Benign and Malignant Tumors of the Conjunctiva
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
conjunctival general anatomy
clear mucus membrane
over sclera = bulbar
eyelids = palpebral
redundant area at corner = fornix
conjunctival anatomy
tear film
conj epithelium
basal —> squamous
basal = melanocytes
goblet cells = produce mucin
helps tear film adhere to opical surface
basement membrane
barrier
lamina propria
adenoid layer
highly lymphatic
has lymphocytes (inflammatory cells)
blood supply
fibrous later
connective tissue
tensile strength
tenons capsule — not part of conj
sclera
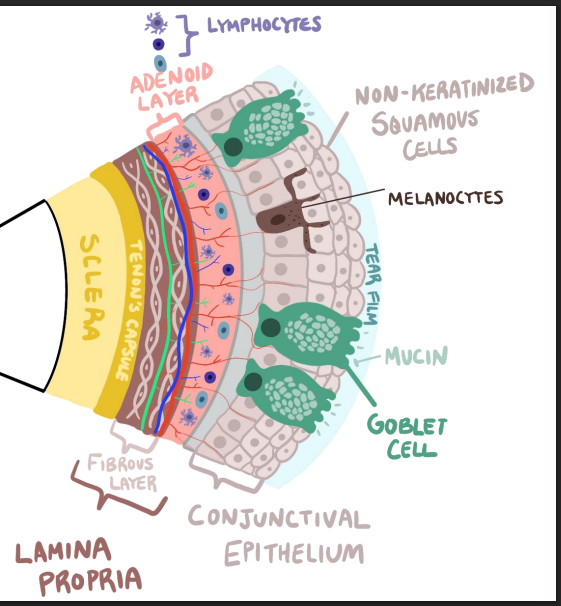
what is special ab squamous ep of conj
NON keratinized
what is a choristoma
Tumor-like growth composed of normal tissue in an abnormal location
what are the 2 choristomas
dermoid
dermolipoma
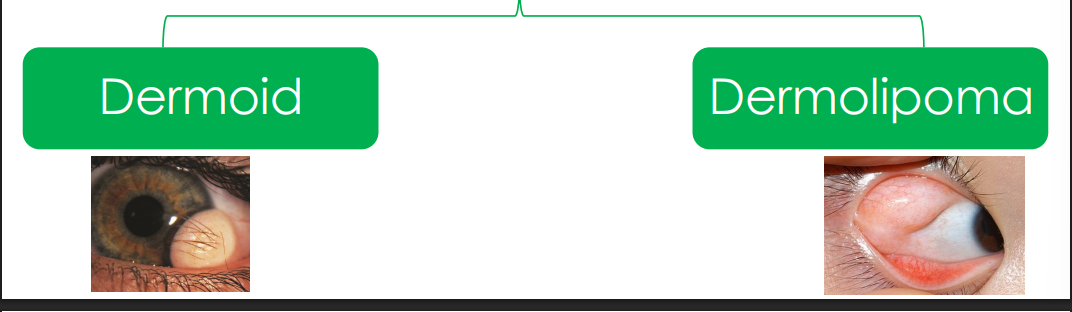
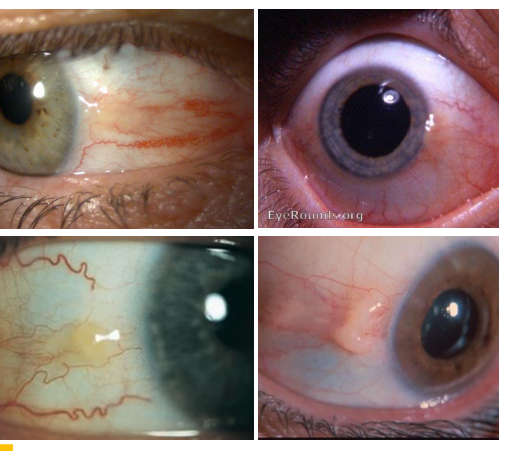
Conjunctival Dermoid cause
Benign congenital choristomas of conjunctiva
epi of conjunctival dermoid
random
clinically present in YA
can be associated w Goldenhar syndrome
eye, ear, spine
pathophys of conjunctival dermoid
“Sequestration” (separation of tissue) of conjunctival epithelium during development.
• Simple: One tissue type
• Complex: >1 tissue type
• Tissue can consist of pilosebaceous unit (hair), sweat glands, fat, skin, and connective tissue.
clinical presentation of conj dermoid
Variable size, yellow -white limbal mass often found Nasal quadrant
• May contain fine hairs .
• May have extensive corneal involvement causing irritation, astigmatism, and incomplete eyelid closure.
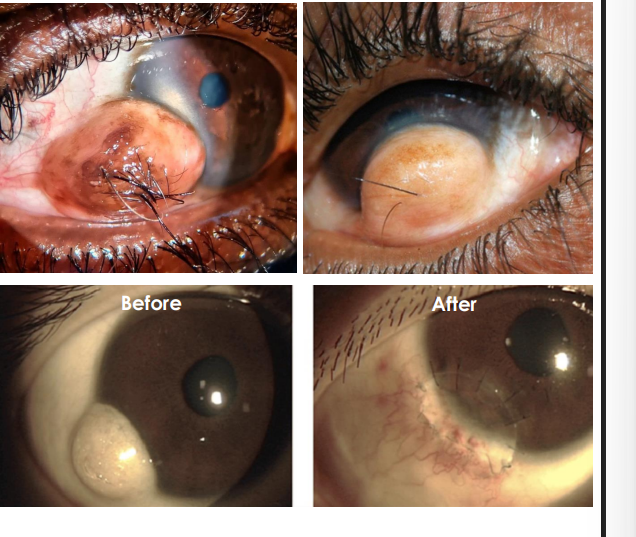
how do you treat conj dermoid
removal - if inducing astig, amblyopia, reducing vision, cosmesis
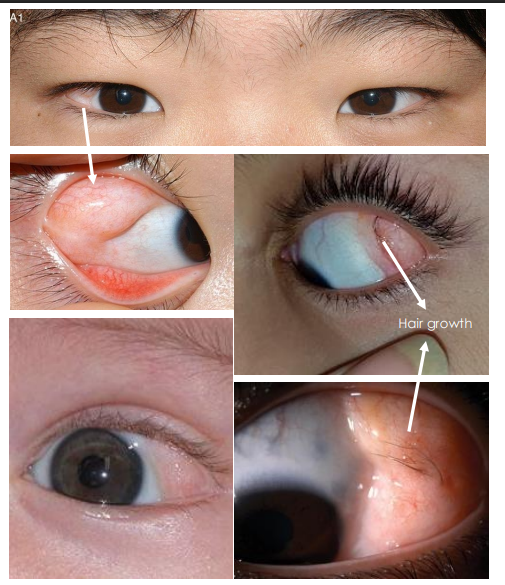
Conjunctival Dermolipoma epi
1st or 2nd decade of life
pathophys of conj dermolipoma
Consist of adipose (Fat) tissue and is contiguous with conjunctival epithelium Can also be associated with Goldenhar Syndrome
clinical presentation
• Less defined than dermoid, pale -white, soft “fatty” lesions fixed to the conjunctiva
• Can have fine hairs
• Location: Often at superotemporal fornix
what are the beningn ep tumors involving
conj ep
what are the 3 benign epithelial tumors
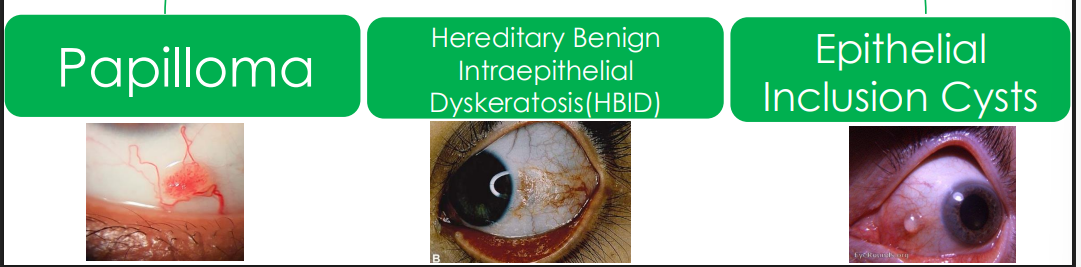
conj papilloma cause
like veracuca vulgaris
from HPV 6 and 11
pathophys of conj papilloma
Human Papilloma Virus is tumorigenic and promote squamous cell proliferation of conjunctival epithelium —> superficial
• Most often benign and low risk for malignancy potential
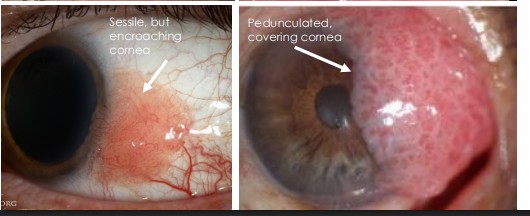
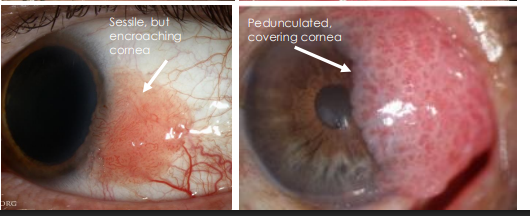
childhood form of conj papilloma appearance
• Single or multiple
• Sessile or pedunculated appearance
• Fleshy red appearance due to many fine vascular channels and has a vascular core
• Location: Inferior fornix, bulbar conjunctiva, rarely touching cornea
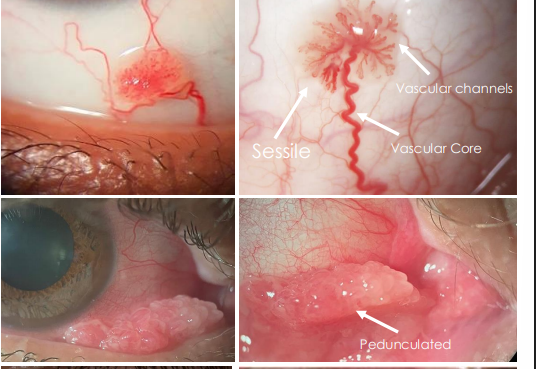
adult form of conj papilloma
resembles Conjunctival Intraepithelial neoplasia (CIN)
cant tell the difference
single and isolated
near limbus and can encroach or cover cornea
management of conj papilloma
excision
Hereditary Benign Intraepithelial Dyskeratosis(HBID) cause
Benign inherited disease of the conjunctival and oral mucosa
epi of Hereditary Benign Intraepithelial Dyskeratosis(HBID)
• Rare
• Autosomal dominance (AD) pattern of inheritance
• Native American heritage: Haliwa-Saponi tribe ancestry
• Predominantly in North Carolina region
• Onset is early childhood with periods of wax and waning
pathophys of Hereditary Benign Intraepithelial Dyskeratosis(HBID)
Exact unknown, abnormally thickened squamous epithelium and keratinization of conjunctiva and oral mucosa.
so interferes w tear film
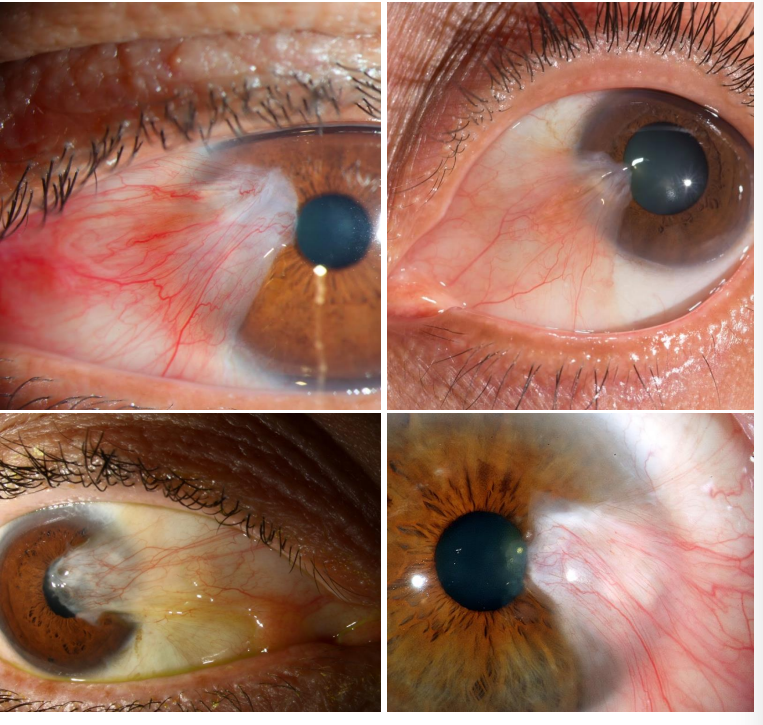
Hereditary Benign Intraepithelial Dyskeratosis(HBID) appearance
• Bilateral conjunctival injection (redness)
• Dilated conjunctival vessels giving red eye appearance
• Bilateral white -gray, painless, elevated gelatinous, spongy, plaques
• Location: nasal or temporal perilimbal area with possible extension onto cornea
• Also apparent on oral cavity • Mouth, lip, tongue
management of HBID
treat ocular surface (DED) from it
can excise plaques if it affects it — they come back
Conjunctival Epithelial Inclusion Cyst cause
• Primary form is congenital
• Secondary form is spontaneous or due to inflammation, trauma or surgery
pathophys of Conjunctival Epithelial Inclusion Cyst
Inclusion of conjunctival epithelium into the substantia propria (stromal region) forming a cystic cavity filled with shed cells or mucoid material
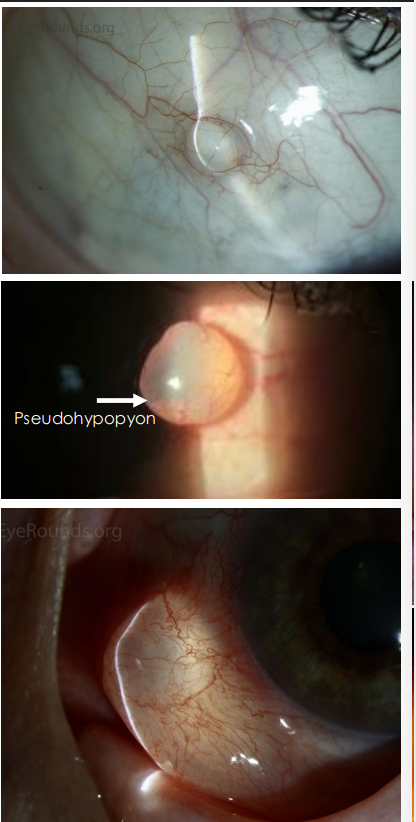
appearance of Conjunctival Epithelial Inclusion Cyst
• Smooth, thin-walled cyst filled with clear serous fluid
• Epithelial debris settles on the bottom forming “pseudohypopyon”
whats the 3 benign melanocytic tumors
melanocytic nevus
ocular melanocytosis
complxion associated melanosis (CAM)
Conjunctival Melanocytic Nevus cause
Congenital lesions consisting of nests of melanocytes
epi of Conjunctival Melanocytic Nevus
• Caucasians> Blacks>Asians, Hispanics
• Malignant transformation <1%
• Onset since birth/childhood - congenital
• Most common pigmented conjunctival tumor
Conjunctival Melanocytic Nevus pathophys
Infiltration of distinct nest of benign melanocytes near the basal layer of conjunctival epithelium and migrates into underlying stroma with age
3 stages
junctional
compound
subethileal
junctional Conjunctival Melanocytic Nevus appearance
solitary
range of pigmentation
flesh to dark
interpalpebral bulbar conj
junctional
younger age
flatter
less pigment
at ep

compound Conjunctival Melanocytic Nevus appearance
solitary
range of pigmentation
flesh to dark
interpalpebral bulbar conj
compound
adults
development of cysts
at level of stroma and protruding in ep

subepithelial Conjunctival Melanocytic Nevus appearance
solitary
range of pigmentation
flesh to dark
interpalpebral bulbar conj
subepithelial
older adults
less pigmented
pseudocyts
level of stroma entirely wo ep component
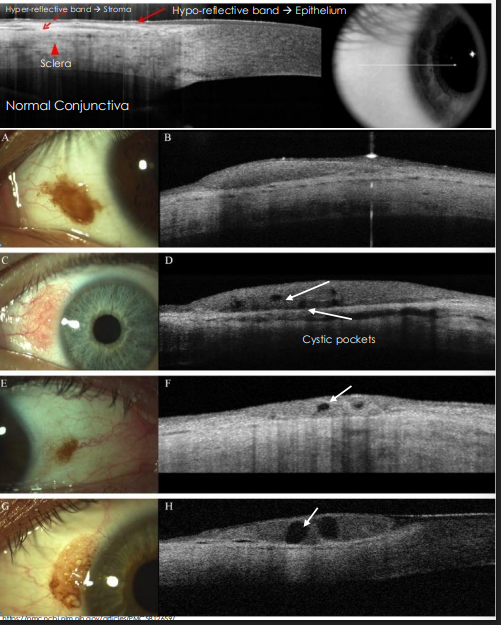
normal oct of conjunctiva
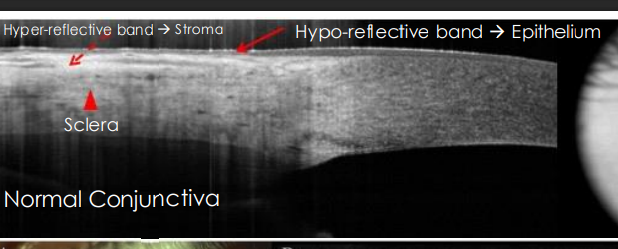
assessing conj melanocytic nevus
OCT - Anterior Segment
melanocytic nevus —> often have cysts!!
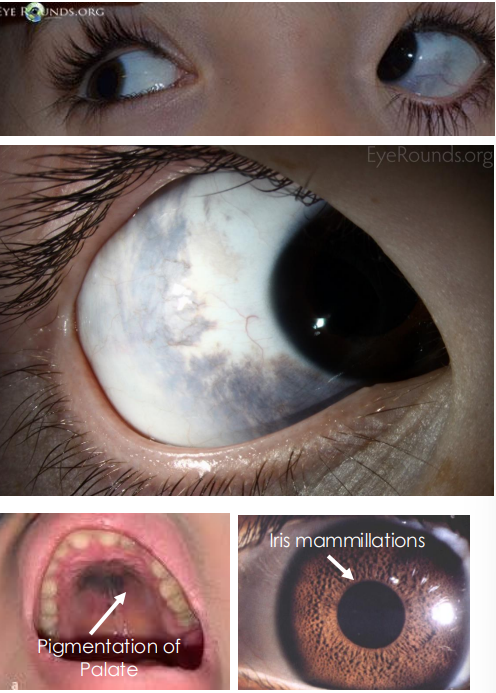
ocular melanocytosis — nevus of ota cause
Congenital pigmentation of periocular skin, uveal tract, sclera sometimes orbits, meninges, and palate.
IF skin involved → Nevus of Ota
epi of ocular melanocytosis
• Present at birth or during 1st year of life •
More common in Asians and blacks, Females > Males
• HOWEVER, Higher risk of malignant uveal melanomas in whites 1:400
clinical presentation of ocular melanocytosis
• Flat, blue-grayish, patchy pigmentation of conjunctiva and sclera; Tends to follow CN 5 V1 & V2 distribution • Can have iris mammillations • Often Unilateral, bilateral in only10% cases • Risk of congenital glaucoma
Complexion Associated Melanosis (CAM) aka
racial melanosis
cuase of CAM
Also known as racial melanosis, benign melanocytic lesion found among darkly pigmented individuals present since childhood or birth
pathophys of Complexion Associated Melanosis (CAM)
Hyperpigmentation of the basal epithelium without melanocytic proliferation, melanocytes are contained to level of basal epithelium without hyperplasia
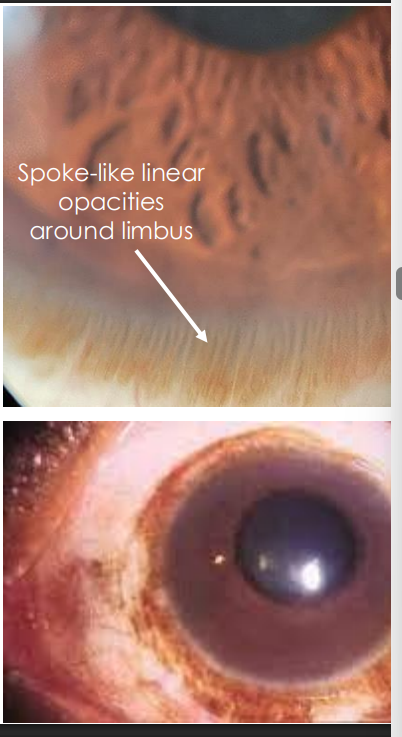
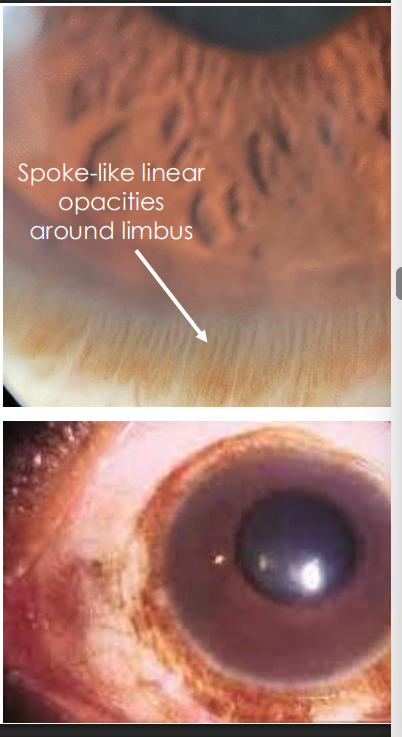
CAM presentation
• Typically bilateral
• Flat, non-cystic pigmentation that can cover the conjunctiva extensively and increase in size with age
• Ill-defined margins
• May have spoke-like appearance
• Location: around corneoscleral limbus
what are the benign vascular/lymphatic tumors (3)
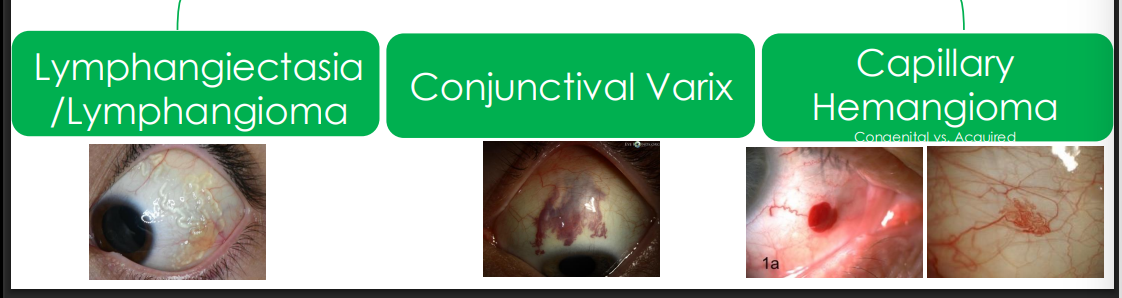
Lymphangiectasia/ Lymphangioma cause
• Congenital form related to developmental disorders.
• Acquired form may be related to trauma, inflammation, or radiation.
Lymphangiectasia/ Lymphangioma pathophys
• Dilated and prominent lymphatic channels of conjunctiva → Lymphangiectasia — string of pearls — looks like mucus on conj
• When it becomes mass-like and diffuse →Lymphangioma
• Filled with lymph fluid (clear)
Lymphangiectasia/ Lymphangioma presentation
• Diffuse distribution of lymph with chemosis
• Localized appearance, "string of pearls”
• Bleeding into lymph channels cause hemorrhagic lymphangiectasia
Conjunctival Varix cause
Venous malformation that is typically an extension of orbital varix, often rarer to be isolated to conjunctiva only
Conjunctival Varix pathophys
One or more dilated venous channels caused by vascular dysgenesis leading to thrombosis
Conjunctival Varix appearance
• Large distinct blood vessels
• May have faint blue-black color
• Freely mobile and not fixed to the sclera
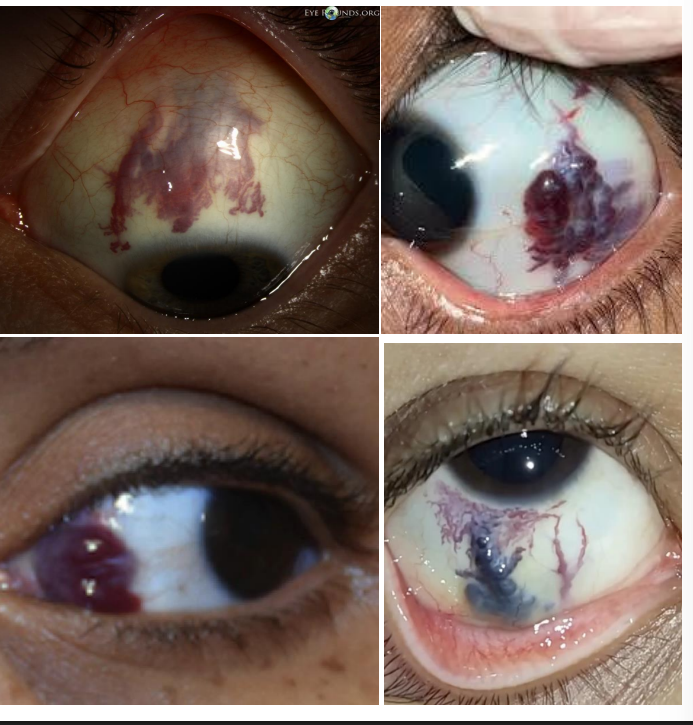
managing Conjunctival Varix
• Isolated conjunctival varix is asymptomatic but may be excised for cosmetic considerations •
Consider orbital varix with proptosis, pain, optic nerve compression.
Conjunctival Capillary Hemangioma congenital pathophys
Vascular endothelial cell proliferation filled with blood - congenital
clinical presentation of congenital Conjunctival Capillary Hemangioma
• Solitary, distinct, red mass, variable size
• Unilatera
l • May progressively enlarge for up to 2 years then gradually spontaneously regress
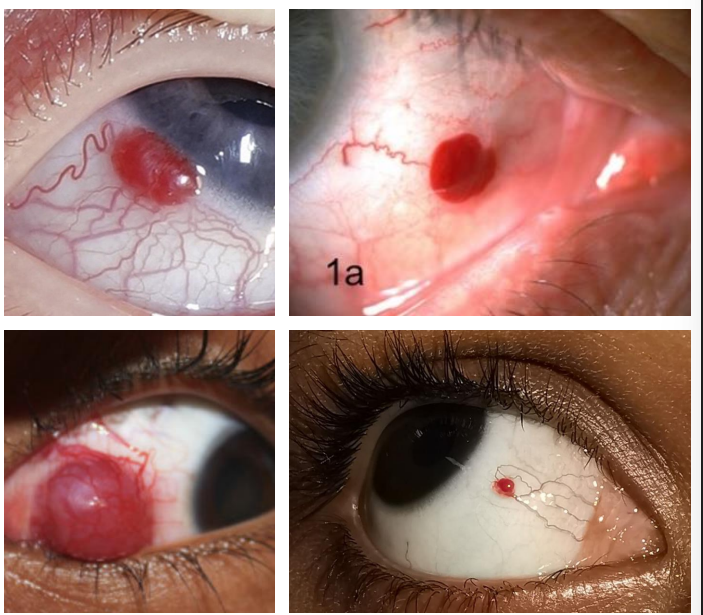
acquired capillary hemangioma clinical presentation
• Sessile/immobile, flat lesion with convoluted intertwining blood vessels
• Often smaller in size
• Often remain stable in size without growth
what are other benign lesions
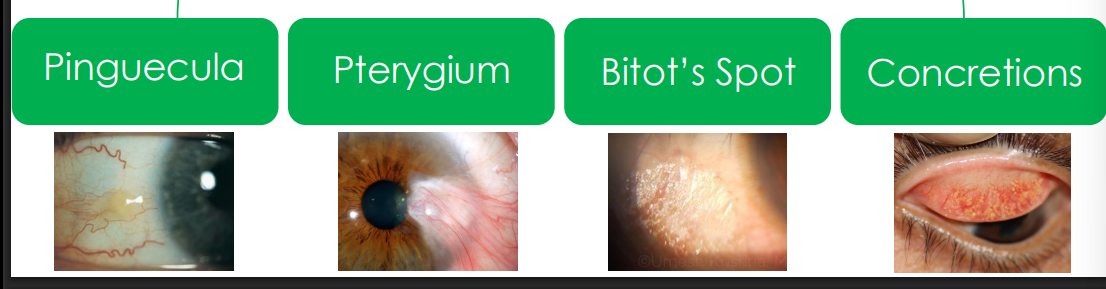
pingeucula pathophys
Related to excessive exposure to UV light, dust, wind and other harsh elements
Zone of thickened conjunctival stroma replaced by degenerated collagen and abnormal elastic tissue
pinguecula pathophys
Zone of thickened conjunctival stroma replaced by degenerated collagen and abnormal elastic tissue
pinguecula clinical presentation
Localized, yellow-gray, slightly elevated lesion
• Unilateral or bilateral
• Location: nasal and temporal near limbus
pterygium cause
Related to excessive exposure to UV light, dust, wind and other harsh elements
pterygium pathophys
like pinguecula w invasion of fibrovascular tissue into corneal Bowmans layer
pterygium clinical presentation
• Dragging of conjunctival tissue and blood vessels across the cornea •
Triangular appearance •
Location: Pinguecula extending onto superficial cornea, nasal and temporal
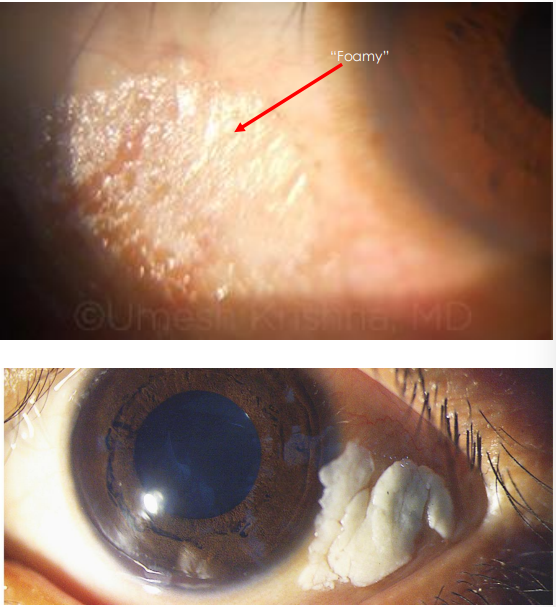
Bitot’s spots cause
Belongs to a range of ocular manifestations called xerophthalmia because of Vitamin A Deficiency (VAD)
epi of bitots spots
• In developing countries •
Malnourished individuals •
Pregnant and nursing mothers
• In developed countries
• Patient with GI disorder = malabsorption •
Patients with liver, bowel, pancreatic disease = impaired Vit A storage
• Patients on strict vegetarian or vegan diets
pathophys of bitots spots
1, • Vitamin A required for normal epithelium
• VAD → Abnormal conjunctival epithelium keratinization
bitots spot appearance
• White-Grayish triangular patches of xerosed (dried) conjunctiva with foamy surface •
The tear film does not “wet” the surface •
Location: Temporal conjunctiva, Often bilateral
concretions pathophys
Degenerated epithelial cells and proteins become trapped in subconjunctival space and become calcified
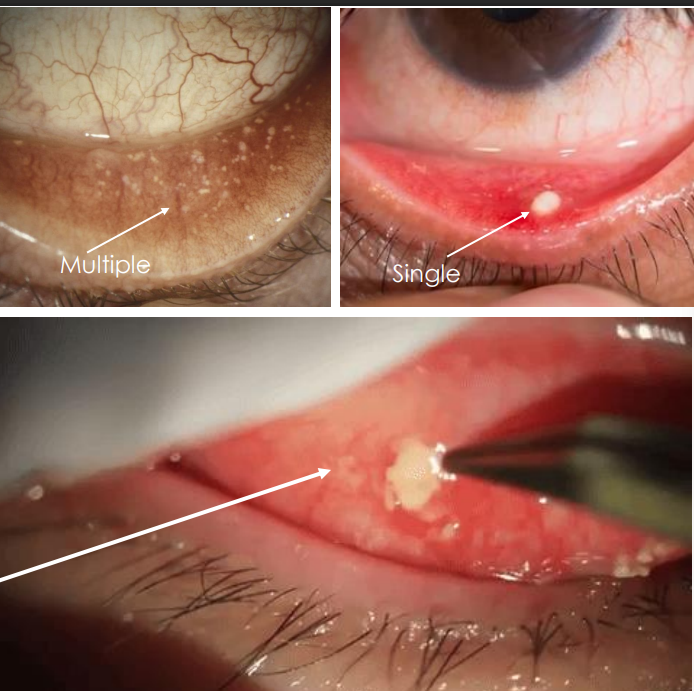
what are these
concretions
management of concretions
• Remove with forceps or needle if eroding through epithelium and causing foreign body sensation
what are the premalignant lesions

primary acquired melanosis (PAM) epi
• Found in lighter pigmented individuals
• 50% progress to melanoma
• Onset is middle aged and older
pathophys of PAM - premalignant
Abnormal melanocytes in the basal layers of epithelium
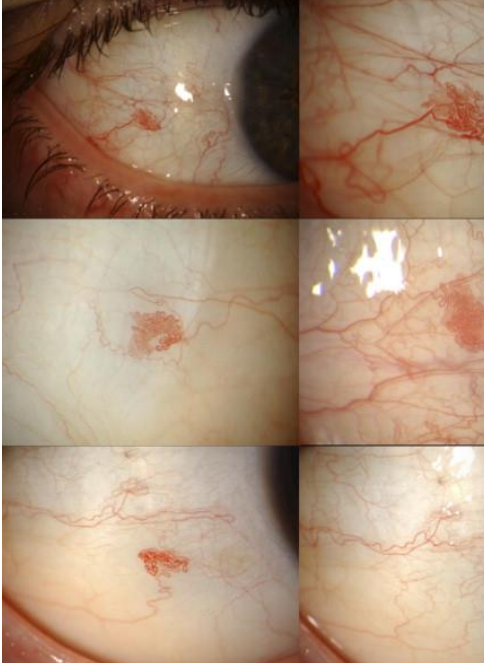
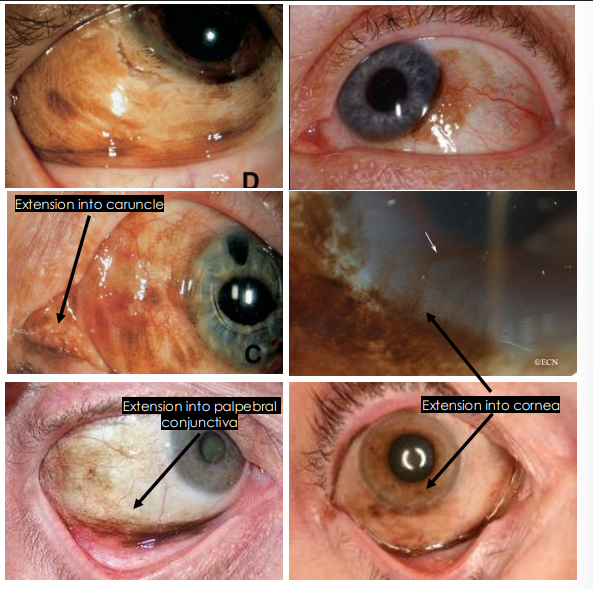
PAM appearance
• Almost always unilateral
• Flat, diffuse, ill-defined borders
• Varies in pigment from light to dark brown
• Location: limbus and bulbar conjunctiva, can extend to palpebral conjunctiva, caruncle, cornea and eyelid = more suspicious
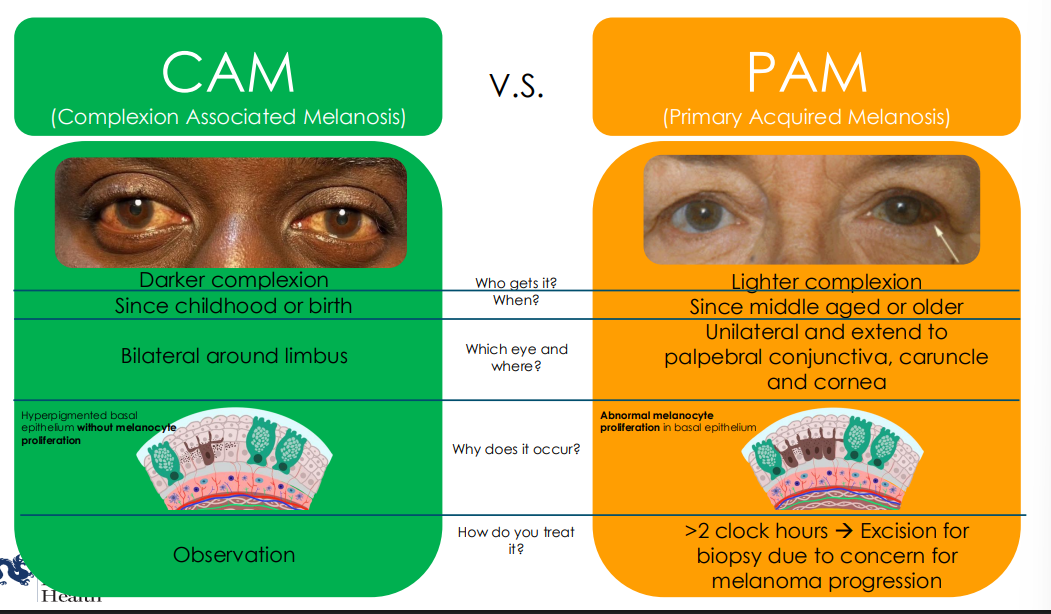
CAM vs PAM
CAM
darker complexion
since childhood or birth
bilatral around limbus
no melanocyte proliferation
observe
PAM
lighter complexion
since middle aged or older
unilateral and can extend to palpebral conj, caruncle, cornea
abnormal melanocyte proliferation
treat if >2 clock hours —> biopsy for concern of melanoma
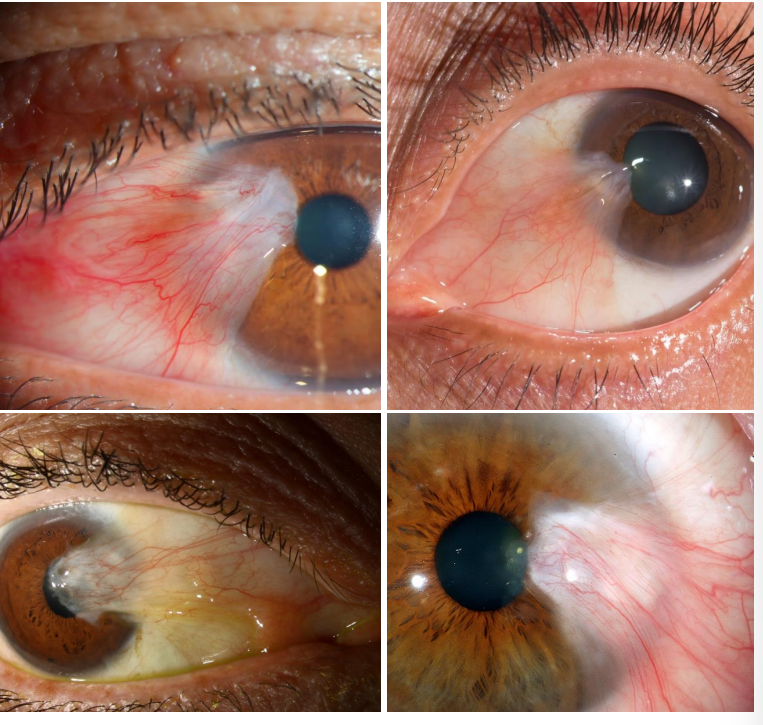
Conjunctival Intraepithelial Neoplasia (CIN) cause
Acquired precancerous lesion arising from various environmental and genetic risk factors
epi/risk factors of CIN
• Fair skinned individuals
• Middle-aged or older individuals
• History of chronic UV exposure •
Immunosuppressed individuals such as those with HIV
• Tobacco use, exposure to petroleum products
• Infection with Human papilloma virus (HPV 16, 18)

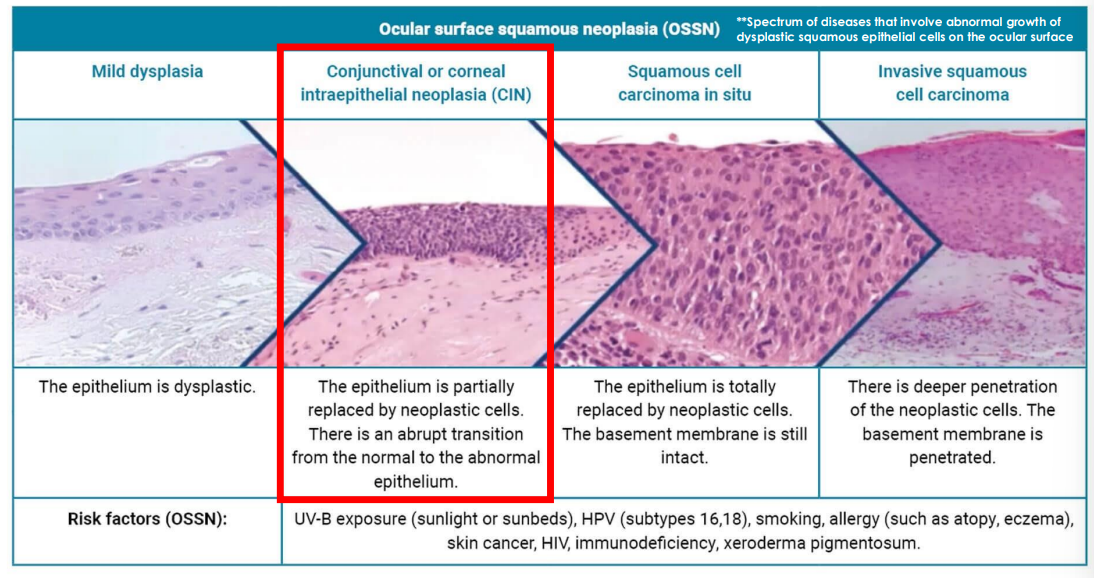
pathophys of CIN
Slow growing, non-invasive, localized tumor with thickened, mutated, and irregular epithelial cell arising from limbal stem cells;
however, basement membrane is intact and underlying substantia propria is spared
• Precursor to squamous cell carcinoma
CIN belongs to what disease
OSSN
ocular surface corneal intraepithelial neoplasia
papilliform of CIN appearance
• Fleshy, papillomatous appearance
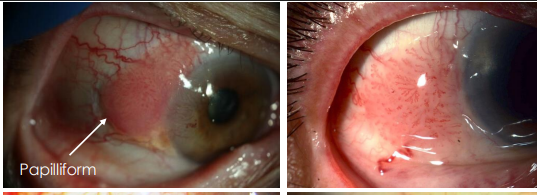
gelatinous from of CIN appearance
• Hairpin configuration of vessels around a sessile/flat lesion
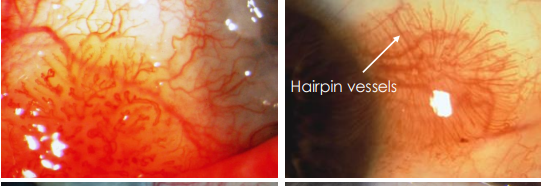
leukoplakic form of CIN appearance
• Whitened and thickened surface with surface hyper -keratinization
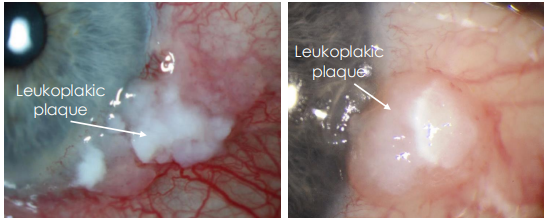
what is true of all CIN appearance
Typically mobile, can have feeder vessels
• Location:
• Common: Limbus and interpalpebral bulbar conjunctiva (nasal & temporal)
• Less common: palpebral conjunctiva and fornix
additional assesment of CIN
OCT ant seg
high resoln!!!
Distinctive, thickened hyperreflective epithelial layer with an abrupt transition from normal to abnormal epithelium
NO CYSTIC POCKETS
rose bengal or lissamine green vital dye
(+) staining/ stipping
stain dying cells
can delineate extent of CIN but non specific
managing CIN
Complete excision recommended
• Surgical •
Chemotherapeutics
what are the malignant conj tumors
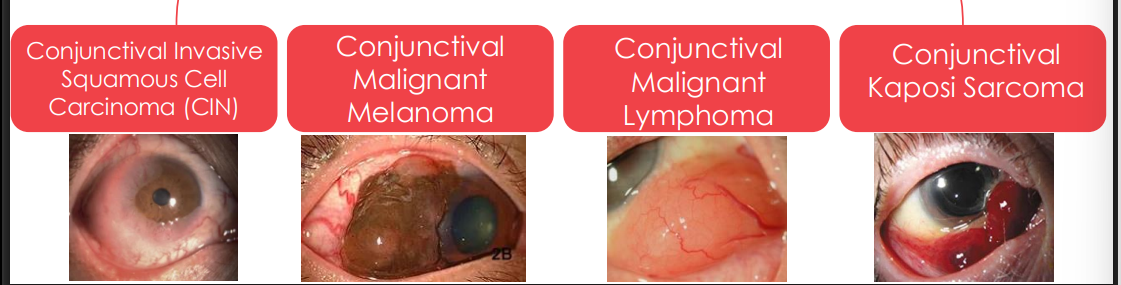
Conjunctival Invasive Squamous Cell Carcinoma cause/pathophys
CIN is precursor
Acquired cancerous lesion arising from precursor lesions such as Conjunctival Intraepithelial Neoplasia (CIN).
a (CIN) breaches the basement membrane of epithelium and invades underlying stroma and other structures
clinical presentation of Conjunctival Invasive Squamous Cell Carcinoma
Similar to Conjunctival Intraepithelial Neoplasia (CIN), difficult to clinically differentiate between the two
• Can have all characteristics of CIN:
• Papillomatous, Gelatinous, Lekoplakic
• Can have: • (+) large, dilated feeder vessels
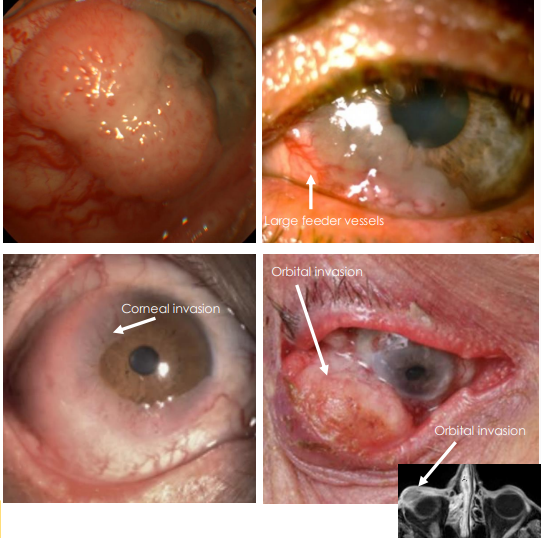
location of Conjunctival Invasive Squamous Cell Carcinoma
Limbus and interpalpebral bulbar conjunctival (nasal & temporal) and can invade into cornea, orbit and globe —> invasive
Conjunctival Malignant Melanoma cause
Acquired cancerous melanocytic lesion that either arise from:
Primary acquired melanosis (PAM)* *Most common
Conjunctival nevus
. De novo (no pre-existing lesion)
pathophys of Conjunctival Malignant Melanoma
Malignant melanocytes that invade the conjunctival stroma and have access to lymphatic channels for metastasis → brain, liver, skin and bone
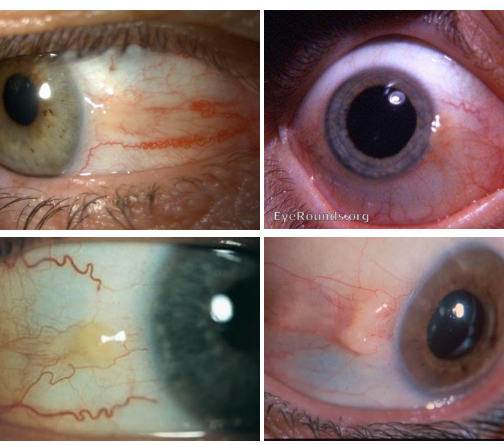
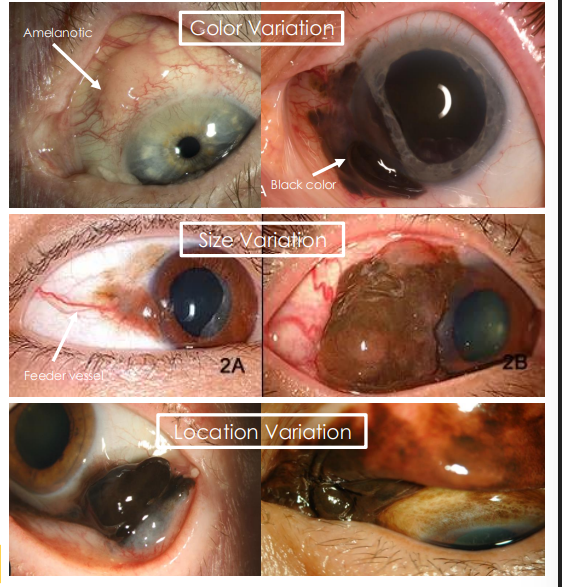
Conjunctival Malignant Melanoma presentation
• Pigmented, elevated lesion with illdefined margins
• Can range in pigment: black to flesh colored (amelanotic)
• May have feeder vessels
• Can range in size
• Location:
• More common: bulbar conjunctiva near
• Less common: fornix or palpebral conjunctiva
pathophys of Conjunctival Malignant Lymphoma
Lymphoma is monoclonal proliferation of B and T lymphocytes
• Uncontrolled replication of single mutated lymphocyte
• Most common subtype of conjunctival lymphoma is:
• Non-Hodgkin, Extra-nodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT-type lymphoma)
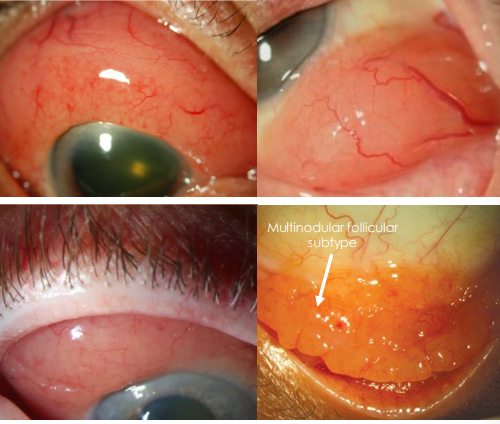
conjunctival malignant lymphoma clinical presentation
• Diffuse, slightly elevated, fleshy pink mass
• Salmon patch
• “Chemotic” appearance
• Mimics inflammatory conjunctivitis
• Most often smooth but follicular subtype has multinodular appearance
• Location:
• More common: Fornix, superior and inferior bulbar conjunctiva
• Less common: Limbus
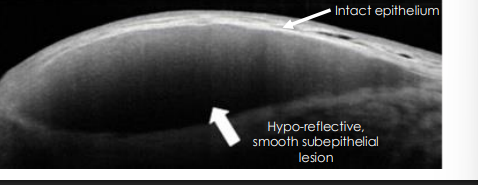
how else can we assess conjunctival malingnant lymphoma
OCT (high resoln)
hyporefelctive/dark
smoooth subepithelial lesion
conj Kaposi sarcoma review
HPV 8 - cause
AIDS/ renal transplant
males
Network of proliferating malignant vascular endothelial cells with blood filled spaces
single - multiple red, purple, brown, blue lesions
locations wi ocualr structures
• Eyelid, conjunctiva (bulbar, palpebral, caruncle), lacrimal sac