Pediatrics Exam #3
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
Diagnostic procedures for neurologic disorders
-CT scan
-angiography
-echonecphalography
-EEG
-Long-term Video EEG
-Lumbar puncture
-MRI
definitive diagnostic test for neurologic dysfunction
-Lumbar puncture
•The provider inserts a spinal needle into the
subarachnoid space between L3 and L4, and L5 vertebral spaces.
•Measures spinal fluid pressure and collects
CSF for analysis.
causes of neurologic dysfunction
Anything that could cause potential for decreased cerebral tissue perfusion.
How would the nurse know??
•Alteration of arterial or venous blood flow
•Cerebral infarction
•Hemorrhage
•Hematoma
•Increased intracranial pressure (ICP)
•Cerebral edema
disorders of neurologic dysfunction
•Meningitis
•Reye Syndrome
•Seizures
•Head Injury
Increased intracranial pressure
Increased ICP reflects the pressure in the brain exerted by the blood, brain, CSF, and any other space-occupying fluid or mass.
Increased ICP is defined as pressure sustained at 20 mm Hg or higher for 5 minutes or longer.
Symptoms:
Infant
-poor feeding or vomitting
-irritability or restlessness
-lethargy
-bulging fontanel
-high pitched cry
-increased head circumference
-separation of cranial sutures
-distended scalp veins
-eyes deviated downward (setting sun sign)
-increased or decreased response to pain
Child
-headache
-diplopia
-mood swings
-slurred speech
-papilledema (after 48 hours)
-altered level of consciousness
-nausea and vomiting, especially in the morning
What might cause increased ICP?
High intracranial pressure (ICP) in children can result from various causes, including:
•Hydrocephalus
•Brain tumors
•Intracranial bleeding/hemorrhage
•Brain infections(Meningitis/Reye Syndrome)
•Trauma
Hydrocephalus
Develops as the result of an imbalance of production and absorption of CVF
-Most often congenital
-Arnold-Chiari malformations
-Enlarged ventricles and ICP
-Head circumference abnormally large
-Treatment consists of ventriculoperitoneal (VP) shunt
Nursing care for a VP shunt
A ventriculoperitoneal (VP) shunt is a surgical device used to divert excess cerebrospinal fluid (CSF) from the ventricles of the brain to the peritoneal cavity.
Nursing care focuses on:
•Preventing complications
•Monitoring for signs of shunt malfunction
•Providing family education.
Postoperative Care & Monitoring
Positioning: Initially, position the infant flat
Monitor for signs of increased intracranial pressure (ICP):
•Bulging fontanel
•High-pitched cry
•Lethargy
•Irritability
•Vomiting
•Sunset eyes (downward gaze)
•Widened Sutures
Assess for bradycardia and hypertension, which may indicate increased ICP.
Monitor the Surgical Site:
Observe for redness, swelling, leaking CSF, or signs of infection at the incision sites (head and abdomen).
•Signs of Shunt Infection (Meningitis or Peritonitis):
•Fever
•Poor feeding
•Vomiting
•Redness/swelling along the shunt tract
•Lethargy or irritability
Family Education
•Teach parents when to seek emergency care for signs of shunt malfunction or infection.
•Explain that regular neurosurgical follow-ups are needed as the child grows (shunt revisions may be necessary).
•Encourage gentle handling and tummy time to prevent pressure on the shunt site.
Acute neurological disorders
•Meningitis is an inflammation of the
cerebrospinal fluid (csF) and meninges.
•Reye syndrome is a life-threatening disorder
that involves acute encephalopathy and fatty
changes of the liver.
•Meningitis and Reye syndrome have similar
manifestations and are both sometimes
preceded by viral infections.
Meningitis
•Viral (aseptic) meningitis usually requires
only supportive care for recovery.
•Bacterial (septic) meningitis is a contagious
infection.
•Prognosis depends on how quickly care is
initiated
Risk Factors
•Incidence of bacterial meningitis has decreased in all age groups except infants under the age of 2 months since the introduction of the Hib and pneumococcal conjugate vaccines
(PCV).
•Injuries that provide direct access to CSF
(skull fracture, penetrating head wound)
•Crowded living conditions
Expected Findings:
- Photophobia
- Nausea
-Irritability
-Headache
Infants to 2 years
•Seizures with a high-pitched cry
•Fever and irritability
•Bulging fontanels- Measure the head circumference every shift!!!
•Possible nuchal rigidity
•Poor feeding
•Vomiting
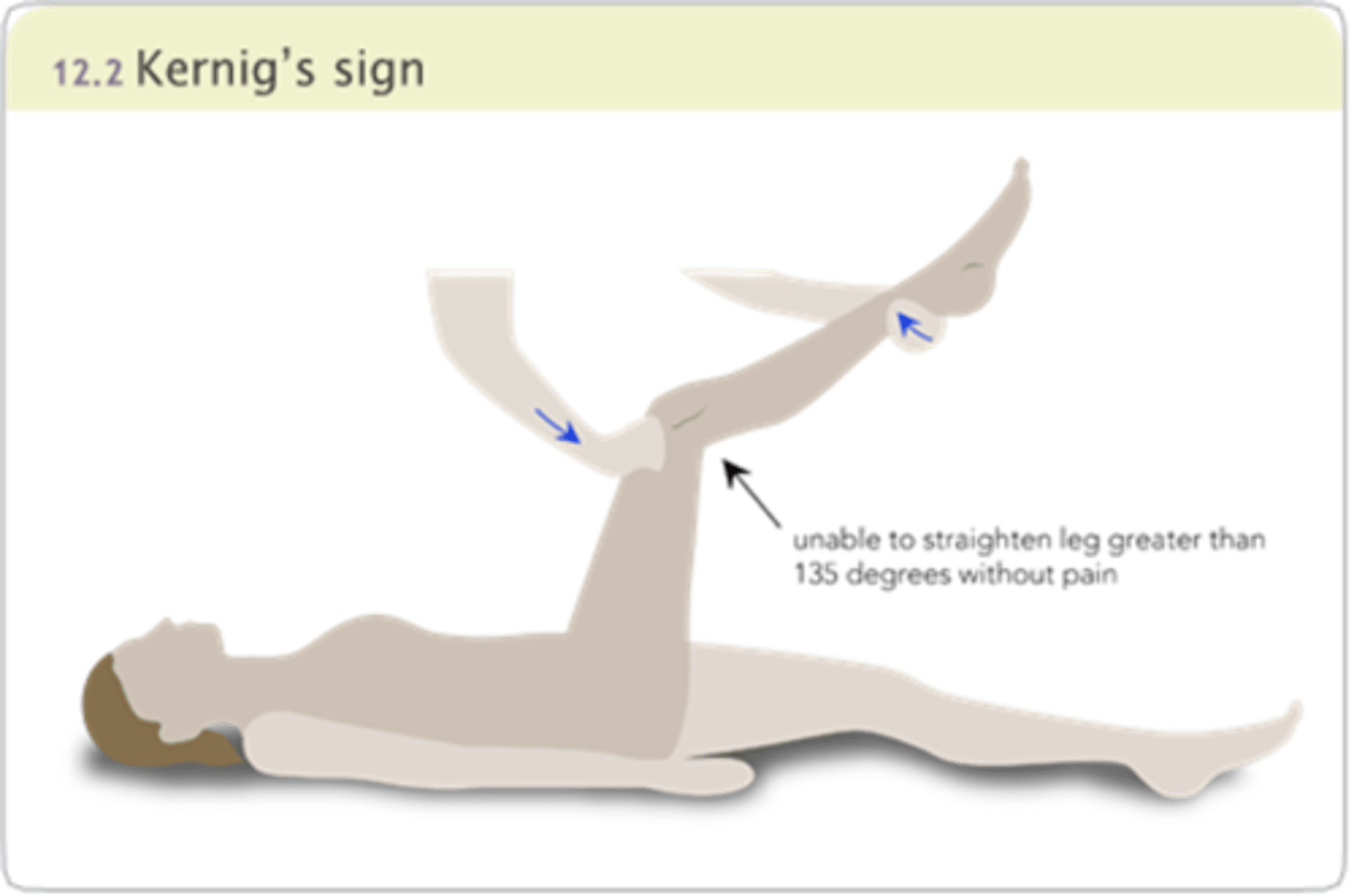
•Brudzinski’s (flexion of extremities occurring with deliberate flexion of the child’s neck) and Kernig’s (resistance to extension of the child’s leg from a flexed position) signs not reliable
for diagnosis
2 years through adolescence
•Seizures (often initial sign)
•Nuchal rigidity
•Positive Brudzinski’s and Kernig’s sign
•Fever and chills, Headache
•Vomiting
•Irritability and restlessness
•Petechiae or purpuric-type rash
•Involvement of joints (with meningococcal and Hib)
•Chronic draining ear
child’s leg from a flexed position)
that can progress to drowsiness, delirium, stupor, and coma (with meningococcal infection)
Brudzinki's sign image
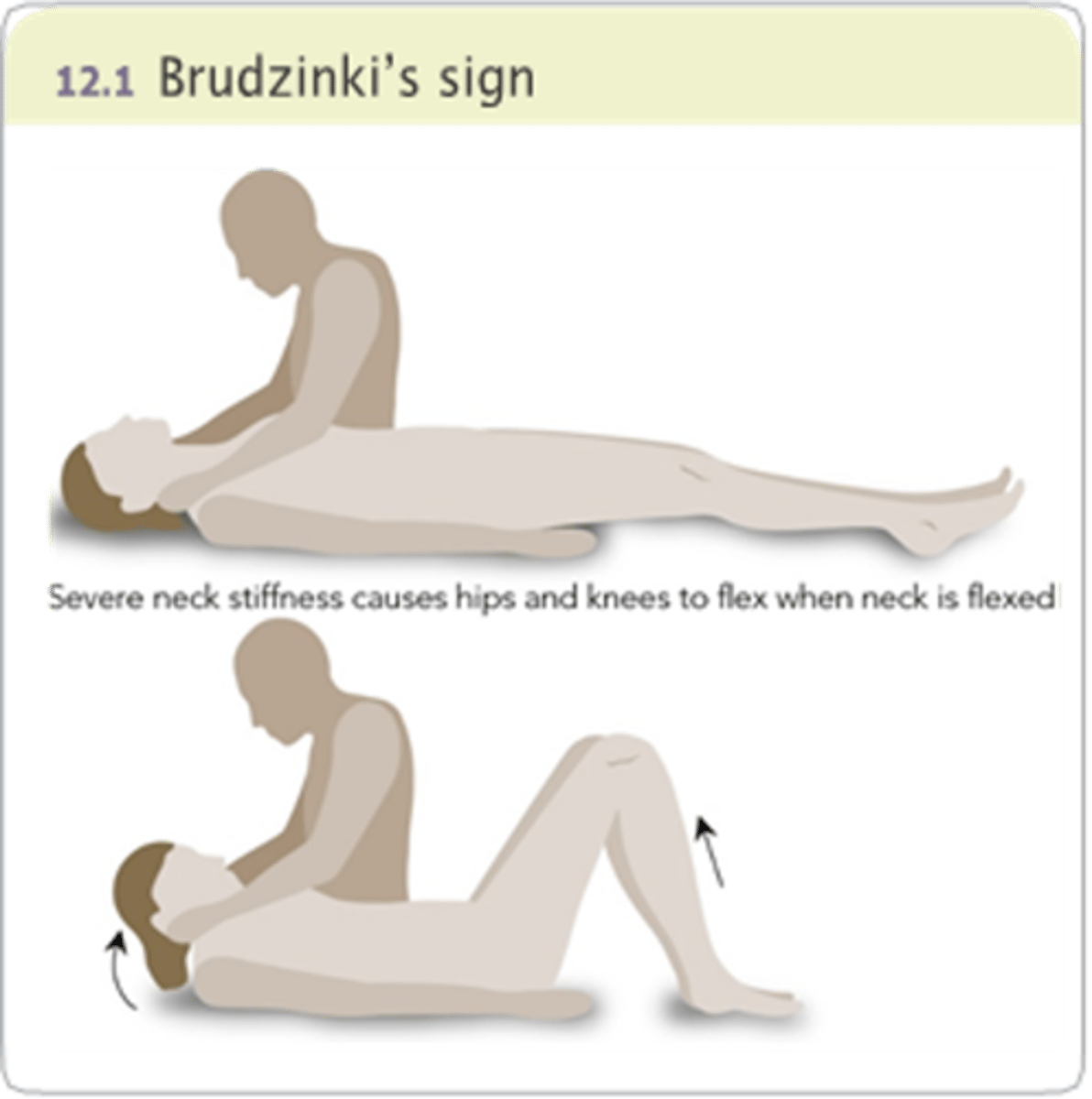
Kernig's sign image
Meningitis labs and diagnostic procedures
Send Blood cultures, CBC
CSF analysis indicative of meningitis:
BACTERIAL
•Cloudy color
•Elevated WBC count, elevated protein
•Decreased glucose content
•Positive Gram stain
VIRAL
•Clear color
•Slightly elevated WBC count
•Normal or slightly elevated protein content
•Normal glucose content
•Negative Gram stain
CT scan or MRI
Performed to identify increased (ICP) or
abscess.
NURSING ACTIONS
Assist with positioning.
Administer sedatives as prescribed.
Nursing care and medications for meningitis
Nursing Care
•The presence of petechiae or a purpuric-type rash requires immediate medical attention.
•Isolate the client as soon as meningitis is suspected, and maintain droplet precautions per facility protocol.
•Providers and visitors should wear a mask.
•Maintain respiratory isolation for a minimum of 24 hr after initiation of antibiotic therapy.
•Monitor vital signs, urine output, fluid status, pain level, and neurologic status.
•For newborns and infants, monitor head circumference and fontanels for changes and bulging.
•Correct fluid volume deficits and then restrict fluids until no evidence of increased ICP and serum sodium levels are within the expected range.
•Maintain NPO status if the client has a decreased level of consciousness.
•As the client’s condition improves, advance to clear liquids and then a diet the client can tolerate.
Medications
Antibiotics
•Administer IV antibiotics.
•Length of therapy is determined by the client’s condition and CSF results.
•Therapy can last up to 10 days.
•Educate the family about the need to complete the entire course of medication.
Corticosteroids: dexamethasone
•Not indicated for viral meningitis.
•Assists with initial management of increased ICP, but might not be effective for long-term complications.
•Most effective for infections caused by Hib.
•Educate on administration and possible adverse effects of the medication.
Complications of meningitis
Complications
Increased intracranial pressure
•Could lead to neurological dysfunction
•Monitor for signs of increased ICP.
•Newborns and infants: bulging or tense fontanels, increased head circumference, high-pitched cry, distended scalp veins, irritability, bradycardia, and respiratory changes
Monitor for Signs of Increased ICP
Newborns and infants: bulging fontanels, increased head circumference, high-pitched cry, distended scalp veins, irritability, bradycardia, and respiratory change.
Children: increased irritability, headache, nausea, vomiting, diplopia, seizures, bradycardia, and respiratory changes.
Provide interventions to reduce ICP (positioning; avoidance of coughing, straining, and bright light, minimizing environmental stimuli).
Reye Syndrome
•Primarily affects the liver and brain, causing dysfunction and cerebral edema.
•The cause of Reye syndrome is not understood.
•Peak incidence of Reye syndrome occurs when influenza is most common, typically January through March.
Risk factors
•There is a potential association between using aspirin (salicylate) products for treating fevers caused by viral infections.
•Reye syndrome typically follows a viral illness
• Influenza
• Gastroenteritis
• Varicella
Expected findings
Recent viral illness or use of aspirin or aspirin-containing products.
Reye syndrome presents in clinical stages based on the severity of liver and neurologic findings.
•Lethargy
•Irritability, Combativeness
•Confusion, Delirium
•Profuse vomiting
•Seizures
•Loss of consciousness
Labs
•Liver enzymes [ALT] [AST]: elevated
•Serum ammonia level: elevated.
•Serum electrolytes: altered due to cerebral edema and liver changes.
•Coagulation times can be extended.
Nursing Care
•Maintain hydration while preventing cerebral edema.
•Administer IV fluids as prescribed.
•Maintain accurate I&O.
•Insert indwelling urinary catheter as ordered.
•Position the client.
•Avoid extreme flexion, extension, or rotation.
•Maintain the head in a midline neutral position.
•Keep the head of the bed elevated 30°.
Reye Syndrome medications, client education, and complications
Medications
Osmotic diuretic: Mannitol
•To decrease cerebral swelling.
•Monitor for increased ICP.
Vitamin K Improves synthesis of blood clotting factors in the liver
•Subcutaneous is the preferred route.
-Identify client sensitivity to benzyl alcohol and castor oil.
•Teach the client about dietary intake of vitamin K.
Client Education
•Teach parents to avoid giving salicylates for pain or fever in children.
•Teach parents to read labels of over-the-counter medications to check for the presence of salicylates.
•Clients regain full liver function, but can have some neurological deficits.
Complications
Neurologic complications include speech or hearing impairment, and developmental delays based on the length and severity of illness.
•Explain the client’s condition and needs to the family.
•Help the family identify support services for home care.
Death
•Support the family in grief.
•Make referrals to spiritual support as appropriate.
seizures
•Some seizures have no known etiology
•Febrile episode
•Cerebral edema
•Intracranial infection or hemorrhage
•Brain tumors or cysts
•Anoxia
•Toxins or drugs/Lead poisoning
•Tetanus, Shigella, or Salmonella
•Hypoglycemia, hypocalcemia, hyponatremia, hypernatremia, or hypomagnesemia
Generalized: Tonic/Clonic
Absence seizure
•Onset between ages of 5 to 8 years and stops by teenage years.
•Loss of consciousness lasting 5 to 10 seconds.
•Minimal or no change in behavior.
•Resembles daydreaming or inattentiveness.
•Lip smacking, twitching of eyelids or face, or slight hand movements.
•Unable to recall episodes, can be momentarily confused.
•Can immediately resume previous activities.
Nursing care
•Protect from injury
•Maintain a position to provide a patent airway.
•Be prepared to suction oral secretions.
•Turn child to a side-lying position
•Loosen restrictive clothing.
•Do not attempt to restrain the child.
•Do not attempt to put anything in the child’s mouth.
•Administer oxygen
•Remain with the child, note onset, time, and characteristics of seizure.
When to call 911
•Child stops breathing
•Seizure lasts more than 5 min
•Status epilepticus occurs
•Pupils are not equal following seizure
•Child vomits 30 min continuously after end of seizure
•Child is unresponsive to pain or cannot be awakened
•Seizure occurs in water
•This is the child’s first seizure
Medications
•Diazepam, phenytoin, carbamazepine, valproic acid, and fosphenytoin sodium, topiramate, lamotrigine, clonazepam.
•Medication selection is based on the client’s age, type of seizure.
•A single medication is initiated at low dosage and gradually increased until seizures are controlled.
•Shake the medication bottle well!
•A second medication can be added to achieve seizure control.
•Dosage can need to be increased as the child grows.
Complications of seizures
•Status Epilepticus
•Developmental Delays
Head Injury
•Concussion is a traumatic injury to the brain that alters the way the brain functions.
•Contusion is bruising of the cerebral tissue.
•Laceration is tearing of the cerebral tissue.
•Fractures: linear, depressed, comminuted, basilar, open, or growing.
Prevention
•Wear helmets
•Wear seat belts when driving or riding in a car
•Avoid dangerous activities (riding a bicycle at night without a light, driving faster than the speed limit or while under the influence of alcohol or controlled substances).
•Never shake a baby.
Head Injury Assessment Findings
Assessment Findings
Severe injury: Increased ICP
INFANTS:
•Bulging fontanel/Separation of cranial sutures
•Irritability, restlessness, increased sleeping
•High-pitched cry, poor feeding, distended scalp veins
CHILDREN:
•Nausea, headache, forceful vomiting
•Blurred vision, increased sleeping, inability to follow simple commands
•Decline in school performance/Seizures
LATE SIGNS:
•Alterations in pupillary response
•Posturing (flexion and extension)
•Bradycardia
•Decreased motor response
•Decreased response to painful stimuli
•Cheyne-Stokes respirations
•Optic disc swelling
•Decreased consciousness
•Coma
Flexion (severe dysfunction of the cerebral cortex):
Demonstrates the arms, wrists, elbows, and fingers flexed and bent inward onto the chest and the legs extended and rotated internally.
Extension (severe dysfunction at the level of the midbrain):
Demonstrates a backward arching of the legs and arms, flexed wrists and fingers, extended neck, clenched jaw, and possibly an arched back.
Head Injury Nursing care and complications
Nursing Care
ICP management is same as adults
Medications
•Mannitol
•Antiepileptics
•Antibiotics: with CSF leakage, lacerations, or penetrating injuries
•Analgesics (acetaminophen)
Therapeutic Procedures
•Transfontanel percutaneous aspiration
•Subdural drains/Burr hole
•Craniotomy
Complications
Epidural hematoma:
Bleeding between the dura and the skull
Manifestations:
Short period of unconsciousness followed by a normal period for several hours, then lethargy or coma due to the accumulation of blood in the epidural space and compression of the brain.
Subdural hemorrhage: Bleeding between the dura and the arachnoid membrane.
Might be a result of birth injury, falls, or violent shaking
Manifestations:
Irritability, vomiting, increased head circumference, lethargy, seizures, coma
Musculoskeletal disorders
Musculoskeletal disorders in children can be congenital, developmental, or acquired.
Some common conditions include:
•Clubfoot (Talipes Equinovarus) – A birth defect where the foot is twisted out of shape or position.
•Congenital Hip Dysplasia (Developmental Dysplasia of the Hip, DDH) – Abnormal hip joint development, leading to instability or dislocation.
Developmental Disorders
Scoliosis – Abnormal lateral curvature of the spine, which can progress as a child grows.
Acquired Disorders
•Juvenile Idiopathic Arthritis (JIA) – An autoimmune disease causing joint inflammation, pain, and stiffness.
•Spinal Bifida
Fractures: partial or complete break of a bone
Trauma
–Increased mobility puts young children at risk
Inadequate motor and cognitive skills
–Accidental trauma
•Falls, sports, motor vehicle crashes
–Nonaccidental trauma
–Child abuse
Pathologic conditions
•Osteogenesis imperfecta
Plastic deformation (bend)
Buckle (torus)
Greenstick: Incomplete fracture of the bone.
Transverse: Break is straight across the bone.
Oblique: Break is diagonal across the bone.
Spiral: Break spirals around the bone.
Physeal (growth plate)
Stress: Small fractures/cracks in the bone
Complete: Bone fragments are separated.
Incomplete: Bone fragments are still attached.
Closed or simple
Open or compound
Complicated fracture
Comminuted
Fractures
Management of fractures in children focuses on:
•Realigning the bone (reduction)
•Closed= non surgical
•Open= surgical
•Immobilizing the injury
•Promoting healing while minimizing complications
•Because children's bones are still growing, proper immobilization is critical to prevent epiphyseal plate disturbances and deformities.
Nursing Care
Each condition often requires long-term treatment including Immobilization and Surgery:
•Splinting
•Traction
•Bracing
•Casting
•Surgery
•A combination of the above
•Assessment for Compartment Syndrome
•Provide emergency care at the time of injury.
•Maintain ABCs.
•Assess the neurovascular status of the injured extremity.
•Stabilize the injured area
•If a pelvic fracture is suspected, monitor urine for blood and for development of hypovolemic shock
•Elevate the affected limb and apply ice packs (not to exceed 20 min).
•Administer analgesics as prescribed.
•Keep the client warm.
Compartment Syndrome
Key Assessment Steps Neurovascular Checks (6 Ps):
1. Pain (Early Sign) – Severe, persistent pain that is disproportionate to the injury and not relieved by medication or elevation.
2. Pallor – Pale, cool skin indicating compromised circulation.
3. Pulselessness (Late Sign) – Weak or absent distal pulses suggest arterial compromise.
4.Paresthesia – Numbness, tingling, or "pins and needles" sensation, indicating nerve compression
5. Paralysis (Late Sign) – Inability to move the affected limb, suggesting severe nerve damage.
6.Pressure – The affected area may feel tight or tense, a sign of increased compartment pressure.
•Capillary Refill – Delayed (>2 seconds) suggests poor perfusion.
•Skin Temperature – Coolness below the cast indicates decreased circulation.
•Swelling and Firmness – Increased edema or tightness around the cast.
•Dyspnea- why?
Nursing Interventions:
•Elevate the limb at heart level (not above) to maintain perfusion.
•Loosen the cast or bandages if allowed per protocol.
•Notify the provider immediately for suspected compartment syndrome—this is a medical emergency.
•Prepare the child for potential fasciotomy if needed.
Immobilizing devices
•Splints
•Casts
•Hip Spica Cast: femur and hip fractures
•Traction
•Skin
•Skeletal
•External fixation devices
•Halo traction
Nursing care of casts
•Provide atraumatic care by showing the procedure on a doll or toy.
•Assess and monitor neurovascular status.
•Elevate the cast above the level of the heart to prevent swelling.
•Apply ice for the first 24 hr.
•Turn and position the client every 2 hr
•Do not use heat lamps or warm hair dryers.
•Keep the affected extremity supported (with a sling) or elevated when sitting.
•Assess for increased warmth or hot spots, which could indicate infection.
Nursing care of spica cast
•Reinforce skin and perineal care with a spica cast.
•Instruct the client not to place any foreign objects inside the cast to avoid trauma to the skin.
•Reinforce use of proper restraints when transporting the client in any vehicle.
•Teach the client and parents about cast removal and cast cutter.
•Instruct the client to soak the extremity in warm water and then apply lotion after the cast has been removed.

Traction
Used for severe fractures or when casting is not immediately possible.
Types:
Bryant's Traction – Used for femur fractures in children <2 years old.
Buck's Traction – Used for lower limb fractures, helps with pain and alignment.
Skeletal Traction – Uses pins/wires inserted into the bone (e.g., for complex femur fractures).
Nursing Considerations:
-Maintain proper alignment.
-Ensure weights hang freely and are not touching the floor.
-Monitor for skin breakdown and infection (especially with skeletal traction).
Musculoskeletal congenital disorders
•Musculoskeletal congenital disorders might be identified at birth or might not be present until later in infancy, childhood, or adolescence.
•These disorders can involve a specific areas of the child's body or affect the child's entire musculoskeletal system.
•Careful assessment and inter-professional management assist in promoting the child's growth, development, and mobility.
Clubfoot
•A complex deformity of the ankle and foot.
•Can affect one or both feet, occur as an isolated defect, or in association with other disorders such as cerebral palsy and spinal bifida
•Categorized as positional clubfoot (occurs from intrauterine crowding)
•Syndromic (occurs in association with other syndromes)
•congenital (idiopathic)
Therapeutic procedures
•Series of castings starting shortly after birth.
•Weekly manipulation of the foot to stretch the muscles with subsequent placement of a new cast.
•Heelcord tenotomy.
•A Denis Browne bar that connects specialized shoes can be applied to maintain the correction and prevent recurrence.
•Assess neurovascular status.
•Perform cast care.
•Teach family follow-up care for cast changes.
Developmental Dysplasia of the Hip (DDH)
•A variety of disorders resulting in abnormal development of the hip structures that can affect infants or children.
•Asymmetry of gluteal and thigh folds
•Limited hip abduction
•Shortening of the femur
•Widened perineum
•Positive Ortolani test (hip is reduced by abduction)
•Positive Barlow test (hip is dislocated by adduction)
CHILD
-One leg shorter than the other
-Positive Trendelenburg sign (while bearing weight on the affected side, the pelvis tilts downward)
-Walking on toes on one foot
-Walk with a limp
Newborns to months:
•Pavlik harness
When adduction contracture is present:
Bryant traction
•Skin traction
•Hips flexed at a 90° angle with the buttock raised off of the bed
•Neurovascular checks
•Maintain traction
•Ensure the client maintains alignment
•Skin care
When adduction contracture is present:
Hip spica cast
•Assess and maintain the hip spica cast.
•Perform frequent neurovascular checks.
•Perform range of motion with the unaffected extremities.
•Perform frequent assessment of skin integrity, especially in the diaper area.
•Evaluate hydration status frequently.
Hip spica cast
•Position casts on pillows.
•Note color and temperature of toes on casted extremity.
•Give sponge baths to avoid wetting the cast.
•Use a waterproof barrier around the genital opening of spica cast to prevent soiling.
•Educate regarding care after discharge on using appropriate equipment(stroller, wagon, car seat) for maintaining mobility.
6 months to 2 years
•Surgical closed reduction with placement of hip spica cast
Older children
•Surgical reduction with presurgical traction
•Femoral osteotomy, reconstruction, and tenotomy are often needed
Pavlik Harness
Pavlik Harness is an orthopedic device used to treat developmental dysplasia of the hip (DDH) in infants.
It helps keep the baby's hips in proper alignment to promote normal joint development.

Bryant traction
•Used primarily for young children with femur fractures or developmental dysplasia of the hip (DDH).
•It helps maintain proper alignment of the hip and femur before surgery or casting.
•The child lies flat on their back in bed.
•Both legs are suspended at a 90-degree angle to the hips.
•The hips are slightly lifted off the bed to maintain traction.
•The weights provide gentle, continuous pulling force to align the femur or hip joint.
Nursing Care
•Perform frequent neurovascular checks (6 Ps).Check capillary refill, skin temperature, and pedal pulses.
•Maintain Proper Positioning
•Ensure hips remain at 90 degrees.
•Keep buttocks slightly off the bed, not resting fully.
•Make sure weights hang freely and are not touching the floor.
•Assess skin under the traction straps for irritation or breakdown.
•Change diapers frequently to prevent skin breakdown.
•Perform range-of-motion exercises for the upper body to prevent stiffness.
•Administer analgesics as prescribed for pain relief.
•Provide age-appropriate activities to prevent boredom.

Spinal Bifida
•Failure of the osseous spine to close.
•Neural tube defects (NTDs) are present at birth and affect the CNS and osseous spine.
•Meningocele: The sac contains spinal fluid and meninges.
•Myelomeningocele: The sac contains spinal fluid, meninges, and nerves.
Risk Factors
•Medications/substances taken during pregnancy
•Maternal malnutrition
•Insufficient folic acid intake during pregnancy
•Exposure to radiation or chemicals during pregnancy
Procedures
•Neurosurgery, neurology, urology, orthopedics, pediatrics, physical therapy, occupational therapy, and social services
•Closure of a myelomeningocele sac is done as soon as possible to prevent complications of injury and infection.
•Protect the sac from injury.
•Place infant in a warmer, without clothing.
•Apply a sterile, moist, nonadhering dressing with 0.9% sodium chloride on the sac, changing it every 2 hr.
•Inspect the sac closely for leaks, irritation, abrasions and localized indications of infection.
•Assess for systemic indications of infection (fever, irritability, and lethargy).
•Place infant in the prone position with hips flexed, legs abducted.
•Administer IV antibiotic as prescribed.
•Avoid rectal temperatures.
•Avoid cuddling or putting pressure on the sac.
Complications
•Skin Ulcerations
•Latex Allergy
•Increased intracranial pressure
•Caused by shunt malfunction or hydrocephalus.
•Bladder Issues
•Orthopedic Issues
(pic is of a repaired myelomeningocele)

Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) is a chronic autoimmune disorder causing joint inflammation, pain, stiffness, and potential long-term disability.
Nursing care focuses on pain management, mobility, and preventing complications.
Pain Management (Priority)
–NSAIDs (e.g., ibuprofen, naproxen) to reduce inflammation.
–Disease-Modifying Anti-Rheumatic Drugs (DMARDs) (e.g., methotrexate) to slow disease progression.
–Biologic Agents (e.g., etanercept, adalimumab) for severe cases.
–Corticosteroids (short-term use for severe inflammation).
•Apply Heat Therapy – Warm compresses or warm baths help relieve joint stiffness.
•Encourage Gentle Range of Motion (ROM)
•Helps reduce morning stiffness.
•Encourage Physical Therapy & Daily Exercise
•Low -impact activities like swimming or yoga improve joint flexibility.
•Use Assistive Devices if Needed
•Splints, braces, or orthotics to prevent contractures.
•Alternate Activity with Rest Periods
•Prevents fatigue while maintaining mobility
•Assess for Joint Swelling, Redness, and Decreased Mobility
•Early signs of worsening inflammation.
•Monitor Growth & Development
•JIA may affect growth plates, leading to limb discrepancies.
•Assess for Uveitis (Eye Inflammation)
•Can cause vision loss; children need regular ophthalmology exams.
•Support Coping Strategies
•Chronic pain can lead to anxiety and depression.
•Ensure Adequate Calcium & Vitamin D Intake
•Prevents osteoporosis due to prolonged corticosteroid use.
Vaccines
•Vaccines have the same antigen as the disease, but it is either killed or weakened and therefore not strong enough to cause the disease.
•Antibodies disappear after they destroy the infection/antigen, but memory cells are formed to protect from future exposures to that same infection.
•This is called immunity.
•Tetanus
•Diphtheria
•Pertussis (Whooping Cough)
•Hemophilis influenza type b (Hib)
•Polio
•Hepatitis A
•Hepatitis B
•Rotavirus
•Mumps
•Measles
•Rubella (German Measles)
•Varicella (Chickenpox)
•Pneumococcus
•Meningococcus
•Influenza
•Human Papilloma Virus (HPV)
Vaccines at birth
Hepatitis B
Vaccines at 2 months
-Hepatits B
-DTap (diptheria, tetanus, pertusis)
-Hib (Haemophilius influenzae type B)
-Polio (IPV)
-PCV (pneumococcal conjugate vaccine)
-RV (rotavirus vaccine)
vaccines at 4 months
-DTap (diptheria, tetanus, pertusis)
-Hib (Haemophilius influenzae type B)
-Polio
-PCV (pneumococcal conjugate vaccine)
-RV (rotavirus vaccine)
Everything from 2 months EXCEPT Hepatitis B
Vaccines at 6 months
-Hepatits B
-DTap (diptheria, tetanus, pertusis)
-Hib (Haemophilius influenzae type B)
-Polio
-PCV (pneumococcal conjugate vaccine)
-RV (rotavirus vaccine)
-Influenza
Everything from 2 months & add flu
vaccines from 12-18 months
-DTap
-Hib
-PCV
-MMR (measles, mumps, rubella)
-Varicella
-Hepatitis A
and can get flu
vaccines from 4-6 years
-DtTap
-Polio
-MMR
-Varicella
(remember starts at 4 years old and the get 4 vaccines) - also can get flu
Health Promotion: Planning to give Vaccines to 6-12 year old
•DtaP again at 4 -6 years
•Td booster once every 10 years
•Hib again at 4 - 6 years
•MMR 12-15mo and 4-6 years
•Varicella vaccine—1 dose at 12-15mo again at 4-6 years
•Meningococcal 11-12 years
•HPV2—11-12years (females) HPV4(males) 9 years
•Check med dose calculations
Vaccine Complications
•A severe allergic reaction can occur in response to any vaccine, and is a contraindication for receiving further doses.
•Moderate or severe illnesses with or without fever are precautions to receiving immunizations.
•The common cold and other minor illnesses are not contraindications to immunizations.
•Severe febrile illness is a contraindication to all immunizations.
•Do not administer live virus vaccines, such as varicella or MMR, to a child who is severely immunocompromised.
Precautions to immunizations require providers to analyze data and weigh the risks that come with immunizing or not immunizing. (35.2)
Health Promotion: Contraindications for MMR Vaccine
•Production of antibodies that prevent illness from a specific microbe.
•Children who have fever should not receive this vaccine.
•Contraindications for MMR vaccination include history of a severe (anaphylactic) reaction to a previous dose or to any component of the vaccine, and patients who are immunocompromised.
Vaccines: Nursing Administration
•Verify informed consent from the child's legal guardian prior to administration.
•Provide vaccine information sheets (VIS)
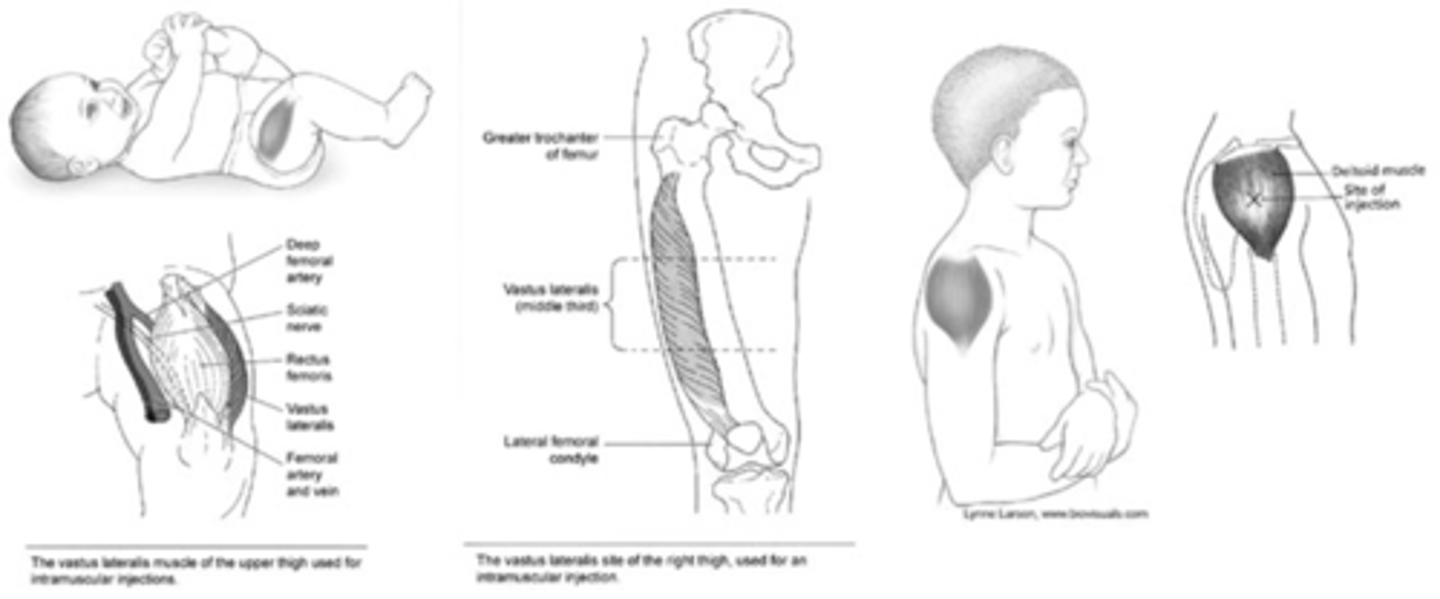
•Include the publication date.
•Give IM immunizations in the vastus lateralis or ventrogluteal muscle in infants and young children, and into the deltoid muscle for older children and adolescents.
•Give subcutaneous injections in the outer aspect of the upper arm or anterolateral thigh.
•Provide distraction
•Apply a topical anesthetic prior to injection, administration
•Give infants a concentrated oral sucrose solution
Use an appropriately sized needle for the route, site, age, and amount of medication. Adequate needle length reduces the incidence of swelling and tenderness at the injection site.
•Have emergency medications and equipment on standby in case the child experiences an allergic response, such as anaphylaxis (rare).
•During the procedure: cuddling, pacifiers
•After the procedure: applying cool compresses to injection site, gentle movement of involved extremity
•Provide praise afterward.
•Apply a colorful bandage, if appropriate.
•Document the administration of the vaccine.
-Date, route, and site of immunization
-Type, manufacturer, lot number, and expiration date of the vaccine
•Encourage parents to maintain up-to-date immunizations for the child.
•Instruct parents to avoid administering aspirin.
•Instruct the parents and child to observe for complications and notify the provider if adverse effects occur.
•Report any adverse reactions to the Vaccine Adverse Event Reporting System.
Communicable diseases
•Easily spread through airborne, droplet, or direct contact transmission.
•Most communicable diseases can be prevented with immunizations.
•Antibiotics and antitoxins reduce serious complications.
•Primary prevention refers to immunizations.
•Secondary prevention controls the spread of the disease to others.
Conjunctivitis
Spread: Direct contact
–Viral: Appears secondary to a viral infection; clears on its own in 7 to 14 days.
–Bacterial: Starts in one eye, spreads to the other; clears with antibiotics
–Allergic: Occurs in people who have other allergic conditions; clears with allergy medications.
•Pink or red color in the sclera of the eyes
•Swelling of the conjunctiva
•Excessive tearing
•Yellow-green, purulent discharge from the eyes
•Crusting of the eyelids in the morning
Epstein-Barr virus (EBV)/mononucleosis
•Spread: Saliva
•Incubation: 30 to 50 days
–Healthy people can carry EBV in saliva, transmitting the virus for a lifetime.
–People who have mononucleosis can transmit for weeks.
•Fever
•Lethargy
•Sore throat
•Swollen lymph glands
•Loss of appetite
•Headache
•Increased WBC
•Atypical lymphocytes
•Splenomegaly
•Hepatic involvement
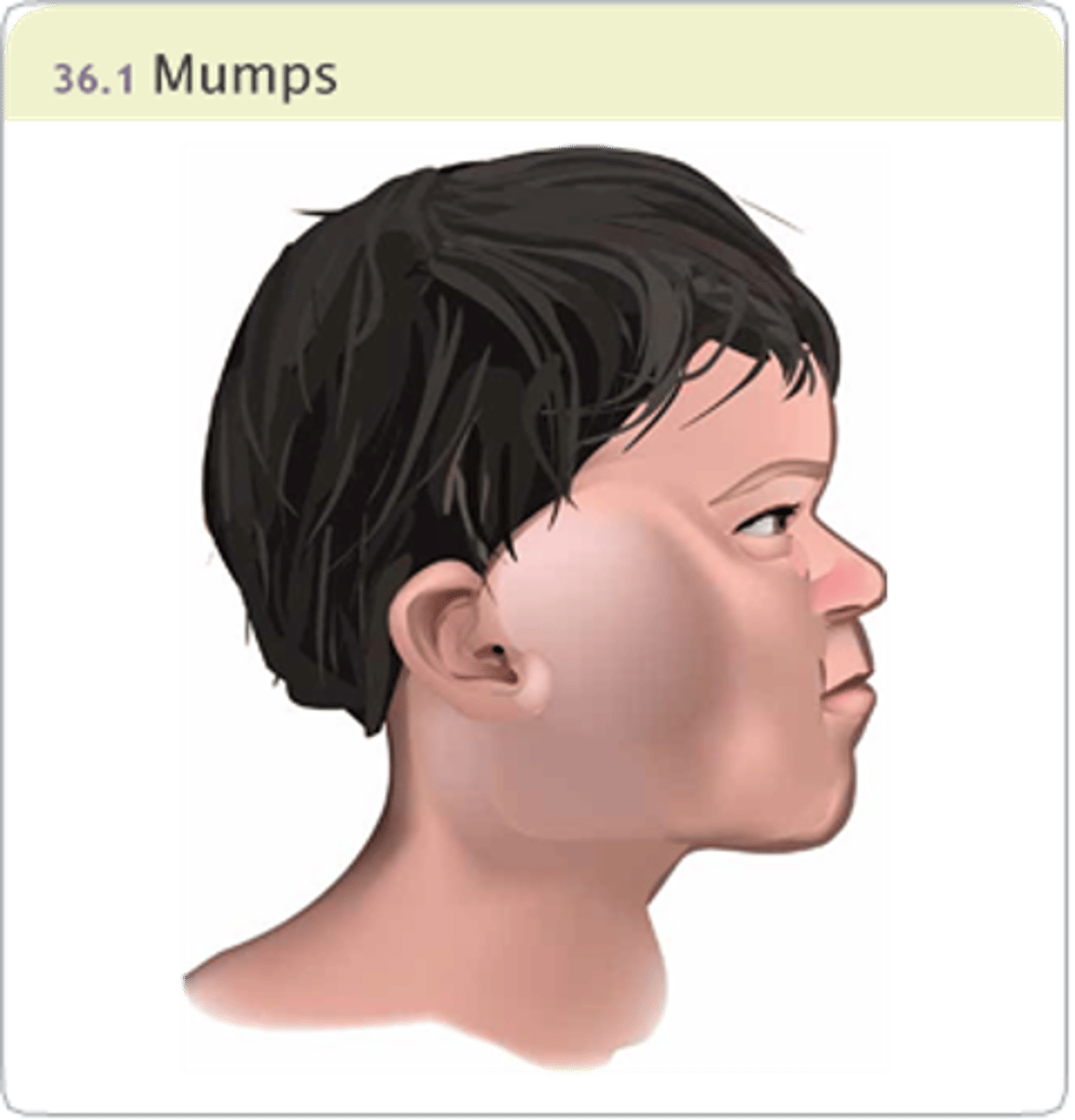
Mumps
•Spread: Direct Contact
•Incubation: 14 to 21 days
•Contagious: Immediately before and after swelling begins
•Painful, swollen parotid glands
•Fever and muscle aches
•Headache
•Earache made worse by chewing
•Fatigue and loss of appetite
Pertussis
•Spread: Direct contact
–Droplet
–Indirect contact with freshly contaminated articles
•Incubation: 6 to 20 days, usually 7 to 10 days
•Contagious: Greatest during catarrhal stage before onset of paroxysmal stage
•Common cold manifestations: runny nose/congestion, sneezing, mild fever, mild cough
•Severe coughing starts in 1 to 2 weeks
•Coughing fits
–Violent and rapid coughing
–Loud “whooping” sound upon inspiration
Rubella (German measles)
•Spread: Direct contact
–Droplet
•Incubation: 14 to 21 days
•Contagious: 7 days before to 5 days after the rash appears
•Low-grade fever and sore throat
•Headache
•Malaise
•Cough
•Lymphadenopathy
•Red rash that starts on the face and spreads to the rest of the body, lasting 2 to 3 days
Rubeola (measles)/rubeola virus
•Spread: Direct contact
–Droplet
•Incubation: 10 to 20 days
•Contagious: 4 days before to 5 days after the rash appears
3 TO 4 DAYS PRIOR TO RASH
•Mild to moderate fever
•Conjunctivitis
•Fatigue
•Cough, runny nose, red eyes, sore throat
RASH
•Tiny white spots appear in mouth 2 days before rash
•Red or reddish-brown rash beginning on the face spreading downward
•Spike in fever with rash
Varicella (chickenpox)/ varicella-zoster virus
•Spread: Direct contact
–Droplet (airborne)
–Contaminated objects
•Incubation: 2 to 3 weeks, usually 14 to 16 days
•Contagious: 1 day before lesions appear until all lesions have formed crusts
1-2 DAYS PRIOR TO RASH
•Fever
•Fatigue
•Loss of appetite
•Headache
RASH
•Macules start in center of trunk, spreading to the face and proximal extremities.
•Progresses from macules, to papules, to vesicles, and crust formation follows.
•Scabs appear in approximately 1 week.
Risk factors for communicable diseases
•History of communicable disease
•Immunocompromised status
•Crowded living conditions
•Poor sanitation
•Poor nutrition
•Poor oxygenation and impaired circulation
•Chronic illness
•Recent exposure to a known case of a communicable disease
•Not immunized or up-to-date on immunizations
•Prodromal manifestations
Nursing care for communicable diseases
•Administer an antipyretic for fever.
•Administer an antipruritic for severe itching
•Administer analgesics for pain.
•Provide fluids and nutritious foods
•Provide quiet diversional activities.
•Promote adequate rest
•Keep the child out of the sun.
•Notify the child’s school or day care center of the child’s infection.
•Notify the health department of communicable diseases.
Skin Care
•Provide calamine lotion for topical relief.
•Keep the skin clean and dry.
•Keep the child cool, but prevent chilling.
•Dress the child in lightweight, loose clothing.
•Give baths in tepid water.
•Keep the child’s fingernails clean and short.
•Apply mittens if the child scratches.
•Teach good oral hygiene.
•Change linens daily.
Isolation precautions for communicable diseases
•Airborne/Contact: Varicella
•Droplet
–Fifth disease
–Mumps
–Pertussis
–Rubella
•Standard
–Conjunctivitis
–Mononucleosis
medications for communicable diseases
Antihistamine
•Diphenhydramine hydrochloride and hydroxyzine used to control pruritus
•Monitor the reaction to the medication because some children can become hyper-alert with the administration of a medication from this group.
•Monitor for drowsiness.
•Educate the family about safety precautions.
•Antibiotic or antiviral therapy
–Acyclovir for high-risk clients who have varicella
–Antibiotics for pertussis
•Antibiotic eye drops for bacterial conjunctivitis
•NSAIDs or acetaminophen
–Decreases fever
–Teach parents the proper dosing for acetaminophen.
Education for communicable diseases
•Good hand hygiene
•Encourage adherence with antibiotic or antiviral therapy.
•Instruct parents to teach the child to cover nose and mouth when coughing or sneezing.
•Instruct parents to wash the child’s bed linens daily in mild detergent.
•Teach parents of children who are immunocompromised to seek prompt medical care if manifestations develop.
•Encourage adolescents to participate in decision-making.
•Rubella
Complications generally rare with this communicable disease
Birth defects (deafness; heart defects; mental, liver, and spleen damage) in fetus of women infected during pregnancy
•Rubeola: Ear infections, pneumonia, diarrhea, encephalitis, death, laryngitis
•Varicella: Pneumonia, bleeding problems, bacterial infection of the skin, encephalitis
Complications for communicable diseases
•Mononucleosis: Ruptured spleen
•Myocarditis: Fetal death if mother is infected during the second trimester of pregnancy
•Mumps: encephalitis, meningitis, deafness, myocarditis, arthritis, hepatitis
•Pertussis
–Infants and children: pneumonia, seizures, apnea, encephalopathy, death, ear infections, hemorrhage, weight loss, hernias
–Teens and adults: weight loss, loss of bladder control, syncope, rib fractures, pneumonia
Acute Otitis Media
•An infection of the structures of the middle ear.
•Otitis media with effusion (OME) is a collection of fluid in the middle ear but no infection.
•Repeated infections can cause impaired hearing and speech delays.
•Many infections clear spontaneously in a few days.
Risk Factors
•Ear tubes in children are shorter and more horizontal than those of adults.
•Most common in the first 24 months of life and again when children enter school.
•Occurs infrequently after age 7.
•Usually triggered by a bacterial infection
–Streptococcus pneumoniae
–Haemophilus influenza
–Moraxella catarrhalis)
–Viral infection (respiratory syncytial virus or influenza)
–Allergies
–enlarged adenoids.
•There is a lower incidence of otitis media in infants who are breastfed.
•Incidence is higher in the winter and spring months.
•Exposure to large numbers of children (day care).
•Exposure to secondhand smoke.
•Cleft lip and/or cleft palate.
•Noncompliance with childhood vaccinations
•Down syndrome
Diagnostic Tests
•A pneumatic otoscope is used to visualize the tympanic membrane and middle ear structures.
•The otoscope also assesses tympanic membrane movement.
•Gently pull the pinna down and back to visualize the tympanic membrane of a child younger than 3 years old.
•For a child older than 3 years, gently pull the pinna up and back.
Expected findings for acute otitis media
•Recent history of upper respiratory infection
•Acute onset of changes in behavior
•Frequent crying, irritability, and fussiness
•Inconsolability
•Tugging at ear
•Reports of ear pain, loss of appetite, nausea, and vomiting
•Rubbing or pulling on ear
•Crying
•Lethargy
•Bulging yellow or red tympanic membrane
•Purulent material in middle ear or drainage from external canal
•Temperature: can be as high as 40° C (104° F)
•Hearing difficulties and speech delays if otitis media becomes a chronic condition
•Feeling of fullness in the ear
•Orange discoloration of the tympanic membrane with decreased movement
•Vague findings including rhinitis, cough, and diarrhea
•Transient hearing loss and balance disturbances
Nursing Care for acute otitis media
•Provide comfort measures.
•Administer pain medication as needed.
•Provide diversional activities.
•Place child in an upright position.
•Management of fevers.
•Acetaminophen or ibuprofen
•Used to provide analgesia and reduce fever
•Obtain a liquid preparation.
•Use age-appropriate techniques to administer medication.
•Myringotomy and tympanoplasty tubes are indicated for a child who has multiple episodes of otitis media.
•This procedure is performed in an outpatient setting with the administration of general anesthesia.
•It is usually completed in 15 min.
•A small incision is made in the tympanic membrane, and tiny plastic or metal tubes are placed into the eardrum to equalize pressure and minimize effusion.
•Recovery takes place in a PACU, and discharge usually occurs within 1 hr.
•Postoperative pain is not common and, if present, will be mild.
•The tubes come out spontaneously (usually in 6 to 12 months).
•Limit the child's activities for a few days following surgery.
•Instruct parents to notify the provider when tubes come out.
•Instruct the family to avoid getting water into the child's ears while the tubes are in place.
•The effectiveness of earplugs is not conclusive.
•Inform the client and parents about comfort measures.
•Encourage the parents to feed the child in an upright position when bottle- or breastfeeding.
•If drainage is present, clean the external ear with sterile cotton swabs. Apply antibiotic ointment.
•Stress the importance of seeking medical care at initial signs of infections (change in behavior, tugging on ear).
•Encourage the parents to keep the child's immunizations up to date.
Antibiotics for acute otitis media
Antibiotics
•Amoxicillin, PO (10 to 14 days)
•Ceftriaxone IM (once)
•Wait 72 hr for spontaneous resolution of otitis media before starting antibiotic.
•Administer in high doses orally, usually 80 to 90 mg/kg/ day in two divided doses.
•IM is used for resistant organisms or for client-specific reasons
•Observe for signs of allergy to the antibiotic, such as rash or difficulty breathing.
complications of acute otitis media
Hearing loss and/or speech delays
•Assess and monitor for deficits.
•Refer the child for audiology testing if needed.
•Speech therapy may be necessary.
HIV/AIDS
•Women who are infected with HIV/AIDS can transmit the virus to the fetus or infant prenatally or by breast milk.
•Exposure to blood products or body fluids that contain the HIV virus
•Sexual abuse
•Risky behaviors, such as unprotected sexual activity and IV substance use
•Sexually transmitted infections
Category N: Not symptomatic
•No manifestations are present
Category A: Mildly symptomatic
•Children have two or more of the following:
–Lymphadenopathy
–Hepatomegaly
–Splenomegaly
–Recurrent upper respiratory infections, sinusitis, or otitis media
–Dermatitis
Category B: Moderately symptomatic
More serious manifestations, such as:
•Bacterial meningitis, pneumonia, or sepsis
•Oropharyngeal candidiasis
•Cardiomyopathy
•Cytomegalovirus infection
•Hepatitis
•Herpes simplex virus (HSV)
•Leiomyosarcoma
•Lymphoid interstitial pneumonia (LIP)
•Persistent fever
•Toxoplasmosis before 1 month of age
•Disseminated varicella
Category C: Severely symptomatic
•Multiple serious bacterial infections
•Esophageal or pulmonary candidiasis, (bronchi, trachea, lungs)
•Cytomegalovirus disease
•HSV stomatitis, bronchitis, pneumonitis, or esophagitis
•Kaposi’s sarcoma
•Disseminated mycobacterium tuberculosis
•Encephalopathy with developmental delays
Complications of HIV/AIDS
•Failure to thrive
•Obtain a baseline height and weight, and continue to monitor.
•Promote optimal nutrition.
•This can require the administration of total parenteral nutrition.
•Assess growth and development.
•Monitor for delays.
•Provide opportunities for normal development (age‑appropriate toys, playing with children of the same age).
•Educate the child and parents about appropriate nutrition and how to meet nutritional needs.
Cranial Nerves
1. Olfactory (Smell)
2. Optic (Ability to see)
3. Oculomotor (Eye movement, pupillary constriction, accommodation, eyelid opening)
4. Trochlear (Eye movement up and down, back and forth)
5. Trigeminal (Facial sensation, taste, and jaw movements)
6. Abducens (abduction of eyes)
7. Facial (facial expression and taste)
8. Vestibulocochlear (sense of hearing and balance)
9. Glossopharyngeal (taste and swallow)
10. Vagus (digestion and heart rate)
11. Accessory (movement of head and shoulders)
12. Hypoglossal (Tongue movement)
Pnemonic to remember cranial nerves
Only
One
Of
The
Two
Athletes
Felt
Very
Good
Victorious
And
Healthy
Pneumonic to remember if cranial nerves are sensory motor or both
Some
Say
Marry
Money
But
My
Brother
Says
Big
Brains
Matter
More
Organ neoplasms diagnostic studies
Wilms’ tumor
•Abdominal ultrasonography
•Abdominal and chest CT
•Bone marrow aspiration (rule out metastasis)
Neuroblastoma
•Skeletal survey
•Skull, neck, chest, abdominal, and bone CT scans
•Bone marrow aspiration (rule out metastasis)
•Biopsy of tumor
Wilms tumor (nephroblastoma)
•Wilms tumor (nephroblastoma) is a malignancy that occurs in the kidneys or abdomen.
•Diagnosis typically occurs before age 5, with most cases diagnosed between 2 and 3 years of age.
•Metastasis is rare.
There are no known risk factors for Wilms’ tumor
Wilms’ tumor clinical findings include:
•Painless, firm, non-tender abdominal swelling or mass
•Fatigue, malaise, weight loss
•Fever
•Hematuria
•Hypertension
•Manifestations of metastasis include dyspnea, cough, shortness of breath, and chest pain.
Nursing care:
•If Wilms’ tumor is suspected, do not palpate the abdomen.
•Use extreme caution when handling or bathing the client to prevent trauma to the tumor site.
•Assess the child’s and family’s coping and support.
•Assess for developmental delays related to illness.
•Assess physical growth (height and weight).
•Provide education and support to the child and family regarding diagnostic testing, treatment plan, ongoing therapy, and prognosis.
•Monitor for findings of infection.
•Administer antibiotics as prescribed for infection.
•Keep the child’s skin clean, dry, and lubricated.
•Provide oral hygiene, and keep the child’s lips lubricated.
•Provide age‑appropriate diversional activities.
•Provide support to the child and family.
•Avoid false reassurance.
•Listen to the child’s concerns.
•Allow time for the child and family to discuss feelings regarding grief and loss.
Neuroblastoma
•Malignancy that occurs in the adrenal gland, sympathetic chain of the retroperitoneal area, head, neck, pelvis, or chest.
•It is usually manifested during the toddler years, with 95% of cases prior to age 10.
•Half of all cases have metastasized before diagnosis.
•Manifestations depend upon the location and stage of disease.
•Manifestations of metastasis include an ill appearance, periorbital ecchymoses, proptosis, bone pain, and irritability.
Treatment options for Wilms' tumor and neuroblastoma
Treatment for Wilms’ tumor
•Surgical removal of the tumor and kidney soon after diagnosis.
•Preoperative chemotherapy or radiation if both kidneys are involved to decrease the size of the tumors and potentially preserve one kidney.
•Postoperative radiation and/or chemotherapy for children who have large tumors, metastasis, reoccurrence, and residual disease.
Treatment for neuroblastoma
•Surgical removal of the tumor.
•Chemotherapy and/or radiation for metastasis and residual disease.
Chemotherapy
The child can have a long‑term central venous access device or peripherally inserted central catheter in place.
Wilms’ tumor
•Acinomycin D and vincristine
•For tumors at more advanced stages, with unfavorable histology, or that recur after treatment, other medications such as doxorubicin and cyclophosphamide can be used.
Neuroblastoma: Various combination of agents are used: cyclophosphamide, doxorubicin, cisplatin, etoposide, vincristine, ifosfamide, and carboplatin.
•Provide an antiemetic prior to administration.
•Allow several food choices, including favorite foods.
•Observe the mouth for mucosal ulcerations.
•Offer cool fluids to prevent dehydration and soothe sore mucous membranes.
•Educate about side effects (mouth sores, loss of appetite, nausea and vomiting, hair loss, diarrhea or constipation, increased risk of infection, easy bruising or bleeding, and fatigue).
•Educate about the importance of immunizations and follow‑up appointments.
•Educate about good infection control practices.
•Use good hand hygiene.
•Encourage the child and family to use good hand hygiene.
•Encourage the child to avoid crowds while undergoing chemotherapy.
•Screen visitors and staff for indications of infection.
•Instruct the child to avoid fresh fruits and vegetables.
•Avoid invasive procedures (injections, rectal temperatures, catheters).
•Apply pressure to puncture sites for 5 min.
•Monitor for signs of bleeding.
•Avoid aspirin and NSAIDs.
Radiation
•Usually delivered in divided treatments over several weeks.
•Wear lead aprons.
•Teach to wash the marked areas with lukewarm water, use hands instead of a washcloth, pat dry, and take care not to remove the markings.
•Teach the child and family to avoid use of soaps, creams, lotions, and powders unless they are prescribed.
•Encourage wearing loose cotton clothing.
•Keep the areas protected from the sun.
•Instruct the family to seek medical care for blisters, weeping, and red/tender skin.
Surgical Intervention for cancers
Tumor de-bulking
•Avoid palpation of Wilms’ tumor.
•Monitor gastrointestinal activity (bowel sounds, bowel movements, distention, nausea, vomiting).
•Provide pain relief.
•Monitor vital signs and assess for any findings of infection.
•Encourage pulmonary hygiene.
•Provide preoperative teaching that includes length of surgery, where the child will recover, and what equipment will be in place (nasogastric tube, IV line, indwelling urinary catheter).
Chemo complications
•Metastasis
•Kidney failure
•Pancytopenia
•Bone marrow depression
•Resulting in anemia, neutropenia, and/or thrombocytopenia
•Report a temperature greater than 37.8° C (100° F).
•Monitor for findings of infection (lung congestion; redness, swelling and pain around IV sites) and lesions in the mouth.
•Monitor the wound site and immunization status.
•Administer antimicrobial, antiviral, and antifungal medications as prescribed.
•Monitor the child for headache, fever, and mild to moderate bone pain.
•Administer epoetin alfa subcutaneously two to three times per week
•Monitor blood pressure.
•Encourage the use of a soft toothbrush.
•Use gentle handling and positioning to protect from injury.
•Organize care to provide for rest. Schedule rest periods.
•Educate the child and family about infection control procedures at home.
Chemo side effects
Anorexia, nausea, vomiting
•Avoid strong odors.
•Provide a pleasant atmosphere for meals.
•Avoid offering the child’s favorite foods during chemotherapy because they can develop an aversion to these foods.
•Suggest and assist in selecting foods/fluids.
•Provide small, frequent meals.
•Administer antiemetics as prescribed, usually
•before meals.
Alteration in bowel elimination
•Diarrhea is a result of radiation.
•Some chemo can cause constipation. If mobility and nutrition decrease, the child is more likely to develop constipation.
•Provide meticulous skin care.
•Determine if certain foods or drinks (high‑fiber, lactose‑rich) worsen the child’s condition.
•Monitor I&O and daily weight.
Mucositis and dry mouth
•Provide a soft toothbrush and/or swabs.
•Lubricate the child’s lips.
•Give soft, nonacidic foods. A pureed or liquid diet can be required.
•Provide analgesics.
•Avoid hydrogen peroxide and lemon glycerin Encourage to visit a dentist before therapy.
•Encourage the use of chlorhexidine mouth wash or salt rinses using ½ tsp table salt mixed with 1 tsp baking soda and 1 quart water.
Alopecia
•Assess the child’s feelings.
•Discuss cutting long hair short.
•Use gentle shampoos. Gently brush the child’s hair.
•Avoid blow dryers and curling irons.
•Suggest wearing a cotton hat or scarf.
•Discuss the use of a wig, turbans, or hats.
•Avoid blow dryers and curling irons.
•Stress the importance of scalp hygiene.
•Teach families that hair grows back in 3 to 6 months.
Blood neoplasms
•Leukemia is the term for a group of malignancies that affect the bone marrow and lymphatic system.
•Classified by the type of WBCs that becomes neoplastic and is commonly divided into two groups:
-acute lymphoid leukemia (all)
-acute myelogenous or nonlymphoid leukemia (aml/aNll).
•Leukemia causes an increase in the production of immature WBCs, which leads to infiltration of organs and tissues.
•Leukemia is the most common cancer of childhood
•Male gender and Caucasian clients
•Peak onset between 2 and 5 years of age.
•Family history of leukemia
•Children who have trisomy 21 (Down syndrome)
Early and Late Manifestations of blood neoplasms
EARLY MANIFESTATIONS
•Low-grade fever/ Pallor
•Bruising and petechiae
•Listlessness/Unsteady gait
•Enlarged liver, lymph nodes, and joints
•Abdominal, leg, and joint pain
•Constipation
•Headache/Vomiting/Anorexia
LATE MANIFESTATIONS
•Pain
•Hematuria
•Ulcerations in the mouth
•Enlarged kidneys and testicles
•Manifestations of increased intracranial pressure
History and physical assessment findings can reveal vague reports (anorexia, headache, fatigue).
blood neoplasms labs
Complete blood count
● Anemia (low blood count)
● Thrombocytopenia (low platelets)
● Neutropenia (low neutrophils)
● Leukemic blasts (immature WBCs)
blood neoplasms diagnostics
Bone marrow aspiration: The most definitive diagnostic procedure.
•The specimen will show prolific quantities of immature leukemic blast cells and protein markers indicating a specific type of leukemia.
•Topical anesthetic may be applied over the biopsy area 45 min to 1 hr prior to the procedure.
•Unconscious sedation is induced using a general anesthetic, such as propofol.
•Positioning depends on the access site to be used (posterior or anterior iliac crest is most common; tibia can be used in infants because it is easier to access and hold the infant).
Cerebrospinal fluid (CSF) analysis
•CSF, obtained by lumbar puncture, is assessed to determine CNS involvement.
•Have the child empty his bladder.
•Assist the provider with the procedure.
•A topical anesthetic cream may be applied over the biopsy area 45 min to 1 hr prior to the procedure.
Liver and kidney function studies
•Used for baseline functioning before chemotherapy
•Draw the appropriate amount of serum.
•Educate the child and parents about the length of time to receive results.
blood neoplasms nursing care
•Provide emotional support to the child and parents.
•Encourage peer contact if appropriate.
•Assess pain using an age-appropriate pain scale.
•Use pharmacological and nonpharmacological interventions to provide around-the-clock pain management.
Chemotherapy for blood neoplasms
Chemotherapy is administered in four phases to treat leukemia:
•Induction therapy
•CNS prophylactic therapy
•Intensification therapy (consolidation)
•Maintenance therapy: To sustain the remission phase
•Control nausea and vomiting with antiemetics prior to treatment.
•May be combined with dexamethasone.
•Manage side effects of treatment.
CHEMOTHERAPY SIDE EFFECTS
•Mucosal ulceration/Jaw Pain
•Neuropathy/Foot Drop
•Constipation
•Loss of appetite
•Alopecia
LATE EFFECTS: Cardiomyopathy, cognitive and neuropsychological defects
◯ Inspect skin daily.
◯ Assess rectal mucosa for fissures.
◯ Avoid rectal temperatures.
◯ Provide sitz baths as needed.
◯ Reposition frequently.
◯ Use a pressure reduction system.
Encourage a diet high in fiber.
■ Administer stool softeners and laxatives as needed.
■ Encourage fluids.
Use a footboard in bed.
■ Weakness and numbness of extremities
■ Assist with ambulation.
•Steroid treatment can cause moon face.
•The child can experience mood changes.
•Teach manifestations of infection, skin breakdown, and nutritional deficiency.
•Encourage good hygiene.
•Avoid individuals who have infectious diseases.
•Instruct how to administer medications and provide nutritional support at home.
•Proper use of vascular access devices.
•Bleeding precautions and the management of active bleeding.
therapeutic procedures for blood neoplasms
Hematopoietic stem cell transplant (HCST)
•Coordinate administration of high-dose chemotherapy and possible full-body radiation.
•Administer donor stem cells via IV infusion.
•Implement protective isolation/Private, positive-pressure room
•At least 12 air exchanges/hr/ HEPA filtration for incoming air
•Respirator mask, gloves, and gowns
•No dried or fresh flowers, and no potted plants
•The child is at an increased risk for infection and bleeding until transfused stem cells grow.
HCST can be indicated for children who have AML during the first remission and for children who have ALL after a second remission.
Allogeneic transplant: The blood-forming stem cells generally are donated by another person.
Radiation therapy to the brain
•Assist with positioning.
•Provide support to the child and family.
•Manage side effects.
•Educate the child and parents regarding side effects (fatigue, infection).
•Encourage adequate rest and a healthy diet.
•Second malignancy
•Cognitive and neuropsychological defects
Complications from therapeutic procedures for blood neoplasms
Infection
•Provide a private room with adequate air flow to reduce airborne pathogens.
•Restrict visitors and health personnel who have active illnesses.
•Adhere to strict hand hygiene.
•Assess potential sites of infections (oral ulcer, open cut)
•Administer antibiotics as prescribed
•Encourage adequate protein and caloric intake.
•Monitor absolute neutrophil count (ANC).
•Educate about manifestations of infection.
•Teach avoidance of live vaccines while the immune system is depressed.
Hemorrhage
•Monitor for findings of bleeding: petechiae, ecchymoses, hematuria, bleeding gums, hematemesis, tarry stools.
•Avoid unnecessary skin punctures, and use surgical aseptic technique when performed.
•Treat a nosebleed with cold and pressure.
•Administer platelets concentrates or platelet rich plasma as prescribed.
•Avoid obtaining temperatures rectally.
•Teach the importance of meticulous oral care to prevent gingival bleeding.
•Use a soft toothbrush, and avoid astringent mouthwashes.
•Teach the parents measures for controlling epistaxis.
Anemia
•Administer blood transfusions as prescribed.
•Allow for frequent rest periods.
•Administer oxygen therapy.
•Administer IV fluid replacement.
•Educate the child and parents about foods high in iron.
bone and soft tissue cancers
•Bone cancer can originate from all tissues involved in bone growth
•Osteosarcoma usually occurs in long bones.
•Soft tissue malignancies arise in muscles, tendons, connective or fibrous tissue, or in blood or lymph vessels.
•Rhabdomyosarcoma originates in skeletal muscle, but most commonly occurs in the head neck, and orbit of the eye.
•Children who undergo irradiation for malignancies in or near the pelvic area can experience sterilization and secondary cancers.
Risk factors:
•Osteosarcoma peaks at age 15 during growth spurts and is more common in boys than girls.
•Ewing's sarcoma occurs prior to 30 years of age and is more common in Caucasian clients than for other races.
Clinical Findings:
•Nonspecific bone pain that is often mistaken for an injury or growing pains
•Temporary relief of pain when extremity is flexed
•Weakness, swelling, or decreased movement of the extremity
•Palpable lymph nodes near the tumor
•Anemia, generalized infection, or unexplained weight loss
•Limpness or inability to hold a heavy object
Diagnostics:
•CBC
•X-ray
•Computed tomography (CT) scans
•Magnetic resonance imaging (MRI)
•Bone marrow biopsy
•CT of the chest and bone scans to evaluate metastasis
Nursing care:
•Be honest when answering questions and when giving information about the disease and treatment.
•Allow the child time, usually several days, to prepare emotionally for surgery and chemotherapy.
•Avoid overwhelming the child with information.
•Provide emotional support for the child and family.
bone and soft tissue cancer medications
Chemotherapy
•Osteosarcoma
•High-dose methotrexate with citrovorum factor rescue, doxorubicin, cisplatin, ifosfamide, and etoposide
•Ewing’s sarcoma: Vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide
Amitriptyline
•A tricyclic antidepressant for use with neuropathic pain or phantom pain in adolescents who have had an amputation.
•Monitor for drowsiness, orthostatic hypotension, anticholinergic effects, seizures, mania, and cardiac dysfunction.
•Teach the child and family how to manage adverse effects.
•Caution the child and parents about taking only the prescribed dosage to prevent toxic reactions.
bone and soft tissue cancer procedures
Limb salvage procedure for bone cancers
•Includes chemotherapy to shrink the tumor and then total bone and joint replacement after the tumor and affected bone are removed.
•Administer preoperative chemotherapy.
•Provide routine postoperative care.
•Provide adequate pain relief.
•Teach the child and family about any expected effects of preoperative chemotherapy, such as hair loss.
Limb amputation for bone cancer
•The child can receive chemotherapy both preoperatively and postoperatively.
•Provide routine preoperative and postoperative care.
•Provide emotional support.
•Care for the stump as prescribed.
•Assess for the presence of phantom limb pain postoperatively, and medicate appropriately.
•Prepare the child for fitting of a temporary prosthesis, which can occur immediately after surgery.
•Encourage cooperation with postoperative physical therapy.
•Role-play issues that the child will need to deal with after discharge, such as talking to strangers who ask about the prosthesis.
•Assist the family to recognize that the child’s emotions, such as anger, are normal grief reactions after amputation, chemotherapy, and other treatments.
•Older children and adolescents can benefit from attending a support group for children who have cancer and/or have had amputations.
•Initiate a referral for mental health counseling to assist the child to resume normal activities.
•Initiate physical and occupational therapy referrals to start while in the hospital and to continue after discharge.
bone and soft tissue cancer complications
Skin desquamation
•Either dry or moist, with permanent hyperpigmentation and possible damage to underlying structures
•Assess the site frequently for infection.
•Teach the parents methods to prevent additional irritation to the site.
•Use loose-fitting clothing.
•Prevent exposure to sunlight or extremes of temperature.
Myelosuppression
•This can cause infection (reduced leukocytes), hemorrhage (reduced thrombocytes), and anemia (reduced red blood cells).
•Evaluate laboratory data and assess for manifestations of complications.
•Infection: elevated WBC and fever
•Hemorrhage: blood in urine or stool, bruising, and petechiae
•Anemia: fatigue and decreased hemoglobin/hematocrit
Prevent infection.
◯ Provide a private room when hospitalized.
◯ Restrict staff/visitors that have infections.
◯ Promote frequent hand hygiene by staff/visitors.
◯ Avoid all live-virus vaccines during periods of immunosuppression.
◯ Ensure that siblings are up-to-date on immunizations.
◯ Provide a diet adequate in protein and calories.
● Prevent hemorrhage or injury from bleeding.
◯ Use a strict aseptic technique for all invasive procedures.
◯ Use gentle technique when providing mouth care.
◯ Clean the perineal area carefully to prevent trauma, and avoid obtaining temperatures rectally.
◯ Infuse platelets as prescribed.
● Prevent anemia or injury from anemia.
◯ Provide rest periods as needed.
◯ Infuse packed red blood cells as prescribed.
CLIENT EDUCATION: Teach family members strategies
to recognize complications at home and to prevent injury from infection, hemorrhage, or bleeding.
rhabdomyosarcoma
•Occurs in children of all ages (but more commonly in children younger than 5 years of age) and is more common in Caucasians than for other races.
•Can cause pain in local areas related to compression by the tumor (sore throat can occur with tumor of the nasopharynx)
•Possible absence of pain in some parts of the body
•CNS: headaches, diplopia, vomiting
•Orbit: unilateral proptosis, ecchymosis of conjunctiva, strabismus
•Nasopharynx: stuffy nose, pain, nasal obstruction, epistaxis, palpable neck nodes, visible mass (late)
•Paranasal sinuses: nasal obstruction, pain, discharge, sinusitis, swelling
•Middle ear: chronic otitis media, pain, sanguinopurulent discharge, facial paralysis
•Retroperitoneal area: usually no symptoms, abdominal mass, pain, intestinal or genitourinary obstruction
•Perineum: visible superficial mass, bowel or bladder obstruction
•Extremity: pain, palpable fixed mass, lymph node enlargement
•CT scans or MRI of the primary site
•Biopsy of tumor is possible
•CT of the chest, bone scans, bone marrow biopsy, and lumbar puncture to evaluate metastasis
•Be honest when answering questions and when giving information about the disease and treatment.
•Allow the child time, usually several days, to prepare emotionally for surgery and chemotherapy.
•Avoid overwhelming the child with information.
•Provide emotional support for the parents and child.
•Treatment includes chemo, radiation and surgery.
•Older children and adolescents can benefit from attending a support group for children who have cancer.
•Initiate a referral for mental health counseling to assist the child to resume normal activities.
•Initiate physical and occupational therapy referrals to start while in the hospital and to continue after discharge.
Epistaxis
Short, isolated occurrences are common in childhood.
Rarely an emergency, it causes anxiety for the child and caregivers.
Risk Factors:
-Trauma, such as picking or rubbing the nose
-Low humidity, allergic rhinitis, upper respiratory infection, blunt injury, or a foreign body in the nose
-Medications that affect clotting factors can increase bleeding.
-Underlying diseases
(von Willebrand disease, hemophilia, idiopathic thrombocytopenia purpura, leukemia).
Nursing care:
-Maintain a calm demeanor
-Have the child sit up with the head tilted slightly forward to prevent aspiration of blood.
-Apply pressure to the lower nose with the thumb and forefinger for at least 10 min.
-If needed, pack cotton or tissue into the side of the nose that is bleeding.
-Apply ice across the bridge of the nose if bleeding continues.
-Inform the family that bleeding usually stops within 10 min.
Complications:
Hemorrhage
-NURSING ACTIONS:
-Provide support to the child during cauterization or packing.
-CLIENT EDUCATION:
-Instruct the child and family to seek medical care if bleeding lasts longer than 30 min, and that repeated episodes require further evaluation for bleeding disorders.
Iron deficiency anemia
-Most common anemia in the United States.
-Adolescents are at risk due to poor diet, rapid growth, menses, strenuous activities, and obesity.
-Usually results from an inadequate dietary supply of iron, and is the most preventable mineral disturbance
Symptoms:
-Tachycardia
-Pallor
-Brittle, spoon-shaped fingernails
-Fatigue, irritability, and muscle weakness
-Systolic heart murmur
Nursing Care:
ØProvide iron supplements
ØRecommend iron-fortified formula when solids are introduced
ØModify diet to include high iron, and vitamin C.
ØMonitor formula intake in infants.
ØLimit formula intake to 32 oz (960 mL) per day.
ØEncourage intake of iron-rich foods.
ØAllow frequent rest periods.
ØIf packed RBCs are required, follow protocols for administration
for preterm and low-birth-weight infants by the age of 2 months.
Provide iron supplements to full term infants by the age of 4 to 6 months.
Medications:
Iron supplements
-Give 1 hr before or 2 hr after milk or antacid to prevent decreased absorption.
-GI upset (diarrhea, constipation, nausea) is common at the start of therapy.
-If tolerated, administer on an empty stomach.
-Give with vitamin C to increase absorption.
-Use a straw with liquid preparation to prevent staining of teeth, follow with brushing.
-Educate the child and family to expect stools to turn a tarry green color if dose is adequate.
Give with meals and start with reduced dose and gradually increase if GI distress occurs.
Iron Food Sources:
-INFANTS: Iron-fortified cereals and formula
-OLDER CHILDREN: Dried beans and lentils; peanut butter; green, leafy vegetables; iron-fortified breads and flour; poultry; and red meat
Complications:
Developmental delay
-Assess level of functioning.
-Improve nutritional intake.
-Refer to appropriate developmental services.
-Provide support to the family.
Sickle Cell Anemia
-A group of diseases in which abnormal sickle hemoglobin S (HbS) replaces normal adult hemoglobin (Hgb A).
-Manifestations and complications are the result of RBC sickling, which leads to increased blood viscosity, obstruction of blood flow, and tissue hypoxia.
-Manifestations are not usually apparent until later in infancy due to the presence of fetal Hgb.
-Tissue hypoxia causes tissue ischemia, which results in pain.
-Increased destruction of RBCs occurs.
-Sickle cell crisis is the exacerbation of SCA.
-SCD is an autosomal recessive genetic disorder.
-SCA primarily affects African-Americans. Other forms of SCD can affect individuals of Mediterranean, Indian, or Middle Eastern descent.
-Children who have the sickle cell trait do not manifest the disease but can pass the trait to their offspring.
Clinical Findings:
-Family history of sickle cell anemia or sickle cell trait
-Reports of pain
-Shortness of breath, fatigue
-Pallor, pale mucous membranes
-Jaundice
-Hands and feet cool to touch
-Dizziness
-Headache
Vaso-Occlusive Episode (painful)
Usually lasts 4 to 6 days
Acute
-Severe pain, usually in bones, joints, and abdomen
-Swollen joints, hands, and feet
-Abdominal pain
-Hematuria
-Obstructive jaundice
-Visual disturbances
Usually lasts 4 to 6 days
Chronic
-Increased risk of respiratory infections and osteomyelitis
-Retinal detachment and blindness
-Systolic murmurs
-Renal failure and enuresis
-Liver cirrhosis; hepatomegaly
-Seizures
-Skeletal deformities; shoulder or hip avascular necrosis
Laboratory tests:
-Screening for SCA in newborns is mandatory in most states.
-CBC to detect anemia.
-Sickle-turbidity screening tool detects the presence of HbS but will not differentiate the trait from the disease.
-Hemoglobin electrophoresis separates the various forms of Hgb and is the definitive diagnosis of sickle cell anemia
Sickle Cell Crisis
-Hgb: decreased
-WBC count: elevated
-Bilirubin and reticulocyte levels: elevated
-Peripheral blood smear reveals sickled cells
Transcranial Doppler (TCD) test
-Used to assess intracranial vascular flow and detect the risk for cerebrovascular accident (CVA).
-A TCD is performed annually on children ages 2 to 16 years who have SCD.
Nursing Care:
-Promote rest to decrease oxygen consumption.
-Administer oxygen as prescribed if hypoxia is present.
-Maintain fluid and electrolyte balance.
-Monitor I&O.
-Give oral fluids.
-Administer IV fluids with electrolyte replacement.
-Administer blood products, usually packed RBCs, and exchange transfusions per facility protocol.
-Observe for manifestations of hypervolemia and transfusion reaction.
-Treat and prevent infection, give antibiotics
-Give oral prophylactic penicillin.
-Administer pneumococcal conjugate vaccine, meningococcal vaccine, and Haemophilus influenzae type B vaccine.
-Monitor and report laboratory results
Nursing Care Pain management:
-Use an interprofessional approach.
-Treat mild to moderate pain with acetaminophen or ibuprofen.
-Manage severe pain with opioid analgesics.
-Apply comfort measures, such as warm packs to painful joints.
-Schedule administration of analgesics to prevent pain.
Opioids
-Codeine, morphine sulfate, oxycodone, hydromorphone, and methadone.
-Administer orally (immediate- or sustained-release) or IV.
-Administer on a regular schedule to maintain control, or prevent pain if possible.
-Use patient-controlled analgesia if appropriate.
-Educate the child and family about the need to avoid activities that require mental alertness.
-Provide reassurance that analgesics can be necessary in high doses, and that addiction is rare.
Client education and complications for sickle cell disease
Education:
ØProvide emotional support, and refer to social services if appropriate.
ØTeach child and family about manifestations of crisis and infection.
ØAdvise the family of the importance of promoting rest and providing adequate nutrition for the child.
ØEncourage the child and family to practice good hand hygiene and avoid individuals who have colds/ infections/viruses.
ØGive specific directions regarding fluid intake requirements, such as how many bottles or glasses of fluid should be consumed daily.
ØProvide information about genetic counseling.
ØEncourage maintenance of up-to-date immunizations.
ØAdvise the child to wear a medical identification wristband or medical identification tags.
Compliations:
Cerebrovascular accident
-Seizures
-Abnormal behavior
-Weakness of, or inability to move an extremity
-Slurred speech
-Visual changes
-Vomiting
-Severe headache
-Blood transfusions are usually performed every 3 to 4 weeks to prevent a repeat CVA.
Acute chest syndrome
-Can be life-threatening
-Chest, back, or abdominal pain
-Fever of 38.5° C (101.3° F) or higher
-Cough
-Tachypnea
-Dyspnea
-Retractions
-Decreased oxygen saturations
Hemophilia
-A group of bleeding disorders characterized by difficulty controlling bleeding.
-Bleeding time is extended due to lack of a factor required for blood to clot.
-Bleeding is internal or external.
-Bleeding tendencies are sometimes recognized during infancy following circumcision, but might not become apparent until the infant becomes more active and prone to injuries during the toddler years.
-Varies in severity based on the percentage of clotting factor a child’s body contains.
uBoth hemophilia A and B are X-linked recessive disorders
Hemophilia A
-Deficiency of factor VIII: Referred to as classic hemophilia
-Accounts for 80% of cases
Hemophilia B
-Deficiency of factor IX
For example, a child who has mild hemophilia can have up to 49% of the normal factor VIII in his body, while a child who has severe hemophilia has very little factor VIII.
Clinical Findings:
-Episodes of bleeding, excessive bleeding, reports of joint pain and stiffness, impaired mobility, easy bruising, and activity intolerance
-Active bleeding, which includes bleeding gums, epistaxis, hematuria, and/or tarry stools
-Hematomas and/or bruising, even with minor injuries
-Hemarthrosis as evidenced by joint pain, stiffness, warmth, swelling, redness, loss of range of motion, and deformities
-Headache, slurred speech, and a decreased level of consciousness
Lab tests:
-Prolonged partial thromboplastin time (aPTT)
-Factor-specific assays to determine deficiency
-Platelets and prothrombin time are within expected reference ranges
-Whole blood clotting time is within expected range or prolonged
Hemophilia nursing care and patient education
-Management of bleeding in the hospital
-Administer injections via the subcutaneous route instead of the intramuscular route whenever possible.
-Avoid unnecessary skin punctures and use surgical aseptic technique.
-Venipunctures are preferred over finger or heel sticks for blood sampling.
-Monitor urine, stool, and nasogastric fluid for occult blood.
-Do not administer aspirin or any products that contain aspirin.
-Acetaminophen is an acceptable substitute for aspirin.
-Control localized bleeding.
-Administer factor replacement.
-Observe for adverse effects, which include headache, flushing, low sodium, and alterations in heart rate and blood pressure.
-Encourage the child to rest and immobilize the affected joints.
-Elevate and apply ice to the affected joints.
Patient Education:
-Teach parents to prevent bleeding at home.
-Environment should be made as safe as possible to prevent injury.
-Set activity restrictions to avoid injury.
-While participating in activities, children should wear protective equipment.
-Encourage the use of soft-bristled toothbrushes.
-Encourage regular exercise and physical therapy after active bleeding is controlled.
-Encourage the family to maintain up-to-date immunizations.
-Teach the importance of wearing medical identification.
-Teach manifestations of internal bleeding and hemarthrosis.
-Teach to control bleeding episodes using the RICE (rest, ice, compression, elevation) method.
-Encourage the family to participate in a support group