TV3001 PARA - pigs endoparasites
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
Ascaris suum
Location - SI
Lifecycle - Direct
Inf. stage - Embrionated eggs, very resistant
Inf. - Oral, ingestion of embryonated eggs
Strongyloides ransomi
Location - SI
Lifecycle - Direct
Inf. stage - L3, susceptible
Inf. - Oral, transcutaneous and milk
Isospora suis
Location - SI
Lifecycle - Direct
Inf. stage - Sporulated oocysts
Inf. - Oral, ingestion of sporulated oocysts
Trichuris suis
Location - LI
Lifecycle - Direct
Inf. stage - Embrionated eggs, very
resistant
Inf- Oral, ingestion of embrionated eggs
Oesophagostomum spp.
Location - LI
Lifecycle - Direct
Inf. stage - L3, moderately resistant
Inf- Oral, ingestion of L3
Hyostrongylus rubidus
Location - Stomach
Lifecycle - Direct
Inf. stage - L3, susceptible
Inf- Oral
Ascarops strongylina
Location - Stomach
Lifecycle - Indirect
Inf. stage - L3 inside coprophagous beetles (IH)
Inf- Oral, ingestion of beetles
Stephanurus dentatus
Location - kidneys
Lifecycle - direct
Inf. stage - L3, susceptible, earthworms are paratenic hosts
Inf- Oral, transcutaneous (with L3 only)
Metastrongylus spp
Location - Lungs
Lifecycle - Indirect
Inf. stage - L3 inside earthworms (IH)
Inf-Oral, ingestion of earthworms
Trichinella spp.
Location - Somatic musculature
Lifecycle - Direct
Inf. stage - L1 within the musculature
Inf- Oral, ingestion of flesh
important zoonosis
Cysticercus cellulosae (larval stage of Taenia solium that infects humans)
Location - Musculature
Lifecycle - indirect
Inf. stage - Eggs that contain an embryo with 6 hooks (hexacanth)
Inf- Oral, ingestion of eggs that contain hexacanths important zoonosis
Toxoplasma gondii
Location - Musculature , brain
Lifecycle - Indirect
Inf. stage - Sporulated oocystsCysts in musculature/brain
Inf- Oral, ingestion of sporulated oocysts and/or cysts (muscle). important zoonosis
Location -
Lifecycle -
Inf. stage -
Inf-
Intensive/Indoor/’all in-all out’ system
Slatted floor
All in - all outRelatively dry/clean environment (faeces do not accumulate)Regular anthelmintic treatments?
Monitor parasitic infections
No intermediate hosts
Dry, clean environment
Sows treated/washed before being brought to farrowing pen
Early weaning (3-4 weeks) parasite eggs do not have time to embrionate (A. suum)
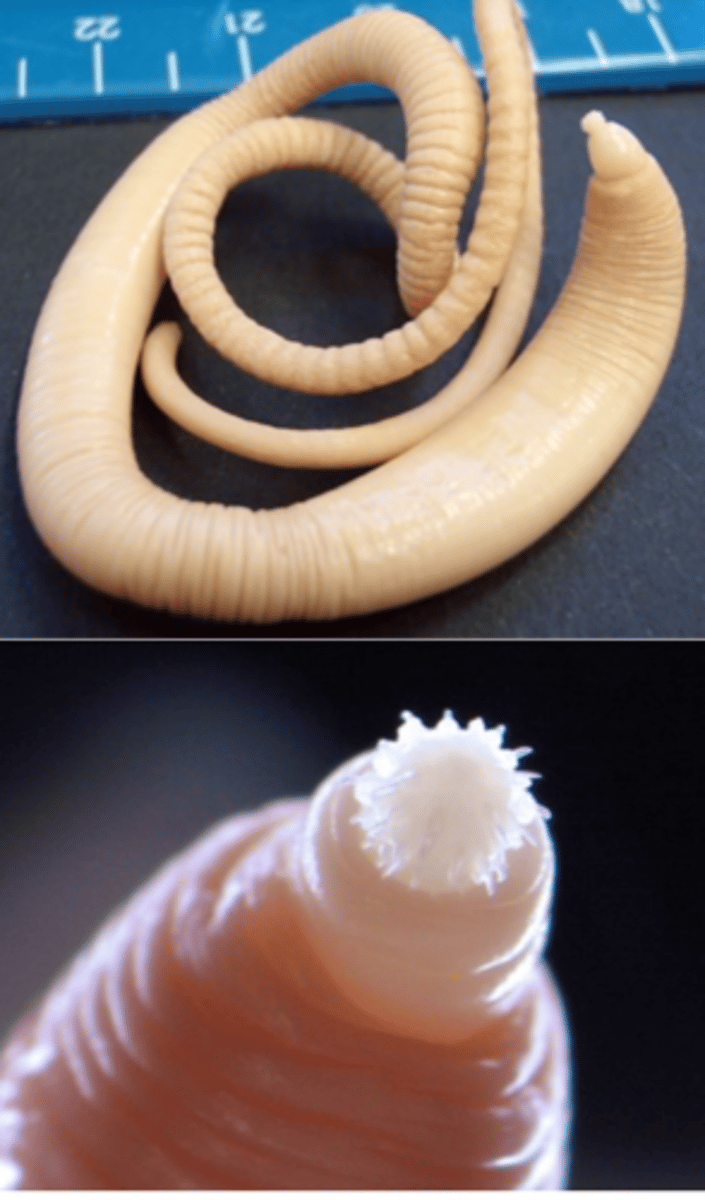
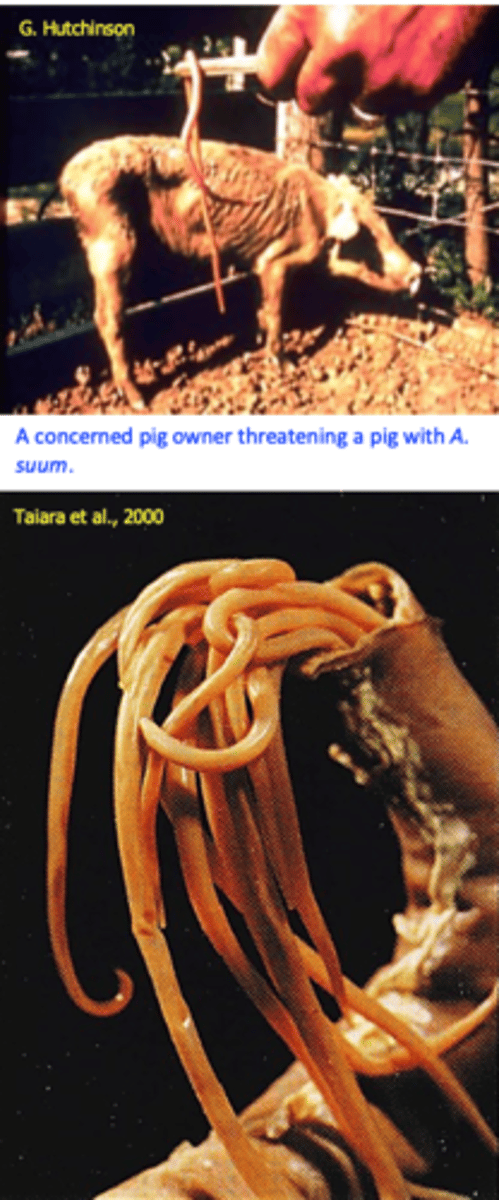
Ascaris suum info
The most important/common gastrointestinal worm parasite in pigs with prevalence of 50-75%;
Location: adult parasites in the small intestine but in heavy infections they may be found in the stomach, bile ducts etc;
Ascaris suum can infect and mature in humans
Stout-body,pinkish-yellow;
Three lips surround the mouth;
Prevalence highest in 2–6-month-old pigs
Diagnosis = Live animals with patent infections
NECROPSY = Presence of parasites in the small intestines and ‘milk spots’ in the liver;
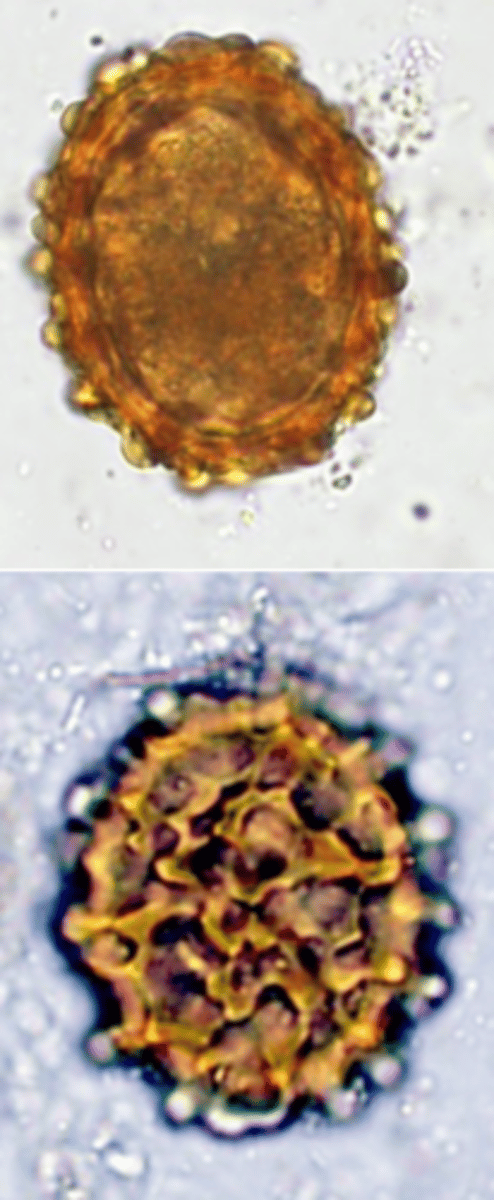
Ascaris suum eggs
Thick shell, yellow brown;
Mammilatedouterlayer:
One cell inside.
Survive long time in the environment (up to 6-9 years);
Resistant to usual disinfectants;
Sticky easily transported by pigs, equipment, worker’s boots, insects (cockroaches, flies), birds etc and get into the rough edges of the concrete material and are not easily removed;
Ascaris suum lifecycle
• Unembrinated eggs (not infective) are passed in the faeces;
Optimum temperature for development: 30-33C
At optimum temperature the infective larvae form inside the eggs in 13-18 days, at 18-20C they form in 30-40 days;
Eggs do not develop (but survive) at temp lower than 15C;
Larvae hatch in the intestine and migrate to liver -> heart -> lungs -> trachea -> pharynx -> small intestine (10-15 days PI) where they mature
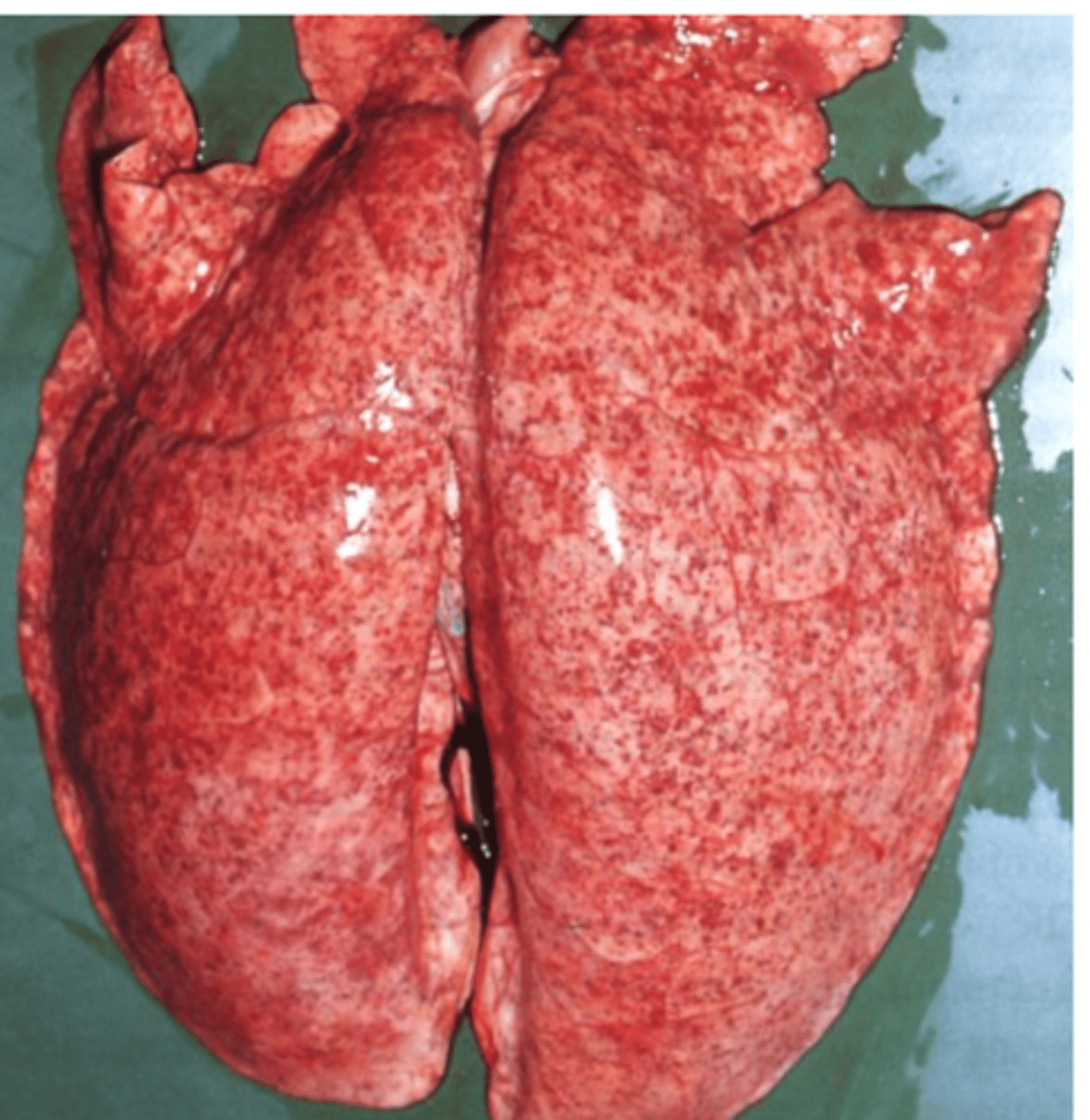
Ascaris suum pathogenesis
Larvae may produce lesions in the liver (milk/white spots) and lungs;
Adult worms cause lesions in the digestive tract;
Liver: milk/white spots (larvae) = Cloudy/whitish spots up to 5 mm in diameter on the surface of liver
Small hemorrhages into the alveoli and bronchioles,oedemainfiltrationof the surrounding pulmonary parenchyma with eosinophils and other cells lungs compromised by these lesions become more susceptible to other conditions
Small intestine (adult worms)
Compete with the host for nutrients retard growth;
Heavy infections → may block the gut;
Perforate the intestine peritonitis;
Immunogenic parasites
pigs continuously exposed acquire a high degree of resistance
Ascaris suum treatment
• Heterocyclic compounds
• Piperazine
• Benzimidazoles
• Fenbendazole • Flubendazole
• Imidazothiazoles
• Levamisole
• Tetrahydropirimidines
• Pyrantel
• Morantel
• Macrocyclic lactones
• Abamectin? • Ivermectin • Doramectin
Ascaris suum intestinal stages susceptible to:
Heterocyclic compounds
- Piperazine
Benzimidazoles
Fenbendazole (Safe-guard), Flubendazole (Flubenol)
Imidazothiazoles
–Levamisole
Tetrahydropirimidines
– Pyrantel, oxantel, Morantel
Macrocyclic lactones (MLs):
Ivermectin, Doramectin;
It is recommended to
Destroy the faeces collected 3-4 days after treatment (contain worms & eggs);
Improve hygiene to destroy eggs (clean floors, steam etc);
Suspected pneumonia
Levamisole, Fenbendazole, Ivermectin, Doramectin
Ascaris suum: Control
Treat boars 2-4 times/year;
Treat pregnant sows two weeks before farrowing;
Wash the sow carefully 4-14 before placing it in the farrowing pen;
Clean and disinfect the farrowing pen
Treat piglets 10-14 days before transfer to clean and disinfected fattening unit and 6 weeks later;
• Medicated food
Ring the snout of the sows
Strongyloides ransomi (suis)
Location: small intestine, embedded into mucosa;
Parasitic and free-living stages;
Parasitic stage: only females (less than 5 mm long);
Eggs: 45-55 μm/26-35μm, thin shell, contain a larva when laid;

Strongyloides ransomi lifecycle
Eggs reach the environment with faeces → larvae hatch and can follow
Homogonic development
Heterogonic development
Within host
After infection L3 can:
a) Mature to (partenogenetic) females in the SI
b) Enter hypobiosis;
Strongyloides ransomi: epidemiology
Present in outdoor and indoor systems;
Infections are prevalent in warm climates;
Infections can be found in all age categories but they are clinically significant in suckling pigs;
Sows are important sources of infection;

Strongyloides ransomi: clinical signs
May appear in pigs as young as 5-10 days
(infection via milk);
Diarrhea, dehydration, emaciation, anorexia, anemia etc;
Strongyloides ransomi: diagnosis
Clinical signs;
History (young age);
Finding eggs in the faeces;
Strongyloides ransomi: treatment and control
• MLs (Ivermectin, Doramectin) & Levamisole are effective chemicals;
Treatment of the sows with Ivermectin 3-16 days before parturition prevents transfer of the larvae via milk
Hygiene, cleaning the pens before farrowing

Macracanthorhynchus hirudinaceus
Location: small intestine of pigs (humans): a nodule is often present at the point of attachment to the small intestine;
Morphology (adult worms);
Size: up to 35 cm;
Proboscis provided with around 6 transverse rows of hooks;
Intermediate hosts: May beetles, dung beetles, water beetles
Nodular lesions that might be invaded by bacteria;
Perforation of the gut peritonitis;
Diarrhoea, weight loss etc;
Diagnosis
• Detection of eggs in the faece
Treatment
Ivermectin
Doramectin