FOM Week 16 LEC 136-146
1/235
Earn XP
Description and Tags
Each question labeled with lecture # (E.g. 138). Check out Amaya's Knowt Deck for Cranial Nerve facts: https://knowt.com/flashcards/77dd97c7-875d-42b1-84ab-8d05714e18a6
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
236 Terms
(138) Example of Medical Diagnosis
Chronic diastolic heart failure, Bilateral lower extremity lymphedema
(138) Example of Osteopathic Diagnosis
somatic dysfunction of thoracic region, somatic dysfunction of the pelvic region
(138) 10 body regions for Osteopathic regional diagnoses
Head, Cervical, Thoracic, Ribs, Lumbar, Sacrum, Pelvis, Upper Extremity (bilateral), Lower extremity (bilateral), Abdomen and other
(139) The Superior Oblique muscle is innervated by:
Trochlear Nerve (CN IV)
(139) The Lateral Rectus muscle is innervated by:
Abducens Nerve (CN VI)
(139) The eye muscles not including Superior Oblique and Lateral Rectus are innervated by:
Oculomotor Nerve (CN III)
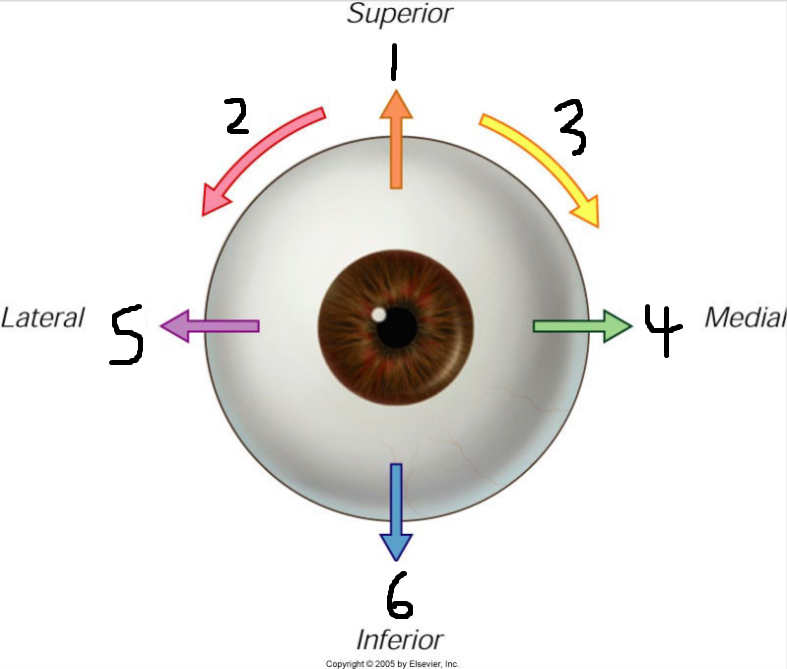
(139) Movement #1 is called:
Elevation
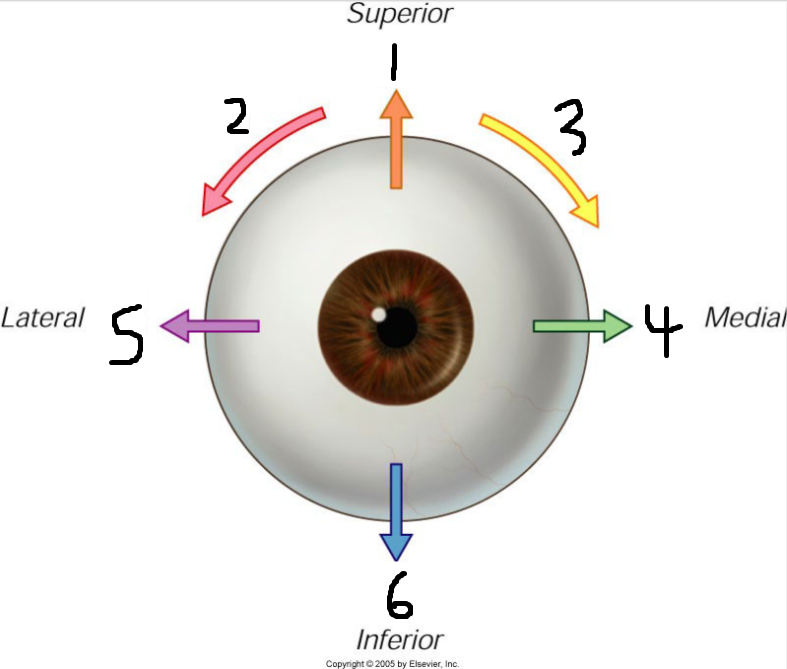
(139) Movement #2 is called:
Extorsion
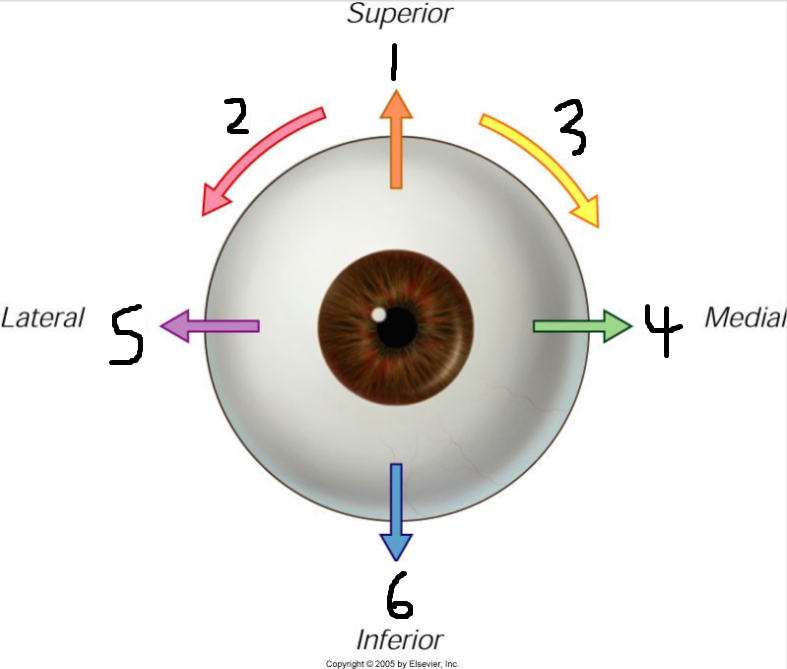
(139) Movement #3 is called:
Intorsion
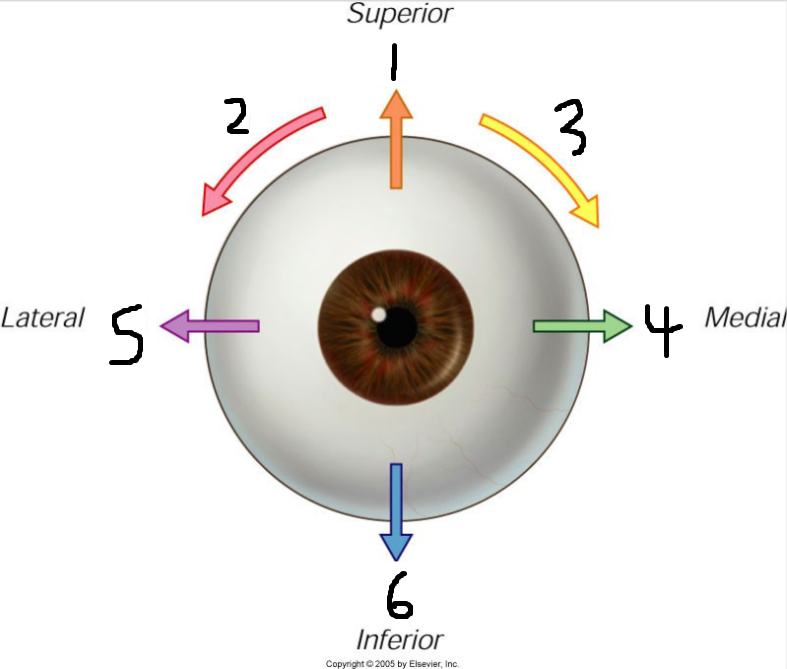
(139) Movement #4 is called:
Adduction
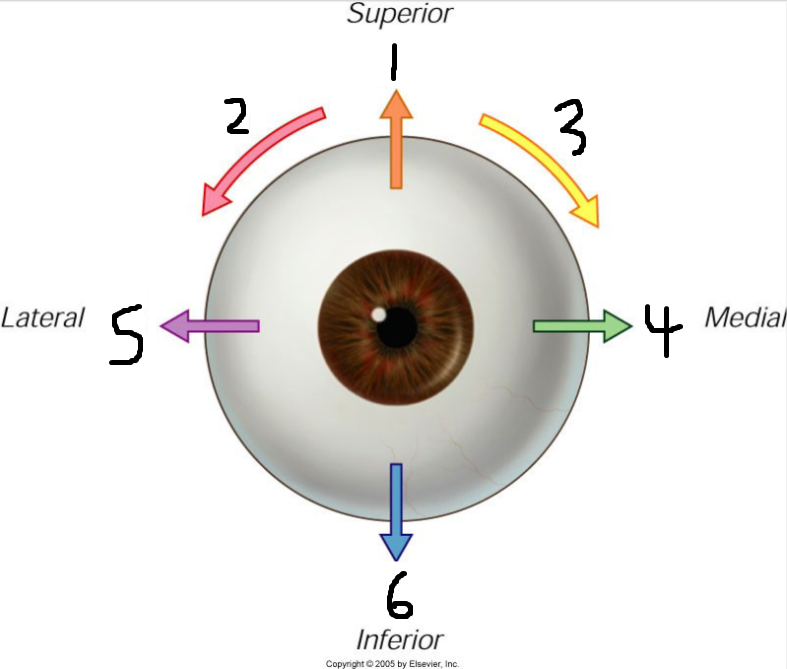
(139) Movement #5 is called:
Abduction
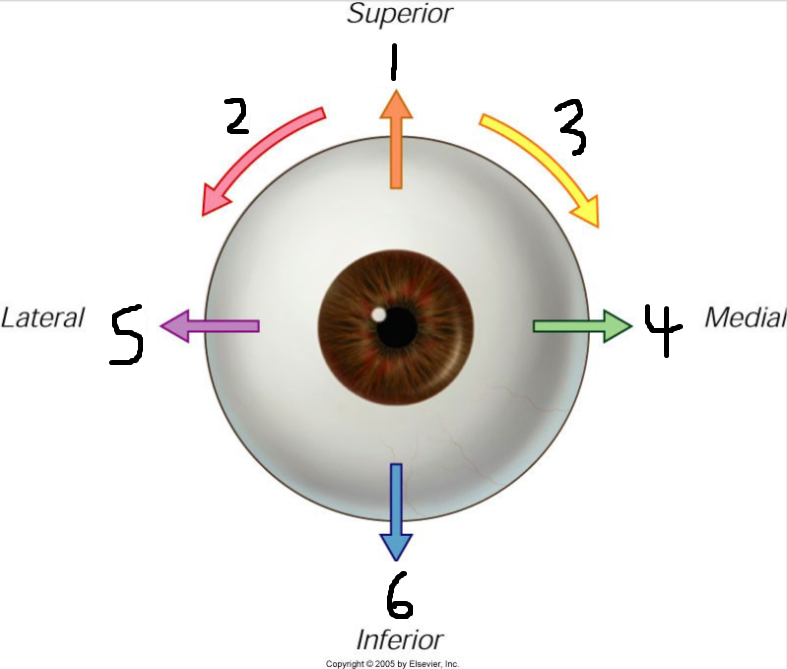
(139) Movement #6 is called:
Depression
(139) Action
what a muscle would do if acted in isolation
(139) Function
what a muscle actually contributes to a particular motion
(139) Superior rectus Function
strong elevator of the already abducted eyeball
(139) Inferior rectus Function
strong depressor of the already abducted eyeball
(139) Inferior oblique Function
strong elevator of the already adducted eye
(139) Paired function of Inferior Oblique and Superior Rectus
Elevation of the eye without torsion
(139) Paired function of Superior Oblique and Inferior Rectus
Depression of the eye without torsion
(139) Paired function of Superior Oblique and Superior Rectus
Intorsion Without Elevation or Depression
(139) Paired function of Inferior Oblique and Inferior Rectus
Extorsion Without Elevation or Depression

(139) Identify the condition:
Ptosis

(139) Identify the muscle not working properly:
Levator palpebrae superioris
(139) Nerve affected in Bielschowsky’s Sign:
Trochlear Nerve (CN IV)

(139) Identify the nerve not working properly:
Oculomotor Nerve (CN III)
(139) A leasion of the Oculomotoer Nerve (CN III) affects which muscles of the eye:
Superior Rectus, Inferior Oblique, Medial Rectus, Inferior Rectus
(139) Bielschowsky’s Sign
Whenever head is tilted to affected side, slight elevation of the eye
(140) Developmental Diseases
Diseases which are genetic or congenital (e.g. Down’s Syndrome)
(140) Inflammatory Diseases
Diseases which include infections, autoimmune conditions, trauma (e.g. snake bite)
(140) Neoplastic Diseases
Diseases which include tumors (benign or malignant) and cancers (e.g. lung cancer)
(140) Degenerative Diseases
Diseases which are related to aging (e.g. Alzheimer’s, Parkinson’s) or muscle breakdown (e.g. Muscular Dystrophy)
(140) Iatrogenic Diseases
Diseases which are drug induced or induced by medical procedure (something meant to help but did not) (e.g. toxicities)
(140) Etiology
cause of disease: genetic, acquired, multifactorial, etc.
(140) Pathogenesis
mechanisms of disease development-cellular, biochemical, and molecular events following exposure of cells/tissues to an (injurious) agent
(140) Morphologic changes
structural alterations induced in the cells and tissues/organs; can be gross or microscopic
(140) Clinical significance
functional consequences of the morphologic changes; clinical manifestations
(140) Sign
objective finding, as perceived by examiner (physician, nurse, etc.) (examples – respiratory rate, heart rate, etc.)
(140) Symptom
manifestation of disease apparent to the patient ; represents the complaints of the patient (subjective) – examples – fatigue, pain, etc.
(140) Lesion
visible changes produced by the disease in the tissue or organ
(140) Sequelae
remote after-effects of a disease
(140) Acute
Disease with a sudden onset, or in a rapid course
(140) Chronic
slow onset and long duration or having a long course
(140) Fulminating
acute (rapid), fatal disease
(140) Idiopathic
Disease with an unknown cause
(140) Teratogenic
Diseases caused by drugs which cross the placenta and harm the fetus
(140) Benign tumors are often described as:
well-circumscribed, encapsulated, non-invasive, noninfiltrating
(140) Malignant tumors are often described as:
metastatic, invasive, infiltrating, poorly circumscribed, hard/firm
(141) Metaplasia
Cellular Adaptation that is replacement of one differentiated (mature, adult) cell by another cell type (most common columnar to squamous). Results from either reprogramming of local tissue stem cells, or, colonization by differentiated cell populations from adjacent sites. Stimulated by signals generated by cytokines, growth factors, and ECM components in cells’ environment
(141) Hyperplasia
Cellular Adaptation that is increase in the number of cells in organ or tissue in
response to stimulus
(141) Physiologic Hyperplasia Examples
hormonal, growth factors (breast at puberty/pregnancy, compensatory hyperplasia of liver)
(141) Pathological Hyperplasia Examples
inappropriate or excessive hormonal (endometrial hyperplasia) or growth factors acting on target cells
(141) Hypertrophy
Cellular Adaptation that is increase in size of cells, resulting in increased size of organ; no new cells.
(141) Physiologic Hypertrophy Examples
increased functional demands, stimulation by growth factors, hormones (examples – uterine growth during pregnancy, skeletal muscle in response to increased demand – e.g body building)
(141) Pathologic Hypertrophy Examples
“abnormal” - heart in hypertension, aortic stenosis
(141) Atrophy
Cellular Adaptation that is reduction in size due to decrease in cell size and number
(141) Physiologic Atrophy Examples
normal development, uterus post partum
(141) Pathologic Atrophy Examples
disuse (decreased workload), denervation, decreased blood supply, decreased nutrition, decreased hormone stimulation, pressure
(141) Causes of Cell Injury
Decreased oxygen – hypoxia (via decreased blood flow, anemia, etc.), Physical agents – trauma, temperature, radiation, electricity, Chemicals/drugs, Infectious agents, Immunological reactions, Genetic abnormalities, Nutrition abnormalities (starvation, obesity, etc.)
(141) Coagulative Necrosis
Architecture (cell outlines) preserved, nucleus disappears (breaks up, disintegrates- pyknosis, karyohexix, karyolysis) – loss of nucleus with outline of cell “ghost” remaining
(141) Liquefactive Necrosis
Digestion of dead cells resulting in liquid, viscous mass. Examples include brain infarcts (strokes), abscesses
(141) Anthracosis
Cellular Accumulation that is especially in lungs in heavy smokers, polluted areas, coal, dust
(141) Hemosiderin
Cellular Accumulation that is old blood
(141) Lipofuscin
Cellular Accumulation that is “wear and tear” pigment associated with aging cells
(141) Reversible Cell Injuries
Reduced Na/K pump leading to cell swelling (hydropic change, vacuolar degeneration). AKA edema
(141) Irreversible Cell Injuries
After 20 – 30 minutes:
-Increase in anaerobic glycolysis – decreases glycogen, increases lactic acid, decreases pH (chromatin clumping)
-Decrease in protein synthesis
-Failure of CA pump----Ca enters cell causing membrane and nuclear damage via activation of enzymes such as phospholipases, proteases, endonuclease, and ATPases
-Denaturation of intracellular proteins, enzymatic digestion of cell, contents leak out and elicit inflammation
(142) WBCs that respond to Acute Inflammation:
Neutrophils
(142) WBCs that respond to Viral Infections:
Lymphocytes
(142) WBCs that respond to Chronic Inflammation:
Monocytes/Macrophages, (occasionally) Lymphocytes and Eosinophils (allergies)
(142) Inflammation factors most predominant around 24 hours:
Neutrophils
(142) Inflammation factors most predominant around 48 – 72 hours:
macrophages
(142) Neutrophils
Predominant inflammatory cell in acute infections especially acute bacterial infections
(142) Fibroblasts
Cells that Create matrix of fibronectin and type III collagen, Lay down collagen and ECM. After about 1 – 2 months fibrous scar is present
(142) Serous Acute Inflammation
cell-poor fluid build up (effusion). E.g. blisters, viral pleuritis
(142) Fibrinous Acute Inflammation
increased permeability, exudative-type fluid, increased fibrin deposition. E.g. fibrinous pericarditis
(142) Suppurative (purulent) Acute Inflammation
exudative type fluid with cells leading to pus. E.g. pyogenic bacteria (staph), abscesses (localized collections of purulent inflammatory tissue)
(142) Ulcer
excavation of surface of tissue because of shedding of inflamed necrotic tissue
(142) The first step of phagocytosis is:
Recognition/Opsonization
(142) The second step of phagocytosis is:
Engulfment
(142) The third step of phagocytosis is:
Killing
(142) Opsonization
microbes are coated with proteins to help WBCs better recognize and destroy them
(142) Engulfment
WBCs engulf microbes to form phagosomes which then fuse with lysosomes (phagolysosomes)
(142) Killing
Myeloperoxidase in neutrophils combines with Cl- and converts H2O2 to hypochlorite (bleach) which kills microbes
(142) The first step of Vascular changes of inflammation is:
Vasodilation
(142) The second step of Vascular changes of inflammation is:
Vascular permeability increase
(142) The third step of Vascular changes of inflammation is:
Stasis
(142) The fourth step of Vascular changes of inflammation is:
Margination
(142) Mechanism of Vasodilation
Inflammatory trigger leads to release of histamines, causing relaxation of
vascular smooth muscle and increased blood flow
(142) Mechanism of Vascular permeability increase
histamines retract endothelial cells to allow openings within the lining of venules. Fluid, proteins, and cells leak out
(142) Mechanism of Stasis
Vasodilation leads to increased blood vessel diameter, combined with fluid loss due to permeability, higher concentration of RBCs causes higher viscosity of blood, blood slows down
(142) Major mediators involved in inflammation
Histamine, prostaglandins, NO, bradykinin, leukotrienes, cytokines, complement
(142) Histamine
Made and stored in mast cells, binding of Abs to mast cells (allergic reactions).
(142) Nitric Oxide
Dissolved gas that acts as signaling molecule, produced by endothelial cells and relaxes vascular smooth muscle (vasodilation)
(142) Histamine (and nitric oxide) mediated vasodilation, increased blood flow and vascular permeability all contribute to:
Rubor (redness), Calor (warmth), Tumor (swelling-edema)
(142) Prostaglandins (PGE2) contribute to:
Rubor (redness), Calor (warmth), Dolor (pain)
(142) Function of Prostaglandins (PGE2)
sensitize nerve endings to the effects of bradykinin
(142) Function of Bradykinin
causes vasodilation at low concentrations and vasoconstriction at higher concentration
(142) The first step of Cellular response in inflammation is:
Margination
(142) The second step of Cellular response in inflammation is:
Rolling
(142) The third step of Cellular response in inflammation is:
Adhesion
(142) The fourth step of Cellular response in inflammation is:
Transmigration