airways are larger there are fewer of them
Why is this counterintuitive
Tiny bronchioles have smaller individual diameter
but so many of them→ tiny amounts of air must flow through each
→ resistance is low
Dynamic control of Airway Resistance: how can bronchioles be dynamic
have muscular walls
contract to restrict air→ flow regionally or across the whole lung
Why is it useful that they are so small?
so narrow so small changes in diameter or accumulation of mucus
within them→ can have dramatic effects on air flow through the lung
Dynamic effects of the lungs
Regional bronchiole constriction:
help maintain a normal ventilation:perfusion ratio
WHEN:constriction occurs in regions of poor perfusion
Dilation of bronchioles:
WHEN: response to sympathetic stimulation
Sympathetic innervation→ only modest
Sympathetic stimulation by circulating adrenaline and noradrenaline→ stimulate beta-adrenergic receptors cause marked dilation of the bronchial tree
Constriction of bronchioles
WHEN: in response to parasympathetic stimulation by the vagus nerve
ALSO: stimulated by local reflexes→ triggered by noxious stimuli
gases or infection
Histamine release by mast cells
or as part of systemic allergic reaction
→ causes bronchoconstriction
Asthma
abnormal degrees of airway narrowing
seen in allergic airway diseases
Inflammation→ causes swelling around the airways
Mucus→ accumulation in the airways
OVERALL: Narrowing the airways
Airways Hyper-reactive
prone to bronchoconstriction when exposed to minor insults like cold air
What is bronchoconstriction perpetuated by
histamine release from mast cells
involved in allergy
Dynamic pressure changes also affect airway resistance
on top of pressure-volume changes during the respiraotry cycle
in terms of the lung parenchyma and alveolar expansion
BUT also airways also experience pressure changes
The diameter of airways with lung volume changes:
the lungs expand the connective tissues
this suspends the airways within the lung parenchyma pull outwards and expand the airway diameter
What happens at respiration at rest (eupnoea)
Alveolar pressures fluctuate from -2 to +2 cmH2O at most
Pleural pressures are always negative
Tend to hold alveoli and airways within the thoracic cavity open
Airway collapse during expiration: what happens during forced expiration
intrathoracic pressures become large and position
→ with important implications
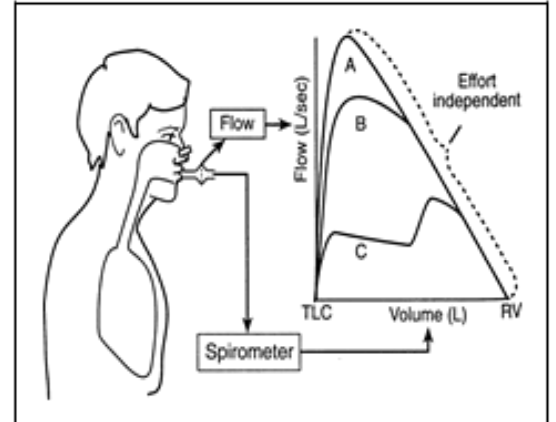
Forced expiration
see a trace when a patient inspires to total lung capacity
then maximally exhales as far as possible→ to residual volume
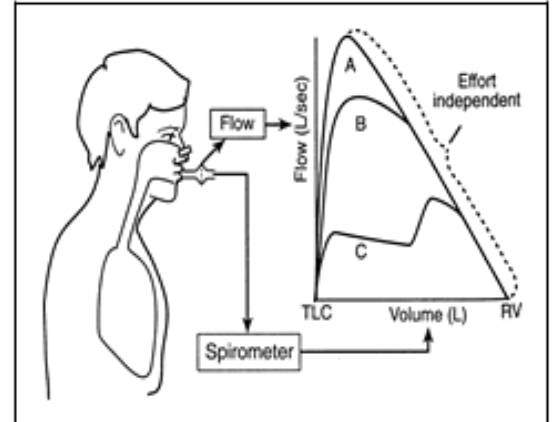
Break down of what happens
A→ subject exhales as fast as they can
B→ exhales more slowly
C→ exhale slowly to begin→ then maximally (at the inflection point)
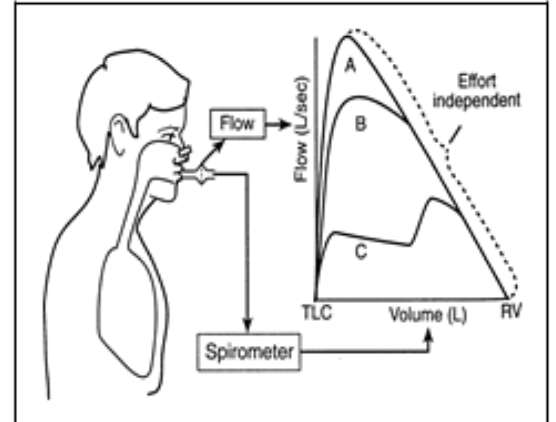
Result of this
Peak flow depends on the force of expiration
BUT
below a given volume, the rate of flow drops and is effort independent
→ However hard you try: it is impossible to increase flow
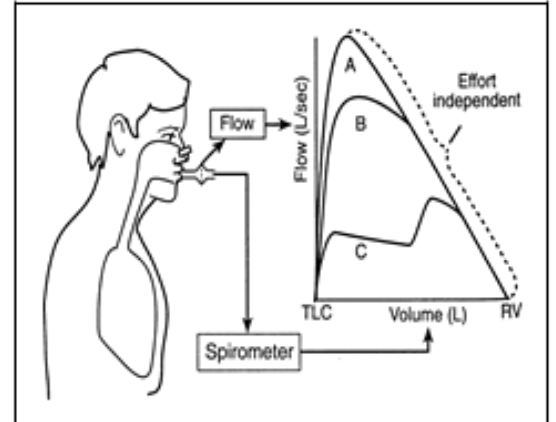
The reason for this?
below a given volume, the pressures within the thorax are such that small airways collapse
→ reducing the maximal rate of flow
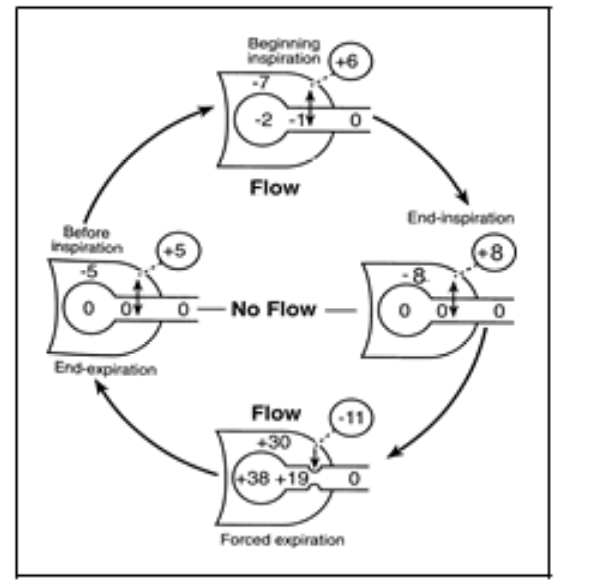
Just as there is transmural pressure on the alveolus→ (intra-alveolar pressure-pleural pressure)
… there is a trans-airway pressure (airway pressure-pleural pressure)
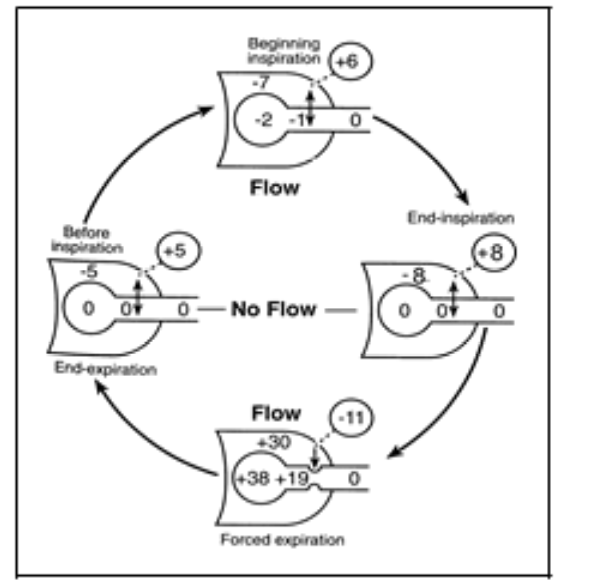
Pressures during different parts of the cycle
During inspiration→ large negative pleural pressure tends to keep airway open
trans-airway pressure large and positive
At end of inspiration→ pressure within the airway and alveolous equilibrates with atmospheric pressure
and the trans airway pressure remain large and positive
During forced expiration→ pleural pressure can be very large and positive
elastic recoil of the lung parenchyma ensures that the alveolar pressure are even more positive
so trans airway pressure remains large and positive
However, as you get further from the alveolus→
the lower the airway pressure is
WHY: airway resistance means the airway pressure reduces gradually along the distance from alveolus to mouth
Due to the decrease in airway pressure…
at some point up the respiratory tree→ the trans-airway pressure (=airway pressure- pleural pressure) will become zero
→ This is Equal pressure point EPP
Beyond this point…
Becomes negative:
The force tending to collapse the airway
What happens when the equal pressure point EPP lies within the airways supported by cartilage?
→ no collapse will occur
But what happens when the equal pressure point EPP lies within the unsupported bronchioles
→ collapse will occur
Due to this narrowed or sompletely collapsed airway…
Resistance:
high
Outward air flow:
stopped or limited
Even in healthy lungs, during forced expiration…
some airways collapse
→ underlies the observation that even if you really try→ still limit to peak expiratory flow
Dynamic airway collapse is only influential during…
forced expiration
where pleural pressures get very high and positive
BUT: some lung pathologies can lead to problematic air trapping due to airway collapse
In conditions with high lung compliance (emphysema)
Elastic recoil of the alveoli is not great:
Even if transmural pressure is positive to keep alveoli open
→ airway pressures will also be lower
→ equal pressure point moves lower in the respiratory tree
How low can the EPP move to
can move so low that airway collapse occurs even during ‘normal’ breathing for that patient
→ leads to:
air trapping
positive pressure within the alveoli at the start of the next inspiration
and lung hyperinflation
What do emphysema patients learn to do to reduce the slope of pressure gradients between alveoli and the outside
learn to breathe out through pursed lips
OVERALL: preventing airway collapse by moving the EPP towards the mouth
What happens in conditions with increased airway resistance (asthma)
pressure within the airways dissipates more rapidly
→ leading:
to the EPP moving lower in the respiratory tree
having the potential to cause airway trapping
Extra-thoracic airway collapse during inspiration: What happens during rapid inspiration
negative pressure within the airways tends to suck soft tissues towards the midline→ obstructing air flow
Problems caused:
where structural or functional integrity is lost for some reason
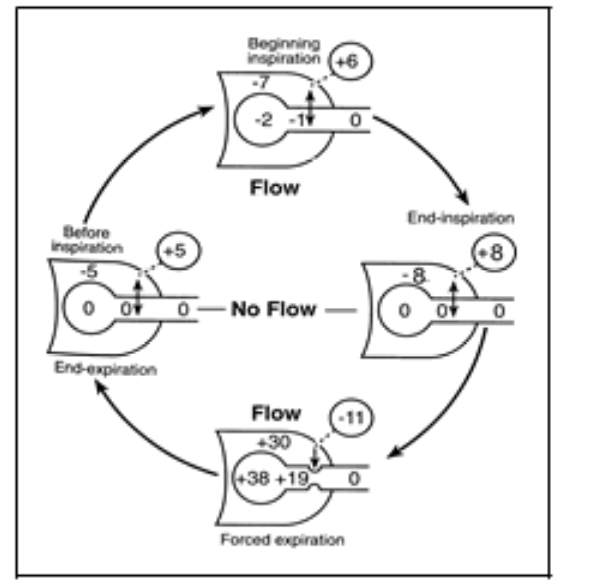
The pulmonary circulation: the two distinct circulations of the lungs
Bronchial circulation
Pulmonary circulation
Bronchial circulation
received <2% of left side cardiac output
high pressure, low flow system
fed by bronchial arteries delivering oxygenated blood to the conducting airways
supporting structures of the lungs
majority is drained into pulmonary circulation
causing a small drop in PO2 between blood leaving the alveoli full oxygenated and entering the left side of the heart
Coz of the venous admixture of deoxygenated blood from the bronchial circulation
Pulmonary circulation: pulmonary artery
receives blood from the right ventricle
arterial branches carry blood to the alveolar capillaries for gas exchange
pulmonary veins return the blood to the left atrium
to be pumped by the left ventricle through the systemic circulation
→ OVERALL: low-pressure high flow system
Pulmonary circulation: capillary bed MAIN FUNCTION
places the blood in intimate contact with the alveoli
to facilitate rapid gas diffusion
Pulmonary circulation: capillary bed SECONDARY FUNCTIONS: blood reservoir
Blood reservoir→ 40% of weight is blood (approx 500m or 10% blood volume in human)
Pulmonary circulation: capillary bed SECONDARY FUNCTIONS: Filters the blood of emboli
eg: clots, fat globules or air
would otherwise enter systemic circulation and blood blood flow to critical organs
Emboli are trapped in small pulmonary arterioles and capillaries
→ pulmonary endothelial cells release fibrinolytic agents→ dissolve clots
Air emboli can be harmlessly absorbed
issue with large emboli?
can block blood flow to significant areas for the lung
→ cause serious clinical signs and many small emboli
many small emboli can also significantly compromise lung function
infectious emboli can set up pulmonary abscesses
Pulmonary circulation: capillary bed SECONDARY FUNCTIONS: metabolises vasoactive hormones
e.g Angiotensin I
converted to angiotensin II→ by angiotensin converting enzyme
located on the cell surface of the pulmonary endothelial cells
With 80% of Ang I converted to Ang II
during a single pass through the pulmonary vasculature
Many other vasoactive hormones are metabolised in the lungs too
Pulmonary circulation: Lymphatics
vessels present in all supportive strucutres of the lung
mainly drain into the right thoracic lymph duct
Pulmonary circulation: Lymphatics→ particulate matter
gets as far as the alveoli
partly removed in the lymph
→ as plasma protein which may leak from lung capillaries
Which might otherwise exert osmotic pressure within the alveoli or interstitium
Differences between pulmonary and systemic circulations
Pul: carries entire output of the right side of the heart
syst: divided between different organs
Pul: blood enters the circulation deoxygenated and returns to the heart oxygenated
syst: opposite is true of the systemic circulation
Pul: driving pressure and mean capillary pressure in pulmonary circulation is much lower than the systemic circulation
Pul: resistance is low compared to systemic
pul: vessels compliant
syst: vessels much less compliant
→ coz there is less muscle in the walls in pulmonary vs systemic arteries
Pul: vessels respond to hypoxia with vasoconstriction
systemics ones→ by vasodilation
REMEMBER THESE DIFFERENCES
Resistance to flow in pulmonary vessels is …
generally low
Cardiac output is driven through the lungs with a pressure gradient of
only approximatley 10 mmHG
in contrast:
pressure gradient for the movement of the same volume of blood in the systemic circulation is 85-90 mmHg
The resistance of the pulmonary circulation compared to the systemic vascular resistance
1/10th of the systemic vascular resistance
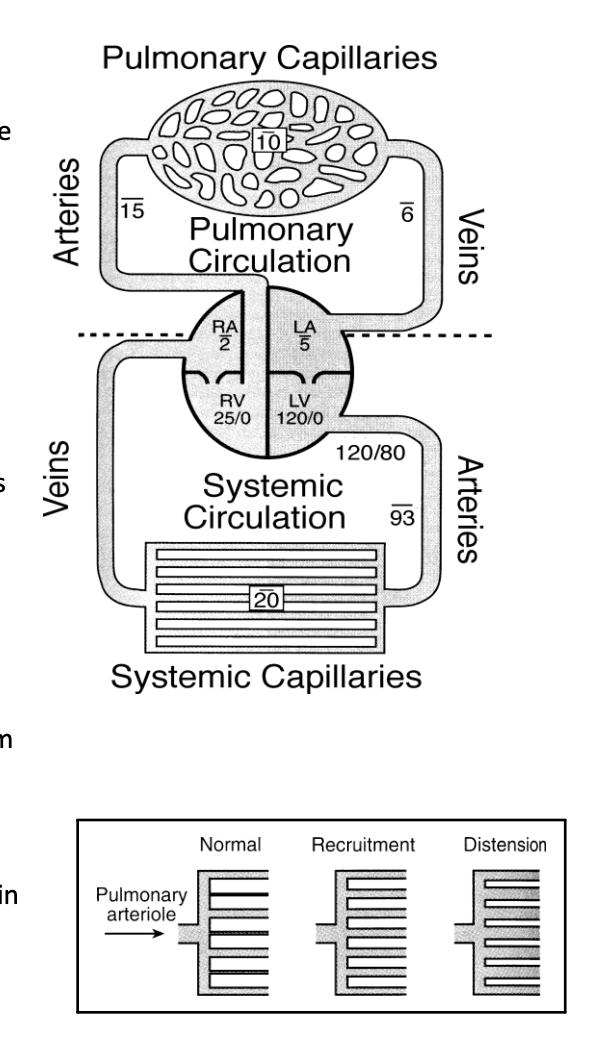
How is this achieved?
enormous number of pulmonary vessles to accommodate flow → easily dilated
when cardiac output increases (e.g during exercise)→ pressure does not increase much
why?→ highly compliant vessels dilate (distension)
this reduces resistance within them
capillaries that were previously collapsed are recruited so increasing the capacity for blood flow
During intense exercise→ pulmonary capillary pressure rise
as high as 40mmHG in humans or 100 mmHg in racehorses
→ damage the delicate alveoli and cause haemorrhage in extreme circumstances
Pulmonary vascular resistance also changes in response to hypoxia:
Pulmonary vessels: vasoconstriction
Systemics: vasodilatation
RESULT: in the lungs→ diverts blood away from poorly ventilated areas of lungs→ to better ventilated ones
THEREFORE: blood contributes more meaningfully to gas exchange
OVERALL: response is an effort to maintain optimum ventilation/perfusion ratio across the lung→ which is more shortly
Fluid exchange in the lungs: low pressure of the pulmonary vasculature also has implications for…
movement of fluid in the lungs
→ (which is susceptible to qualitatively similar but qunatitiatively different hydrostatic and osmotic pressures)
Net fluid exchange across the capillary is determined by…
difference in hydrostatic and colloid osmotic pressure across the capillary wall
Compared to the lungs…
we cannot stop at considering leakage of fluid from the capillary into the interstitium
→ ALSO potential for fluid to leak into the alveolus within the alveolus
and effect of surface tension within the alveolus
Forces tending to cause movement of fluid outward from the capillaries and into the pulmonary interstitium
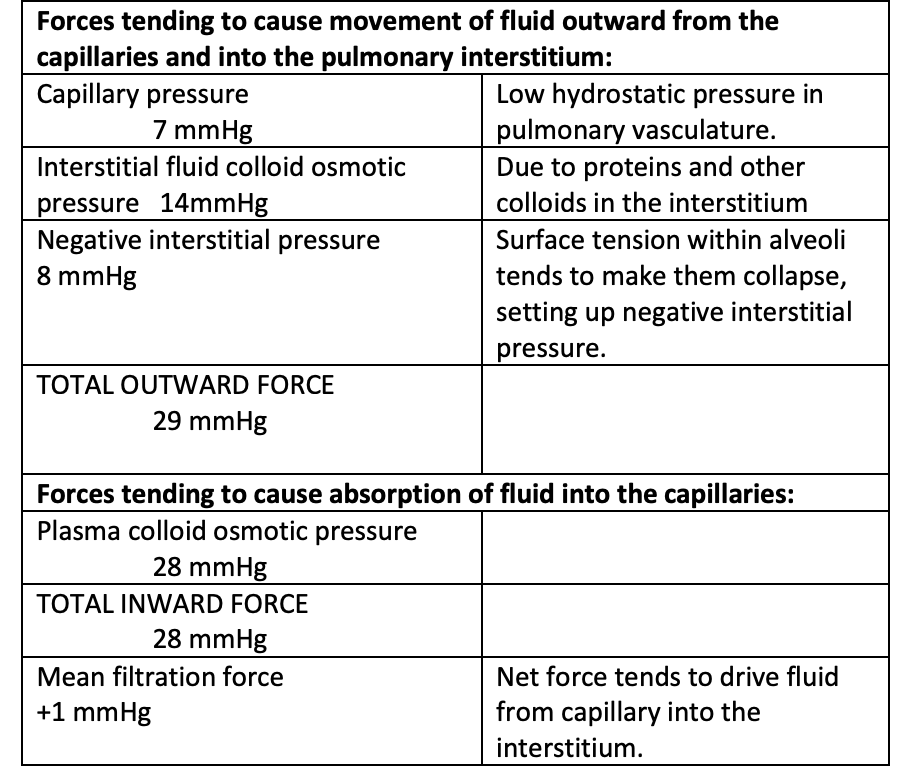
Forces tending to cause absorption of fluid into the capillaries:
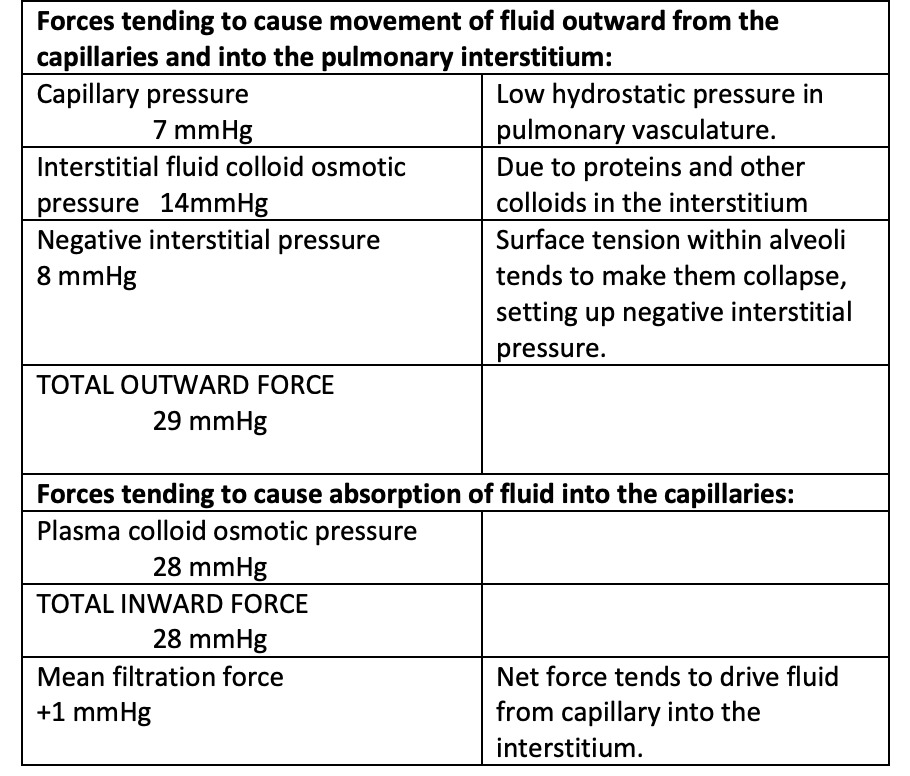
This net flow of fluid into the interstiatil space is drained…
by the lympth system
Under normal circumstances, what happens to the interstitial fluid?
does not enter the alveoli
Two factors that ensure this:
interstitial pressure is negative→ THUS pulling water away from the alveoli
Surfactant acts as a barrier to fluid movement that attempts to enter the alveoli via capillary action
However…
this is a fine balance and susceptible to disruption
If filtration of fluid exceeds removal…
oedema ensures
→ with filling of the interstitial spaces and alveoli with fluid
This can occur as a result of:
increase in pulmonary capillary pressure
(e.g left side heart failure)
increase in pulmonary permeability
(e.g inflammation, mechanical damage due to overinflation, exposure to toxic gas)
Decreased capillary colloid osmotic pressure
(e.g hypoalbuminemia in some kidney diseases or starvation)
Increase in surface tension in alveoli
(e.g lack of surfactant in premature neonates)
Failure of lymphatic drainage
(e.g inflammation of lympthatics physical obstruction)