Anatomy and histology of the Female reproductive organs
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
Internal Genitalia (Female)
Includes two ovaries, two uterine tubes, a cervix, and a vagina. Their structure and appearance change with hormonal and physiological states (age, menstrual cycle, pregnancy).
How does hormonal and physiological state affect female reproductive organs?
The organs’ structure and function vary depending on age (pre-pubertal or mature) and reproductive status (menstrual cycle stage or pregnancy).
Ovary Anatomy
Oval or almond-shaped organs located in the abdominal cavity, one on each side of the uterus.
What are the two main parts of the ovary and their functions?
Medulla: Inner part with blood vessels, connective tissue, and nerves.
Cortex: Outer part containing ovarian follicles where eggs develop.
Ovarian Follicles
Small sacs in the ovarian cortex containing eggs. Their growth leads to ovulation, releasing the egg into the uterine tube.
What is a primordial follicle?
An immature follicle with a single layer of flat follicular cells surrounding the egg, the starting stage for follicle development.
What changes occur as a primordial follicle grows into a primary follicle?
Supporting cells become cuboidal (cube-shaped), the number of cell layers increases, and the layers differentiate into theca cells (outer layer) and granulosa cells (innermost layer surrounding the egg).
Theca and Granulosa Cells
Theca cells: Form the outer follicle layer, rich in blood vessels, lymph vessels, and nerves (which do not enter granulosa layer).
Granulosa cells: Form the inner layer directly surrounding the egg.
What is the secondary follicle stage?
The follicle develops a fluid-filled space called the antrum.
Cumulus Oophorus
A stalk-like cluster of granulosa cells near the egg that supports it during follicle maturation.
What is a Graafian follicle?
The fully mature follicle ready to release the ovum during ovulation.
Corpus Luteum
A temporary endocrine structure formed from the remaining follicular cells after ovulation; it secretes progesterone to support the uterine lining.

Uterine Tube (Fallopian Tube/Oviduct)
A tube connecting the ovary to the uterus, composed of three segments, which transports the ovum and is the site of fertilization.
What is the first segment of the uterine tube and its function?
The infundibulum, a funnel-shaped opening near the ovary that captures the ovum after ovulation.

Fimbriae
Finger-like projections surrounding the ovary that help guide the released ovum into the uterine tube by moving closer to the ovary after ovulation.
How does the uterine tube align with the ovary during ovulation?
Blood vessels in the uterine tube become engorged (welling with blood), increasing firmness and helping the tube align with the ovary.
Ampulla
The widest portion of the uterine tube and the primary site where fertilization occurs.

Isthmus
The narrow segment of the uterine tube connecting the ampulla to the uterus.
Layers of the Uterine Tube Wall
The uterine tube wall consists of three layers:
Mucosa (innermost lining the lumen)
Muscularis (two layers of smooth muscle)
Serosa (outer visceral peritoneum)
What is the function of the mucosal folds in the uterine tube, especially in the ampulla?
They slow down the movement of the ovum, increasing the chance of fertilization at the ampullary-isthmic junction.
Mucosal Epithelium Cell Types
Two types of columnar cells line the mucosa:
Ciliated cells (with kinocilia) that move the ovum toward the uterus
Non-ciliated secretory cells with microvilli that produce nutritive and protective fluid
How do ciliated cells in the uterine tube respond to hormones?
Their numbers increase near ovulation in response to estrogen, enhancing ovum transport.
Role of the Secretory Fluid in the Uterine Tube
Produced by non-ciliated cells, this viscous fluid helps transport ova and sperm, nourishes the early embryo, and protects sperm and embryos from maternal immune attack.
What drives the increased blood supply and secretory activity in the uterine tube during ovulation?
Ovarian estrogens stimulate the blood supply increase and the enhanced secretory activity of the mucosa.
Muscularis Layer of the Uterine Tube
Composed of two smooth muscle layers: an inner circular layer and an outer longitudinal layer.
How do the muscularis contractions assist ovum transport and protect the peritoneal cavity?
Peristaltic contractions combined with cilia movement push the ovum toward the uterus and prevent microbes from ascending to the peritoneal cavity.
Function of the Serosa Layer in the Uterine Tube
The outermost layer that lubricates the uterine tube, preventing adhesions and allowing free movement within the abdominal cavity.
What is an ectopic pregnancy, and where does it most commonly occur?
An ectopic pregnancy is when a fertilized egg implants outside the uterus, most commonly in the uterine (fallopian) tube or abdominal/pelvic cavity; it is non-viable.
The lamina propria reacts by forming cells similar to those in the uterine endometrium, resembling early placental cells despite abnormal implantation.
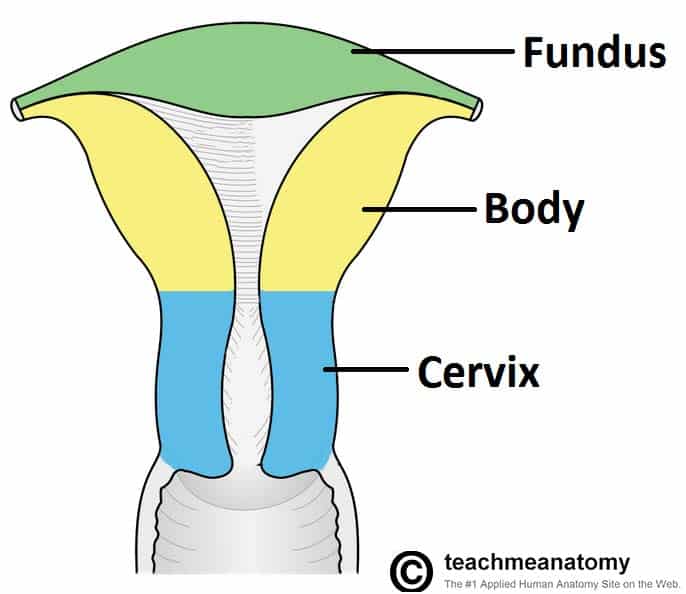
Human Uterus Structure
Pear-shaped organ divided into three main parts: fundus (top), body (largest central part), and cervix (lower narrow part connecting to vagina).
How does the uterus of domestic animals differ from the human uterus?
Domestic animals have two uterine horns (cornua), a uterine body, and a cervix; humans have a single pear-shaped uterus with fundus, body, and cervix.
The uterine wall consists of three distinct layers
Perimetrium
Myometrium
Endometrium
Perimetrium
The outermost uterine layer; a serosal covering continuous with the broad ligament that anchors the uterus in the pelvic cavity.
Myometrium
Thick middle layer made of smooth muscle fibers arranged spirally, longitudinally, and circularly; thickest at fundus and uterine horns (contracts during labor), thinnest at cervix (softens and dilates during birth).
Endometrium
Inner mucosal layer of the uterus that proliferates to prepare for embryo implantation; sheds during menstruation if fertilization does not occur; contains branched glands that nourish the early embryo.
endometrial glands secrete nutrients to nourish the early embryo before placenta formation
Cervix Structure
Mainly connective tissue with some smooth muscle, thick wall, and narrow lumen; usually closed except near ovulation, menstruation, and childbirth.
When does the cervix open or relax?
Around ovulation to allow sperm entry, during menstruation for discharge, and during parturition (birth canal opening).
Cervical Discharge
Mucosal secretions from the cervix that can fill the cervical lumen and be expelled through the vagina; varies with the reproductive cycle.
Vagina Function
Serves as the copulatory organ and birth canal; also provides a passage for menstrual flow in primates.
Vagina Anatomy
Extends from cervix to vestibule; lined with mucous membrane; has thick, flexible transverse folds called vaginal rugae.
What are vaginal rugae and their functions?
Transverse folds that allow stretching during intercourse and childbirth, and create friction ridges that stimulate the glans of the penis during copulation.
Where is most of the acidic mucus in the vagina produced?
Most acidic mucus is produced by the uterine glands, not the vaginal mucosa itself.
What is the function of the acidic vaginal environment?
The low pH slows bacterial growth and protects against infection, but it can also be hostile to sperm.
Semen (pH 7.5) neutralizes vaginal acidity, enabling sperm survival and mobility.
The female external genitalia are collectively known as the vulva and include:
Vestibule (area into which the urethra nf vagin open)
Labia majora
Labia minora
Clitorus
What structures open into the vestibule?
The urethra and vagina open into the vestibule, which is a longitudinal cleft surrounded by the labia majora.
Suburethral Diverticulum
A small blind-ending sac located just in front of the urethra, opening into the vestibule.
/sc-assets/prd/practices/177ad831-d3bb-4400-956b-46c3eb9759d3/VgYUkpPvnJWa4XMVE9KYmUeZnqokXYcNGRapWZqy2u8FpoQ-QIyGM_HrORTLVwLCWxEUgT_D4O74rmRyOdtP9CSu3zBldMo.jpeg)
What are the Bartholin glands and their function?
Also called vestibular glands, they open into the vestibule and secrete viscous fluid, especially near ovulation, to aid lubrication during sex.
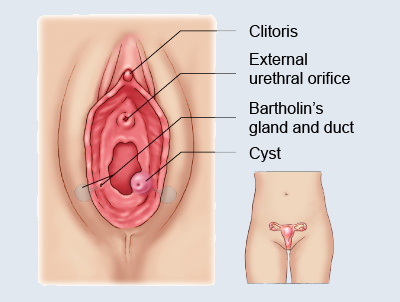
What tissue does the clitoris originate from, and what is it made of?
The clitoris originates from the same embryonic tissue as the penis and is made of erectile tissue with a highly sensitive glans.
Stimulation of the glans clitoris can result in orgasm, similar to the glans penis in males.
Labia Majora
Thick, elongated folds of skin containing fat and smooth muscle, derived from the same tissue as the scrotum. They protect the vulva and meet at the perineum.
They are separated by the pudendal cleft and meet at the perineum (area between the vulva and anus).

Labia Minora
Thin, inner folds located within the labia majora, they shield the vaginal orifice and are highly sensitive due to rich nerve supply.
