Silverstein and Hopper Chapter 39: Ventilator-Induced Lung Injury + Hess Chapter 3: Ventilator-Induced Lung Injury
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
Ventilator-Induced Lung Injury (VILI)
Injury to the lung caused by mechanical ventilation in experimental models
Ventilator-Associated Lung Injury
Worsening of pulmonary function, or presence of lesions similar to ARDS in a clinical patient that is thought to be associated with the use of mechanical ventilation, with or without underlying lung disease
Barotrauma Description
Extraalveolar air
Pneumothorax
Pneumomediastinum
Subcutaneous emphysema
Barotrauma Preventative Strategies
Minimize plateau airway pressure
Target <30 cm H2O
Volutrauma Description
Overdistension causing stretch injury
Volutrauma Preventative Strategies
Minimize TV
Target TV <10 ml/kg
Atelectrauma Description
Cyclic recruitment - derecruitment injury
Atelectrauma Preventative Strategies
Application of PEEP
Mechanical Power Description
Total energy transferred to the lung - includes TV, driving pressure, respiratory rate, flow rate, and PEEP
Mechanical Power Preventative Strategies
Minimize all ventilator settings - all energy transferred to the lung has the potential to cause injury
Spontaneous Breathing while Receiving Mechanical Ventilation Description
Alveolar distension, shear stress, atelectrauma, etc., during spontaneous breathing is equally as injurious as mechanical ventilator breaths.
May promote edema formation more than positive pressure ventilation
Spontaneous Breathing while Receiving Mechanical Ventilation Preventative Strategies
Minimize spontaneous breathing including patient-ventilator asynchrony with appropriate sedation, optimization of ventilator settings ± neuromuscular blockade
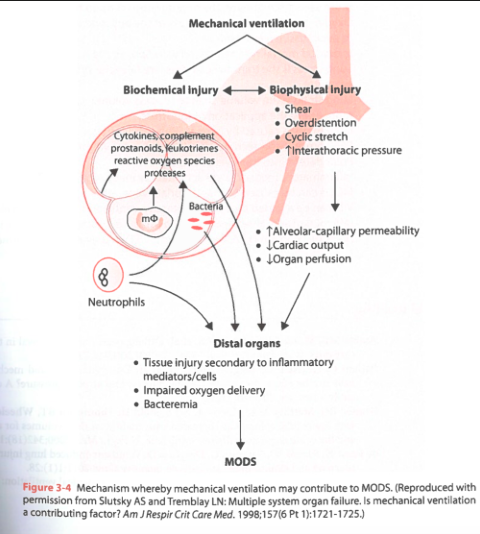
Biotrauma Description
Release of inflammatory mediators from the injured lung leading to systemic inflammation, which may promote multiple organ dysfunction
Biotrauma Preventative Strategies
Lung-protective ventilation strategies to limit lung injury and implement strategies to reduce microaspiration of oropharyngeal fluid
Oxygen Toxicity Description
High oxygen concentrations may directly cause lung injury as well as contribute to absorption atelectasis
Oxygen Toxicity Preventative Strategies
Minimizing FiO2 within 24 hours
Target FiO2 <0.60
Barotrauma
Barotrauma implies pressure-related injury to the lung
In terms of VILI, barotrauma is defined as extraalveolar air and is manifested clinically by pneumothorax, pneumomediatstinum, or subcutaneous emphysema
Disruption of the alveolar capillary membrane allows air to dissect along facial planes, accumulating within the pleural space or other compartments, or the development of subcutaneous emphysema
What was associated with a higher incidence of pneumothorax in human ARDS patients?
In a study of human ARDS patients, the use of high airway pressures (peak inspiratory pressure >40 cm H2O) was associated with a higher incidence of pneumothorax than when lower airway pressures were used
In another study, when plateau pressure was maintained at less than 35 cm H2O, no relationship was found between ventilator setting and the occurrence of pneumothorax
When does barotrauma occur?
In lungs ventilated with high alveolar pressures and large tidal volumes (VT)
Evaluation of what pressure is best to assess risk of VILI?
Airway pressure may not accurately reflect the stress imposed on the lung parenchyma as it includes the pressure needed to expand the chest wall
The distending pressure of the lung is best reflected by the transpulmonary pressure and this would be a better measure to use when assessing the risk of VILI
Volutrauma
Results in an increase in the permeability of the alveolar capillary membrane, the development of pulmonary edema, the accumulation of neutrophils and proteins, the disruption of surfactant production, the development of hyaline membranes, and a decrease in compliance of the respiratory system
Stretch injury as a result of high volume is more injurious to the lung than high pressure, without a large increase in volume
In a study, rats were ventilated with either high volume/high pressure, high volume/low pressure (negative pressure ventilation), or low volume/high pressure (chest wall was restricted)
Both high-volume strategies caused substantial lung injury while the low volume/high pressure strategy had far less evident injury
Concerns for volutrauma are supported by human clinical studies showing improved outcomes with use of low tidal volume ventilation
Chest Wall Effects on Volutrauma
Alveolar distension is determined by the difference between alveolar and pleural pressure so the chest wall has a role in determining the extent of overdistension
When the chest wall is stiff (low compliance) or heavy, a high Pplat may be associated with less risk of overdistension
A stiff or heavy chest (e.g. obesity, abdominal distension, massive fluid resuscitation, chest wall deformity, chest wall burns) protects the lungs from VILI
Effect of Active Breathing Efforts on Volutrauma
The alveolar distending pressure can change markedly on a breath-by-breath basis in a spontaneous breathing patient
When the airway pressure is constant and the patient forcefully inhales, the alveolar distending pressure may exceed what is expected by the airway pressure setting
During pressure-targeted ventilation, the contribution of patient's effort to alveolar distending pressure must be appreciated
Dependent pleural pressure changes can exceed the average measured pleural pressure due to in pendelluft, movement of gas from one part of the lungs into another during inspiration but without increasing overall tidal volume
Causes local distension and an increased risk of VILI
Avoid excessive patient effort regardless of mode of ventilation
Effect of Preexisting Injury of Development of VILI
Increases the likelihood of VILI
Two-hit process of lung injury
Previous injury predisposes the lungs to a greater likelihood of ventilator induced injury
Atelectrauma
Atelectrauma or cycle recruitment-derecruitment injury - trauma to epithelial cells and injury to adjacent alveoli via shear stress from repetitive opening and closing of collapsed alveoli
In healthy lungs, there are relatively few collapsed alveoli, but in injured lungs, alveoli become progressively unstable, changing shape during inflation and completely collapsing at the end of expiration
The junction between an open and a closed alveolus serves as a stress raiser
When rats are ventilated with high pressures and no PEEP, the rapidly develop severe, diffuse pulmonary edema
If they are ventilated at the same pressure with the addition of PEEP, it is far less injurious
PEEP can reduce the cyclic collapse and reexpansion of alveoli and minimize atelectrauma
Mechanical Power
The total mechanical power or energy transferred to the lung during ventilation may correlate with the likelihood for VILI
It is recommended that the mechanical power is normalized to the area of ventilated lung available
This normalized value for mechanical power has been described as intensity
In lungs with smaller areas participating in ventilation, the value for intensity for a given degree of mechanical power would be higher
A novel aspect of this approach is the inclusion of respiratory rate and PEEP as potential contributors to VILI
PEEP can be protective of lung injury, but does increase the energy load transmitted to the lung and may contribute to VILI in some circumstances
What does mechanical power include?
Mechanical power includes all components of a ventilator breath that can contribute to VILI
Tidal volume
Driving pressure
Respiratory rate
Flow rate
PEEP
What are the primary determinants of lung injury?
Stress and strain
Stress
The internal counterforce per unit area that balances an extern load on a structure, or the pressure gradient across a structure (e.g. alveolar capillary membrane)
Strain
Deformation of the system as a result of the external load or the change in size or shape of the structure (alveolar distension)
What are stress and strain from a pulmonary perspective?
Stress is the alveolar distending pressure (alveolar pressure minus pleural pressure) and strain is the ratio of volume change (VT plus volume increase caused by PEEP) to functional residual capacity (FRC) during the application of the stress
What lung strain is considered injurious to the lungs?
Lung strain of more than 2 (i.e. double the resting lung volume)
How are lung stress and strain related?
Stress and strain are related by the specific lung elastance of 12 cm H2O
Lung stress is 12 cm H2O times lung strain
Surrogates for stress and strain are plateau pressure (Pplat) and VT
Spontaneous Breathing and VILI
Mechanisms of VILI are a product of the dynamic stress applied to the lung during breathing efforts and this stress can be equally injurious if breaths are generated by mechanical ventilation or spontaneous respiratory efforts
The decrease in pleural pressure as a result of spontaneous breathing efforts increases transvascular pressure (the transmural pressure of pulmonary vessels)
Then there is distension of the vessels which can promote the formation of edema
These concerns are relevant to spontaneous breathing modes, in addition to animals with patient-ventilator asynchrony
Biotrauma
VILI causes cell damage and results in an inflammatory response
The release of proinflammatory cytokines caused by VILI may promote multiple organ dysfunction and increased inflammatory cytokines can worsen VILI in a circular fashion
Pro-inflammatory and anti-inflammatory mediators increase edema formation, neutrophil migration, and relaxation of vascular smooth muscle
The morbidity and mortality associated with VILI, from any mechanism, are largely the result of the subsequent systemic inflammation known as biotrauma
Lung-protective ventilation strategies limit lung injury and have been shown to reduce multiple organ dysfunction and improve outcomes
Oxygen Toxicity
Patients receiving PPV are invariably on supra-atmospheric levels of oxygen supplementation
This may have an additive effect to the injury caused by VILI, especially if a high oxygen concentration is delivered for an extended period
Inspired oxygen concentration of 100% in the short term can cause absorption atelectasis and decreased oxygen diffusion capacity
Beyond 24 hours, an FiO2 between 50-100% promotes the production of reactive oxygen and nitrogen species and causes pathologic changes similar to ARDS and VILI, including interstitial edema, hyaline membrane formation, damage to the alveolar membrane, altered mucociliary function, and fibroproliferation
The damage appears to be positively associated with the level of FiO2 and the length of time that oxygen was administered
Laboratory data suggest that former exposure to bacterial endotoxin, inflammatory mediators, and sublethal levels of oxygen (less than or equal to 85%) protect the lungs from further injury when inspiring a high FiO2
Combination of bleomycin and oxygen results in marked injury to the lungs
In this setting the lowest FiO2 should be used, tolerating a PaO2 as low as 50 mm Hg (SpO2 85-88%)
What FiO2 should be administered whenever there is uncertainty about the PaO2?
1
What should the target PaO2 when adjusting FiO2 be?
FiO2 should be lowered to the level resulting in a PaO2 of 50-80 mmHg (SpO2 88-95%) as soon as possible
What is the target FiO2 in the mechanically ventilated patient?
Less than or equal to 0.50
Translocation of Cells and VILI
Leakage of inflammatory mediators into the bloodstream increases systemic inflammation
Bacteria instilled into the lungs of otherwise healthy animals produce bacteremia when inappropriate respiratory patterns are employed
Other Mechanisms of VILI
Higher vascular infusion volumes, rapid respiratory rates and inspiratory flows, and high body temperature potentially cause greater injury
Histopathology Associated with VILI
Histopathologic changes associated with VILI are hard to distinguish from changes associated with ARDS
Include decreased integrity of small airway epithelial cells, destruction of type 1 alveolar epithelial cells, alveolar and airway flooding, hyaline, membrane formation, interstitial edema, and infiltration of inflammatory cells
Lesions usually have an uneven distribution but tend to be worse in the dependent lung, likely because of worsened airway flooding and shear injury
VILI and MODS
Disruption of the alveolar-capillary membrane allows leakage of pulmonary inflammatory mediators into the bloodstream, allowing downstream organ failures
Low Tidal Volume Ventilation
Growing evidence that high-volume/low-PEEP ventilation can cause harm and worsen preexisting lung injury
Volume limitation in patients with ALI and ARDS has shown the most dramatic results in outcome, with the landmark ARDSnet study showing a decrease in mortality when 6 ml/kg tidal volume was used vs 12 ml/kg
The group receiving lower tidal volumes also, incidentally, received slightly higher PEEP and inspired oxygen concentration
Evidence that low tidal volume ventilation may be of benefit in people without ARDS or ALI
Meta-analysis of intraoperative ventilation concluded that low tidal volume (<10 ml/kg) ventilation decreased the frequency of pneumonia and the need for postoperative ventilatory support
Lung Protective Ventilation Strategy
Limits tidal volume to 4-8 mL/kg
Maintains plateau pressure less than 28 cm H2O
Maintains driving pressure less than 15 cmH2O
Sets PEEP based on the patient's pathophysiology and respiratory mechanics
Provides a FiO2 that maintains the PaO2 between 55 and 80 mmHg and SpO2 between 88 and 95%
Low Tidal Volume Ventilation to Prevent VILI
There is strong evidence for limiting tidal volume to less than normal in human studies, where values of 4-6 ml/kg have been recommended in ARDS patients
Optimal target for tidal volume in dogs and cats is unknown and likely varies between breeds due to anatomical differences
Most clinical veterinary studies on mechanical ventilation have reported the use of tidal volumes of greater than 10 ml/kg
Recommended to target the lowest possible tidal volume needed to maintain adequate blood gases, likely to be in the range of 6-12 ml/kg in dogs and cats
Healthy dogs have a higher normal tidal volume than other species, but the volume of functional units available for gas exchange in injured lungs may be much reduced
Inflammation in the lung causes heterogenous changes throughout, with regions of poorer compliance and atelectasis, which causes more compliant regions to become overdistended
Limit tidal volume to prevent portions of the lung from being overdistended
Low tidal volume increases the risk of perpetuating atelectasis and creating further shear injury so application of PEEP is vital
What is a common consequence of low tidal volume ventilation?
Hypercapnia
Permissive hypercapnia - tolerating higher than normal PaCO2 levels rather than increasing ventilator settings
This approach may reduce the likelihood of VILI, but there are physiological consequences of hypercapnia that may impact patient outcome
Positive End-Expiratory Pressure to Prevent VILI
Well established that some PEEP is better than no PEEP or zero end-expiratory pressure
Minimum amount of PEEP needed to reduce VILI has not been established
Common levels of PEEP considered adequate in human medicine are in the range of 5-10 cm H2O
Limitation of Plateau Pressure to Prevent VILI
Plateau pressure best represents the pressure applied to the lung as it is not impacted by resistance of the system
Measured during an inspiratory hold maneuver and the animal should not be making active respiratory efforts during measurement
The combination of high PEEP, auto PEEP (PEEP created by increased outflow resistance during expiration, asynchrony, or incomplete expiration), and tidal volume can lead to high end-inspiratory volume, which may be indicated by high plateau pressure
Protective lung ventilation strategies in human medicine recommend targeting a plateau pressure of less than 30 cm H2O
Peak inspiratory pressure may be used as a surrogate for plateau pressure unless there is increased resistance in the system
Respiratory Rate and Inspiratory Flow to Prevent VILI
Some evidence that high respiratory rates and inspiratory flow rates can promote VILI
Subjective Analysis of the Pressure Volume Loop to Prevent VILI
An optimal ventilator breath avoids both alveolar collapse on exhalation and overdistension on inhalation
The upper and lower inflection points of the pressure-volume loop theoretically show where these events occur and maintaining PEEP and peak inspiratory pressure between these points could be beneficial
Subjective analysis of the pressure-volume loop may be of some benefit, in particular recognition of overdistension from the presence of "beaking"
Recommendations for Spontaneous Breathing to Prevent VILI
In severe ARDS, spontaneous breathing effort has been associated with poorer outcomes, while in less severe pulmonary disease, spontaneous breathing may actually provide benefits such as better lung recruitment and improved diaphragmatic tone
A recent human clinical practice guideline recommended against the routine use of NMBA in patients with moderate or severe ARDS that tolerate light sedation
In patients that require deep sedation or prone ventilation, the use of NMBA is reasonable
Advanced Pulmonary Support Techniques to Prevent VILI
Advanced strategies such as partial liquid ventilation, high-frequency oscillatory ventilation, extracorporeal membrane oxygenation, and carbon dioxide removal are being researched to look for strategies with lower risk of VILI than conventional mechanical ventilation