SOAP notes
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
Subjective
S, what the patient tells you
Objective
O, What you see/measure
Assessment
A, what you conclude
Plan or procedure
P, what will you do
Subjective
WHAT PATIENT TELLS YOU
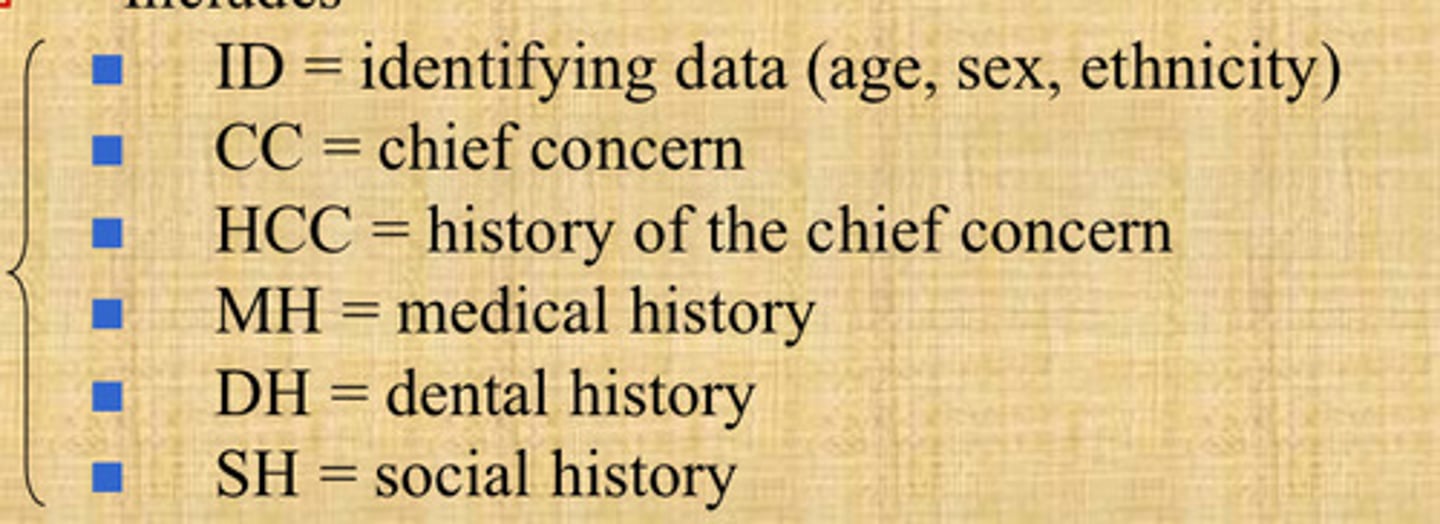
Includes chief concern, history of chief concern (CC), medical history (MH), dental history (DH), social history (SH)
Symptoms:
- pain, where, when, relievers
Esthetic concerns
Fears and feelings about treatment
Objective
WHAT ARE YOUR OBSERVATIONS/MEASUREMENTS
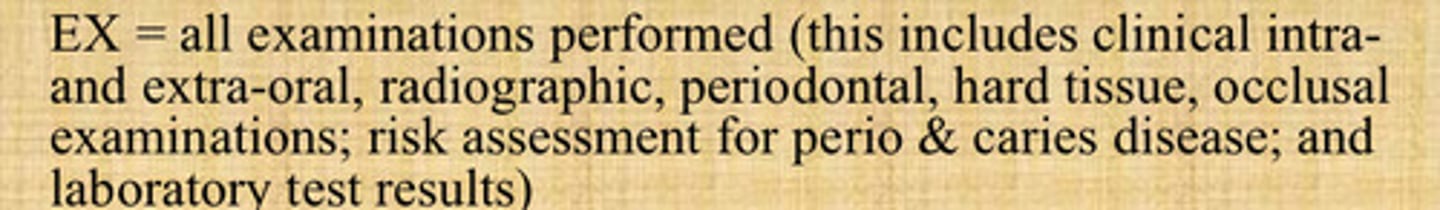
Includes Physical exam (PE)/Vital Signs (VS), Extraoral exam (EOE), Intraoral exam (IOE), summary of appearance of both soft (perio) and hard tissue exams (HTE), and radiographic exam (RE)
Signs (as opposed to symptoms)
- swelling, fractured cusp/exposed dentin, carious legion, peri-apical radiolucency in radiography
Assessment
WHAT IS YOUR DIAGNOSIS/CONCLUSION?
Based on S and O what to include?
- Perio DX: periodontal diagnosis and risk assessment
- CRA: caries diasease diagnosis and risk assessment
- Occlusion/TMJ assessment
- Restor Dx: restorative needs, surgical and non surgical
Know etiology (cause of all above) and come up with prognosis (ideal outcome of treatment)
Perio Dx
Periodontal diagnosis and risk assessment
CRA
Caries disease diagnosis and risk assessment
Restor Dx
Restorative needs, surgical and non-surgical
Etiology
cause of disease
Prognosis
Ideal outcome of treatment
Plan
WHAT TREATMENT WILL YOU PROVIDE?
Includes notes on:
- treatment plan discussion (be detailed)
= procedures
- instructions, recommendations, referrals
- Perscriptions (DWP, RBA, ABC)
DWP
discussed with patient
RBA
Risk and benefits of alternatives
ABC
Alternatives with benefits and complications
If treatment was not performed
details of discussion (DWP) proposed treatment with options and referrals
If treatment was performed
Step by step details of clinical procedure, what where how much anesthetic, type and quality of materials used, details of perspectives (drugs, mg, tabs, DWP)
Subjective
Objective
Assessment
DX: diagnoses of treatment conditions
Plan/procedure
Date, procedure code, who made entry
Each SOAP note must contain
Don't
Do/Dont: alter or destroy information or "cover up"
diagnostic or treatment errors
Do
Do/Dont: correct documentation errors in a written record
by putting a single line through the error and make
correction above with the date and your initials
Do
Do/Dont: correct such errors in our electronic record by a
new entry which records the student provider and
attending faculty with the date when error corrected