Exam 3
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
Clinical Description of Female Sexual interest/arousal disorder
Lack of or significantly reduced sexual interest/arousal (factors could be losing interest in your partner or relationship stress)
Typically manifesting in:
Reduced sexual interest
Reduced sexual activity
Fewer sexual thoughts
Reduced arousal to sexual cues
Reduced pleasure or sensations during almost all sexual encounters
And causes significant distress
Research suggests 7-46% of women experience low sexual desire
Clinical Description of Male hypoactive sexual desire disorder
Little or no interest in any type of sexual activity
Masturbation, sexual fantasies, and intercourse are rare
Affects approximately 5% of men
As with other disorders: not better explained by something else
Clinical description of Genito-pelvic pain/penetration disorder
In females, difficulty with vaginal penetration during intercourse, associated with one or more of the following:
Pain during intercourse or penetration attempts
fear/anxiety about pain during sexual activity
Tensing of pelvic floor muscles in anticipation of sexual activity
Clinical description of erectile disorder
Difficulty achieving or maintaining an erection
Sexual desire is usually intact
Most common problem for which men seek treatment
Prevalence increases with age
50% of men over 60 experience erectile dysfunction (correlation between age and experiencing erectile dysfunction)
Social/cultural influences on sexual functioning?
Learned negative attitudes toward sex and sexuality (Erotophobia)
Negative sexual experiences
Relationship challenges; dissatisfaction within romantic relationships
How physical disorders/disability can impact sexual functioning?
Physical disability often increases the likelihood of sexual functioning problems
People with more severe physical disability report on average lower-sexual satisfaction
Treatment options for sexual dysfunction
Educate clients and patients, not assume that they know anything,
Masters and Johnson’s psychosocial intervention (no actual sexual intercourse)
Sensate focus and nondemand pleasuring
Sexual activity with the goal of focusing on sensations without trying to achieve orgasm
Use of dilators to help women with painful intercourse
Exposure to erotic material for problems with low sexual desire
Medications (oral, injectable), vacuum-pump devices for ED
Referral to appropriate medical professionals (PCP, PT)
Psychological disorders that may make someone more vulnerable to sexual dysfunction
Anxiety disorders
Mood disorders
Trauma
Somatic disorders
Substance use disorders
Recognize circumstances where a diagnosis may be inappropriate despite symptoms being present
Outside factors such as severe relationship stress that could be accounting for symptoms
Reasons as to why healthcare professionals may be less inclined to bring up sexual health in an appointment with a patient/client
It’s often minimally covered in professional and medical education
assuming patient doesn’t want to talk about sex or would feel too embarrassed if you brought it up
Distinguish between substance use and abuse?
Substance use: taking moderate amounts of a substance in a way that doesn’t interfere with functioning
Substance abuse: use in a way that is dangerous or causes substantial impairment (e.g. affecting job or relationships)
Distinguish between tolerance and withdrawal?
Tolerance: needing more of a substance to get the same effect/reduced effects from the same amount
Withdrawal: physical symptom reaction when substance is discontinued after regular use
Clinical Features of substance use disorders
Pattern of substance use leading to significant impairment and/or distress
Symptoms (need 2+ within a year mild) (4 or 5 moderate) (6 or more severe)
Taking more of the substance than intended
Desire to cut down use
Excessive time spent using/acquiring/recovering
Craving for the substance
Role disruption (e.g. can’t perform at work
Interpersonal problems
Reduction of important activities
Use in physically hazardous situations (e.g. driving)
Keep using despite causing physical or psychological problems
Tolerance
Withdrawal
Recognize 5 main categories of substances, common features of each, and example of drugs that belong to each category?
Depressants
Behavioral sedation (e.g. alcohol, sedative, anxiolytic drugs)
Stimulants
Increase alertness and elevate mood (e.g. cocaine, nicotine)
Opiates
Produce analgesia and euphoria (e.g. heroin, morphine, codeine)
Hallucinogens
Alter sensory perceptions (e.g. marijuana, LSD)
Other drugs of abuse
Include inhalants, anabolic steroids, medications
What are the long-term effects of heavy drinking?
Tremors
Nausea/vomiting
Hallucinations
Agitation
Insomnia
Seizures
Delirium tremens
Liver disease (½ of cases are because of alcohol abuse, includes cirrhosis-scarring of the liver)
Pancreatitis
Cardiovascular disorders
Depression
Certain cancers (breast cancer link to alcohol,
Brain damage
Dementia
Wernicke-korsakoff syndrome
What are delirium tremens (DT)?
in severe cases (3-5% will experience)
when people appear disoriented and affects their voluntary muscle movement and have tremors
can be serious because it involves body's ability to regulate basic functions, can affect heart rate and respiration (breathing)
Long term-effects of heavy drinking: Fetal Alcohol Syndrome
Condition that affects children exposed to alcohol before birth. Commonly affects behavior, learning, and physical features (low iq, hyperactive behavior, speech and language delays, learning disabilities)
Physically looks like: large forehead, thin upper lip, minor skin folds on ears
Common comorbid diagnoses with substance use disorders?
Approximately 75% of people in addiction treatment meet criteria for at least one other psychiatric disorder
Mood disorders (40% or more)
Anxiety disorders and PTSD (25% or more)
When other psychiatric symptoms occur in the context of active substance use, clinicians must proceed carefully with diagnosis
What counts as a standard drink for beer, wine, and liquor?
12 oz of regular beer (5% alc)
5 oz of table wine (12% alc)
1.5 fl oz of distilled spirits (40% alc)
What is meant by moderate, heavy drinking, and binge drinking for men and women?
According to the 2020-2025 Dietary Guidelines for Americans
Recommend for adults of legal drinking age to drink no more than 2 drinks/day (men) or 1 drink/day (women)
Some people (e.g. pregnant women) should not drink
Heavy drinking according to NIAAA
For men, consuming >4 drinks on any day or more than 14/week
For women, consuming >3 drinks on any day or more than 7/week
Binge-drinking
4+ drinks for women; 5+ drinks for men within 2-hour period
What is meant by prescription drug misuse/abuse?
Prescription drug misuse and abuse is when someone takes a medication inappropriately (NIDA)
Adolescents are particularly vulnerable
Most of the prescription drugs that are misused are pain-relieving drugs
How do opioids have their effect?
Opioid drugs bind to opioid receptors in the CNS
Inhibit production of GABA (dopamine police, increase in euphoria)
Allows more dopamine to be available in the brain
Why would someone be at high risk of overdose from a relapse after a period of abstinence?
They do not realize that they do not need as much to get the same effect, so they take a higher amount
Relevant biological treatments (like Naltrexone and Methadone) for opioid use disorder and alcohol use disorder?
Naltrexone
FDA-approved for opioid and alcohol use disorders
Blocks pleasant effects of drugs; reduce cravings
Patients must complete detox (medically managed withdrawal) prior to initiating
Suboxone (is an opioid)
FDA-approved for opioid use disorders
Blocks pleasant effects of drugs; reduce cravings
Potentially addictive
Methadone (is an opioid)
FDA-approved for opioid use disorders
Blocks pleasant effects of drugs; reduce cravings
Potentially addictive
Describe some of the positive outcomes of medication-assisted treatment for opioid use disorder?
Lower the risk of fatal overdoses by approx. 50%
Lower the risk of non-fatal overdoses
Reduce drug-injecting
Reduce HIV transmission
Reduces criminal activity by opioid users
Questions asked on the CAGE alcohol use disorder screening tool?
1. Have you felt the need to Cut down on your drinking?
2. Do you feel Annoyed by people complaining about your drinking?
3. Do you ever feel Guilty about your drinking?
4. Do you ever drink an Eye-opener in the morning to relive the shakes?
General Nature of Personality Disorders (PD)
Enduring, inflexible predispositions
Maladaptive, causing distress and/or impairment
High comorbidity
Poorer prognosis
What are the 3 personality clusters and what PDs belong to each cluster?
A (follows B)
Odd or eccentric cluster
Includes paranoid, schizoid, schizotypal
B (most prevalent in US)
Dramatic, emotional, erratic cluster
Includes antisocial, borderline, histrionic, narcissistic
C (follows A)
Fearful or anxious cluster
Includes avoidant, dependent, obsessive-compulsive
Common focus of treatment for Cluster A PDs?
Focus on interpersonal skills
Building trust where paranoia is a factor
Address comorbid conditions
Clinical features of antisocial PD?
Failure to comply with social norms
Violation of the rights of others
Irresponsible, impulsive, and deceitful
Lack of a conscience, empathy, and remorse
May be charming, interpersonally manipulative
Most often diagnosed in males
Antisocial PD: Common features of early/family history?
Relation with early behavior problems and conduct disorder
Early histories of behavioral problems including conduct d/o
“Callous-unemotional” type of conduct disorder most likely to evolve into antisocial PD
Families with inconsistent parental discipline and support (modeling and demonstrating)
Families often have histories of criminal and violent behavior
Clinical features of Borderline PD?
Unstable moods and relationships
Impulsivity, fear of abandonment, poor self-image
Self-mutilation and suicidal gestures
Treatment options for Borderline PD?
Antidepressant medications provide some short-term relief
Dialectical behavior therapy is most promising treatment; 4 components:
Mindfulness: the practice of being fully aware and present
Distress Tolerance: how to tolerate pain in difficult situations
Interpersonal effectiveness: how to ask for what you want and say no while maintaining self-respect and relationships with others
Emotion regulation: how to decrease vulnerability to painful emotions and change emotions that you want to change
Clinical features of Obsessive-Compulsive PD and how it differs from OCD?
Excessive and rigid fixation on doing things the right way
Highly perfectionistic and orderly (to an extreme)
Obsessions and compulsions are rare
DSM-5 criteria for schizophrenia?
A. Two (or more) of the following each present for a significant portion of time during a one-month period:
Delusions
Hallucinations
Disorganized speech
Grossly disorganized or catatonic behavior
Negative symptoms
B. For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self-care, is markedly below the level achieved prior to the onset
C. Continuous signs of the disturbance persist for at least six months
In children, not making milestones
Parkinsons and dementia
What are hallucinations?
Experience of sensory events without environmental input
Can involve all senses (e.g. tasting something when not eating, having skin sensations when not being touched)
Most common: auditory
What are some types of hallucinations?
Auditory (hearing things that aren’t there)
Subtype: command hallucinations (are when a voice tells you to do something)
Visual (seeing things that aren’t there) (tree trunks falling in front of you)
Olfactory (smelling things that aren’t there) (rotten eggs)
Tactile (feeling things that aren’t there) (bugs crawling on skin)
What are delusions?
Gross misrepresentations of reality
What are some examples of delusions?
Delusions of grandeur (beliefs that I have special skills or famous person, unique abilities)
Delusions of persecution (believe other people are out to harm or get them, being followed, CIA is tracking them)
Clinical Description for schizophreniform
Psychotic symptoms lasting between one and six months
Need 2+ symptoms (delusions, hallucination, disorganized speech, disorganized or catatonic behavior, negative symptoms)
Clinical description for brief psychotic disorder
Psychotic symptoms lasting less than one month
Need 1+ symptom(s) (delusions, hallucinations, disorganized speech, disorganized or catatonic behavior)
Clinical description for schizoaffective disorder
Symptoms of schizophrenia + additional experience of a major mood episode (depressive or manic)
Psychotic symptoms must also occur outside the mood disturbance
Prognosis is similar for people with schizophrenia
Such persons do not tend to get better on their own
Clinical description for catatonia
Unusual motor responses, particularly immobility or agitation, and odd mannerisms
Tends to be severe and quite rare
May be present in psychotic disorders or diagnosed alone
May include
Stupor, mutism, or maintaining the same pose for hours
Opposition or lack of response to instructions
Repetitive, meaningless motor behaviors
Mimicking others’ speech or movement
Positive Symptom Cluster in Schizophrenia (things happening on top of normal experiences)
Hallucinations
Experience of sensory events without environmental input
Can involve all senses (e.g. tasting something when not eating, having skin sensations when not being touched)
Most common: auditory
Delusions
Gross misrepresentations of reality
Most common:
Delusions of grandeur (beliefs that I have special skills or famous person, unique abilities)
Delusions of persecution (believe other people are out to harm or get them, being followed, CIA is tracking them)
Negative symptom cluster in schizophrenia (absence of normal experiences)
The negative symptoms
Absence of insufficiency of normal behavior
Spectrum of negative symptoms
Avolition (or apathy) - lack of initiation and persistence (even if offered enticement, will still be incapable of doing it)
Alogia - relative absence of speech (when asked a question, will answer in only one or two words)
Anhedonia - lack of pleasure, or indifference (normal things that brings one joy is not getting joy anymore)
Affective flattening - little expressed emotion (expression is flat, not showing anything)
Disorganized symptom cluster in schizophrenia
Disorganized speech
Tangentiality - “going off on a tangent” (start at point a, end at point d, never make point back to a)
Loose associations - conversation in unrelated directions (ideas loosely held together and don’t make a lot of sense, person has lumped them together)
Disorganized affect (what they are saying doesn’t match outward expression of emotion)
Inappropriate emotional behavior
Disorganized behavior
Includes a variety of unusual behaviors
Catatonia
Considered a psychotic spectrum disorder in its own right or, when occurring in the presence of schizophrenia, a symptom of schizophrenia
Describe differential diagnoses for schizophrenia (i.e. disorders we would need to rule out because they share similar clinical features)
Multiple personality/dissociative identity disorder
Sleep paralysis
Substances
Bipolar (Type 1)
Major depression
Parkinsons
Lewy Body
Prevalence Rate of Schizophrenia
Onset and prevalence of schizophrenia worldwide
about 1% of the population
Often develops in early adulthood
Can emerge at any time; childhood cases are very rare
Tends to follow chronic course
Most with mod-severe impairment
Lower life expectancy (due to increased risk of suicide, accidents, and poorer self-care)
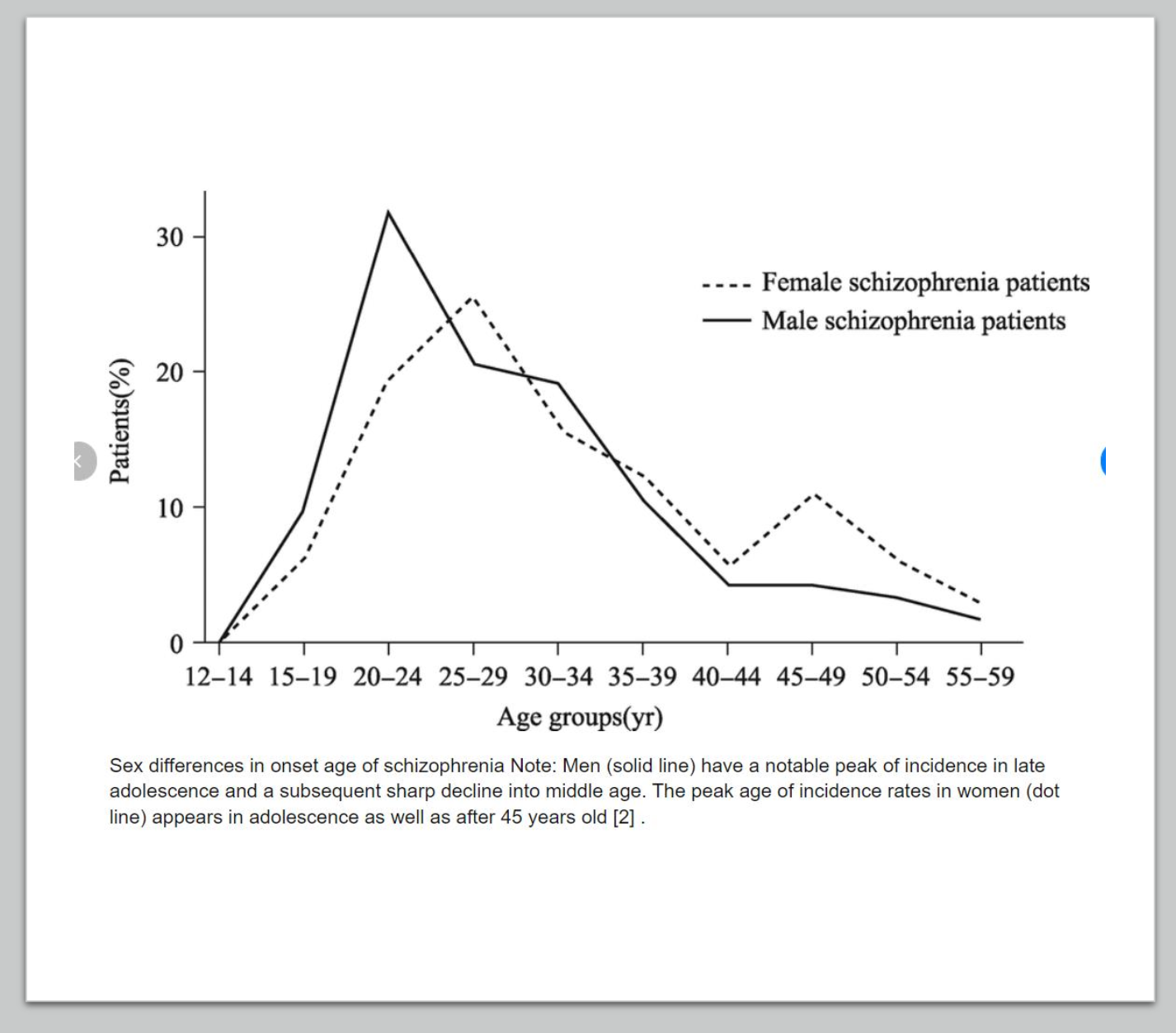
Demographic patterns in age of onset
Affect males and females about equally
Onset slightly earlier for males
females tend to have one big peak from ages 20-24
males have two peaks from 25-29 and 45-49
Relationship between schizophrenia and life expectancy
Lower life expectancy (due to increased risk of suicide, accidents, and poorer self-care)
Describe what is meant by the “prodromal” phase of schizophrenia
unusual psychotic-like behaviors
What are the causal factors and correlates of schizophrenia?
Degree of genetic relatedness matters
Adoption studies
Adopted children whose bio parents have schizophrenia are still at risk for developing schizophrenia
BUT a healthy environment is a protective factor
The dopamine hypothesis: Schizophrenia is partially caused by overactive dopamine
Drugs that increase dopamine (agonists) result in schizophrenic-like behavior
Drugs that decrease dopamine (antagonists) reduce schizophrenic-like behavior
Structural and functional abnormalities in the brain
Enlarged ventricles and reduced tissue volume
Hypofrontality - less active frontal lobes
Viral infections during early prenatal development
Findings are inconclusive
The role of stress
May activate underlying vulnerability (think: diathesis-stress)
May also increase risk of relapse
Cold parenting - unsupported theory
High expressed emotion within families - associated with relapse
Describe treatment options for schizophrenia
Typically involves antipsychotic medication plus psychosocial interventions such as
Social skills/living skills training
Family therapy
Vocational rehabilitation
Noncompliance with medication is a common issue
Meds can have major and permanent side effects
Eg. Tardive dyskinesia
What is tardive dyskinesia?
Tardive dyskinesia is caused by long-term use of neuroleptic drugs, which are used to treat psychiatric conditions.
Tardive dyskinesia causes repetitive, involuntary movements, such as grimacing and eye blinking.
Inattentive symptoms of ADHD
Not giving close attention to details
Difficulty maintaining attention
Trouble with follow-through
Avoid tasks that require sustained mental effort (reading intense book, often see procrastination)
Often loses things necessary for tasks/activities
Easily distracted and/or forgetful
Hyperactive/impulsive symptoms of ADHD
Fidgeting in seat
Often unable to engage in leisure activities quietly
“Driven by a motor”
Running/climbing in situations where inappropriate (or feelings of restlessness in adults)
Blurting out answers before question is completed
Difficulty waiting their turn
Prevalence rates/trends of ADHD
Prevalence
It occurs in approximately 5% of school-aged children
Symptoms are usually present around age 3 or 4
Children with ADHD have similar problems as adults
Gender differences
Boys outnumber girls 3:1
Cultural factors
ADHD is most commonly diagnosed in the US but also diagnosed worldwide (2-7% prevalence rate)
Diagnoses are increasing as the years go by
Childhood prevalence by race or ethnicity, according to large national sample
White, non-hispanic 78.8%
Hispanic 9.1%
Black 6%
Asian 3.2%
Other 3.0%
Autism prevalence rates/trends
1 in 44 children in the US meet criteria
More commonly diagnosed in males
IQ interaction
Approx 35% show intellectual disabilities
Worldwide prevalence = 1%
Biological Treatment Options for ADHD
Stimulant medications
Currently prescribed for approximately 4 million American children
Low doses of stimulants improve focusing abilities
Examples include Ritalin, Dexedrine, Adderall
Problem: may increase risk for later substance abuse
Behavioral Treatment for ADHD
Behavioral treatment
Reinforcement programs
To increase appropriate behaviors/decrease inappropriate behaviors
May also involve parent training
Combined biopsychosocial treatments
Often recommended
May be superior to medication or behavioral treatments alone
Biological Treatment for ASD
Biological treatments
Medical interventions has had little positive impact on core dysfunction
Some drugs decrease agitation
Tranquilizers
SSRIs
Indicators of good prognosis
High IQ, good language ability
Behavioral Treatment for ASD
Behavioral approaches
Skill building
Reduce problem behaviors
Communication and language training
Increase socialization
Early intervention is critical - may ”normalize” the functioning of the developing brain
Risk Factors of ADHD
Genetic contributions
ADHD seems to run in families
DAT1 - Dopamine transporter gene has been implicated
Some ADHD drugs work by inhibiting DAT1
Neurobiological correlates of ADHD
Smaller brain volume
Inactivity of the frontal cortex and basal ganglia
Abnormal frontal lobe development and functioning
Risk Factors of ASD
Significant genetic component
Familial component: if one child with autism, the chance of a second child with autism is 20% (100x greater risk than general population
Possible link between autism and oxytocin receptor genes
Older parents associated with increased risk
Neurobiological influences
Amygdala
Larger size at birth = higher anxiety, fear
Elevated cortisol
Neuronal damage in the amygdala results from high stress, which may affect processing of social situations
Oxytocin (helps explain social withdrawal)
Lower levels
Vaccinations do not increase the risk of autism
Mercury in some vaccinations was rumored to increase autism risk
Large scale studies do not support this
High rates of vaccinations do not increase risk for autism in the community at large
Health risk of not vaccinating is substantial
What are the main areas of impairment in ASD? What are some examples?
Deficits in social communication and social interaction, including
social -emotional reciprocity
Nonverbal communication behaviors
Developing, maintaining, and understanding relationships
Restricted, repetitive patterns of behavior, interests, or activities, including
Stereotyped or repetitive motor movements
Insistence on sameness; inflexible adherence to routines
Highly restricted, fixated interests
Hyper- or hyperactivity to sensory input
What is the relationship between ASD and intellectual disability?
Those w/ ASD can have intellectual disability bc of their slower development
ADHD Central Features
Central features - inattention, overactivity, and impulsivity
Associated with various impairments
Behavioral
Cognitive
Social and academic problems
3 symptom types
Inattentive
Hyperactive/impulsive
Combined
Diagnostic Features of ADHD
Several symptoms must be present prior to age 12
Symptoms present in two or more settings (home and school or work)
Significant distress or impairment
Not better explained by another condition (anxiety, substance use disorders, schizophrenia)