Physiology- Immune System
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
68 Terms
what is the immune system?
network of biological systems that protect an organism from disease, infection, and injury/harmful cellular changes
what are the functions of the immune system?
defend against invading pathogens
respond to cellular injury and innate repair (“healing”- can be with or without infection)
monitor and remove malignant or problematic cells (immune surveillance)
example of “not self”
pathogens (bacteria, virus, fungi)
malignant cells
damaged or “old/worn out” cells
type of cell ALL leukocytes are derived from
hematopoietic progenitor cell
two major types of leukocytes
myelocytes
lymphocytes

what type of leukocytes are involved in the INNATE immune system?
myelocytes
what type of leukocytes are involved in the ADAPTIVE immune system?
lymphocytes
two "arms” of the immune system
innate
adaptive
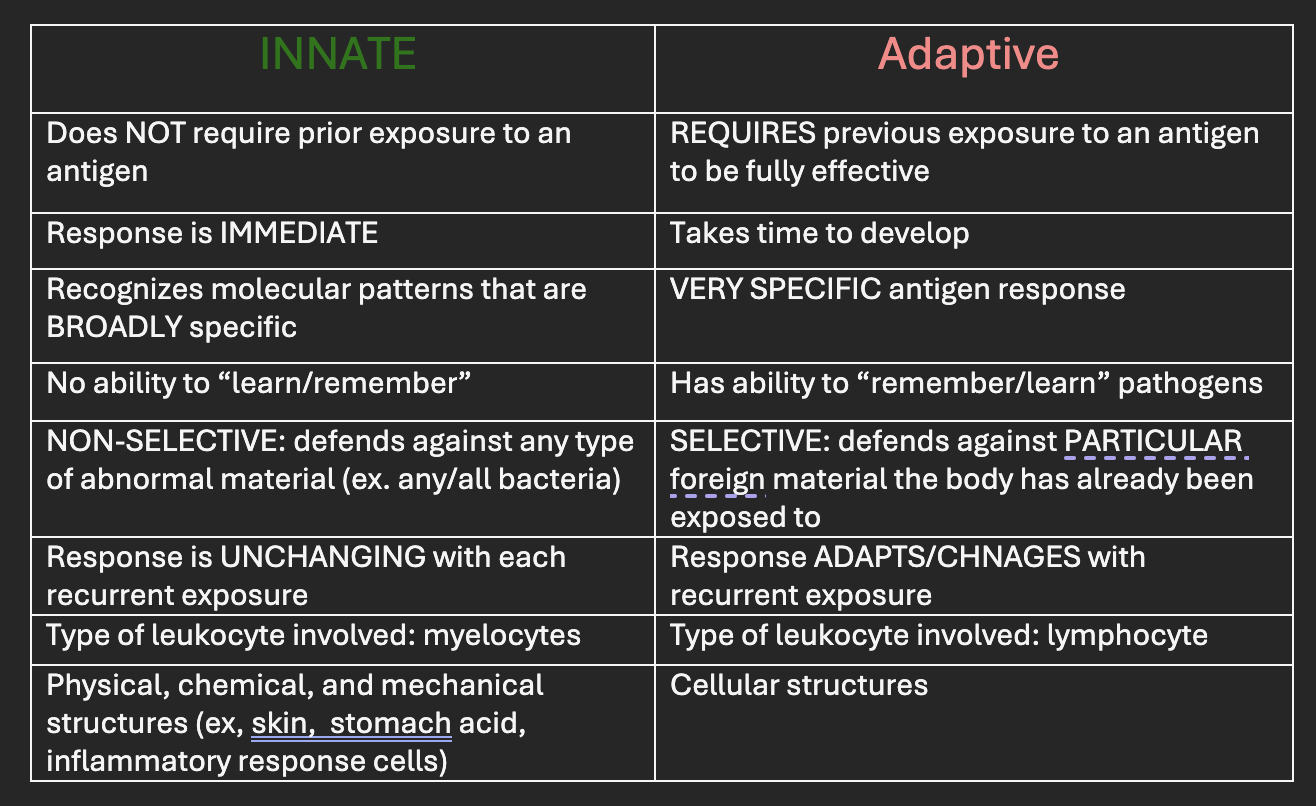
compare and contrast innate vs adaptive immune system
what is the first line of defense?
barrier defenses
mechanical
biochemical
mechanical barriers
epithelial cells (skin and mucosa)
tight junctions to prevent furthering of infection btwn cells
high turnover
regular “washing” (cough, sneeze, urinaiotn, vomitting)
biochemical barriers
secretions
mucus
sweat/tears
stomach acid
microbiome
compete with pathogens for nutrients
block attachment to epithelium
produce toxins to inhibit pathogen growth
what is the second line of defense
inflammation (non specific response)—recruit oxygen, nutrients, proteins, and immune cells to sites of tissue damage or injury (infectious OR non-infectious)
goals of inflammation
destroy pathogens
trigger the ADAPTiVE immune system
initiate healing
true or false: inflammation is a non-specific response to a pathogen or injury
true; there is a similar (rapid) response no matter what the triggering event was
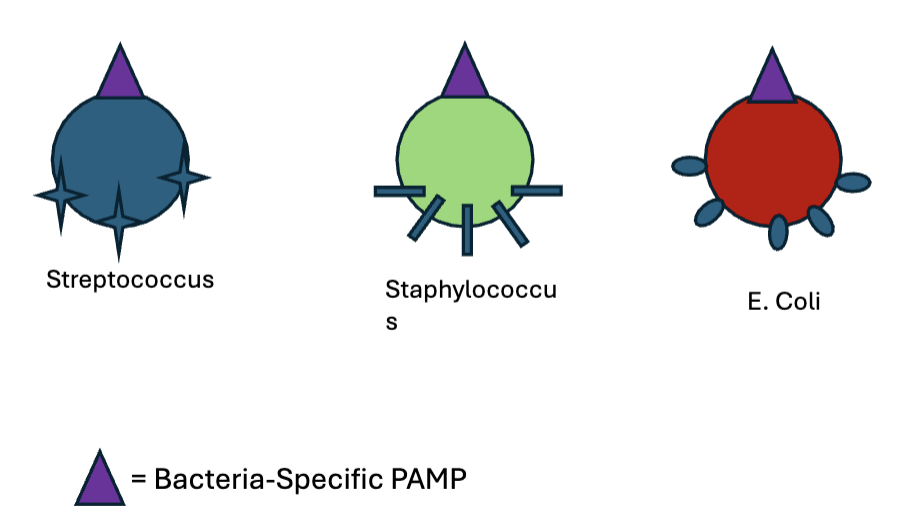
P.A.M.Ps
pathogen associated molecular patterns
broad specificity
similar carb/protein presented on different cells, therefore can be recognized by TOLL LIKE RECEPTORS on macrophage
phagocytosis
cellular process of ingesting and eliminating particles including mircroorgisnism, foreign substances, and damages/dying cells
what are phagocytes and what are the types of phagocytes?
phagocytes are calls that perform phagocytosis
neutrophils: mobile; specialized cells in bacterial response (ex. puss)
monocytes and macrophages: tissue bound
Inflammation STEP 1- tissue injury introduces foreign material (ex. bacteria)
macrophages are activated by presence of foreign material—> phagocytosing the infected or damaged cells—> release of cytokines to amplify response
what are cytokines?
small proteins that act as a chemical messenger between cells
involved in mediating inflammation
ex. HISTAMINE
Inflammation STEP 2-3
cytokines attract neutrophils and monocytes to the injury site—> MORE cytokines are released that exert various immune responses
when phagocytes destory pathogens and release more cytokines…
recruit more immune cells
stimulate hypothalamus to produce FEVER (fever increase, bacteria decrease)
stimulate liver to produce ACUTE PHASE REACTANTS (CRP)
stimulate blood marrow to produce more white blood cells (LEUKOCYTOSIS)
when/ for what conditions is CRP test ordered for most
autoimmune and inflammatory diseases
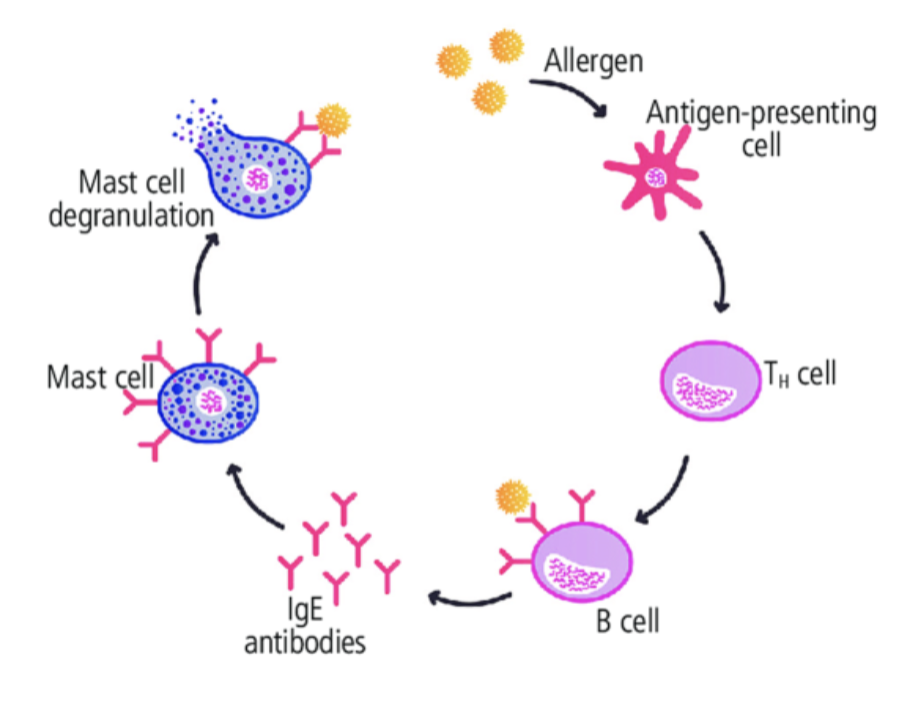
what type of cytokine does a mast cell release?
histamine
Inflammation STEP 4-5
mast cells are activated by presence of foreign pathogen
degranulate and release histamine
Inflammation STEP 6
histamine dilates local blood vessels and widens capillary pores—> increase blood flow to the sight of injury—> increase cells, oxygen, etc
clinical manifestations of inflammation/increased blood flow to tissue
SUBJECTIVE
heat
redness
swelling
pain
loss of function
OBJECTIVE
fever
leukocytosis
elevated CRP
Inflammation STEP 6/7
increased blood flow also causes INCREASED leaking of plasma proteins to the wound site
exposure to factors involved in injury will active fibrinogen to FORM FIBRIN CLOTS to wall off the injury site
people more prone to fibrin clots = inflammatory disease, cancer, etc
what must occur after the inflammatory response has mounted a RAPID and NONSPECIFIC response?
the ADAPTIVE immune system must be triggered to provide a tailored response to SPECIFIC threat
inflammation: activiating the adaptive immune system
phagocytes can play a role in recruiting adaptive immunity by functioning as APCs
APCs
antigen presenting cells
macrophages and dendritic cells that engulf pathogens, digest the material, then present it on the cell surface to be “recognized/read” by adaptive immune cells
what is the third line of defense
adaptive immune system
what makes up the adaptive immune system?
lymphocytes
T cells
B cells
antibodies
characteristics of the adaptive immune system
SPECIFIC response to SPECIFIC antigen
PRIMARY response to fight infection with initial exposure—> increased response with increased exposure
has ability to “remember” and provide LONG-TERM protection (secondary response)
primary lymphoid organs
where lymphocytes are produces and mature
B lymphocytes are produced and matures in BONE marrow
T lymphocytes are produced in bone marrow, but mature in the THYMUS
secondary lymphoid organs
where lymphocytes reside
T and B cells migrate to spleen, lymph nodes, and made available to interact with APCs and other immune cells
cells of the adaptive immune system
T-helper cells (CD4)
T-cytotoxic cells (CD8)
plasma cells
Memory B cells
Memory T cells
what is the type of cell(s) of the adaptive immune system recognize and regulate?
T-helper cells (CD4)
who is more susceptible to infection due to CD4 deficiency?
those with HIV/AIDS
what is the type of cell(s) int he adaptive immune system that kill and destroy?
T-cytotoxic cells (CD8)
Plasma cells
interaction of T-cytotoxic cells (CD8) with pathogen
act DIRECTLY with pathogen through cytotoxic chemicals
interaction of plasma cells with pathogen
act INDIRECTLY through antibodies
what type of cell(s) in the adaptive immune system remember?
memory B cells
memory T cells
next time the body is re-exposed, can release quick and greater response
what are the two “arms” of the adaptive immune system?
humoral and cellular
components of the humoral arm of the adaptive immune system
B cells
memory B cells create lasting immunity
plasma B cells produce antibodies to defense against EXTRACELLULAR pathogens (ex. bacteria, fungi, parasites)
afect pathogens from “AFAR” through antibodies
components of the cellular arm of the adaptive immune system
T cells
T-helper cells regulate B and T cells
t-cytotoxic cells (CD8) defend against INTRACELLULAR pathogens (own infected cells, VIRAL) or cancer cells
must be “CLOSE” to be effective
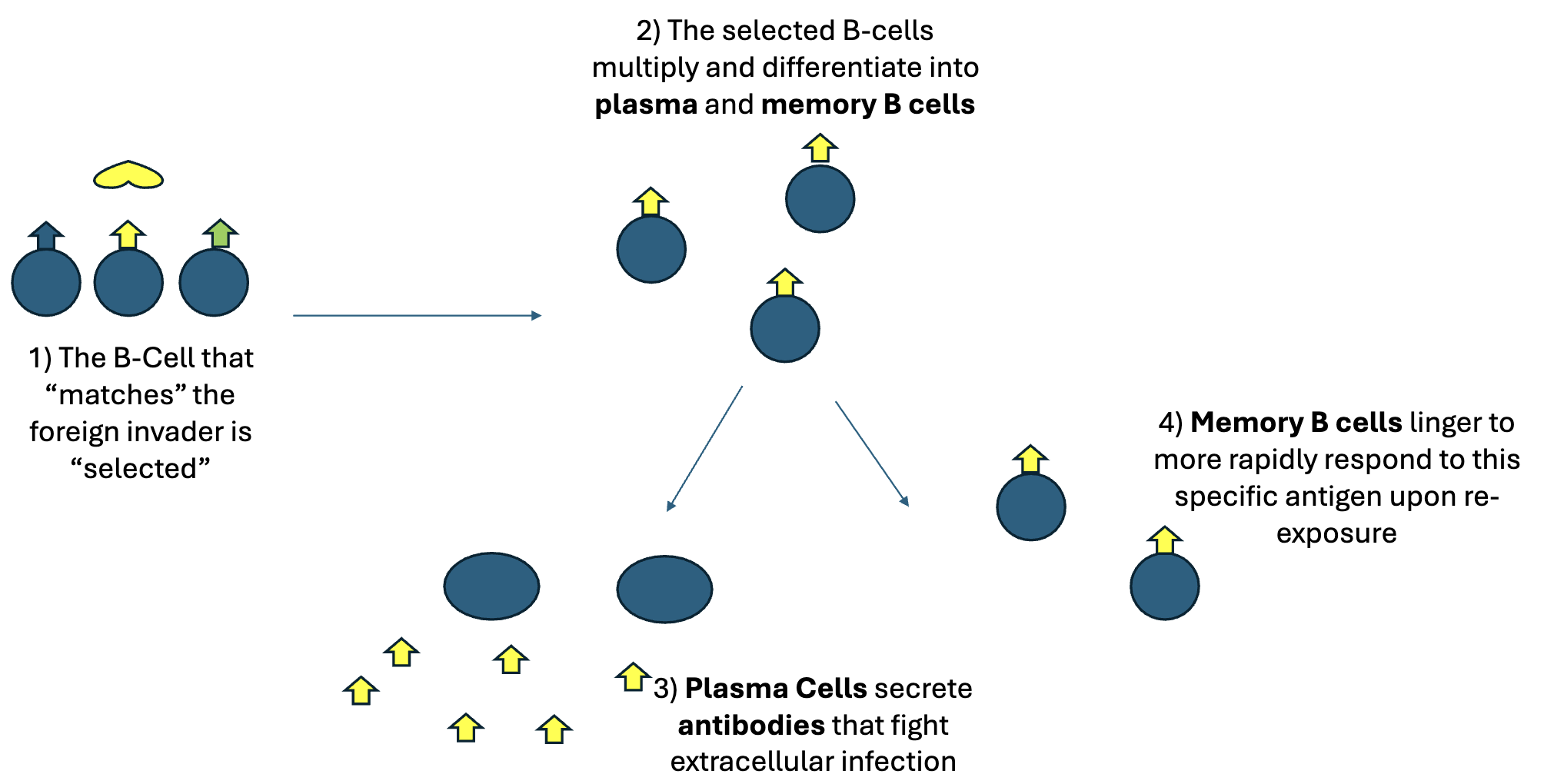
anti bodies and memory
the B cell that “matches” the foreign pathogen is “selected”
the selected B cells multiply and differentiate into PLAMA or MEMORY B cells
3a.PLASMA cells secrete antibodies ot fight EXTRACELLULAR infection
3b.MEMORY B cells linger to more rapidly respond to this SPECIFIC antigen upon re-exposure
what are antibodies/immunoglobulins
proteins secreted by B cells that have SPECIFIC action against SPECIFIC extracellular antigens
classes of antobodies/immunoglobulins
IgM
IgG
IgE
what are the main ways antibodies destroy pathogens?
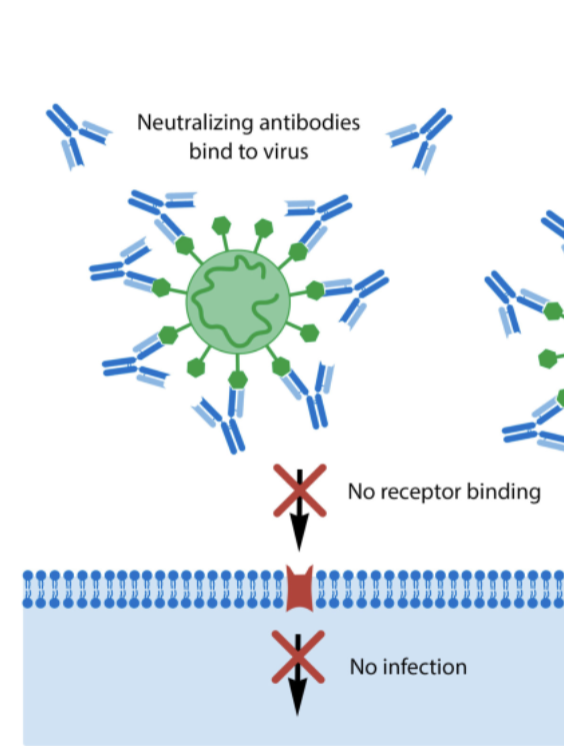
neutralization
opsonization
trigger inflammatory response (activate innate immunity)
neutralization
antibodies surround the virus and block ability to bind to host cell
opsonization
antibodies bind to the pathogen and make more “palatable” to phagocytes
trigger inflammatory response
antibodies activate innate immunity/inflammatory response in order to recruit phagocytes to the area with pathogen
IgM
Mighty fast
FIRST antibody released during FIRST EXPOSURE to antigen (primary immune response)
clinical relevance: presence if IgM often indicates acute infection
increased onset of symptoms
overtime, IgM will decrease
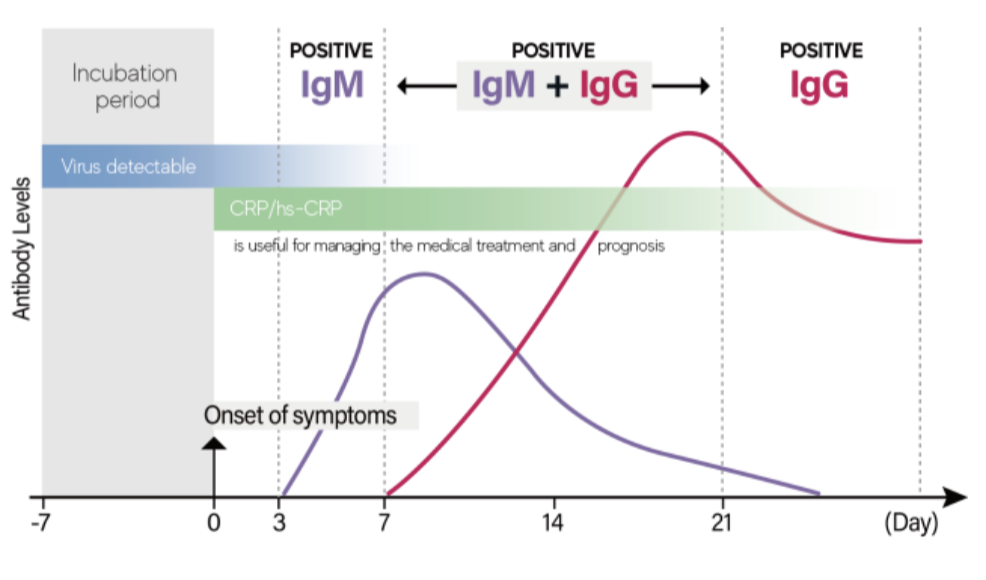
IgG
most abundant and lonG lasting
crucial role in secondary immune response (re-exposure) and development of “immunity”
clinical relevance: presence of IgG indicates “IMMUNITY” from previous infection of vaccine —> remain elevated over longer period of time, therefore longer immunity
maternal IgG crosses the placenta during pregnancy to protect newborn during first 6months of life

IgE
binds to mast cells and stimulates release of histaminE
clinical relevance: ALLERGIC REACTIONS occur when IgE is produced in response to harmless antigen (allergen)—proteins that cause response but shouldn’t
initiates responses to fight against parasitic infection
bind to PARASITE and tag fro removal eosinophils
what type of pathogen do neutrophils target?
bacteria
what targets parasites and allergens?
eosinophils —→ IgE
Helper T Cell (CD4)
interact with APCs to coordinate cellular and humoral arms of immunity
CD4 receptors bind ti APC to detect foreign antigens and initiate an immune response
*each helper T cell has SPECIFIC CD4 receptor*
what markers are used by lymphocytes to determine what cells to act against?
MHC (major histocompatibility complex) complexes
what type of MHC does every nucleated human cell possess?
MHC I
what type of cell can have MHC II
ONLY APCs
used to attach pathogen particles and presenting pathogen to lymphocyte
MHC I complex vs MHC II complex
MHC 1
all nucleated human cells
presents self antigens
presents VIRAL antigens if needed
presents MALIGNANT antigens if cancerous
MHC II
only APCs
APCs present foreign antigens on the MHC II complex
cell mediated immunity
T helper cells use CD4 receptor to read viral antigen on MHC II of APC
T helper cell releases cytokines to stimulate proliferation of cytotoxic T cells specific to that antigen
memory T cells also created
cytotoxic T cells have CD8 receptors that interact with MHC I receptors on cells to scan for viral particles that indicate infected
if infected, cytotoxic T cells destroy
what is a vaccine
harmless pieces of pathogen (antigens) that will trigger adaptive immunity but cannot cause infection
how do vaccines provide protection from pathogens?
use the immune system’s memory and robust secondary immune response
induces the production of antibodies memory T and B cells
IgM levels increase after vaccine
booster vaccine
over time, memory B cells/antibodies gradually decline. administering booster vaccine re-introduces larger and longer lasting
titters are used to assess need for 'boost” or if person is above minimum threshold and still considered immune to the pathogen
overview of immune system
bacteria enters through break in barrier defense (first defense)
resident neutrophils and macrophages engulf and digest bacteria —> release cytokines to recruit more immune cells as well as inflammatory cytokines that amplify immune response
Cell injury triggers inflammatory response
mast cells recognize PAMPS (broad specificity) on bacterial cells—> bind to corresponding to TLRon mast cell surface
mast cell degranulates and releases histamine—> increase vascular permeability and dilation
APCs link to adaptive immunity
macrophages and neutrophils serve as APCs, presenting bacterial antigen on MHC II—> travel to the spleen and lymph noes to “meet “ with helper T cells that can read their signal
humoral (B cells) and cellular (T cells) are activated
helper T cells (CD4) signal B cells to create plasma cells —> produce antibodies IF PATHOGEN IS EXTRACELLULAR THREAT (ex. bacteria)
helper T cells signal cytotoxic T cells (CD8) to create more cytotoxic cells if pathogen is an INTRACELLULAR threat
killing mechanisms engaged:
antibodies are released by plasma B cells and kill EXTRACELLULAR threats
cytotoxic T-cells release chemicals to lyse infected cells displaying antigen
memory cells created
helper T-cells signal both T and B cells to create memory cells—> allow for the more robust secondary immune response when re-exposed