Overview of Cardiac Physiology and Arrhythmias
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
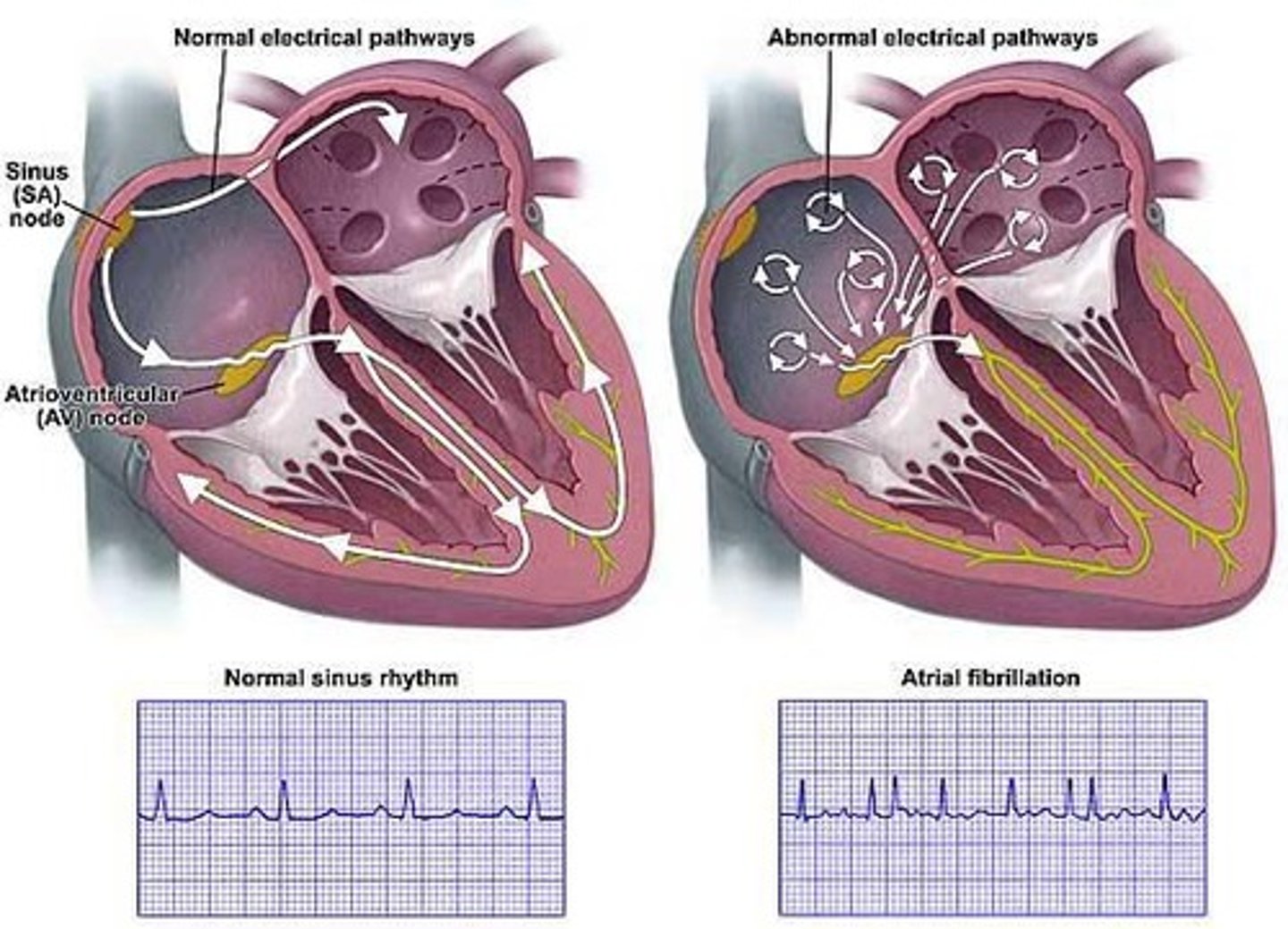
Cardiac arrhythmia
Refers to abnormal rhythm due to defects in the heart's conduction system.
Heart sounds
Sounds produced by the heart during the cardiac cycle, often assessed during a physical examination.
Cardiac output
Volume of blood ejected from left (or right) ventricle into aorta (or pulmonary trunk) each minute.
Stroke volume
The amount of blood ejected per beat from each ventricle.
Regulation of heart rate
The mechanisms that control the speed of the heartbeat.
Premature beats
Most common arrhythmia, usually harmless, often caused by exercise, stress, caffeine, nicotine, alcohol or other drugs.
Atrial fibrillation (AF or A fib)
Most common problematic arrhythmia affecting about 1% of Americans, characterized by misfiring of the SA node.
Bradycardia
A slowed heartbeat defined as under 60 bpm, considered normal unless accompanied by fatigue, dizziness, lightheadedness or fainting.
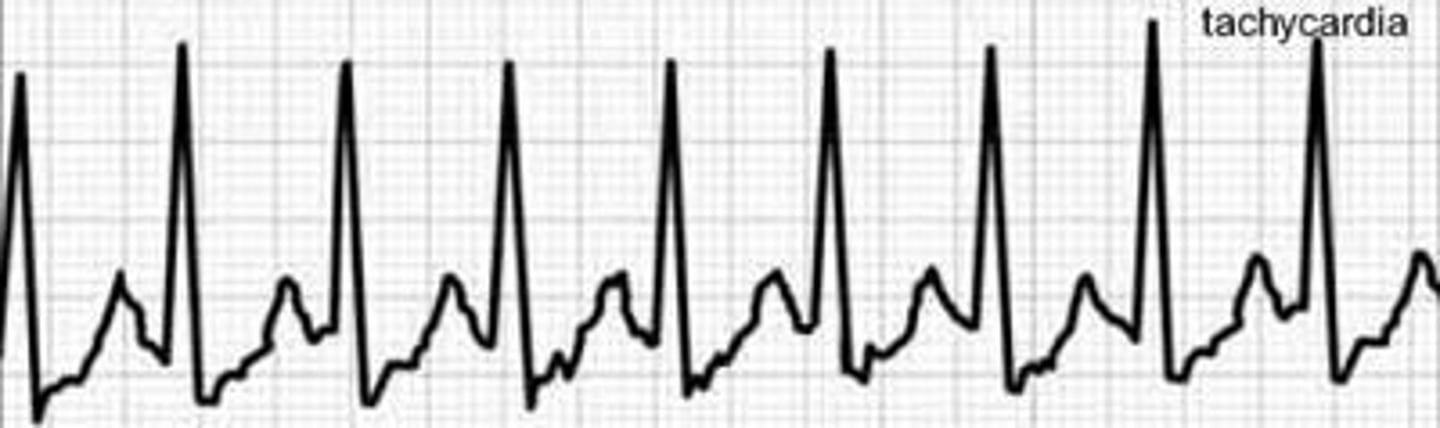
Tachycardia
A rapid heartbeat defined as more than 100 bpm in adults, felt as palpitations or noticeable rapid heart action.
Ventricular arrhythmias
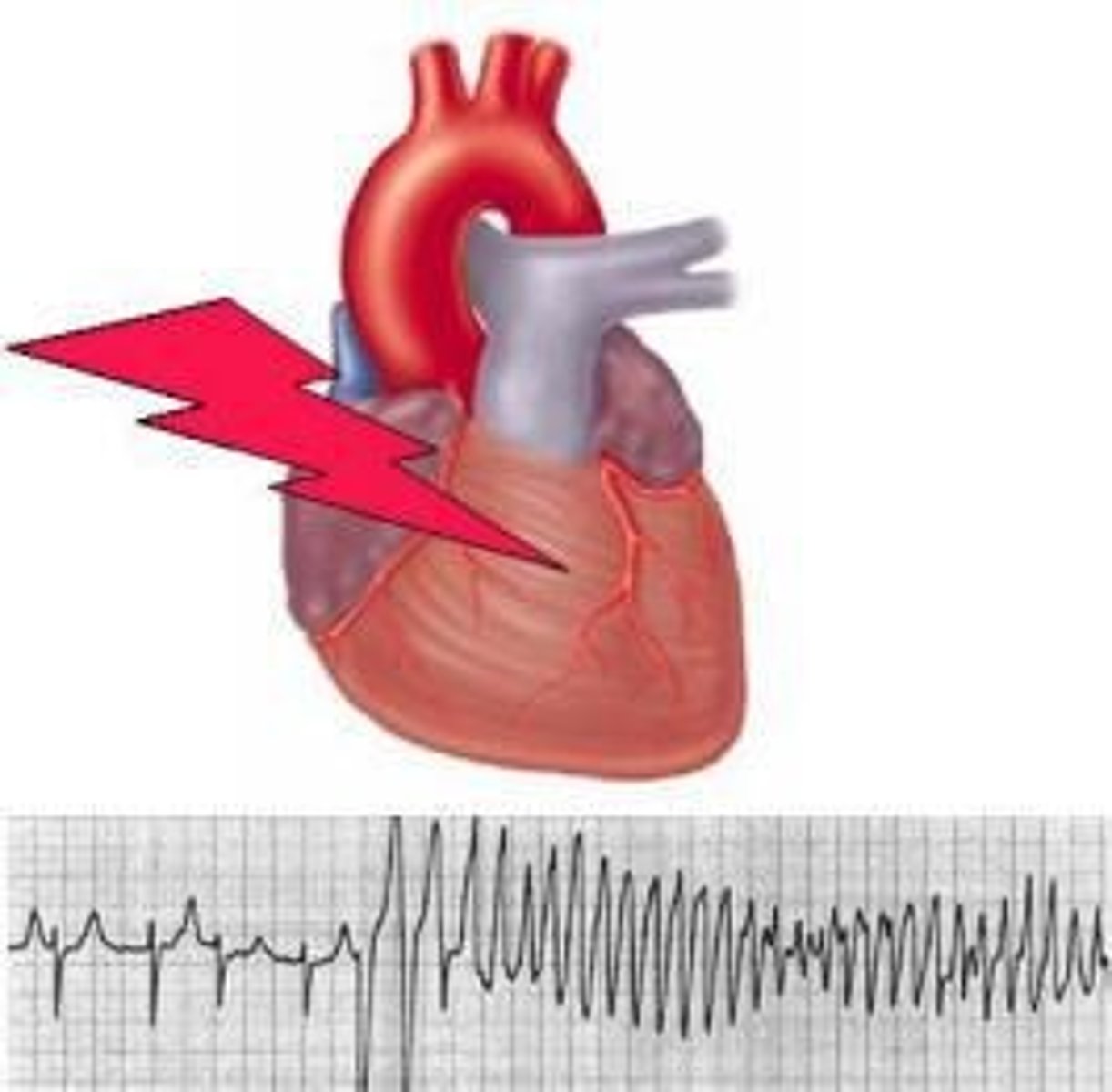
The most severe and life-threatening arrhythmias, including ventricular tachycardia and ventricular fibrillation.
Ventricular tachycardia (V tach)
A rapid heartbeat arising in the ventricles that can lead to ventricular fibrillation.
Ventricular fibrillation
Occurs when the ventricles go out of control, quivering and beating ineffectively, stopping the pumping action.
Defibrillation
The process of delivering an electric shock to restore a normal heart rhythm.
Cardiac output formula
CO = stroke volume (SV) x heart rate (HR).
Resting cardiac output range
Between 4.8 and 6.4 L per min.
Stroke volume formula
Stroke volume = EDV - ESV.
End-diastolic volume (EDV)
The maximal amount of blood that the ventricle can hold just prior to ventricular contraction.
End stroke volume (ESV)
The amount of blood remaining in the ventricle after contraction (systole).
Example of stroke volume calculation
For a 70 kg male: EDV about 120 ml, ESV about 50 ml, Stroke volume = 120 ml - 50 ml = 70 ml.
Heart palpitations
The sensation of feeling the heart skip a beat, have a double beat, or an especially strong beat.
Standard estimate
1 ml/1kg body weight
Average resting HR
About 75 beats per min
Cardiac Output (CO)
CO = 70 ml x 75 bpm = 5250 ml/min or 5.25 L/min
Total blood volume of a 70 kg male
~ 5 L
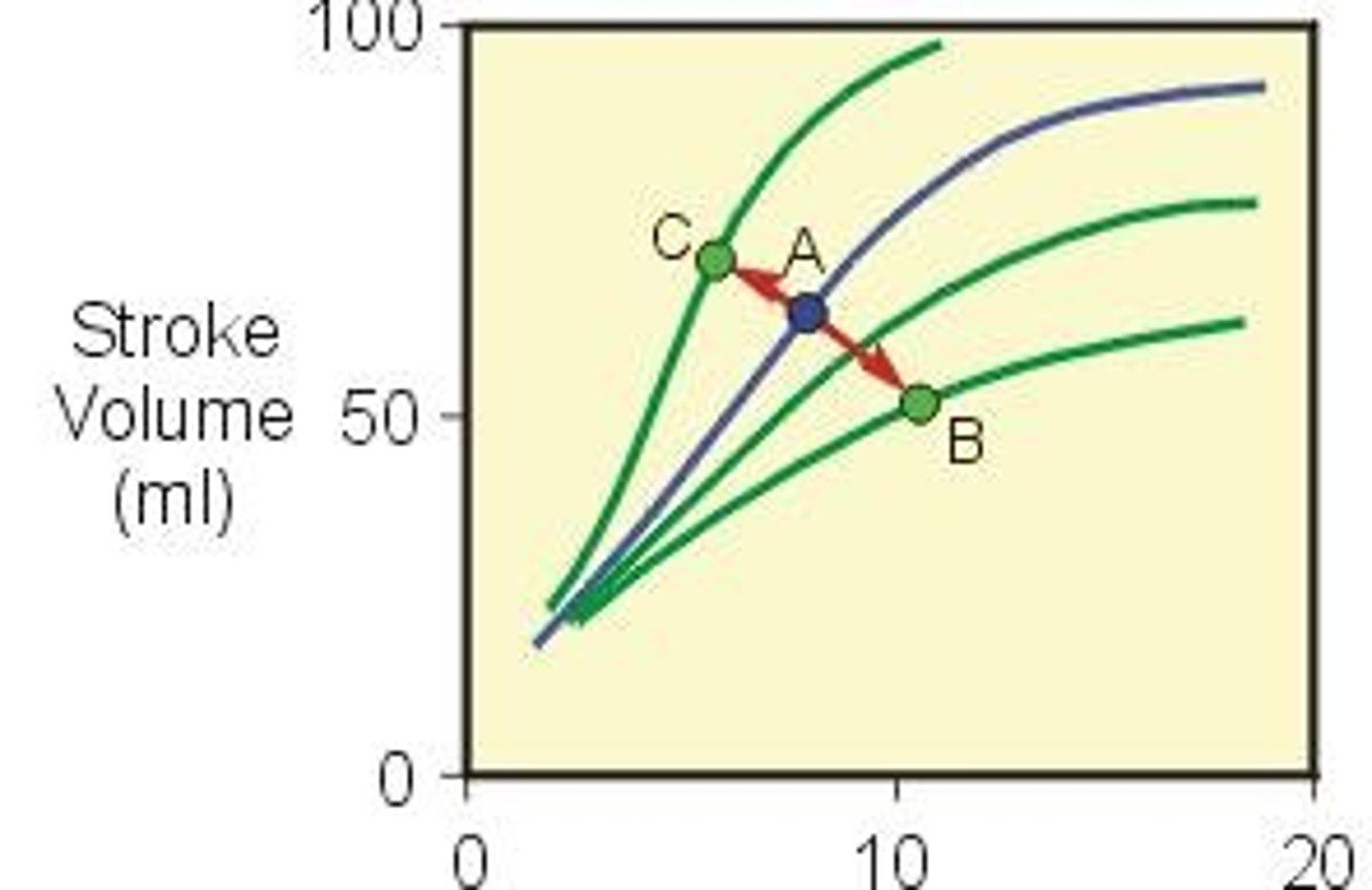
Regulation of stroke volume
Three factors regulate stroke volume and ensure left and right ventricles pump equal volumes of blood
Factors that alter stroke volume (SV)
1. Preload 2. Contractility 3. Afterload
Preload
Degree of stretch on the heart before it contracts
Frank-Starling law
The more the heart fills with blood during diastole, the greater the force of contraction during systole
End Diastolic Volume (EDV)
Determined by 1. Duration of ventricular diastole 2. Venous return - volume of blood returning to right ventricle
Contractility
Strength of contraction
Positive inotropic agents
Increase contractility, often promote Ca2+ inflow during cardiac action potential
Negative inotropic agents
Decrease contractility, examples include very low blood oxygen levels, high or low pH, some anesthetics, beta blockers
Afterload
Pressure that must be overcome before a semilunar valve can open
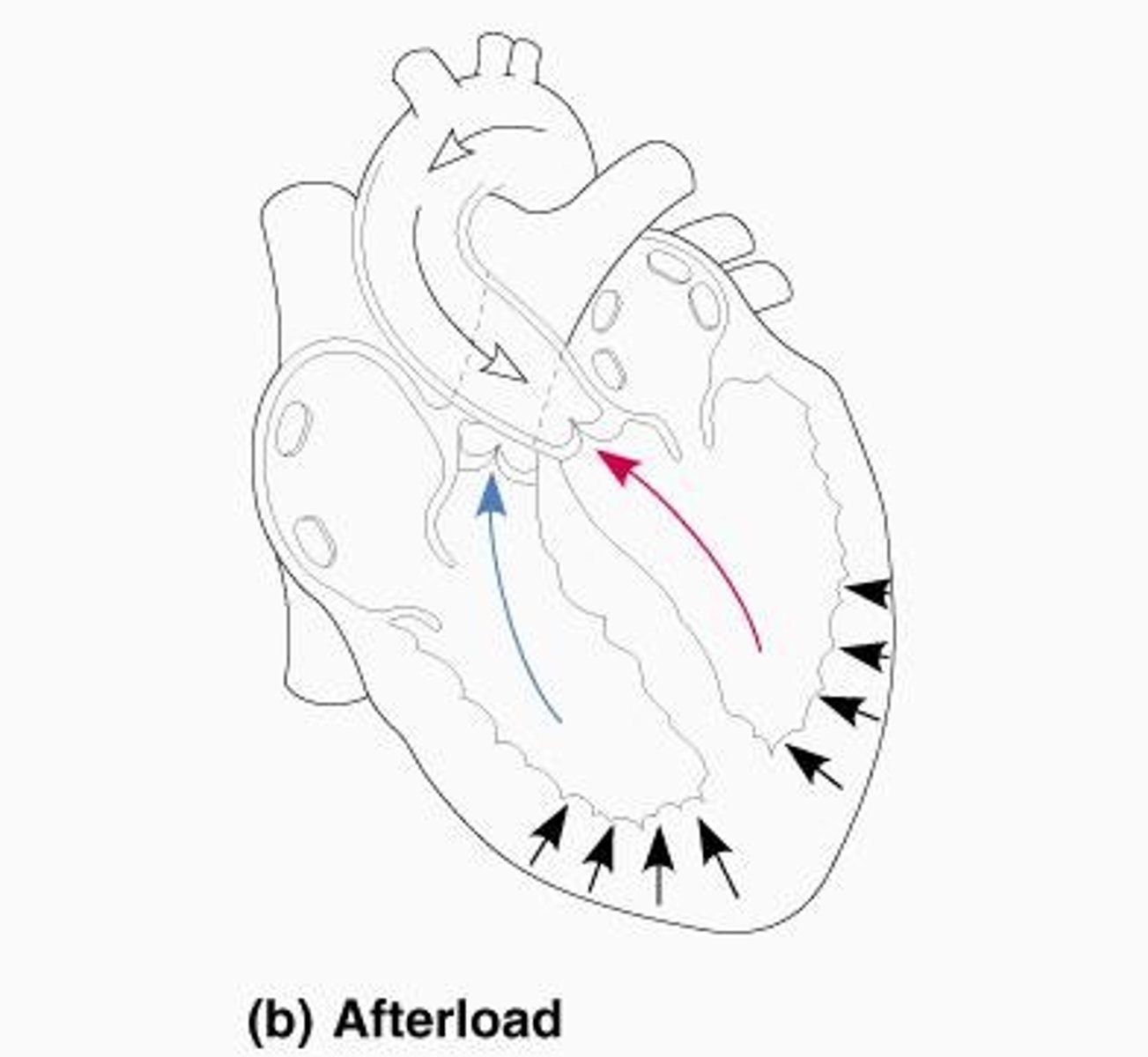
Effect of increased afterload
Causes stroke volume to decrease; blood remains in ventricle at the end of systole
Factors increasing afterload
Hypertension, atherosclerosis, aortic narrowing, or physical pressure on the aorta
Regulation of Heart Rate
Cardiac output depends on heart rate and stroke volume
Heart rate adjustments
Largely controlled by direct innervation of the autonomic nervous system (ANS), hormones (especially epinephrine and norepinephrine), and cations
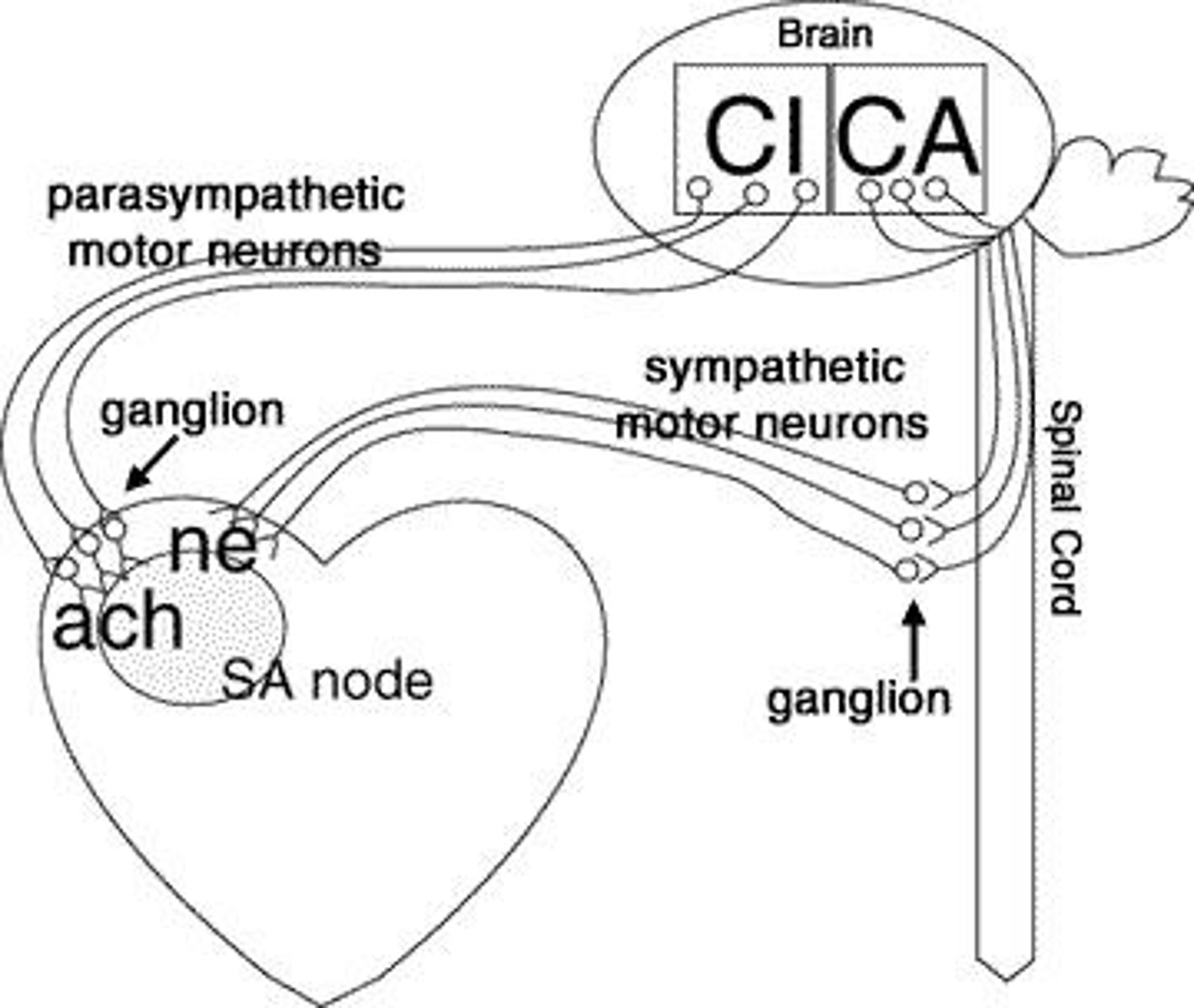
Influence of ANS
The sympathetic and parasympathetic divisions of the ANS can modify timing and/or strength of each heartbeat
Autonomic HR regulation
Originates in cardiovascular center of medulla, receives input from a variety of sensory receptors
Types of receptors influencing HR
Proprioceptors, Baroreceptors, Chemoreceptors
Sympathetic HR regulation
Sympathetic neurons called cardiac accelerator nerves extend to heart, triggering release of norepinephrine (NE)
Effects of norepinephrine (NE)
1. In autorhythmic fibers speeds rate of spontaneous depolarization 2. In contractile fibers enhances Ca2+ entry increasing contractility
Parasympathetic HR regulation
Parasympathetic impulses reach heart via the vagus nerve, triggering release of acetylcholine (ACh)
Effect of acetylcholine (ACh)
Decreases heart rate by slowing rate of spontaneous depolarization
Checkpoint Questions
1. Which type of heart arrhythmia is most life-threatening? 2. Which heart arrhythmia is best treated with an artificial pacemaker? 3. What does it mean if a physician states that a patient is 'tachy'? 4. What is the formula to calculate stroke volume (SV)? 5. What is the relationship between cardiac output (CO) and SV? 6. Given an EDV of 130ml, an ESV of 75ml, and a HR of 72bpm, calculate CO. Is the CO in the average range? 7. Consider preload, contractility, and afterload. An increase in which parameter decreases CO? 8. In general, would you expect the sympathetic division of the ANS to increase or decrease HR?