Equine Viral Diseases
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
•Species specific
•Three subfamilies: alpha, beta (none in horses), gamma
•9 documented strains, but only ___ affect domestic horses
•Only ___________commonly cause diseases in horses
Equine Herpes Virus
5
EHV1, EHV3 and EHV4
_________
a.Rhinopneumonitis (respiratory form)
b.Abortion
c.Birth of weak foals
d.Peracute vasculitis – lungs; fatal in adults
e.Neurological
1.EHV-1 (a) - Subtype 1 of EHV1
•__________ is common throughout the world and most important viral cause of abortion in horses
•Can be sudden and deadly
•High temperature
•_______ respiratory disease
•May see all 5 of the syndromes at once
•Horses of all ages are affected
•Mares_________pregnant most susceptible
•_________ first identified in the 1940s
EHV-1
“Fulminating”
3-9 months
Abortion storm virus
Mode of Transmission
•Horse to horse by direct contact, nasal secretion, reproductive discharge, placenta or aborted fetus
•Short-distance airborne spread also possible
Clinical Signs
•Viral incubation for__________
1.Fever (__________)
2.Malaise, depression, anorexia
3.Congestion and serous discharge from the nostrils
4.Swollen lymph nodes
5.Mild incoordination to severe ataxia, paresis and paralysis
6.Loss of bladder tone, tail tone, skin sensation in hind limbs
EHV1
2-10 days
38.8 to 41.6’C for 1-7 days
Diagnosis of EHV1
1.Fluorescent antibody, PCR
2.Virus isolation from fetal tissues
3.Differential diagnosis with ______and other resp dss
EI, EVA
Treatment of EHV1
1.Supportive nursing
2._____to control malaise and fever; will encourage eating
3.Fluid therapy if dehydrated
4.Antibiotics to prevent secondary bacterial infection (especially if respiratory disease); _______ 30mg/kg,PO, bid
5._____ to reduce nerve inflammation
•If horse remains standing, prognosis is _____
NSAIDs
Valacyclovir
Corticosteroids
good
Prevention of EHV1
1.Vaccination at ______month of gestation
2.Prevent exposure to other horses attending shows or other equine events
5, 7 and 9
2._____
•Venereal disease
•________
•Rare but important
•Doesn’t cause death
•Self-limiting
•Characteristic lesions on genitalia of stallions and mares
EHV-3
Equine Coital Exanthema
3.____
•Subtype 2 of EHV1
•Respiratory infection only (“Rhino”); ________
•Non-fatal, rarely results in abortion
•Severe, widespread outbreaks in young horses; foals → 3 years old in training
•Not a problem in older horses (develop immunity)
EHV-4
rhinopharyngitis and rhinotracheitis
4._____
•Gamma family
•“Ubiquitous” but rarely causes disease
•Found in nearly 100% of healthy foals
•Can cause problems in the following diseases:
1.EHV2 - _________ in young foals; may act as a forerunner that leads to Rhodococcal infection (through immune suppression)
2.EHV5–_____________; in middle-aged horses
EHV-2 and EHV-5
Herpetic keratoconjunctivitis
equine multinodular pulmonary fibrosis (EMPF)
•Has emerged as a pathogen (EMPF)
Clinical Signs
1.Tachycardia, tachypnea, increased inspiratory effort and poor body condition
2.Wheezing and crackling, maybe mistaken as _____
•Associated with lymphoproliferative diseases and lymphoma
EHV5
heaves
Diagnosis of EHV5
1. CBC – ________
2.Thoracic radiographs
3.Virus-specific PCR test on pulmonary secretions or percutaneous lung biopsy sample
•Prognosis for survival is approx. ___
neutrophilic leukocytosis with or without hyperfibrinogenemia and anemia
50%
Treatment of EHV5
1.___30 mg/kg, PO, tid and/or _____10ng/kg, IV in 1L of isotonic crystalloid fluid as infusion over 1 hour, bid for 2 days
2.____ – 5 to 10mg/kg, PO, 1-2 times daily; for 2ndary bacterial infection and anti-inflammatory properties
3. _____ – 0.08-0.1 mg/kg IV very 24-48 hours; reduction of pulmonary cytokines and inflammatory mediators; cause immunosuppression and enhance viral replication
Valacyclovir
acyclovir
Doxycycline
Corticosteroid
Diagnosis of EHV
•PCR and isolation of virus from nasopharygeal swabs and blood samples during early stage of infection
Treatment
• Anti-inflammatory drugs
•IV fluid
•Antibiotics for secondary bacterial infection
Prevention
•Vaccination
Control
•Biosecurity practices
•Arthropod-borne viruses that cause central nervous system dysfunction and moderate to high mortality
•Caused by alphaviruses of the family Togaviridae
•Endemic in North, South and Central America
•Western (WEE) - 20-50% fatal
•Eastern (EEE) - 50-90% fatal
•Venezuelan (VEE) - 50-75% fatal
•Highland J virus, Everglades virus
•Semliki Forest virus – East and West Africa
•Japanese encephalitis virus (JEE/Flavivirus) – Asia, India, Russia, Western Pacific – 35-45%
•Madariaga (MADV/Flavivirus) in South America and Caribbean
•WNV (Flavivirus) in Africa, Middle East, Europe, NSC Americas, Australia
Equine Arboviral Encephalomyelitis
Transmission of
1. ____
•Transmitted by mosquitoes; not horse-horse or horse-human; dead-end hosts
•Life cycle of alphaviruses between birds/rodents and mosquitoes
•Sylvatic cycle between passerine birds and _____
EEE
Culiseta melanura
Transmission
2.MADV principal vector belong to ____
3.WEE transmitted by ____
4.VEE in jungle or swampy areas; two life cycles, the ____ cycle “paddling”
a.Enzootic – mosquito (____) serves as primary vector for bird/rodent-mosquito life cycle; sylvatic rodents spiny and cotton rats
b.Epizootic – mutation to subtype I (A, B, C and possibly E) with change in mammalian pathogenesis
b.and several bridge vectors; horse infection becomes predominant feature in maintenance of epizootic ___
•All encephalitides caused by ____ transmitted by mosquito, Culex spp usually the most efficient
5. ____ – widest geographic distribution of all flaviviruses
Culex (Melanoconion) spp
C. tarsalis, Dermacentor andersoni
enzootic and epizootic
ci
VEE
Flaviviruses
WNV
Equine Encephalomyelitis
Clinical Signs:
•Neurologic signs occur____ days after infection
1.Quiet and depressed
2.Ataxia, wandering, impaired vision, reduced reflexes, circling, inability to swallow, drooling, fever
3.Paralysis usually followed by death ____days after onset of signs
9-11
2-3
Diagnosis of Equine Encephalomyelitis
1.Clinical assessment
2.CSF examination – in EEE with neutrophilic pleocytosis (count > 50%)
3.IgM capture ELISA – 85-90%; neutralizing antibodies gold standard (
____)
4.PCR – midbrain and brain stem
Treatment:
1.Supportive nursing care
2.Management of pain and inflammation
3. For WNV, _____1.1mg/kg, IV, bid to prevent muscle tremors and fasciculations
IgG
flunixin meglumine
Prevention of Equine encephalomyelitis
1. Core annual vaccination one month prior to mosquito season; formalin-inactivated whole viral vaccines
•Mares vaccinated ____ month before foaling
•With colostrum, foals vaccinated at ____ months plus 2 additional vaccinations 30 and 90 days after
•Zoonotic risks
1
5-6
•Highly contagious respiratory disease caused by Orthomyxovirus Influenza virus A/equine 2
•Subtyupes H7N7 and H3N8; ____spreads rapidly and cause severe clinical diases
•Horses ___ years most susceptible
•Endemic in many countries except New Zealand and Iceland
•Rarely fatal except in donkeys, zebras and debilitated horses
Equine Influenza
H3N8
1-5
Transmission of ____
•Incubation period < 48 hrs
•Morbidity 60-90%
•Mortality <1%
•Outbreak due to close contact
•Transmission by direct contact via nasal secretion or droplet infection
Clinical Signs
1.High fever up to 41.1’C
2.Harsh, dry cough
3.Loss of appetite
4.Depression
5.Watery nasal discharge
•Signs last <3 days; recovery in 2-3 weeks
•Virus replicates in respiratory epithelial cells resulting in destruction of tracheal and bronchial epithelium and cilia
Equine Influenza
Treatment of Equine Influenza
1.Fresh air, rest for 1-3 weeks
•Avoid dust
2.NSAIDs for fever above 40’C
3.Antibiotics to control secondary infection
Prevention:
1. Vaccination
•Most vaccines are effective against multiple strains
2.Hygienic practices
3. Isolation of newly acquired horses
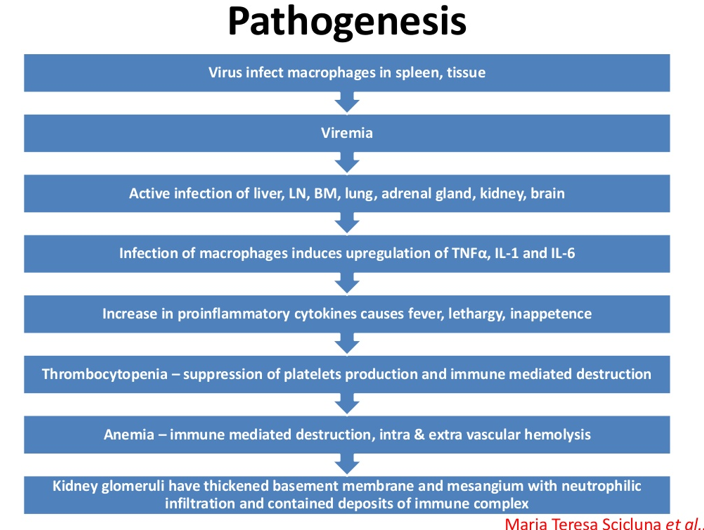
Equine Infectious Anemia
•_____, Coggins disease; non-contagious, infectious disease
•Caused by an RNA Lentivirus, Retroviridae
•____ are the only known natural host
•No treatment available to eliminate EIA from an infected horse
•Horses surviving EIA can
relapse and/or pass it on to
other horses
•Lifetime Quarantine
•Euthanasia
Transmission
•Blood from infected animal is source of infection
1.Mechanical transmission by Tabanus sp and Stomoxys calcitrans
2.Vertical transmission – in utero/colostrum feeding
3.Venereal transmission via semen
4.Iatrogenic – blood contaminated products
Mode of Transmission
•Blood from infected horses
•Blood-sucking flies, mosquitoes
•Needles
•Surgical instruments
•Dental floats
•Bridle Bits
“Swamp Fever”
Horses
_____
Clinical Signs
•Incubation period ____ days
1.Sudden onset of high fever of 40º - 42.2º C
2.Severe depression
3.Depressed appetite
4.Weight Loss
5.Weakness/incoordination
6.Jaundice
7.Ventral edema
8.Rapid destruction of red blood cells
EIA
15-45
Types of infection of EIA
1.____ – 1 to 3 days characterized by fever, depression and thrombocytopenia
2.____ - most common
•Similar symptoms to acute, but not as severe
•Death not as common
3. ____:
•Horses are unthrifty and lack stamina
•May have acute or subacute attacks
Acute
Subacute form
Chronic EIA
EIA - Diagnosis
1. _____
•Dr. Leroy Coggins of Cornell University
•Only 10 cc of blood is needed for the test
•Results can be available in 24 to 48 hours
•Most require a negative Coggins test for transporting horses, racing, breeding
•Most shows require negative Coggins test for participants
•Required negative Coggins for sales
2. ____
v
ELISA
______
•Vector-borne virus first in North America in 1999
•Caused by a Flavivirus
•Humans, horses, and birds are incidental hosts
•Wetland and terrestrial birds involved in natural cycle
•Routes of infection in man thru blood transfusions, organ donations, breastmilk, via placenta
•Many horses infected with WNV do not become ill
•Other symptoms: colic, lameness, anorexia, fever
•Approximately ___ die
West Nile Virus
33%
WNV
Prevention
1.Vaccination –95% control rate
2.WNV Antibody for horses already
infected (____, Inc.)
Control
•Mosquito control
•Eliminate standing water
•Mosquitoes can breed in as little
as an inch of water
Novartis Animal Vaccines
_____
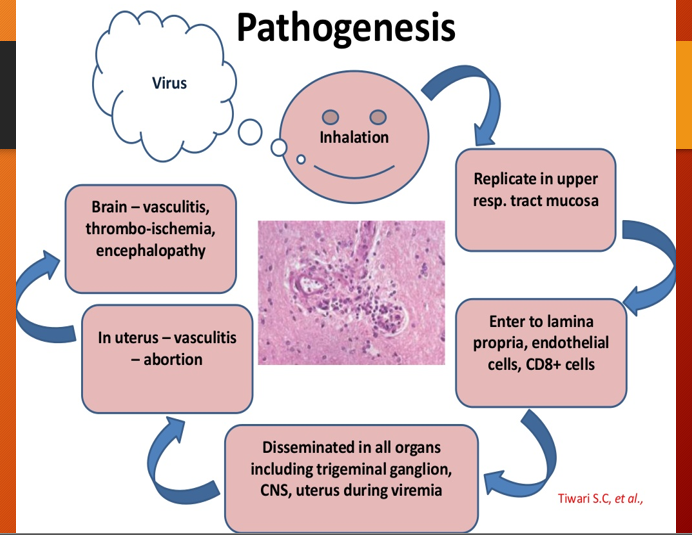
•Acute upper respiratory infection caused by an RNA Arterivirus, family Togaviridae
•Similar to influenza and rhinopneumonitis
•All age groups susceptible
•Most common in_____
•Degenerative and inflammatory changes in the endothelium
•Transmission:
1.Inhalation of droplets from infected horses
2.Ingestion
3.Venereal transmission by stallion
4.Tissues and fluids from aborted fetus
5.Shedding in the urine
Equine Viral Arteritis
Saddlebreds and Standardbreds
Clinical Signs of______
1.Fever (38.8-41.1ºF)
2.Nasal discharge
3.Can cause abortion (approximately
50%)
4.Edema of the limbs
5.Increased respiratory rate
6.Skin rash
Treatment
•Most animals recover without treatment
•Vet may prescribe antibiotics to prevent secondary infection
EVA
Prevention
•Vaccination
Control
•Sound management practices
Equine Viral Arteritis
____
•Neurotropic Lyssavirus, Rhabdoviridae
•Saliva of infected animal à horse
•Travels up the NERVES to the brain
•Reproduces in the brain
•Sheds virus through the salivary glands
•BLOOD TEST WON’T DIAGNOSE DISEASE
Symptoms:
1.Neurological disorder, choking, weakness, staggering, unprovoked excitement
2.Behavioral changes are most common
3.May take 2-6 weeks or even 3 months to show symptoms after infection
NO EFFECTIVE TREATMENT
Prevention - annual vaccination
•Problem in horses in the Mid-Atlantic where raccoon strain is predominant
Rabies
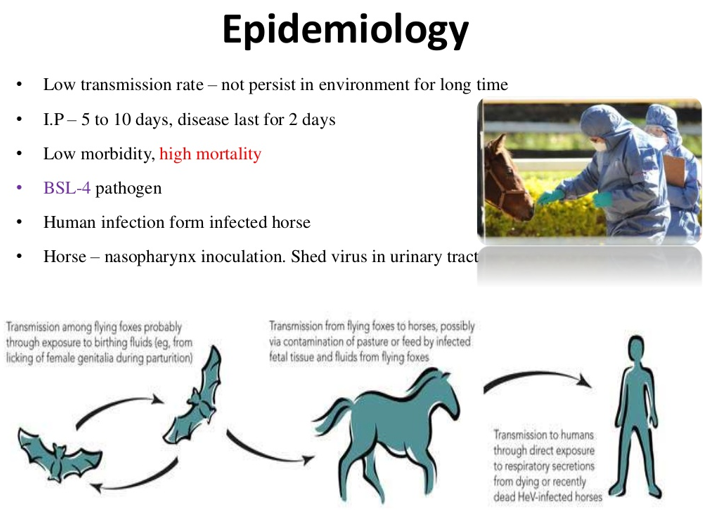
____ is prototype species of the new genus Henipavirus of the subfamily Paramyxovirinae
•A pleomorphic enveloped RNA virus
•First identified in Australia in 1994 as an acute respiratory disease in a Thoroughbred and a human
•Endemic in fruit bats or flying foxes of the suborder Megachiroptera, _____reservoir host and suspected to facilitate transmission of HeV to horses
•Classified as a biosafety ____ agent
•Horses only species naturally infected
•Zoonotic
•Infection via oro-nasal route and excretion via the urine, saliva, and respiratory secretions
Case fatality rate in horses and humans high
•Transmission in very close contact among horses and from horse to people
•Virus not considered highly contagious
•Equine veterinarians considered at occupational risk
Hendra Virus (Equine Morbllivirus)
Pteropus sp.
Level 4
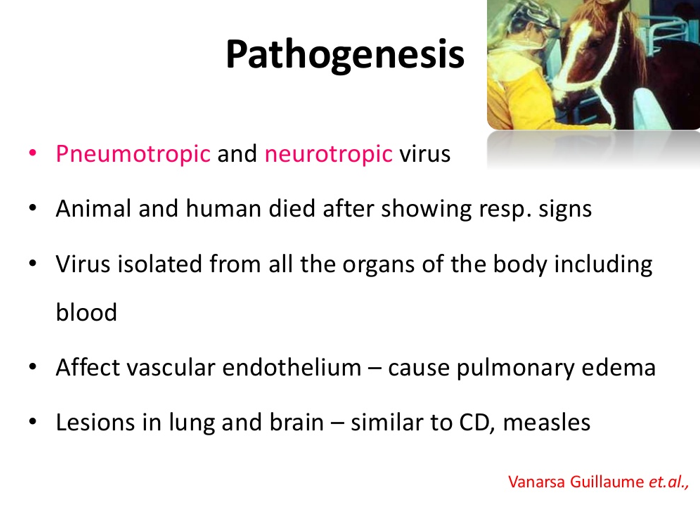
Clinical Signs of Hendra Virus
1.Severe and often fatal respiratory disease characterized by dyspnea, vascular damage, pulmonary edema, respiratory difficulty and frothy nasal discharge, jaundice
3.Depression
4.Anorexia
5.Fever
6.Ataxia
7.Tachycardia
Treatment
•Supportive treatment
•No specific treatment against the virus
Prevention
1.Commercial HeV vaccination available for release to veterinarians who have completed an online training program
•Horses must have microchip to be vaccinated
•Vaccine consists of soluble forms of G glycoproteins of HeV and does not contain modified or inactivated virus
2.In humans, prevent contact with infected horses and use appropriate personal protective equipment
African horse sickness