Allergic Conjunctivitis - Bansal
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
whats teh first thing you think ab w allergic conjunctivitis
itching
what are the 3 types of allergic conjunctivitis
vernal
atopic
seasonal perennial
define allergy
A type of hypersensitivity reaction in which the immune system will overreact to normally harmless substances
seasonal allergic conjunctivitis
OUTDOOR env
pollen
tend to peak in the spring and summer of ea year
Perennial allergic Conjunctivitis
INDOOR allergens
dust mites, pet or pest dander, feathers, fungi, and mold
seasonal/perenial conj pathophys
Type I Hypersensitivity rxn
• After exposure- IgE forms in the body and binds to Mast Cells - these release histamine
• Wait for activation when in contact with allergen present
the more you rub the more histamine you release
signs/symptoms of Seasonal/Perennial Conjunctivitis
• Generally Bilateral
• Itching - esp in medial canthus, redness, clear watery discharge, puffy eye lids,
inferior papillae
antihistamines/mast cell stabilizers moa
- inhibits histamine receptor and stabilizes mast cells
how do we treat seasonal/perennial conj
• Pataday 0.7% 1 gtt once a day
• Oral- Non sedating antihistamines such as Zyrtec, Claritin and Allegra
why do we use something cold w Seasonal/Perennial Conjunctivitis
slows the blood down
so use a refridgerated artificial tear along w antihistamine
what do we use to treat severe Seasonal/Perennial Conjunctivitis
Add Loteprednol 0.2% QID x 1-2 weeks with taper after
• SHOULD monitor IOP to rule out steroid response
• MOA- binds to glucocorticoid receptors suppressing release of inflammatory mediators
whats the eye side effect w a steroid
inc IOP
if you catch a pt w a inc pressure from steroid …
they have over a 90% chance of getting primary open angle glaucoma
Vernal Keratoconjunctivitis epi
Generally, begin before the age of 10 and last 2-10 years
- resolves during puberty.
usually affects more young males
SEASONAL
symptoms of Vernal Keratoconjunctivitis
Severe itching, redness, tearing, and photophobia
signs of Vernal Keratoconjunctivitis
thick ROPY mucous discharge
large papillary reaction = cobblestone
shield ulcer (convex)- epi erosion formed from superior tarsal inflammation
if not reated will form a plaque fibrin and mucus
you got to debride this
shield ulcer blocks wound form healing
trantas dots - accumulated eosiniophil and epithelium toward the limbus
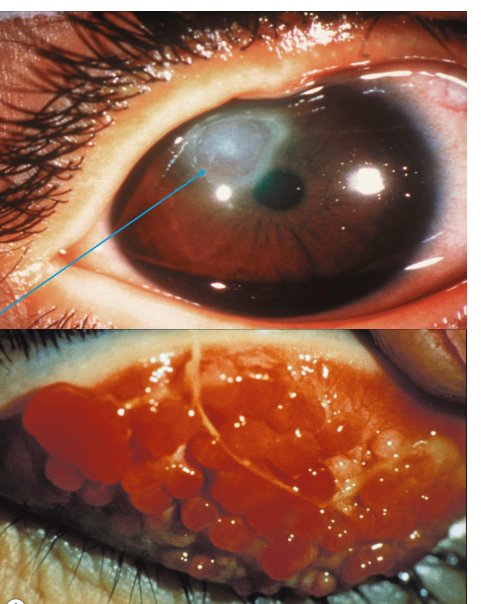
what this
trantas dots
accumulated eosiniophil and epithelium toward the limbus
whats pathaneumonic for Vernal Keratoconjunctivitis
trantas dots
how do we treat Vernal Keratoconjunctivitis
cool compress/ refridgerated artificial tears
• Antihistamine/Mast Cell Stabilizer
• Pataday 0.7% 1 gtt QD
severe - steroid
Loteprednol 0.2% QID x 1-2 weeks
how do you treat a shield ulcer from Vernal Keratoconjunctivitis
• May need to be removed/scraped prior to treatment,
• Add antibiotic gtt- ofloxacin QID or polytrim ung 3-4 times per day •
Could add cyclopentolate for pain
dilates by paralyzing CB — most pain comes from CB
• Follow up every 2-3 days if present otherwise, every few weeks
Atopic Keratoconjunctivitis
Chronic BILATERAL conjunctival and lid inflammation due to allergic conditions
• Mass cell and eosinophil activation- Type I and Type IV hypersensitivity rxn

epi of Atopic Keratoconjunctivitis
Generally, between 2nd -5 th decade of age
symptoms of Atopic Keratoconjunctivitis
Severe itching, redness, tearing, and photophobia,

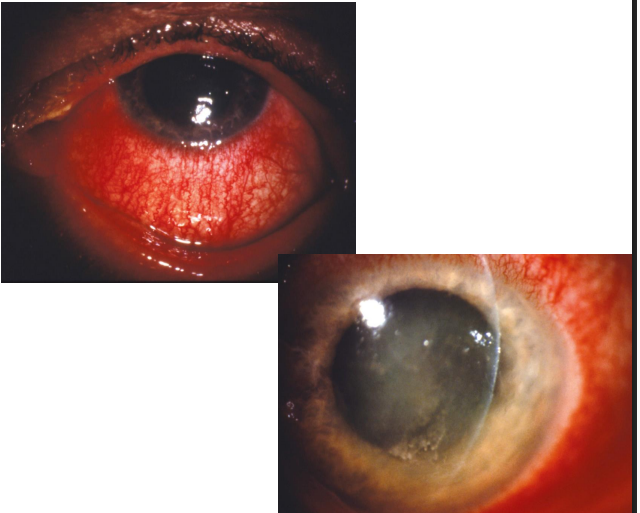
signs of atopic keratoconjunctivitis
Mucus/watery discharge, scaly lids/dermatitis, inf papillae, hyperemia

how do we treat Atopic Keratoconjunctivitis
• Antihistamine/Mast Cell Stabilizer
• Pataday 0.7% 1 gtt once a day
• If severe- steroid treatment
• Add Loteprednol 0.2% QID x 1-2 weeks
• Cool compresses/refrigerated artificial tears
• If there is atopic dermatitis of the lid
• Consider tacrolimus .03% ung QHS or BID
• Topical steroid ung- fluorometholone 0.1% QID to the affected area for 1- 2 weeks

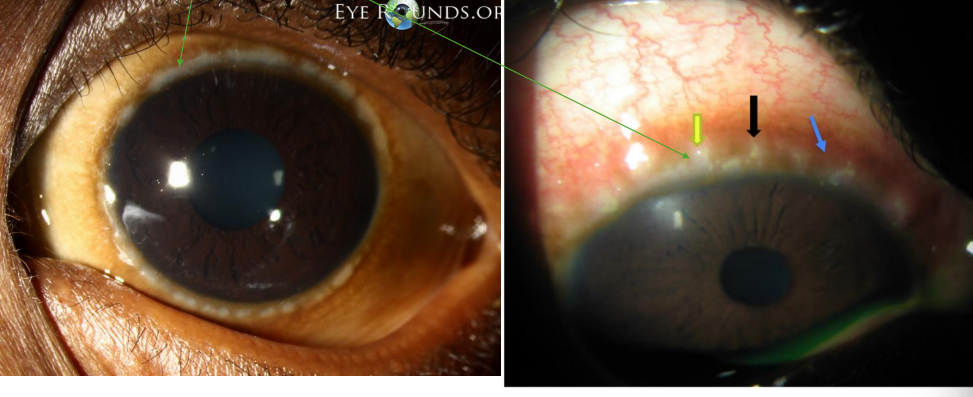
what this
atopic dermatitis
giant papillary conjunctivitis
• Non-infectious inflammatory condition of the superior tarsal conjunctiva with the presence of “giant papillae” (papillae greater than 1 mm in diameter)
Thought to be mechanical trauma and inflammatory in the presence of CL antigens
if contact lens doesnt fit you get friction w superior palpebral conj

symptoms of giant papillary conjunctivitis
• FBS, itching,
signs of giant papillary conjunctivitis
• Large papillae superior palp conj greater than 1mm

treatment of giant papillary conjunctivitis
• Replace/refit lens- daily wear would be best
• If severe:
• Discontinue lens wear
• Loteprednol 0.2% QID x 1-2 weeks
• Antihistamine/mast cell combo gtt
• Refit lens once clear
• Follow up in 2-4 weeks
• Can resume CLs once resolved
Toxic Conjunctivitis/ Medicamentosa signs/symptoms
• Hyperemia
chemosis
lid or periorbital swelling
mucous discharge
follicular palpebral conjunctival reaction
and itching
toxicity in Toxic Conjunctivitis/ Medicamentosa is
- Damage to tissues of ocular surface, could be due to the drug itself, preservatives within, or breakdown products of the drug
treatment of Toxic Conjunctivitis/ Medicamentosa
recognition is KEY
• Cessation of offending agent
• Cool compresses/refrigerated Ats
• Can add a soft steroid such as Loteprednol 0.2% QID with a taper
what does he really hate bc it causes follicular palpebral conjunctival reaction, and itching due to a rebound reaction
Lumify (brimonidine)
what meds can cause potential toxic agents
Gentamycin
Brimonidine
neomycin
amphotericin B
atropine
pilocarpine
apraclonidine