Exam 2 General Info
1/212
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
213 Terms
Besides BPPV, what is another cause of recurrent vertigo?
Meniere's disease
Does Meniere's disease have central or peripheral vertigo characteristics?
peripheral
Vertigo attacks last longer in which condition: BPPV or Ménière's disease?
Meniere's disease
(1-24 hours vs. seconds)
True or false: Ménière's disease has a predictable onset similar to BPPV.
false
(more spontaneous)
What is the triad of symptoms present in Ménière's disease?
1. vertigo
2. tinnitus
3. unilateral hearing loss
(different from BPPV, which is not associated with any auditory symptoms)
How does vestibular neuritis differ from BPPV and Ménière's disease?
single acute episode of vertigo rather than recurrent, and lasts much longer (hours to days)
Because Ménière's disease is caused by too much fluid in the cochlea, how is it commonly treated?
salt restriction + diuretics
Does vestibular neuritis have central or peripheral vertigo characteristics?
peripheral
BPPV does not have auditory symptoms, and Ménière's disease does have tinnitus and hearing loss. What about vestibular neuritis?
usually none
**if hearing loss is present, then it would be called vestibular labyrinthitis
What are 4 red flags of dizziness & vertigo that warrant an urgent ENT referral?
1. neurological symptoms or signs
2. acute deafness
3. new type/onset headache
4. vertical nystagmus
Which causes of vertigo are much more unremitting and disabling: peripheral or central?
central
causes include: vascular strokes, tumors, MS, migraines, and certain drugs (e.g., sedatives, anti-seizure meds)
What are 3 main causes of central vertigo?
1. brainstem infarction
2. vestibular migraine
3. vertebrobasilar TIA
True or false: Central vertigo is usually associated with auditory symptoms.
false
(EXCEPT: anterior inferior cerebellar artery syndrome)
Other than the vertigo, how are the symptoms of brainstem infarction, vestibular migraine, and vertebrobasilar TIA different from those of BPPV, Ménière's disease, and vestibular neuritis?
other neurological symptoms (e.g., headache) are present
Do brainstem infarction, vestibular migraine, and vertebrobasilar TIA have central or peripheral vertigo characteristics?
central
Other than vertigo, what are 3 other forms of dizziness that a patient may experience?
1. presyncope
2. disequilibrium
3. lightheadedness
refers to ear pain
otalgia
If your patient comes in with otitis externa ("swimmer's ear"), what 3 signs/symptoms are they most likely experiencing?
pain, pruritus, discharge
Otitis externa is just swimmer's ear and presents with pain, pruritus, and discharge. However, malignant otitis externa has these symptoms + what else?
CNS signs (e.g., CN palsies, esp. CN VII)
**treated with 6-8 week course of antibiotics
What cranial nerve palsy is most likely with malignant otitis externa?
CN VII palsy
What is the main potential complication of malignant otitis externa that we are concerned about?
osteomyelitis of skull base or TMJ
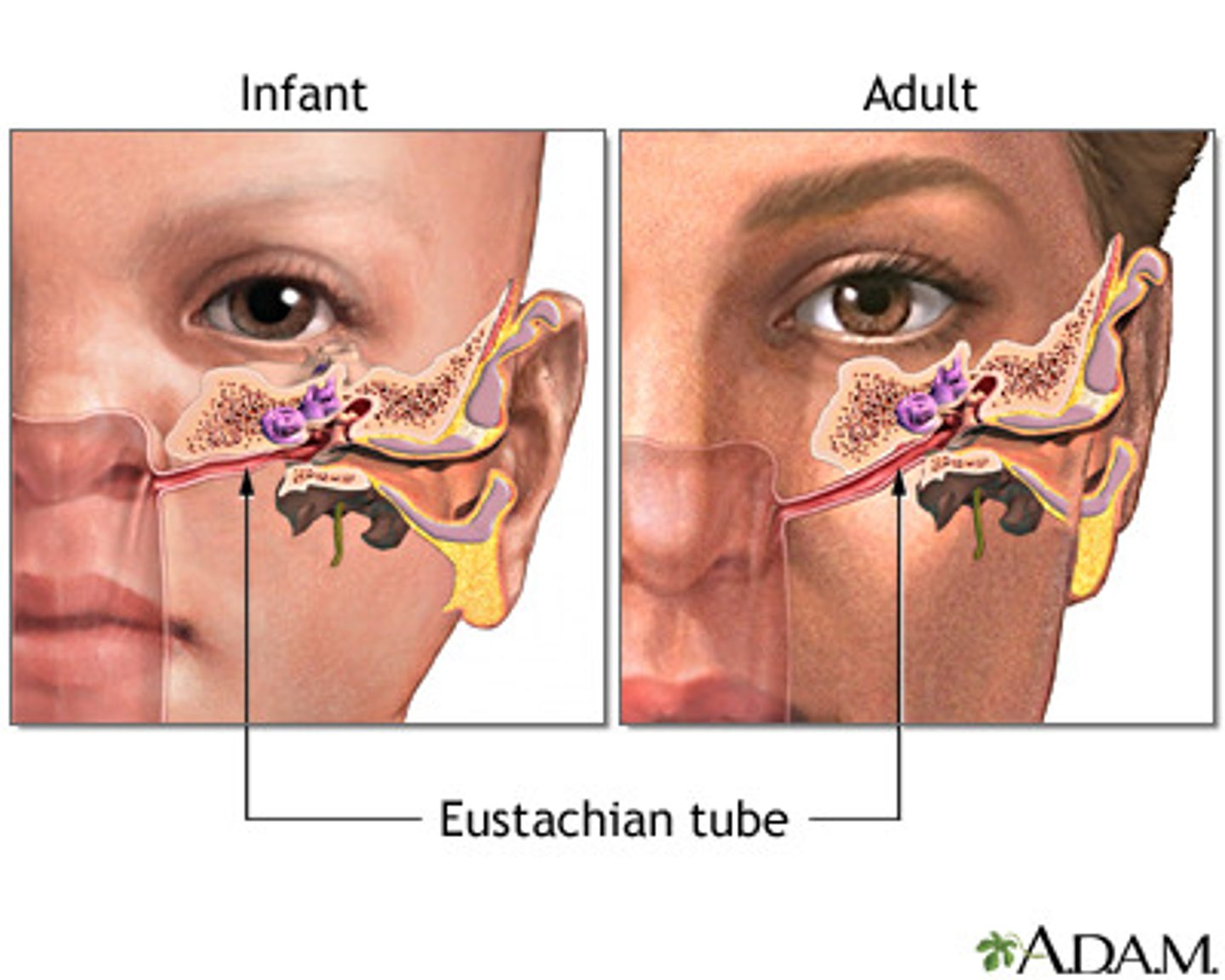
Why is it not uncommon for kids to get an ear infection (i.e., middle ear otalgia) right after a cold?
their eustachian tubes are more horizontal, so it's easier for the infection to spread
True or false: Antibiotics should be used initially to treat serous otitis media.
false
**this is usually a viral cause, but if it doesn't resolve, then it could progress to bacterial and then we'd used antibiotics or drain the abscesses
Sometimes, a patient's ear pain actually indicates that the pain is referred from somewhere else. Persistent ear pain should thus be referred out to exclude what serious cause?
upper airway tumor
refers to nose bleeds
epistaxis
Anterior epistaxis can occur from what 4 most common causes?
1. trauma
2. rhinitis
3. mucosal dryness
4. blood thinners (e.g., aspirin, warfarin)
How should a patient be positioned to help a nosebleed resolve faster?
sitting with their head bent forward
**this reduces venous pressure and diminishes the risk of aspiration
Anterior epistaxis is common, but posterior epistaxis is more severe since this bleeding occurs from an artery. Bleeding of what 2 arteries most commonly leads to posterior epistaxis?
internal maxillary or ethmoidal artery
Is nasal congestion present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
both
Is sneezing present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
both
Is watery discharge present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
both
Is sore throat present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
viral
Is malaise present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
viral
Is eye tearing/itching present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
allergic
Are nasal polyps present in viral rhinitis (common cold) or allergic rhinitis (hay fever)?
allergic
In which type of rhinitis is the nasal mucosa red (erythematous): viral or allergic?
viral
In which type of rhinitis is the nasal mucosa pale and purple (violaceous): viral or allergic?
allergic
If nasal discharge is serous, then we usually just treat viral rhinitis with phenylephrine nasal spray for 3 days as a decongestant. However, at what point would we treat with antibiotics?
if nasal discharge becomes purulent ("boogers are cloudy")
Allergic rhinitis is mediated by what immunoglobulin?
IgE
How do we usually treat allergic rhinitis/hay fever?
oral antihistamines or topical steroids
True or false: Routine sinus imaging is often warranted in allergic rhinitis.
false
True or false: Leukotriene receptor antagonists are often used as primary therapy in allergic rhinitis.
false
rebound nasal congestion that occurs as a result of prolonged use of nasal decongestants
only recourse is to stop use and anticipate a period of further worsening of symptoms, which may respond to nasal steroids
rhinitis medicamentosa
fungal infection mimicking bacterial sinusitis, usually occurring in an immunocompromised host (e.g., with diabetes, renal disease, recent transplant)
characterized by black necrotic nasal tissue, has high mortality rate and requires immediate anti-fungal therapy and likely surgical debridement
rhinocerebral mucormycosis

What are the 3 components of the airway inflammatory syndrome Samter's triad, sometimes seen in patients with allergic rhinitis?
1. nasal polyps
2. asthma
3. aspirin sensitivity
If a patient has nasal polyps and asthma, what medication should they probably avoid?
aspirin
If nasal polyps are present in kids, what condition should be considered?
cystic fibrosis
Hoarseness is primarily a symptom of what kind of disease?
laryngeal
A red flag of acute laryngitis is what high-pitched sound when breathing in?
stridor
A red flag of acute laryngitis is what 2 recent medical procedures pertaining to the neck?
neck surgery or radiotherapy
A red flag of acute laryngitis is a history of what?
smoking
A red flag of acute laryngitis is what 3 professions?
singer, actor, teacher
**basically just some kind of professional that relies on speaking often and loudly
A red flag of acute laryngitis is what body change?
weight loss
A red flag of acute laryngitis is what 2 swallowing signs?
dysphagia or odynophagia
A red flag of acute laryngitis is what ear symptom?
otalgia
GERD and laryngopharyngeal reflux (LPR) are both inflammatory etiologies of hoarseness. How can these 2 conditions be distinguished?
GERD frequently presents with heartburn and very rarely throat clearing
LPR doesn't usually present with heartburn but throat clearing is common
In addition to inflammatory etiologies, hoarseness may also have a neoplastic cause. It could just be benign nodules, but it could also be laryngeal leukoplakia, which puts patients at significant risk for what more serious condition?
squamous cell carcinoma (SCCA)
A patient is seen for hoarseness and comes back over 3 weeks later and says the hoarseness still hasn't gone away. At this point, they should be referred for what kind of evaluation?
cancer (e.g., HPV in younger patients)
True or false: Stridor is a medical emergency and should be treated as such.
true
**need to maintain airway via intubation or emergent tracheostomy and monitor closely
A patient comes in complaining of sore throat, hoarseness, difficulty swallowing, and unilateral ear pain. Upon examination, you notice a lump in their neck, and you can hear a high-pitched wheezing sound on each breath the patient takes in. At this point, you are highly suspicious of what condition?
head/neck cancer
Your patient comes in with a cranial nerve palsy and orbital mass. Remembering what Dr. Gurka taught you, you refer them to an ENT specialist. When reading the record, you find that the patient also had red/white oral lesions and ulcerations, a lateral neck mass, a thyroid mass, and unilateral ear effusion. The patient will be further evaluated, but what is the most likely condition?
head/neck cancer
thickened, white, leathery-looking spots on the inside of the mouth that are non-removable and may be an early sign of SCCA
leukoplakia
What medical procedure is necessary to make a possible diagnosis of SCCA based on white oral lesions?
biopsy
**early diagnosis of SCCA is critical to successful therapy
What is another form of white oral lesions besides leukoplakia due to SCCA?
candidiasis (oral thrush)
Which comes off the tongue: leukoplakia patches or oral thrush?
oral thrush
Similar to leukoplakia, a patient can also have erythroplakia: red oral lesions. Which are more often malignant: red or white lesions?
red lesions
**these warrant an immediate biopsy since 90% are dysplastic or early SCCA!
What is the main function of RBCs?
transport oxygen
refers to the presence of small RBCs on a blood smear
microcytosis
refers to the presence of large RBCs on a blood smear
macrocytosis
refers to the presence of RBCs of variable size on a blood smear
anisocytosis
refers to the presence of RBCs of variable shape on a blood smear
poikilocytosis
refers to RBCs with reduced color on a blood smear
hypochromia
refers to spherical RBCs seen on a blood smear
spherocytosis
What is the main function of platelets?
clot formation
What is considered a normal platelet count?
150-450k/µL
Anemia associated with renal failure results in low levels of what hormone?
erythropoietin
Deficiency of what vitamin can lead to anemia?
vitamin B12
excessive amount of red blood cells
erythrocytosis (polycythemia)
excessive amount of platelets
thrombocytosis
excessive amount of white blood cells
leukocytosis
Neutrophilia is common in what conditions?
infections (especially bacterial), stress, drugs (steroids)
Lymphocytosis is common in what what conditions?
viral infections
Eosinophilia is common in what conditions?
allergies, asthma, parasitic infections
What condition is characterized by low hemoglobin & hematocrit?
anemia
Blood loss, hemolysis, and marrow suppression all result in what type of anemia?
A. microcytic
B. macrocytic
C. normocytic
C
type of anemia resulting from reduced RBC survival
bone marrow compensates by increasing production 8-fold, but anemia results when this capacity is outstripped by excessive destruction or impaired marrow function
lab features:
--abnormal peripheral smears
--reticulocytosis
--elevated indirect bilirubin
--hemoglobinuria
hemolytic anemia
Is haptoglobin increased or decreased in hemolytic (e.g., sickle cell) anemia?
decreased
Are liver enzymes like LDH and SGOT/AST increased or decreased in hemolytic (e.g., sickle cell) anemia?
increased
Iron deficiency, thalassemias, and sickle cell disease all result in what type of anemia?
A. microcytic
B. macrocytic
C. normocytic
A
What is the gold standard for diagnosis of iron deficiency anemia?
bone marrow biopsy
**absent iron stores are pathognomonic for this type of anemia
What is the most common route of chronic slow blood loss, leading to iron deficiency anemia?
GI bleeding
other causes: heavy menstruation; repeated frequent blood donations; iron deficient diet
Vitamin B12 deficiency, liver disease, and hypothyroidism all result in what type of anemia?
A. microcytic
B. macrocytic
C. normocytic
B
Anemia commonly results from intrinsic RBC defects, such as what X-linked genetic condition characterized by episodic hemolysis due to infections or oxidant drugs?
glucose 6-phosphate dehydrogenase (G6PD) deficiency
Sickle cell anemia is an inherited hemoglobinopathy caused by a point mutation leading to what amino acid substitution?
Glu → Val
True or false: Fetal hemoglobin is vulnerable to sickle cell disease.
false
**sickling is normally reversible with oxygenation but is also impaired by the presence of fetal hemoglobin
Cell sickling present in sickle cell disease can cause damage to what organ, causing it to be non-functional?
spleen
Sickle cell disease can result in what GI complication?
gallstones
other complications: vascular occlusion, bones and lungs affected, strokes, priapism
True or false: Sickle cell anemia is a multiple-organ disease and can have an effect all across the body.
true
hereditary disorders with reduced synthesis of globs, resulting in microcytic and hypochromic anemia
thalassemias
There are 4 genes that code for normal hemoglobin. Which of the following can result in serious medical conditions that may reduce life expectancy?
A. 4 genes/0 deletions
B. 3 genes/1 deletion
C. 2 genes/2 deletions
D. 1 gene/3 deletions
E. 0 genes/4 deletions
D & E
--C = thalassemia minor, mild anemia
--D = thalassemia major, normal at birth but need transfusions by first year
--E = stillborn