8B- nutrition in adolescence, adulthood, and the elderly
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
33 Terms
nutrients needed in adolescence
surpasses needs at any other time of life
due to rapid growth
iron for hemoglobin production in expanding blood volume for all and female increase from onset of menstruation
increased calcium for bone
increased zinc for muscle growth
do males or females develop more lean body mass
males develop greater lean body mass
female adolescent body
more adipose and less lean body mass then males
adipose tissue
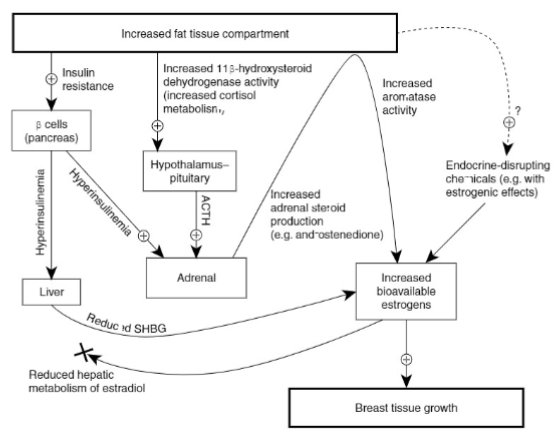
endocrine tissue (secretes hormones)
expresses aromatase
increased adiposity in young females i sassoicated with early onset of puberty
aromatase
enzyme involved in the production of estrogen
how is HPO axis initiated
leptin (adipokine) stimulates expression of kisspeptin
kisspeptin stimulates release of gonadotropin releasing hormone (GnRH)
GnRH contributes to increased production of estrogen
breast tissue growth in females
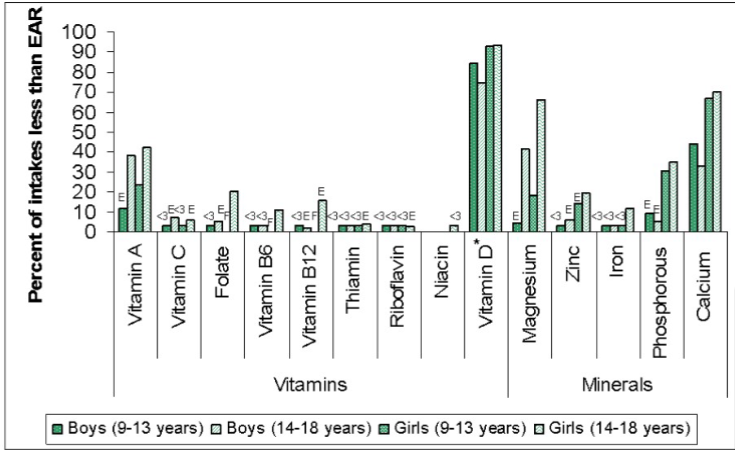
Canadian Community Health Survey
boys and girls 9-18 did not have enough vit A intake
girls 14-18 low B6, folate, B12
12% adolescent girls not meeting iron requirements
70% girls 9-13 AND 30% BOYS 14-18 not meeting calcium requirements
15% girls 9-13 adn 20% girls 14-18 not meeting zinc requirements
dietary concerns for adolescents
vegetarian and vegan: may be adopted in teen years even if family not vegetarians
health teaching: important to prevent nutrient deficiencies especially for teens following different dietary plan than their family members
optimal non-meat protein sources
possible requirement for iron and zinc supplementation
avoiding deficiencies in vitamin B12, calcium, and vitamin D in vegans
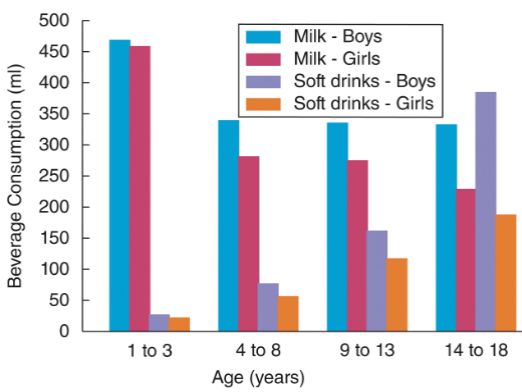
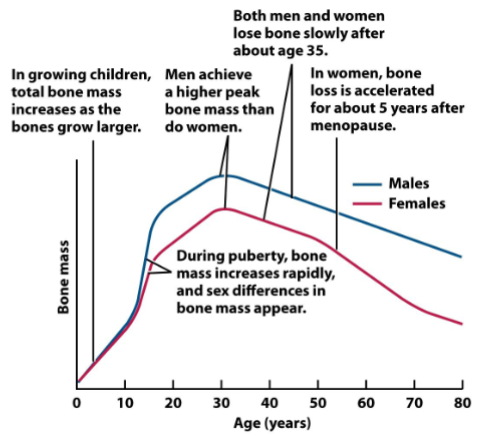
bone health in adolescence
milk consumption tends to decrease during adolescence
social eating habits: fast food with soft drinks
calorie-free soft drinks may be chosen as well
for females: concern that calcium intake is adequate
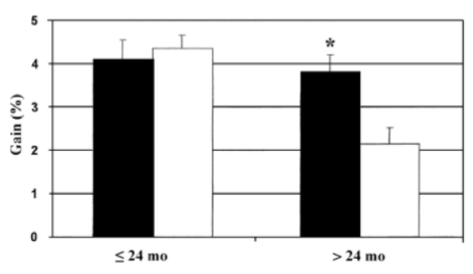
window opportunity for adolescent girls
calcium supplement of postmenarcheal girls with low calcium intakes enhances bone mineral acquisition, especially in girls over 2 years in the past onset of menarche
calcium supplements after this period are less effective
bone mass across the lifespan
dietary concerns for adolescents
eating disorders
adolescent pregnancy
impacts nutritional needs, nutrients are required for the growth of the fetus and the teen
smoking
risk factor for chronic diseases later in life, it increases the need for nutrients such as vitamin C due to added oxidative stress from tobacco use
alcohol consumption
alters absorption and metabolism of nutrients; also replaces calories from nutritious food. binge drinking
cannabis use in adolescents
linked to brain structure changes
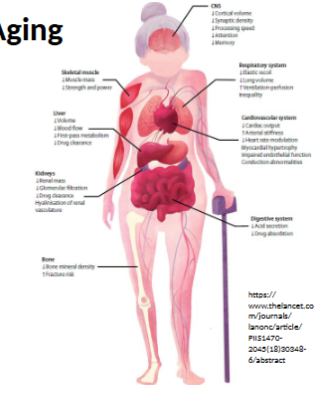
body structures during aging
number of cells decrease and function of remaining cells declines
tissue and organ cells lose ability to maintain homeostasis
people are living longer but not everyone enjoys increase in life expectancy
what impacts rate of aging
environment
disease, accident, toxins
lifestyle
nutrition, exercise, stress
genetics
susceptibility to environmental stress
ability to repair cellular damage
only method to extend longevity
calorie restriction
studies only done in animals
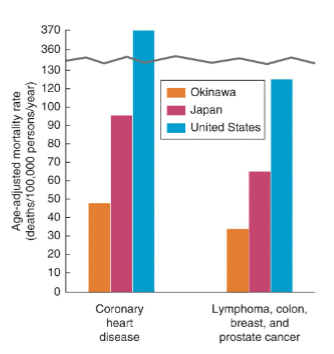
Indigenous Okinawans of Japan, have one of the longest life expectancies in the world (83.8 years)
lower incidence and mortality of chronic diseases including CV and cancer
nutrient dense, traditional diet includes many leafy and root vegetables, soy, little meat, sweet potato instead of rice
potentially related to long term calorie restriction: adults only eat around 80% of a typical Japanese diet
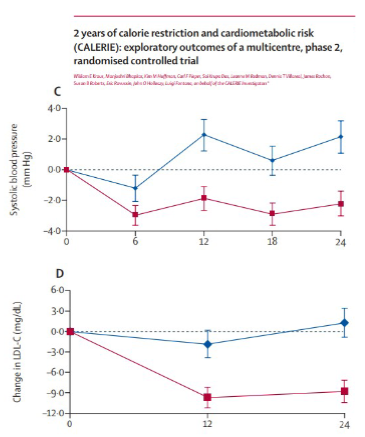
CALERIE study
stands for: comprehensive assessment of long-term effects of reducing intake of energy
2 phase multicenter RCT
assessed young and middle-aged (21-50) health non-obese (BMI 22-27.9) men and women
participants were randomly assigned (2:1) to a 25% calories restriction diet or as ad libitum control diet
2 years of moderate calorie restriction significantly reduced multiple cardiometabolic risk factors in young, non-obese adults
systolic (C) and diastolic BP
LDL-cholesterol (D), total chol, to HDL-cholesterol ratio
C-reactive protein (= inflammatory marker), insulin sensitivity index, and metabolic syndrome score
suggests moderate calorie restriction i n test population has substantial advantages for CV health, maybe long term population health benefits
follow up studies implicate changes in gene transcription related to stress response
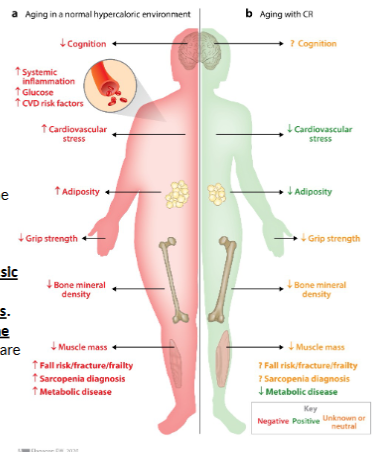
calorie restriction and aging in humans study
Evidence from observational, preclinical, and clinical trials
suggests the ability to increase life span by 1–5 years with an
improvement in health span and quality of life. CR moderates intrinsic
processes of aging through cellular and metabolic adaptations and
reducing risk for the development of many cardiometabolic diseases.
Yet, implementation of CR may require unique considerations for the
elderly and other specific populations.
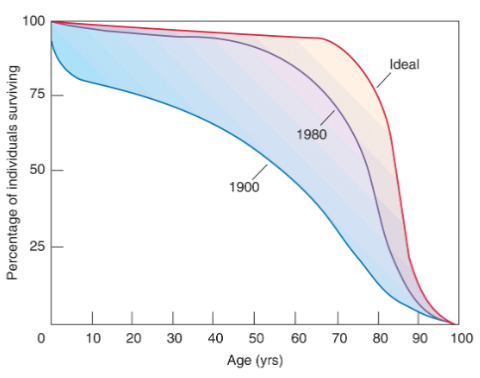
life expectancy in society
about 78 years
only about 69 of these years are disease adn disability free
compression of morbidity
the delaying of onset of symptoms of disease so that they take up less of later life
this would increase the health of the aging population and spare the healthcare system
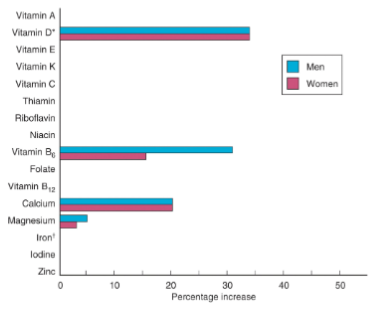
nutrient requirements in older adults
higher vitamin B6 dietary intakes are needed to maintain the same functional levels in the body
vitamin D and calcium
low intake contributes to osteoporosis
iron needs in families is decreased due to menopause
vitamin B12 reduced absorption and low dietary intakes
RDA in not increased but fortified foods recommended in over 50 years
folate can be a concern due to anemia (with low vitamin B12), with is common in older adults
zinc can be a concern due to a combination of lower energy intake, damage, and medication. can impact taste acuity and contribute to low food intake
vitamin C and E (antioxidants)
RDA not increased, but often lower intake due to less fruits and vegetables in diet
physiological effects of aging
sensory decline
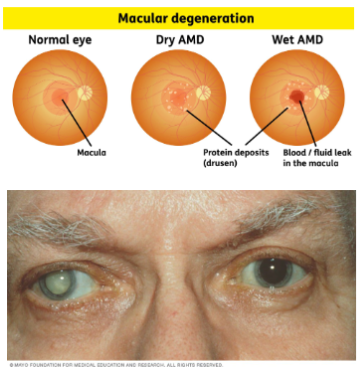
macular degeneration
cataracts
periodontal disease
atrophic gastritis
decline in size and functioning of liver and kidneys
Alzheimer’s disease and dementia
reduced hormone levels
decrease in mobility
increase in body fat, decrease in lean body tissue
immune function and underlying illness
sensory decline
over 60 years there is sensory decline leading to impaired taste and smell
a decrease in the amount of saliva also contributes to this decreased sense
thirst sense decreased (increased risk of dehydration)
decreased visual acuity makes shopping and food preparation more difficult
periodontal disease
may impact chewing and swallowing
atrophic gastritis
stomach empty slower, allowing older adults to feel full longer and decrease food intake
10-30% of adults over 50 have atrophic gastritis; incidence can be as high as 40% in adults 80+
decreased motility and elasticity of the large intestine, along with low fibre and liquid intake can result in constipation
pharmaceuticals can decrease nutrient absorption, and food can enhance or inhibit the absorption and metabolism of medications
shift in body composition
shift to greater % of fat (sarcopenia)
decreased strength and endurance affect mobility and balance, which increases the risk of fractures and falls
also impacts cardiac muscles and muscles associated with breathing
emerging research highlights the role of exercise in delaying these effects
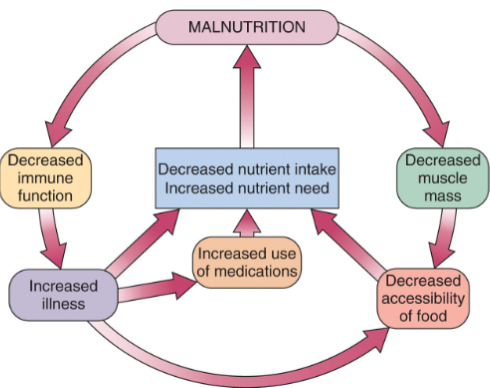
immune function
decline in immune function due to aging (and/or associated nutritional deficiencies)
sickness limits nutrient intake and absorption, this in turn affects the body’s ability to mount an immune response= increased risk for disease, including cancer
immune surveillance and destruction of cancerous cells may be impacted
interventions to reduce risk of infection and illness:
supplementation
proper nutrition including omega-3 fatty acids
exercise
risk of malnutrition
the prevalence of malnutrition increases as people age
decreased basal metabolic rate means that fewer calories are needed, but the same or increased amount of nutrients
increases the risk of malnutrition as food intake decreases
less enjoyment of food and eating
age 60+, sensory decline leading to impaired taste adn smell
less saliva produced
thirst sense is decreased as well, increasing the risk of dehydration
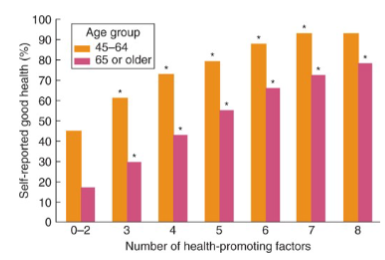
CCHS Study of Health-promoting factors in Older Adults
never smoked daily or quit for 15 years or more
not obese (ex. BMI <30)
sleeps well
good oral health
eat 5 or more servings of fruits and vegetables per day
frequent walker
frequent social participation
low daily stress
cognitive impairments
cognitive decline can affect the ability to acquire and prepare food
physical activity can delay the onset of Alzheimer’s and dementia
a multidomain approach that includes diet, exercise, cognitive training, and vascular risk monitoring demonstrated improvements or maintenance of cognitive function
cohort studies have shown that the MIND dietary pattern can delay cognitive decline, but recent clinical trials have not shown an effect

healthy aging- economics, social and psychological factors
seniors are often on a fixed (and low) income, however rising costs, including those related to healthcare can push individuals into poverty
old age security benefits estimator
healthy foods are expensive
risk of malnutrition may also be due to mobility issues, making it more difficult to get and prepare food
depression as result of social isolation or loss of loved one can have an effect on the desire to eat
health teaching important so patients make good choices for their health (vs for food companies/advertising)
older adult exercise
important for prevention of illness and maintained of independence (ex. maintain mobility)
regular exercise can help reduce incidence of chronic disease and maintain mobility, bone and muscle mass and importantly, independence
social connections
important for mental health adn can provide motivation
ex. to eat, to get out of the house and do something
Canadians with increased social participation demonstrated greater physical, psychological, social and self-rated wellness