Unit 5 - Cervicothoracic Spine II
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
Pathoanatomy: Neck Pain with Headaches
What is the proposed underlying cause of neck pain with headaches?
Cervicogenic Headaches (CGH)
Disorder of the cervical spine and its component bony, disk, and/or soft tissue elements
Cervical Spine Impairments
Upper cervical spine (C0/C1, C1/C2, C2/C3) facet joint impairments
Muscle impairments including myofascial trigger points
Medical Screening: Neck Pain with Headaches
What other conditions should be considered with this patient presentation?
Viscerogenic
Neoplastic conditions
• Inflammatory or systemic disease
• Cardiopulmonary conditions
• Cervical vascular pathology
Medical Screening: Neck Pain with Headaches
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Spinal fracture
Cervical myelopathy
Upper cervical ligamentous instability
Differential Diagnosis: Neck Pain with Headaches
What other conditions should be considered with this patient presentation?
Primary Headaches
Migraine without aura
Migraine with aura
Frequent episodic tension-type
Chronic tension-type
Cluster headache (trigeminal autonomic cephalgia)
Differential Diagnosis: Neck Pain with Headaches
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Neck pain with movement coordination impairments (WAD)
Temporomandibular disorders
Subjective Examination: Neck Pain with Headaches
What system, structure, pain mechanism, and phases of healing are unique to this patient presentation?
System
Musculoskeletal
Structure
Zygapophyseal joint, muscle (myofascial trigger points)
Pain mechanism
Nociceptive
Phase of healing
None
Subjective Examination: Neck Pain with Headaches
What are common subjective reports for neck pain with headache?
General symptoms
Noncontinuous unilateral neck and associated (referred) headache
Unilateral headache with onset preceded by neck pain
Headache aggravated by neck movements or sustained positions
Symptoms progress occipital to frontal in a ram's horn distribution
Subjective Examination: Neck Pain with Headaches
What are common subjective reports for neck pain with headache?
Nociceptive Pain
Clear, proportionate mechanical/anatomic nature to aggravating and easing factors
Localized pain with/without somatic referral
Usually rapidly resolving in accordance with expected recovery times
Often intermittent and sharp with movement/mechanical provocation
May have more constant dull ache or throb at rest
Responsive to simple analgesics/NSAIDs
Clear diurnal or 24-hr pain pattern
Subjective Examination: Neck Pain with Headaches
What are common subjective reports for neck pain with headache?
Aggravating factors
Dull ache with sustained positions
Symptoms reproduced with active movements
Subjective Examination: Neck Pain with Headaches
What are common subjective reports for neck pain with headache?
Easing factors
Frequent change of positions
Progressive cervical spine movement
Subjective Examination: Neck Pain with Headaches
What are common subjective reports for neck pain with headache?
2-hour pain behavior
Morning
Rarely morning pain unless neck maintained in an awkward position
Noon to evening
Symptoms may vary throughout the day depending on the patient’s activities, may have increased pain with sustain positions or specific movements
Night
Symptoms may disturb depending on sleeping positions, severity and irritability
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
Systems review (as indicated from the subjective exam): Cardiopulmonary
Vitals
BP, HR, auscultate
Assess for mechanical reproduction of symptoms and/or adverse response to movement
AROM, PIVM, compression/distraction, neurodynamic tests
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
Systems review (as indicated from the subjective exam): Neuromusculoskeletal
Cranial nerves
Reflexes/pathological reflexes
Dermatomes/myotomes
Upper cervical ligamentous testing
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
specific tests and measures
muscle performance exam
MLT
muscle palpation
muscle endurance, coordination, and strength
ICHD-3 diagnostic criteria
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
MLT
Limited length of the cervicothoracic musculature
Upper trapezius, levator scapulae, scalenes, suboccipitals, SCM, pec minor/major
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
Muscle palpation
Active and latent myofascial trigger points of the cervicothoracic musculature
Upper trapezius, SCM, suboccipitals, temporalis, splenius capitis and cervicis, semispinalis capititis
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
Muscle endurance, coordination, and strength
Longus capitus and longus colli
Cervical multifidus
Middle and lower trapezius
Rhomboids and serratus anterior
Physical Examination: Neck Pain with Headaches
What are the key examination procedures for neck pain with headache?
ICHD-3 diagnostic criteria
Evidence of causation demonstrated by at least two of the following:
Headache has developed in temporal relation to the onset of the cervical disorder or appearance of the lesion
Headache has significantly improved or resolved in parallel with improvement in or resolution of the cervical disorder or lesion
Cervical range of motion is reduced, and headache is made significantly worse by provocative maneuvers
Headache is abolished following diagnostic blockade of a cervical structure or its nerve supply
Prognosis: Neck Pain with Headaches
What is the prognosis of the condition?
Clinical course and prognosis
• Acute idiopathic neck pain has variable recovery with slowing of progress noted at 6-12 weeks from onset
Chronic non-specific, atraumatic neck pain may be stable or fluctuating with periods of improvement and worsening
Prognosis: Neck Pain with Headaches
What is the prognosis of the condition?
Factors that may impact prognosis
Older age
Prior history of musculoskeletal disorders
Prior health
Regular exercise
History of previous neck pain
Sick leave
Prognosis: Neck Pain with Headaches
What is the prognosis of the condition?
Factors that may impact new onset or recurrence
Female gender
History of previous neck pain
Older age
High demand jobs
History of smoking
Low social support
History of previous low back pain
Stage of Condition: Neck Pain with Headaches
How does this present differently based on stage of condition?
Acute
Severity and irritability are often high
Pain at rest or with initial to mid-range spinal movements: before tissue resistance
Pain control is often the intervention goal at this stage
Stage of Condition: Neck Pain with Headaches
How does this present differently based on stage of condition?
Subacute
Severity and irritability are often moderate
Pain experienced with mid-range motions that worsen with end-range spinal movements: at tissue resistance
Movement control is often the intervention goal at this stage
Stage of Condition: Neck Pain with Headaches
How does this present differently based on stage of condition?
Chronic
Severity and irritability are often low
Pain that worsens with sustained end-range spinal movements or positions: overpressure into tissue resistance
Functional optimization is often the intervention goal at this stage
Interventions: Neck Pain with Headaches
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Acute
Exercise
C1/C2 self-sustained natural apophyseal glide (SNAG)
Interventions: Neck Pain with Headaches
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Subacute
Exercise
C1/C2 self-sustained natural apophyseal glide (SNAG)
Manual therapy
Cervical mobilization and manipulation
Interventions: Neck Pain with Headaches
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Chronic
Exercise
Combined cervicoscapulothoracic exercise including endurance, neuromuscular re-education with/or without biofeedback, stretching, and strengthening elements
Manual therapy
Cervicothoracic manipulation and mobilization
Interventions: Neck Pain with Headaches
When should we consider interprofessional referral and what are other treatment options?
Imaging
In the absence of red flag signs and for those classified as low risk, imaging is not indicated
Medications/injections
NSAIDs
Facet joint injections
Radiofrequency ablation
Pathoanatomy: Neck Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
“Direct pathoanatomical causes of mechanical neck pain are rarely identifiable.”
“Although the cause of neck pain may be associated with degenerative processes or pathology identified during diagnostic imaging, the tissue that is causing a patient’s neck pain is most often unknown.”4
“There are numerous anatomical structures in the cervical region that can be sources of nociception, including zygapophyseal joints, vertebrae, muscles, ligaments, neural structures, and the intervertebral disc.”
“Evidence is lacking to support the hypothesis that these pathoanatomical features are a primary source of mechanical neck pain across the age spectrum in the majority of patients.”
spondylosis
sprain / strain
Pathoanatomy: Neck Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Spondylosis
Gradual progression of age-related joint changes
Adaptive shortening of the joint connective tissue and periarticular soft tissue
Pathoanatomy: Neck Pain with Mobility Deficits
What is the proposed underlying cause of the condition?
Sprain / Strain
Acute onset sudden awkward movement causing
Muscle strain and/or ligament sprain
Primary/secondary disk-related condition
Intra-articular meniscus entrapment
Medical Screening: Neck Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Viscerogenic
Neoplastic conditions
Inflammatory or systemic disease
Cardiopulmonary conditions
Cervical vascular pathology
Medical Screening: Neck Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Spinal fracture
Cervical myelopathy
Upper cervical ligamentous instability
Differential Diagnosis: Neck Pain with Mobility Deficits
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Neck pain with movement coordination impairments
Neck pain with radiating pain
Rotator cuff related shoulder pain
Thoracic and/or rib pain with mobility deficits
Subjective Examination: Neck Pain with Mobility Deficits
What system, structure, pain mechanism, and phases of healing are unique to this patient presentation?
System
Musculoskeletal
Structure
Zygapophyseal joint and periarticular soft tissue
Pain mechanism
Nociceptive
Phase of healing
Muscle strain 2-4 weeks, ligament sprain and cartilage injuries 10-12 weeks
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
General symptoms
Central or unilateral symptoms
Possible (somatic referred) upper extremity pain
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Spondylosis Symptoms
Gradual onset with progressive loss of motion
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Sprain/strain Symptoms
Immediate onset of pain and loss of motion
Recent unguarded/awkward movement or position
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Nociceptive pain
Clear, proportionate mechanical/anatomic nature to aggravating and easing factors
Localized pain with/without somatic referral
Usually rapidly resolving in accordance with expected recovery times
Often intermittent and sharp with movement/mechanical provocation
May have more constant dull ache or throb at rest
Responsive to simple analgesics/NSAIDs
Clear diurnal or 24-hr pain pattern
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Aggravating factors
Dull ache and stiffness with inactivity
Symptoms reproduced with certain active movements which may be sharp
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
Easing factors
Staying active
Progressive cervical spine movement
Subjective Examination: Neck Pain with Mobility Deficits
What are common subjective reports for patients with mobility deficits?
24-hour pain behavior
Morning
May have pain and stiffness that is worse upon waking that eases with activity and movement
Noon to evening
Symptoms may vary throughout the day depending on the patient’s activities, may have increased pain and stiffness after being sedentary
Night
Symptoms may disrupt sleep with changing positions depending on symptom irritability
Physical Examination: Neck Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Systems review (as indicated from the subjective exam): Cardiopulmonary
Vitals
BP, HR, auscultate
Assess for mechanical reproduction of symptoms and/or adverse response to movement
AROM, PIVM, compression/distraction
Physical Examination: Neck Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Systems review (as indicated from the subjective exam): Neuromusculoskeletal
Cranial nerves
Reflexes/pathological reflexes
Dermatomes/myotomes
Upper cervical ligamentous testing
Physical Examination: Neck Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Specific Tests and Measures
Movement and provocation exam
Active range of motion
Passive intervertebral motion (PIVM)
Diagnostic test-item cluster
Physical Examination: Neck Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Active range of motion
Cervical range of motion limitations and symptom provocation consistently reproduced at end range
Symptom provocation with the addition of overpressure and/or combined motions
Physical Examination: Neck Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Passive intervertebral motion (PIVM)
Hypomobility of the cervicothoracic spine with characteristic pattern of restriction
Hypomobility of the involved segment(s) with local and/or somatic referred symptom reproduction
Physical Examination: Neck Pain with Mobility Deficits
What are the key examination procedures for patients with mobility deficits?
Diagnostic test-item cluster
Younger Individual (age < 50 years)
Acute neck pain (duration < 12 weeks)
Symptoms isolated to the neck
Restricted cervical range of motion
Prognosis: Neck Pain with Mobility Deficits
What is the prognosis of the condition?
Clinical course and prognosis
Acute idiopathic neck pain has variable recovery with slowing of progress noted at 6-12 weeks from onset
Chronic non-specific, atraumatic neck pain may be stable or fluctuating with periods of improvement and worsening
Prognosis: Neck Pain with Mobility Deficits
What is the prognosis of the condition?
Factors that may impact prognosis
Older age
Prior history of musculoskeletal disorders
Prior health
Regular exercise
History of previous neck pain
Sick leave
Prognosis: Neck Pain with Mobility Deficits
What is the prognosis of the condition?
Factors that may impact new onset or recurrence
Female gender
History of previous neck pain
Older age
High demand jobs
History of smoking
Low social support
History of previous low back pain
Stage of Condition: Neck Pain with Mobility Deficits
How does this present differently based on stage of condition?
Acute
Severity and irritability are often high
Pain at rest or with initial to mid-range spinal movements: before tissue resistance
Pain control is often the intervention goal at this stage
Stage of Condition: Neck Pain with Mobility Deficits
How does this present differently based on stage of condition?
Subacute
Severity and irritability are often moderate
Pain experienced with mid-range motions that worsen with end-range spinal movements: at tissue resistance
Movement control is often the intervention goal at this stage
Stage of Condition: Neck Pain with Mobility Deficits
How does this present differently based on stage of condition?
Chronic
Severity and irritability are often low
Pain that worsens with sustained end-range spinal movements or positions: overpressure into tissue resistance
Functional optimization is often the intervention goal at this stage
Interventions: Neck Pain with Mobility Deficits
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Acute
Education
General exercise and patient education to stay active
Exercise
Cervical ROM, stretching, and isometric strengthening
Supervised exercise, including interventions for cervicoscapulothoracic strengthening, stretching, and endurance training
Manual therapy
Thoracic manipulation
Cervical mobilization and/or manipulation
Interventions: Neck Pain with Mobility Deficits
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Subacute
Exercise
Cervicoscapulothoracic endurance exercise
Manual therapy
Thoracic manipulation
Cervical mobilization and/or manipulation
Interventions: Neck Pain with Mobility Deficits
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Chronic
Education
“Stay active” lifestyle approaches
Exercise
Combined cervicoscapulothoracic exercise
Mixed exercise for cervicoscapulothoracic regions including coordination, proprioception, postural training, aerobic conditioning, and cognitive effective elements
Manual therapy
Thoracic manipulation and cervical mobilization
Biophysical agents
Dry needling, TENS, low-level laser, pulsed or high-powered ultrasound, intermittent mechanical traction, repetitive brain stimulation, and electrical muscle stimulation
Interventions: Neck Pain with Mobility Deficits
What additonal interventions are recommended for this condition?
Clinical Prediction Rule
3/4 (+LR 13.5; 90% probability)
Symptom duration less than 38 days
A positive expectation that manipulation will help
Side-to-side difference in cervical rotation ROM of 10 degrees or greater
Pain with posteroanterior spring testing of the middle cervical spine
Interventions: Neck Pain with Mobility Deficits
When should we consider interprofessional referral and what are other treatment options?
Imaging
In the absence of red flag signs and for those classified as low risk, imaging is not indicated
Medical Intervention
Medications/injections
NSAIDs
Facet joint injections
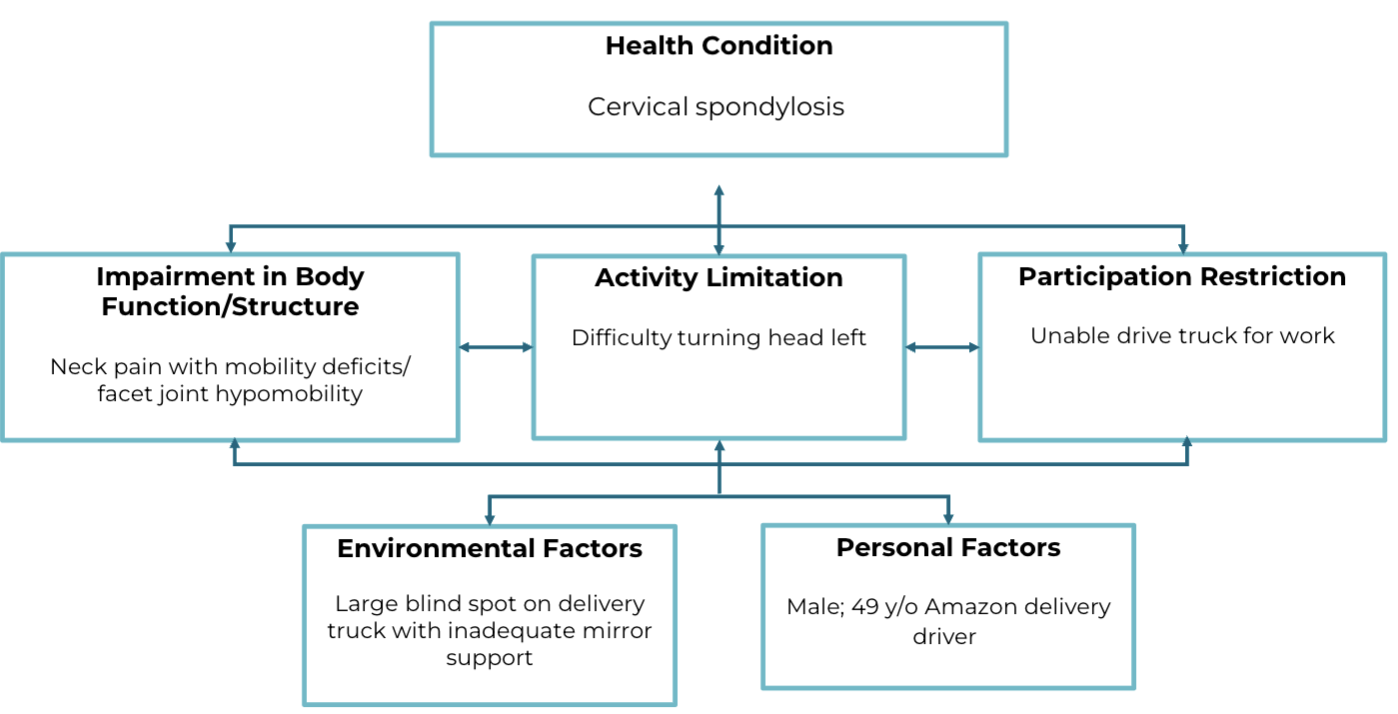
ICF example: Neck Pain with Mobility Deficits
Pathoanatomy: Neck Pain with Radiating Pain
What is the proposed underlying cause of the condition?
Lateral foraminal stenosis (70-75%)
Herniated nucleus pulposus (25%)
Pathoanatomy: Neck Pain with Radiating Pain
What is the proposed underlying cause of the condition?
Lateral foraminal stenosis (70-75%)
Space-occupying lesion of the intervertebral foramen
Combination of factors including
Decreased disk height
Degenerative changes (spondylosis)
Uncovertebral joints anteriorly
Zygapophysial joints posteriorly
Pathoanatomy: Neck Pain with Radiating Pain
What is the proposed underlying cause of the condition?
Herniated nucleus pulposus (25%)
Less prevalent
Structural differences in the cervical disk
Vertically oriented posterior annular fibers
Posterior annulus reinforcement
Posterior longitudinal ligament
Uncovertebral joints
Medical Screening: Neck Pain with Radiating Pain
What other conditions should be considered with this patient presentation?
Viscerogenic
Neoplastic conditions
Inflammatory or systemic disease
Cardiopulmonary conditions
Cervical vascular pathology
Medical Screening: Neck Pain with Radiating Pain
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Spinal fracture
Cervical myelopathy
Upper cervical ligamentous instability
Differential Diagnosis: Neck Pain with Radiating Pain
What other conditions should be considered with this patient presentation?
Neuromusculoskeletal
Mobility deficits or movement coordination impairments
Somatic referred pain (disc, ligaments, facets, muscles)
Thoracic outlet syndrome
Rotator cuff related shoulder pain
Lateral epicondylalgia
Radial nerve entrapment
Carpal tunnel syndrome
Subjective Examination: Neck Pain with Radiating Pain
What system, structure, pain mechanism, and phases of healing are unique to this patient presentation?
System
Neuromusculoskeletal
Structure
Nerve root and disk (if HNP)
Pain mechanism
Neuropathic5 (nerve root), nociceptive4 (disk)
Phase of healing
Disk/annulus tear 10-12 weeks
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Neuropathic pain
May be described as burning, shooting, sharp, aching or electric-shock-like
May have other neurological symptoms e.g., pins and needles, numbness, weakness
Can refer in a dermatomal pattern
Not as responsive to NSAIDs, more responsive to anti-epileptics/anti-depressants
Often presents with pain that is of high severity/irritability
May spontaneous and/or sudden intensification of pain
Can have latent pain response to movement/mechanical stress
Often worse at night with sleep disturbances
Often associated with psychological affect
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Lateral foraminal stenosis
Gradual onset of worsening lancinating arm pain
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Herniated nucleus pulposus
May be gradual or immediate onset of local and/or somatic referred neck pain and lancinating arm pain
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Lateral foraminal stenosis: Aggravating factors
Intensification and/or peripheralization of radicular symptoms into the upper extremity with activities and movements that place a mechanical load on the neural structure
Cervical extension, ipsilateral rotation and lateral flexion, axial compression
Looking up or over the ipsilateral shoulder
Positions of the upper quarter that tension the nerve root
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Lateral foraminal stenosis: Easing factors
Reduction and/or centralization of radicular symptoms into the upper extremity with activates and movements that reduce the mechanical load on the neural structure
Cervical flexion, contralateral rotation and lateral flexion, axial distraction
Looking down or over the contralateral shoulder
Positions of the upper quarter that reduce tension to the nerve root
Shoulder abduction sign/Bakody’s sign
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Lateral foraminal stenosis: 24-hour pain behavior
Morning
Sleeping in cervical extension, ipsilateral rotation or lateral flexion, or in an upper extremity position that tensions the nerve root, they may wake up with arm pain
Noon to evening
Symptoms will vary through the day depending on the patient's activities
Night
Sleeping in cervical extension, ipsilateral rotation or lateral flexion, or in an upper extremity position that tensions the nerve root, they may wake up with arm pain
Neuropathic pain is often worse at night
May have disrupted sleep
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Herniated nucleus pulposus: Aggravating factors
Intensification and/or peripheralization of radicular symptoms into the upper extremity with activities and movements that place mechanical load on the disk and nerve root
Cervical protraction and flexion
Forward head position (often in sitting) or looking down to read
Positions of the upper quarter that tension the nerve root
Median nerve upper limb tissue tension position of the upper extremity
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Herniated nucleus pulposus: Easing factors
Reduction and/or centralization of radicular symptoms into the upper extremity with activates and movements that reduce mechanical load on the disk and nerve root
Cervical retraction and extension
Neutral to extended head position (often during standing/walking) or looking up
Positions of the upper quarter that reduce tension to the nerve root
Shoulder abduction sign/Bakody’s sign
Subjective Examination: Neck Pain with Radiating Pain
What are common subjective reports for patients with radiating pain?
Herniated nucleus pulposus: 24-hour pain behavior
Morning
Sleeping in cervical flexion or in an upper extremity position that tensions the nerve root, they may wake up with arm pain
Noon to evening
Symptoms may vary throughout the day depending on the patient's activities
Night
Sleeping in cervical flexion or in an upper extremity position that tensions the nerve root, they may wake up with arm pain
Neuropathic pain is often worse at night
May have disrupted sleep
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Systems review (as indicated from the subjective exam): Cardiopulmonary
Vitals
BP, HR, auscultate
Assess for mechanical reproduction of symptoms and/or adverse response to movement
AROM, PIVM, compression/distraction, neurodynamic tests
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Systems review (as indicated from the subjective exam): Neuromusculoskeletal
Cranial nerves
Reflexes/pathological reflexes
Dermatomes/myotomes
Upper cervical ligamentous testing
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Specific Tests and Measures
Neurological examination
Movement and provocation examination
Neurodynamic testing
Shoulder abduction test (+LR 2.1. –LR 0.91)
Diagnostic test-item cluster
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Neurological examination
Deep tendon reflexes
Bicep (+LR 4.8, -LR 0.8), tricep (+LR 0.42, -LR 1.04), brachioradialis (+LR 1.2, -LR 0.98)
Dermatomes (light touch and/or sharp/dull)
C4-T1
Sharp/dull (+LR 0.7 to 2.07, -LR 0.82 to 1.15)
Myotomes
C4-T1
(+LR 0.37 to 17.5, -LR 0.66 to 1.12)
Cluster of dermatomes, myotomes, and reflexes
(+LR 9.0, -LR 0.83)
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Movement and provocation examination: AROM
Range of motion limitations and symptom provocation will depend on individual patient presentation
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Movement and provocation examination: Passive intervertebral motion
Hypomobility and symptom reproduction at the involved segment(s)
Possible hyper- or hypomobility at adjacent segments
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Movement and provocation examination: Orthopaedic examination tests
Spurling A (+LR 3.5, -LR 0.58)
Distraction test (+LR 4.4, -LR 0.62)
Arm squeeze test (+LR 10.6 to 48.0, -LR 0.04 to 0.44)
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Neurodynamic testing
ULTTA/ULND1 (median) (+LR 1.3, -LR 0.12)
ULTTB/ULND2b (radial) (+LR 1.1, -LR 0.85)
ULND 3 (ulnar)
ULND 1-3 cluster
1/3 (Sp 0.69)
0/3 (Sn 0.97)
Physical Examination: Neck Pain with Radiating Pain
What are the key examination procedures for patients with radiating pain?
Diagnostic test-item cluster
Wainner Cluster
3/4 (LR+ 6.1; 65% probability), 4/4 (+LR 30.3; 90% probability)
+ ULTTA
Reproduction of symptoms or sensitized with a distal maneuver or side to side difference of 10deg elbow extension
Ipsilateral rotation less than 60deg
+ Distraction test
Alleviation of distal symptoms
+ Spurling A
Reproduction of distal symptoms
Prognosis: Neck Pain with Radiating Pain
What is the prognosis of the condition?
Clinical course and prognosis
The condition is self-limiting with a favorable prognosis with resolution of symptoms occurring weeks to months
70-90% of patients experience improvement without surgery
Most patients will see symptom improvement over time in both lateral foraminal stenosis and herniated nucleus pulposus
Spontaneous resolution of disk herniations are common
Patients should be monitored for progressive neurological dysfunction
Prognosis: Neck Pain with Radiating Pain
What is the prognosis of the condition?
Factors that may impact prognosis
High pain intensity (NPRS >/= 6/10)
High self-reported disability (NDI >/= 30%)
High pain catastrophizing (PCS >/= 20)
Older age
Prior health
Previous exercise
History of previous neck pain
History of other musculoskeletal disorders
Stage of Condition: Neck Pain with Radiating Pain
How does this present differently based on stage of condition?
Acute
Severity and irritability are often high
Pain at rest or with initial to mid-range spinal movements: before tissue resistance
Pain control is often the intervention goal at this stage
Stage of Condition: Neck Pain with Radiating Pain
How does this present differently based on stage of condition?
Subacute
Severity and irritability are often moderate
Pain experienced with mid-range motions that worsen with end-range spinal movements: at tissue resistance
Movement control is often the intervention goal at this stage
Stage of Condition: Neck Pain with Radiating Pain
How does this present differently based on stage of condition?
Chronic
Severity and irritability are often low
Pain that worsens with sustained end-range spinal movements or positions: overpressure into tissue resistance
Functional optimization is often the intervention goal at this stage
Interventions: Neck Pain with Radiating Pain
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Acute
Education
Possible short-term semi-rigid collar use
Exercise
Exercise with mobilizing and stabilizing elements
Biophysical agents
Low-level laser
Interventions: Neck Pain with Radiating Pain
What are interventions recommended by the clinical practice guidelines based on stage of condition?
Chronic
Education
Education counseling to encourage participation in occupational and exercise activity
Exercise
Combined exercise: stretching and strengthening elements
Manual therapy
Mobilization or manipulation to cervical and thoracic region
Biophysical agents
Intermittent traction
Interventions: Neck Pain with Radiating Pain
What additional interventions are recommended for this condition?
Exercise
Craniocervical flexion exercises
Exercises that promote the accessibility of an upright posture
Repeated or sustained motions in the direction of symptoms centralization
Manual therapy
Upper quarter nerve mobilization procedures
Manual traction
Cervicothoracic manipulation
Biophysical agents
Mechanical traction
Interventions: Neck Pain with Radiating Pain
What additional interventions are recommended for this condition?
Clinical Prediction Rule (cervical traction)
Raney CPR
3/5 (+LR 4.81; 79.2% probability), 4/5 (+LR 23.1; 94.8% probability)
Peripheralization of symptoms with a PA at C4-C7
Positive shoulder abduction test
Age >55 years
+ ULTTA/ULND 1
+ Neck distraction test
Interventions: Neck Pain with Radiating Pain
When should we consider interprofessional referral and what are other treatment options?
MRI
Patients with progressive neurological deficits or those without improvement over 4-6 weeks should be referred for imaging
Preferred modality for patient who do not respond to conservative care
Medical Intervention
Medications/injections
SSRIs/SNRIs, antiepileptics5
Spinal injections
Surgical
Laminectomy/discectomy with cervical fusion