Pressure Volume Loops
1/6
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
7 Terms
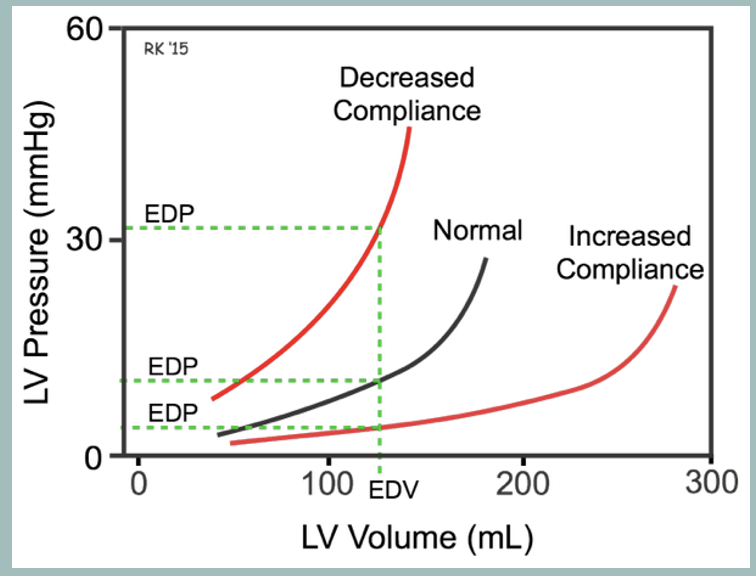
EDPVR
line that reflects the end-diastolic (minimal pressure) state of the heart.
generally a non-linear relationship and it is a measure of diastolic compliance and stiffness.
Not affected by HR
Inc. in preload causes PVL → the right along steeper portions of EDPVR
Indicates decreased compliance
Actual EDPVR may shift upwards or downwards causing a change in compliance regardless of LV volume
compliance is decreased → slope of the EDPVR will increase with an upward shift of the curve.
compliance is increased → slope of EDPVR will decrease with a downward shift of the curve
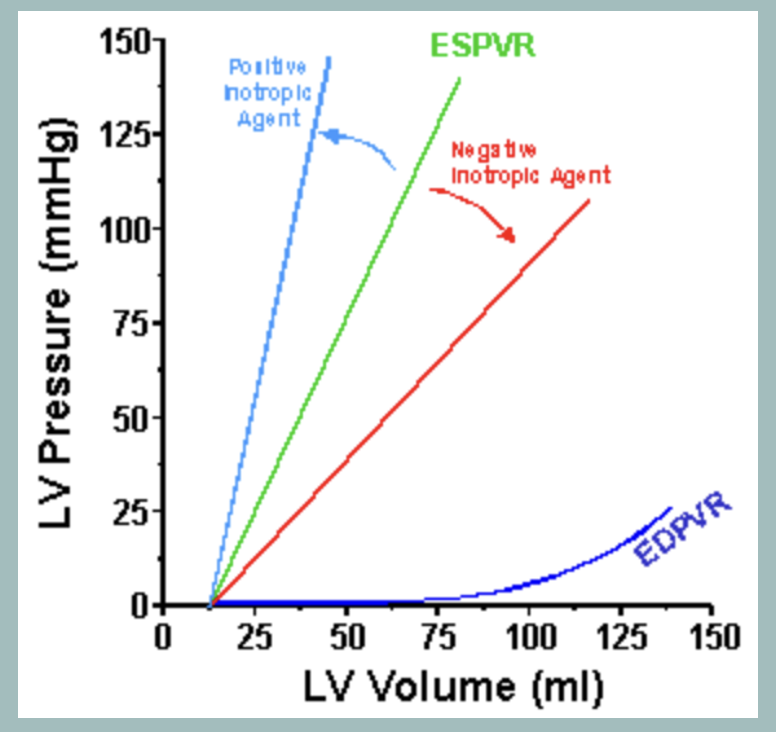
ESPVR
line that reflects the end-systolic (maximal pressure) state of the heart.
Generally a linear relationship.
ESPVR intersects the x-axis at V0.
It does not intersect the volume axis at zero because it requires at least a small amount of volume in the ventricle before any pressure can be generated
Changes in myocardial contractility will alter the slope of the ESPVR
Contractility improves (positive inotropy) the slope will increase with a shifting of the slope to the left.
Contractility decreases (negative inotropy), the slope of the ESPVR will decrease with a shifting of the curve to the right
Point at which the pressure volume loop contacts the ESPVR is called the Pes (pressure at end systole
Not affected by preload, afterload, or HR
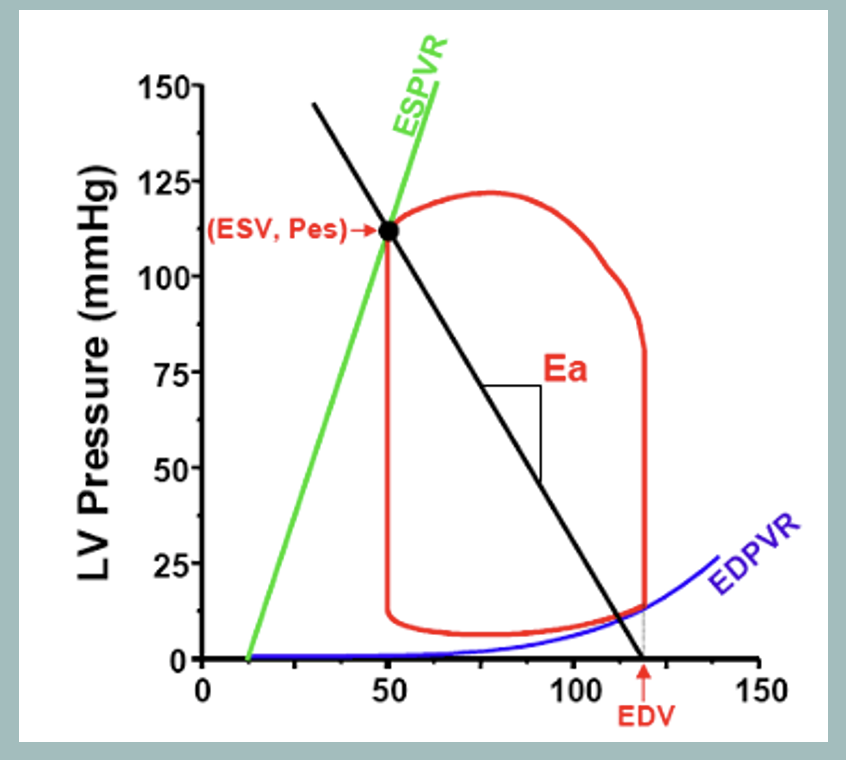
Ea / Arterial Elastance
Measure of total peripheral resistance and is depicted as a line that extends from end-systolic pressure (Pes) to the end-diastolic volume
Changes in total peripheral resistance change the slope of EA.
If total peripheral resistance increases→ the slope of EA will increase. This causes the end-systolic pressure to shift to the right along the ESPVR as we would expect with an increase in afterload.
Conversely, the slope of EA will decrease with a decrease in total peripheral resistance
Changes in contractility and preload (end-diastolic volume) do not affect the slope of EA but will alter the intersection points of the line
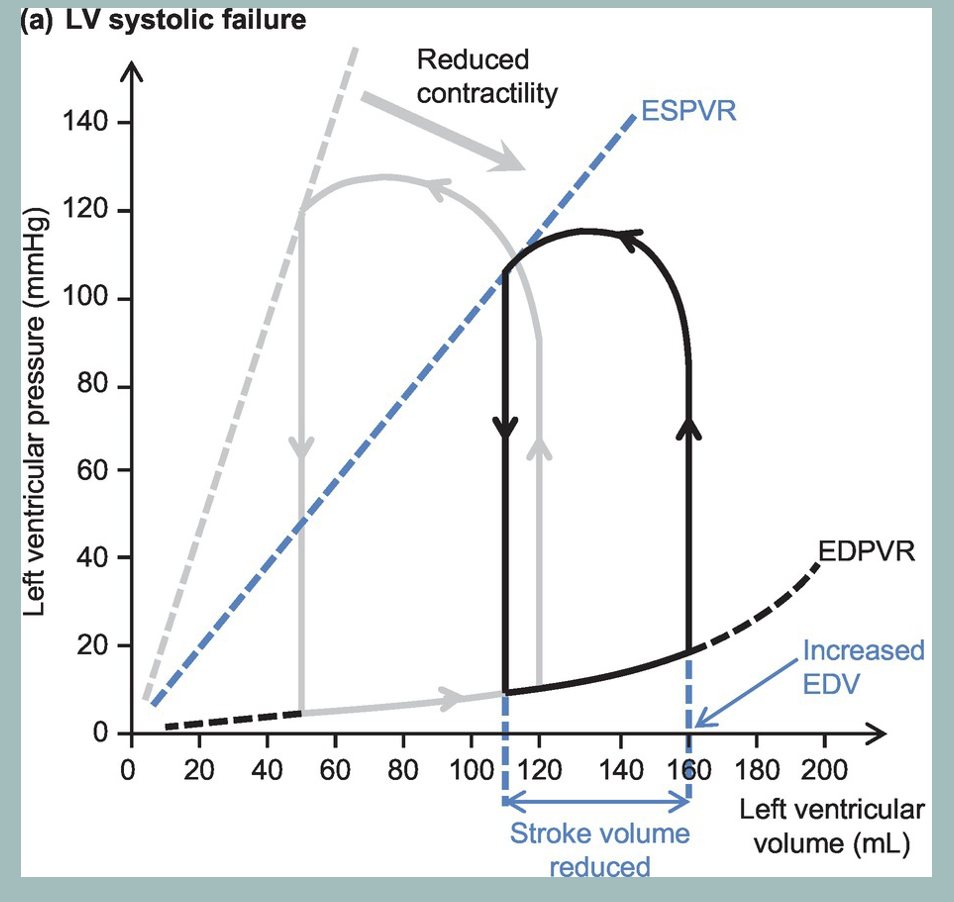
DCM/systolic dysfunction
loss in systolic function decreases the slope of the ESPVR. This shifts the pressure volume loop to the right (black loop). The result is an increase in end-systolic volume as well as an increase in end-diastolic volume (compensatory increase in preload). The increase in end-diastolic volume is not as great as the increase in end-systolic volume therefore the stroke volume decreases as does the stroke work (area within the loop).
With acute systolic dysfunction, there is no change in the EDPVR; however, with chronic systolic dysfunction the EDPVR relationship would shift downward and to the right as the ventricle responds by remodeling (anatomical dilation) which increases ventricular compliance (not shown in the diagram on the right).
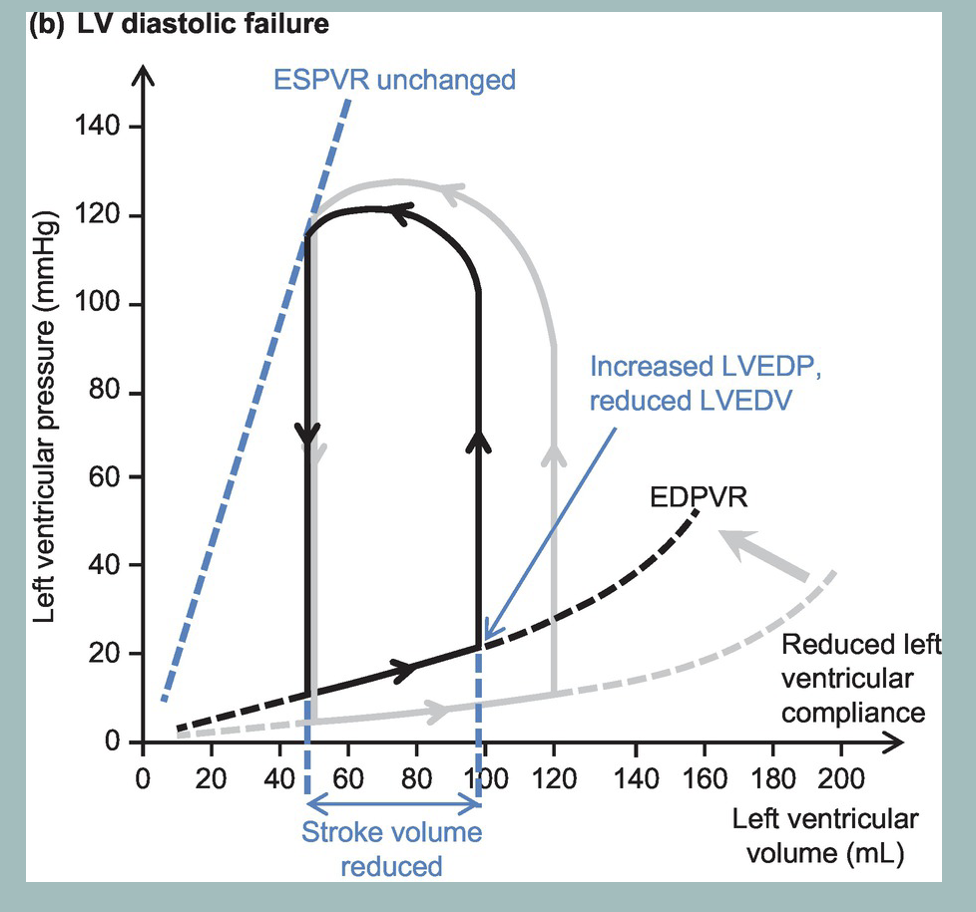
HCM/diastolic dysfunction
there is a reduction in ventricular compliance which increases the slope of the EDPVR. This shifts the pressure volume loop to the left (black loop). The result is a decrease in end-diastolic volume (less ventricular filling) and an increase in end-diastolic pressure. Stroke volume decreases and stroke work also decreases.
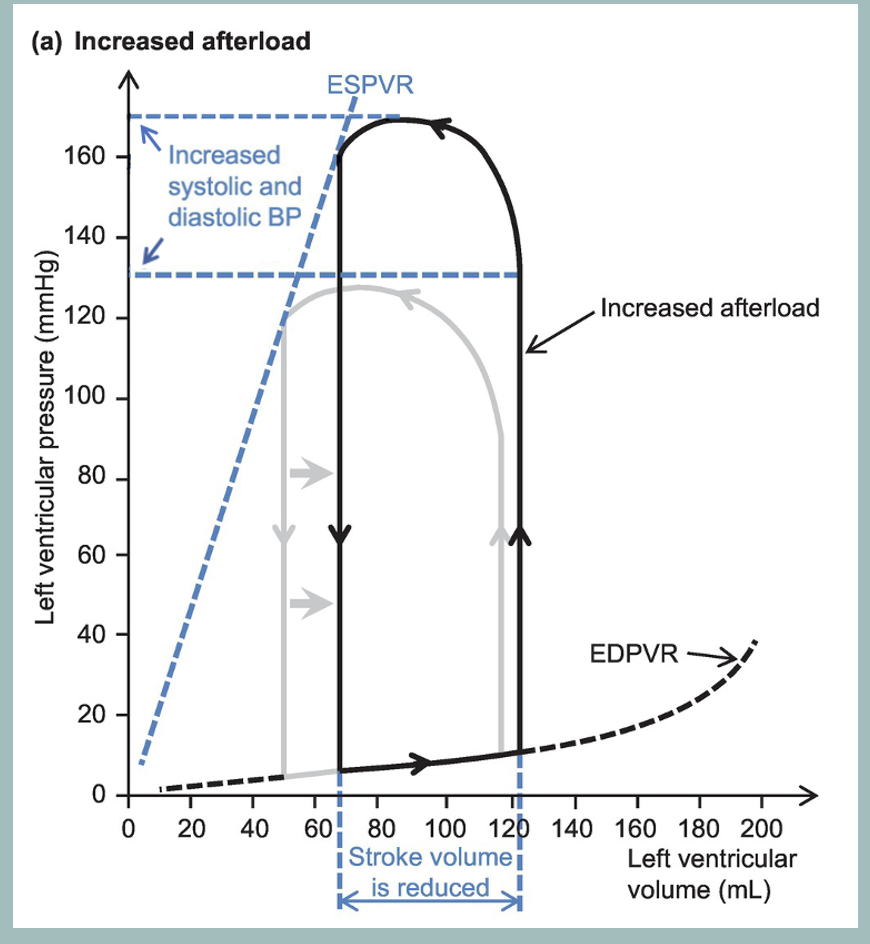
Aortic stenosis
an increase in afterload (rightward shift of the left limb).
obstruction causes a large pressure gradient to occur during ejection such that end-systolic pressure in the ventricle is greatly increased.
The impairment in left ventricular emptying results in an increase in end-systolic volume and a decrease in stroke volume.
Note that the shift in the loop will cause a dramatic increase in the internal work (potential energy) due to the energy spent increasing left ventricular pressure prior to ejection of blood
Mild increase in end-diastolic volume due to excess volume from increased end-systolic volume
Chronic HCM leads to decreased compliance/increase in slope of EDPVR + end-diastolic pressure