26-31 Blood Physiology
1/254
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
255 Terms
Define Normovolemia, Hypervolemia, and Hypovolemia
Normovolemia: Normal blood volume; essential for proper physiological function.
Hypervolemia: Excess blood volume; can cause complications such as edema and hypertension.
Hypovolemia: Decreased blood volume; leads to inadequate perfusion and potential organ failure.
Define Normocythaemia, Oligocythaemia, and Polycythaemia
Normocythaemia: Normal RBC count and function.
Oligocythaemia: Decreased RBC count leading to potential anemia.
Polycythaemia: Increased RBC count that may cause complications related to elevated blood viscosity.
Define Acidosis, Alkalosis
Acidosis: A condition with excess acid leading to a pH below 7.35; can be respiratory or metabolic.
Alkalosis: A condition with excess base resulting in a pH above 7.45; can also be respiratory or metabolic.
Define Hypoproteinaemia, Hyperproteinaemia
Hypoproteinaemia: Low protein levels in the blood, often due to inadequate intake, malabsorption, liver disease, or kidney disorders.
Hyperproteinaemia: High protein levels in the blood, commonly caused by dehydration, chronic inflammation, or certain diseases like multiple myeloma.
Define Hyperkalaemia, Hypokalaemia
Hyperkalaemia: Elevated potassium levels (>5.6 mmol/L) that can lead to serious cardiac complications.
Hypokalaemia: Low potassium levels (<3.5 mmol/L) that can cause muscle weakness and arrhythmias.
Define Hypercalcemia, Hypocalcaemia
Hypercalcemia: Elevated blood calcium levels (>2.62 mmol/L), often due to parathyroid disorders or malignancies, with symptoms ranging from mild to severe.
Hypocalcaemia: Low blood calcium levels (<2.12 mmol/L), caused by hormonal deficiencies or nutritional deficiencies, leading to muscle and neurological symptoms.
Define Hypoglycaemia, Hyperglycaemia
Hypoglycaemia: Low blood sugar levels (<6.1 mmol/L), often leading to symptoms like shakiness and confusion, requiring prompt treatment.
Hyperglycaemia: High blood sugar levels (>2.8 mmol/L fasting), associated with symptoms like increased thirst and frequent urination, necessitating management to prevent complications.
Define Erythrocytosis, Erythropenia
Erythrocytosis: Increased RBC count, which may lead to complications like thrombosis.
Erythropenia: Decreased RBC count associated with symptoms of anemia and potential tissue hypoxia.
Define anemia
reduced ability of the blood to carry oxygen due to a deficiency in the number of red blood cells (RBCs) or a decrease in the amount of hemoglobin within those cells
Define Oxyhemoglobin, Carbaminohemoglobin, Carboxyhemoglobin, and Methaemoglobin
Oxyhemoglobin: Hemoglobin bound with oxygen; crucial for oxygen transport.
Carbaminohemoglobin: Hemoglobin bound with carbon dioxide; involved in CO2 transport.
Carboxyhemoglobin: Hemoglobin bound with carbon monoxide; can cause hypoxia.
Methaemoglobin: Oxidized form of hemoglobin that cannot bind oxygen effectively; may lead to tissue hypoxia if elevated.
Define Leucocytosis, Leukopenia
Leucocytosis: Elevated WBC count (>10.5 × 109/L), often indicating infection or inflammation.
Leukopenia: Decreased WBC count (<3.5 × 109/L), leading to increased risk of infections and related complications.
Define Lymphocytosis, Lymphopenia
Lymphocytosis: Elevated levels of lymphocytes (>3.9 × 109/L), often due to infections or malignancies.
Lymphopenia: Decreased levels of lymphocytes (<1.3 × 109/L), associated with increased infection risk and various underlying health issues.
Define Monocytosis
increase in the number of monocytes in the blood, typically > 1.0 x 10^9/L in adults.
Define Eosinophilia
abnormal increase in the number of eosinophils in the blood, > 0.13 x 10^9/L
Define Thrombocytosis, Thrombopenia
Thrombocytosis: Elevated platelet count (>400 x 10^9/L), which can be primary (essential) or secondary (reactive), potentially leading to clotting complications.
Thrombopenia: Decreased platelet count (<140 x 10^9/L), associated with increased bleeding risk due to various underlying conditions.
Functions of Blood
Transportation: It transports oxygen from the lungs to tissues and carbon dioxide from tissues to the lungs. Additionally, it carries nutrients from the digestive tract to cells and waste products to excretory organs
Regulation: Blood helps regulate body temperature, pH levels, and fluid balance. It plays a role in homeostasis by maintaining the internal environment of the body
Protection: Blood contains white blood cells and antibodies that are essential for immune responses, helping to fight infections and diseases. Platelets in the blood are crucial for clotting, preventing excessive bleeding during injuries
Volume and Components of Blood
The average blood volume in an adult is approximately 5 liters, constituting about 7-8% of total body weight. Blood is composed of:
Plasma: About 55% of blood volume, plasma is a yellowish fluid that contains water, electrolytes, proteins (like albumin and globulins), hormones, nutrients, and waste products.
Formed Elements (Cells): Approximately 45% of blood volume consists of red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). RBCs are responsible for oxygen transport. WBCs play roles in immune defense. Platelets are involved in clotting.
pH of Blood - reference values
arterial blood is 7.36-7.44
venous blood is 7.25-7.35
Bilirubin Reference Values
total: 3.4-21 micromoles/litre
direct: 0.8-8.5 micromoles/litre
Regulation of Blood Volume and Composition
Blood volume is primarily regulated by the kidneys through mechanisms that control both plasma volume and red blood cell mass. The kidneys adjust fluid balance by filtering blood, reabsorbing water and solutes, and excreting waste. Key hormones involved in this regulation include:
Antidiuretic Hormone (ADH): Increases water reabsorption in the kidneys when blood volume decreases.
Aldosterone: Promotes sodium retention, which indirectly increases water retention due to osmotic effects.
Atrial Natriuretic Peptide (ANP): Released by heart atria when blood pressure rises; it promotes sodium excretion and reduces blood volume
Plasma Constituents and Their Regulation
Plasma is primarily composed of water (about 90%), with proteins accounting for about 7-8%. The main proteins include:
4.5% Albumin: Maintains oncotic pressure and transports various substances. (In capillaries, hydrostatic pressure pushes fluid out into surrounding tissues at the arterial end, while oncotic pressure (primarily due to albumin) pulls fluid back into the capillaries at the venous end.)
2.7% Globulins: Involved in immune functions.
0.4% Fibrinogen: Essential for blood clotting.
0.9% Salts
1.5% organic substances
The concentration of these plasma constituents is regulated by dietary intake, liver synthesis (for proteins), and kidney function (for electrolytes)
Hematocrit - Definition, Reference Values and Changes in HCT levels
Hematocrit (HCT) is the volume percentage of blood cells (mostly erythrocytes) in the total blood volume.
Female 0.36-0.47 L/L (36-47%)
Male 0.40-0.54 L/L (40-54%)
higher from males than females because testosterone stimulates erythropoiesis by enhancing erythropoietin (EPO) production in the kidneys
Blood in different organs has different hematocrit values - high in the spleen, low in the kidneys and brain.
Hematocrit is reduced by anemias and increased plasma volume.
It is elevated by erythrocytosis and reduction in the blood plasma volume (loss of liquids).
Hematocrit levels can indicate various health conditions; for instance, high levels may suggest dehydration or polycythemia, while low levels may indicate anemia or other underlying issues
Blood Reservoirs - Definition
Blood reservoirs refer to areas in the body where blood can be stored or pooled.
The spleen, liver, and venous system act as reservoirs.
The spleen can store a significant amount of red blood cells and release them into circulation when needed.
During periods of high demand (e.g., physical activity), these reservoirs can quickly mobilize stored blood to maintain adequate circulation
Overview of Blood Types - ABO and Rh Systems
Blood types are classified based on the presence or absence of specific antigens on the surface of RBCs.
The two primary blood group systems are the ABO system and the Rh system, which together determine an individual's blood type.
There are four main ABO blood groups: A, B, AB, and O, each of which can be either RhD+ or RhD-, resulting in a total of 8 possible blood types.
ABO Blood Group System
The ABO blood group system is the most clinically significant for blood transfusions and organ transplants. It is characterized by:
Antigens: Two main antigens are present on RBCs:
A antigen (Type A)
B antigen (Type B)
Antibodies: Corresponding antibodies in plasma:
Individuals with Type A blood have anti-B antibodies.
Individuals with Type B blood have anti-A antibodies.
Type AB individuals have neither antibody and can receive blood from any group (universal recipients).
Type O individuals have both anti-A and anti-B antibodies and can donate to any group (universal donors)
The ABO antigens are genetically inherited and follow Mendelian principles. The presence of these antigens leads to a reciprocal relationship with antibodies.
Rh Blood Group System
The Rh system is defined by the presence or absence of the RhD antigen. If present, the individual is RhD+; if absent, they are RhD-. This system is particularly important in pregnancy and transfusions:
RhD Positive: Presence of the D antigen.
RhD Negative: Absence of the D antigen.
Approximately 85% of individuals are RhD positive, and mismatches in Rh status during transfusions can lead to serious complications
Blood Typing Methods
Blood typing involves testing a sample of blood to determine its ABO and Rh status. Common methods include:
Serological Testing: Mixing blood samples with known anti-A and anti-B antibodies to observe agglutination reactions.
Gel Testing: Using gel technology to separate agglutinated from non-agglutinated cells.
Molecular Typing: Analysing DNA to identify specific alleles associated with blood group antigens
These methods ensure accurate matching before transfusions to avoid adverse reactions.
Agglutination
Type A Blood: Agglutination occurs when mixed with anti-A serum (due to A antigens) but not with anti-B serum.
Type B Blood: Agglutination occurs with anti-B serum (due to B antigens) but not with anti-A serum.
Type AB Blood: Agglutination occurs with both anti-A and anti-B serums (due to both A and B antigens).
Type O Blood: No agglutination occurs with either anti-A or anti-B serum (no A or B antigens present).
Rh Factor: Agglutination with anti-Rh serum indicates the presence of Rh antigens; no agglutination indicates Rh-negative status.
Principles of Blood Transfusion
Blood transfusion is a critical medical procedure that requires careful matching of donor and recipient blood types to prevent hemolytic reactions. Key principles include:
Compatibility Testing: Prior to transfusion, compatibility tests are performed to ensure no agglutination occurs between donor RBCs and recipient plasma.
Universal Donors and Recipients:
Type O RhD- blood is often used in emergencies as it lacks A, B, and RhD antigens, making it compatible with all other groups.
Type AB individuals can receive from any group without risk of antibody-mediated reactions
Transfusion reactions can occur if incompatible blood types are mixed, leading to severe immune responses that may be life-threatening. Therefore, meticulous screening and testing are essential components of safe transfusion practices
Number of Erythrocytes - Reference Values
In a healthy adult, the normal range of red blood cells (RBCs) is approximately:
Men: 4.6 to 6.0 million cells per microliter (µL) or trillion cells per litre (1012/L)
Women: 3.9 to 5.3 million cells per microliter (µL) or trillion cells per litre (1012/L)
Reticulocytes - Reference Values
immature RBCs in the bone marrow
24-84 billion per litre (x 109/L)
Hemoglobin - Reference Values
female: 120-160 g/L (140 ± 20)
male: 140-180 g/L (160 ± 20)
Functions of RBCs
RBCs, also known as erythrocytes, have several critical functions:
Oxygen Transport: They carry oxygen from the lungs to tissues throughout the body via hemoglobin, a protein that binds oxygen.
Carbon Dioxide Removal: RBCs transport carbon dioxide from tissues back to the lungs for exhalation. This process involves converting carbon dioxide into bicarbonate ions in the presence of carbonic anhydrase, facilitating efficient gas exchange.
Acid-Base Balance: By regulating the levels of carbon dioxide and bicarbonate, RBCs help maintain the body's pH balance.
Erythrocyte Sedimentation Rate (ESR)
The erythrocyte sedimentation rate (ESR) is a blood test that measures how quickly RBCs settle at the bottom of a test tube over a specified period.
It is used as a non-specific indicator of inflammation in the body.
A higher ESR can indicate conditions such as infections, autoimmune diseases, or cancers, while a normal ESR suggests the absence of significant inflammation
RBC Indices - Types and Formulas
Erythrocyte indices are calculations based on RBC counts and hemoglobin levels that provide information about the size and hemoglobin content of RBCs. Key indices include:
Mean Cell Volume (MCV): Indicates the average volume of individual RBCs, helping to classify anemia as microcytic, normocytic, or macrocytic.
MCV = HCT (L/L)/RBC (1012/L)
Mean Cell Hemoglobin (MCH): Reflects the average amount of hemoglobin per RBC.
MCH = HGB (g/L)/RBC (1012/L)
Mean Cell Hemoglobin Concentration (MCHC): Measures the average concentration of hemoglobin in a given volume of packed RBCs.
MCHC = HGB (g/L)/HCT (L/L)
Iron Metabolism and Reference Values
Iron is essential for hemoglobin synthesis in RBCs. The body regulates iron metabolism through:
Dietary Intake: Iron is absorbed from food in the intestines; heme iron from animal sources is more readily absorbed than non-heme iron from plant sources.
Storage and Transport: Iron is stored in ferritin and hemosiderin and transported by transferrin in the bloodstream. The liver plays a crucial role in regulating iron levels by producing hepcidin, a hormone that controls iron absorption and release.
Recycling: Macrophages recycle iron from aged or damaged RBCs, which is reused for new erythropoiesis.
Reference Value:
In men: 12.5-26.7 micromoles/litre
In women: 10.7-23.4 micromoles/litre
Haemolysis - Definition and Factors
Hemolysis refers to the destruction of RBCs, leading to the release of hemoglobin into the bloodstream. This process can occur due to various factors:
Intrinsic Factors: Genetic defects in RBC membranes or enzymes can lead to conditions such as hereditary spherocytosis or G6PD deficiency.
Extrinsic Factors: Autoimmune reactions, infections, or mechanical damage (e.g., from artificial heart valves) can also cause hemolysis. Symptoms may include anemia, jaundice, and dark urine due to increased bilirubin levels from hemoglobin breakdown
Regulation of Erythropoiesis and RBC Count
Erythropoiesis is the process of forming RBCs. It is regulated primarily by erythropoietin (EPO), a hormone produced by the kidneys in response to low oxygen levels (hypoxia). Key regulatory mechanisms include:
Oxygen Sensing: Specialized kidney cells detect oxygen levels and adjust EPO production accordingly.
Feedback Mechanism: Increased EPO stimulates the bone marrow to produce more RBCs, enhancing oxygen delivery to tissues. Conversely, high RBC counts lead to decreased EPO production.
Nutritional Factors: Adequate levels of iron, vitamin B12, and folate are essential for effective erythropoiesis; deficiencies can lead to anemia
Types of Physiological Haemoglobin - Structure and Function
Physiological hemoglobins effectively bind and release oxygen, facilitating efficient oxygen transport from the lungs to tissues and aiding in carbon dioxide transport back to the lungs.
Hemoglobin A (Hb A):
Description: The most common type in adults, comprising about 95-98% of total hemoglobin.
Structure: Composed of two alpha (α) and two beta (β) chains (α2β2).
Function: Efficiently carries oxygen from the lungs to tissues.
Hemoglobin A2 (Hb A2):
Description: Constitutes about 2-3% of adult hemoglobin.
Structure: Composed of two alpha (α) and two delta (δ) chains (α2δ2).
Function: Its exact role is not fully understood but it may assist in oxygen transport.
Hemoglobin F (Hb F):
Description: The primary hemoglobin in fetuses and newborns, is typically present at low levels in adults.
Structure: Composed of two alpha (α) and two gamma (γ) chains (α2γ2).
Function: Has a higher affinity for oxygen than Hb A, facilitating oxygen transfer from maternal blood to the fetus.
Types of Pathological Haemoglobin - Structure and Function
Pathological hemoglobins are abnormal forms that can result from genetic mutations affecting the structure or function of hemoglobin. These variants can lead to various disorders known as hemoglobinopathies.
Hemoglobin S (Hb S):
Description: Causes sickle cell disease, a genetic disorder characterized by sickle-shaped red blood cells.
Structure: Results from a mutation in the beta-globin gene that causes valine to replace glutamic acid at position 6.
Function: Hb S can polymerize under low oxygen conditions, leading to distorted red blood cells that obstruct blood flow and cause pain.
Hemoglobin C (Hb C):
Description: Associated with a mild form of anemia.
Structure: Caused by a mutation in the beta-globin gene that leads to lysine replacing glutamic acid at position 6.
Function: Hb C does not carry oxygen as efficiently as Hb A and can lead to red blood cell abnormalities.
Hemoglobin E (Hb E):
Description: Common in Southeast Asian populations; can cause mild anemia.
Structure: Results from a mutation in the beta-globin gene leading to an amino acid change at position 26.
Function: Generally causes mild clinical symptoms but may have implications when inherited with other hemoglobin disorders.
Methemoglobinemia:
Description: A condition characterized by elevated levels of methemoglobin, where iron in heme is oxidized to the ferric state (3+)
Function: Methemoglobin cannot effectively bind oxygen, leading to tissue hypoxia and cyanosis.
Thalassemias:
These are inherited disorders characterized by reduced production of normal hemoglobin due to mutations affecting globin chain synthesis. They can be classified into:
Alpha-thalassemia: Involves underproduction of alpha globin chains.
Beta-thalassemia: Involves underproduction of beta globin chains.
WBCs - Definition + Reference Values
White blood cells, or leukocytes, are a crucial component of the immune system, responsible for defending the body against infections and foreign invaders.
They constitute about 1% of total blood volume and are produced primarily in the bone marrow.
The normal range for WBC count is approximately 3.5-10.5 billion per liter (109/L) of blood, with slight variations based on age and sex
Types of WBCs + Reference Values
Granulocytes (42-82%)
Neutrophils NF (42-76% of WBCs) - 2.2-6.5 billion per litre (109/L)
Eosinophils EO (0-4% of WBCs) - 0-0.13 billion per litre (109/L)
Basophils BA (0-2% of WBCs) - 0-0.5 billion per litre (109/L)
Agranulocytes (23-62%)
Lymphocytes LY (22-48% of WBCs) - 1.3-3.9 billion per litre (109/L)
Monocytes MO (1-14% of WBCs) - 0.1-1 billion per litre (109/L)
Neutrophils NF
Granulocytes
(42-76% of WBCs) - 2.2-6.5 billion per litre (109/L)
Function: Neutrophils are the body's first line of defense against bacterial infections. They perform phagocytosis, engulfing and digesting bacteria and other pathogens.
Characteristics: They are the most abundant type of WBC (50-70% of all WBCs - banded = 0-6%, segmented = 42-70%). Neutrophils have a multilobed nucleus, and their cytoplasm is filled with fine granules.
Life Span: Short-lived (few hours to days).
Key Role: Neutrophils are essential in acute inflammation and are involved in pus formation at infection sites.
Stab or Band cells - the presence of these can be the earliest sign of a WBC response, immature form of NFs
Eosinophils EO
Granulocytes
(0-4% of WBCs) - 0-0.13 billion per litre (109/L)
Function: Eosinophils are primarily involved in combating parasitic infections (such as those caused by worms) and play a role in allergic reactions (e.g., asthma, hay fever).
Characteristics: Eosinophils have a bilobed nucleus and cytoplasmic granules that stain bright red or orange with eosin, a dye.
Life Span: Few days in circulation but can reside in tissues for longer periods.
Key Role: Eosinophils release toxic proteins to destroy parasites and help modulate inflammation during allergic responses.
decrease in EO = stress, steroid exposure
Basophils BA
Granulocytes
(0-2% of WBCs) - 0-0.5 billion per litre (109/L)
Function: Basophils release histamine and other chemicals during allergic reactions and inflammatory responses, contributing to the development of conditions like anaphylaxis.
Characteristics: Basophils have a large, bilobed nucleus and large granules that stain dark blue with basic dyes.
Life Span: Short-lived in the bloodstream.
Key Role: They are involved in immune responses related to allergies and inflammation and release heparin to prevent blood clotting.
diminished BA = stress reactions, some allergic reactions, hyperthyroidism, prolonged steroid exposure
Lymphocytes LY
Agranulocytes
(22-48% of WBCs) - 1.3-3.9 billion per litre (109/L)
Function: Lymphocytes are central to the adaptive immune response and include B cells, T cells, and natural killer (NK) cells.
B Cells: Produce antibodies that recognize and neutralize pathogens. They also have memory capabilities for long-term immunity.
T Cells: These include Helper T cells (which aid other immune cells) and Cytotoxic T cells (which kill infected cells directly).
Natural Killer (NK) Cells: These are involved in innate immunity and can recognize and destroy infected or cancerous cells without the need for antigen presentation.
Characteristics: Lymphocytes have a large, round nucleus with a small amount of cytoplasm. They make up about 20-40% of all WBCs.
Life Span: Lymphocytes can live for days, months, or even years, depending on the type and whether they become memory cells.
Key Role: Lymphocytes play an essential role in both humoral immunity (via B cells) and cell-mediated immunity (via T cells).
Increased in viral infections, some bacterial infections, some cancers, Graves disease
Decreased in steroid exposure, some cancers, immunodeficiency, renal failure, Lupus
Monocytes MO
Agranulocytes
(1-14% of WBCs) - 0.1-1 billion per litre (109/L)
Differentiate into macrophages and dendritic cells in tissues, where they phagocytize pathogens and present antigens to T cells.
Function: Monocytes are the largest WBCs in the blood and play a role in both innate immunity and adaptive immunity. They are involved in phagocytosis and antigen presentation to other immune cells.
When monocytes move into tissues, they differentiate into macrophages or dendritic cells, which are important for phagocytosis of pathogens, dead cells, and debris.
Characteristics: Monocytes have a large, kidney-shaped nucleus and abundant cytoplasm. They make up about 2-8% of all WBCs.
Life Span: Monocytes circulate for about 1-3 days before migrating into tissues, where they can live for months.
Key Role: Monocytes and their tissue-resident forms (macrophages and dendritic cells) are crucial for innate immunity and help activate the adaptive immune system.
Increased MO = recovery from acute infection, viral illness, parasitic infections, collagen disease, and some cancers
Decreased MO = HIV infection, rheumatoid arthritis, steroid exposure and some cancers
Regulation of Leucopoiesis
Leucopoiesis is the process by which WBCs are produced in the bone marrow. This process is regulated by various factors:
Cytokines and Growth Factors: Substances such as interleukins and colony-stimulating factors (CSFs) stimulate the production and differentiation of specific types of WBCs.
Infection and Inflammation: Increased demand for WBCs during infections or inflammatory responses leads to enhanced leucopoiesis.
Hormonal Regulation: Hormones like cortisol can influence WBC production by modulating the activity of bone marrow stem cells.
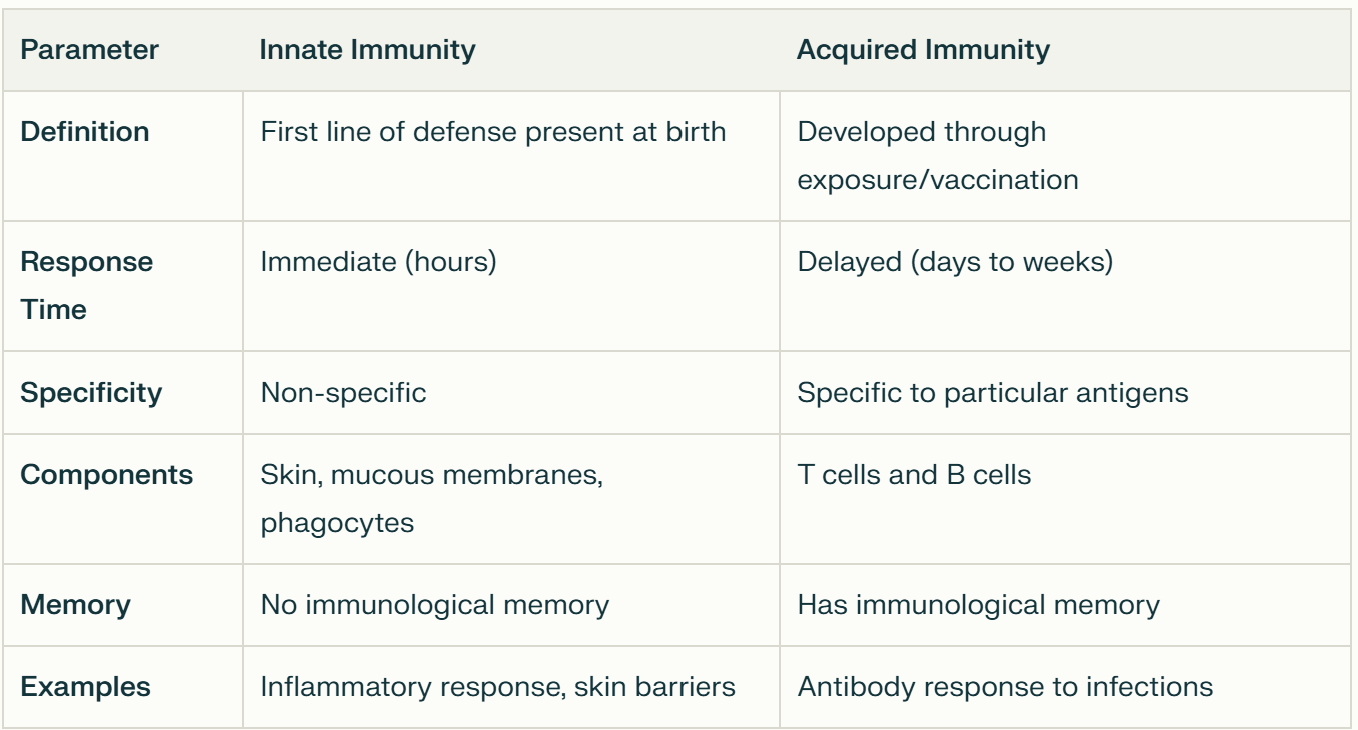
Immunity - 2 Main Types
Innate Immunity:
Neutrophils and macrophages provide immediate defense against pathogens through phagocytosis and the release of antimicrobial substances.
Present from birth
Non-specific
Doesn’t have immunological memory
Against inflammation.
Adaptive Immunity:
Lymphocytes (B and T cells) are central to adaptive immunity, providing a targeted response to specific pathogens.
B cells produce antibodies that neutralize pathogens
T cells destroy infected host cells or help orchestrate the immune response.
Developed over time
Specific
Has immunological memory
Against infections
Acquired Immunity - Types + Sub Types
Natural
Active: exposed to live pathogen, develops the disease
Passive: antibodies received from the mother (IgG from placenta before birth and through breastmilk after birth)
Artificial
Active: vaccination and immunization
Passive: medicines (antitoxins, polytoxins)
Formation of Lymph
Lymph is a clear, colorless fluid that is formed from interstitial fluid, which is the fluid that surrounds cells in tissues. The formation of lymph occurs through the following processes:
Filtration: Blood plasma leaks out of capillaries into the interstitial space, where it nourishes cells and facilitates nutrient exchange. This fluid contains water, electrolytes, proteins, and waste products.
Collection: Excess interstitial fluid is collected by lymphatic capillaries, which are small, thin-walled vessels that are permeable to larger molecules and particles. This collected fluid is termed lymph.
Content of Lymph
Water: The primary component.
Proteins: Lower concentration than in blood plasma but includes antibodies and other proteins.
Lipids: Chylomicrons (fatty particles) are present after digestion.
Cells: Lymph may contain lymphocytes (B cells and T cells), macrophages, and other immune cells.
Functions of Lymph
Fluid Balance: It returns excess interstitial fluid to the bloodstream, preventing edema (build up of bodily fluids in tissues)
Immune Function: Lymph transports immune cells throughout the body and filters out pathogens and debris via lymph nodes.
Fat Absorption: In the intestines, lymphatic vessels (lacteals) absorb dietary fats and fat-soluble vitamins from the digestive tract.
Structure of the Spleen
The spleen is a vital organ located in the left upper quadrant of the abdomen. It consists of two main types of tissue:
White Pulp: Composed primarily of lymphoid tissue, it surrounds central arterioles and contains B and T lymphocytes. This area is crucial for initiating immune responses.
Red Pulp: Made up of splenic cords (Cords of Billroth) and venous sinuses, it plays a significant role in filtering blood, removing old or damaged RBCs, and recycling iron.
Functions of the Spleen
Filtration: It filters blood by removing old or damaged erythrocytes through macrophages located in the red pulp. These macrophages phagocytize abnormal RBCs that cannot pass through the slits between endothelial cells in venous sinuses.
Immune Response: The white pulp houses immune cells that respond to pathogens. Macrophages in both red and white pulp help to initiate immune reactions by presenting antigens to lymphocytes.
Storage: The spleen serves as a reservoir for blood, storing platelets and monocytes. During times of increased demand (e.g., haemorrhage), it can release these stored components into circulation.
Iron Metabolism: The spleen recycles iron from hemoglobin during the breakdown of old red blood cells, making it available for new erythropoiesis.
Regulation of Spleen Functions
Blood Flow: The splenic artery supplies blood to the spleen, while the splenic vein drains it. Changes in blood flow can influence filtration rates and immune responses.
Hormonal Signals: Hormones such as adrenaline can stimulate contraction of splenic muscle fibers, releasing stored blood into circulation when needed.
Platelets PLT - Reference Values
thrombocytes
140-400 billion per litre (x 109/L)
Hemostasis
Hemostasis is the physiological process that prevents and stops bleeding, maintaining blood within a damaged vessel.
It involves a complex interplay of vascular, platelet, and coagulation factors, which can be categorized into three main stages:
vascular spasm
primary hemostasis
secondary hemostasis
Vascular-Platelet Hemostasis
Vascular Spasm: Immediately following vascular injury, blood vessels undergo vasoconstriction to reduce blood flow. This response is mediated by the release of substances such as endothelin from endothelial cells and thromboxane A2 from activated platelets.
Primary Hemostasis: This phase involves the formation of a temporary platelet plug at the site of injury:
Platelet Adhesion: Platelets adhere to exposed collagen fibers in the damaged vessel wall, facilitated by von Willebrand factor (vWF), which acts as a bridge between platelets and collagen.
Platelet Activation: Adhered platelets become activated, releasing granules containing ADP, thromboxane A2, and other mediators that recruit additional platelets to the site.
Platelet Aggregation: Activated platelets aggregate to form a stable plug, effectively sealing small vascular injuries.
Coagulation Hemostasis
Secondary hemostasis involves the coagulation cascade, which stabilizes the platelet plug through fibrin formation. This cascade can be initiated via two pathways:
Intrinsic Pathway: Activated by factors within the blood (e.g., exposure to collagen), leading to a series of reactions that activate factor X.
Extrinsic Pathway: Triggered by tissue factor (factor III) released from damaged tissues, which interacts with factor VII (proconvertin - dependent on vit.k) to activate factor X.
Both pathways converge at the common pathway:
Activation of Factor X: Factor X is activated to Xa, which converts prothrombin (factor II) into thrombin (factor IIa).
Fibrin Formation: Thrombin converts fibrinogen (factor I) into fibrin strands, which weave through the platelet plug, solidifying it into a stable clot.
Fibrinolysis
Fibrinolysis is the process that removes clots after healing:
Plasminogen is incorporated into the clot and later activated to plasmin by tissue plasminogen activator (tPA) or urokinase.
Plasmin digests fibrin strands, leading to clot dissolution.
Anticlotting Mechanisms
Antithrombin III: Inhibits thrombin and other coagulation factors.
Protein C and S: Inactivate factors Va (proaccelerin = cofactor for prothrombin activation) and VIIIa (tissue factor = cofactor of extrinsic pathway of prothrombin activator formations), reducing further clot formation.
Regulation of Hemostasis
Hemostasis is tightly regulated to prevent excessive bleeding or thrombosis:
Feedback Mechanisms: The coagulation cascade is regulated by positive feedback loops (e.g. thrombin amplifying its own production) and negative feedback mechanisms (e.g. antithrombin III).
Balance Between Coagulation and Fibrinolysis: The body maintains a delicate balance between clot formation and breakdown to ensure that clots form when needed but are also removed once healing occurs.
Functions of Blood
Transport of Substances
Oxygen and Carbon Dioxide: Blood transports oxygen from the lungs to tissues throughout the body and carries carbon dioxide, a waste product, from tissues back to the lungs for exhalation. Red blood cells, which contain hemoglobin, are essential in this process.
Nutrients: After digestion, blood carries nutrients like glucose, amino acids, fatty acids, vitamins, and minerals from the gastrointestinal tract to tissues.
Waste Products: Blood transports waste products such as urea, creatinine, and bilirubin to the kidneys, liver, and lungs for excretion.
Hormones and Enzymes: Blood acts as a medium for endocrine glands to distribute hormones throughout the body, allowing for regulation of processes like metabolism, growth, and mood.
Regulation of Body Functions
Temperature Regulation: Blood helps to distribute heat produced by metabolic reactions. Blood vessels in the skin can dilate to release excess heat or constrict to conserve heat, maintaining body temperature.
pH Balance: Blood maintains acid-base balance (pH) by acting as a buffer. Bicarbonate and other ions in blood help neutralize excess acids or bases, keeping the blood pH within a narrow range (around 7.35-7.45).
Fluid and Electrolyte Balance: Blood plasma contains electrolytes like sodium, potassium, and calcium, which are essential for muscle function, nerve signaling, and maintaining fluid balance.
Protection and Immune Defense
Clotting Mechanism: When blood vessels are damaged, platelets and clotting proteins in the blood activate to form clots, preventing excessive blood loss and allowing healing.
Immune Response: White blood cells (leukocytes) in the blood defend against infection. Different types of leukocytes target bacteria, viruses, and other pathogens, while antibodies recognize and neutralize foreign invaders.
Antibody Production: Blood transports antibodies and other immune proteins that help identify and neutralize foreign pathogens, providing immunity.
Nutrient Reservoir: Blood serves as a reserve for certain nutrients, such as amino acids and lipids, that can be mobilized during periods of need.
Signal Transmission: Blood also serves as a vehicle for signaling molecules like cytokines, which help regulate inflammation and immune responses.
Define blood volume
Blood volume is the total amount of blood circulating in the body, typically consisting of both plasma (the liquid component) and blood cells (mainly red blood cells).
Blood volume plays a crucial role in maintaining blood pressure, ensuring adequate circulation, and supplying oxygen and nutrients to tissues.
Normal Blood Volume - in adults, children and distribution
Adults: In healthy adults, blood volume is approximately 5-6 liters or about 70-80 mL per kilogram of body weight.
Children: Blood volume varies by age and body size, with infants and children having a relatively higher blood volume per kilogram.
Distribution: About 60% of blood volume is in veins and venules, 15% in arteries, 12% in the pulmonary circulation, and 8% in capillaries and arterioles.
Increased Blood Volume - Hypervolemia (causes and effects)
Causes of Hypervolemia:
Excessive Fluid Intake: Consuming large amounts of fluids, especially in cases of intravenous (IV) therapy.
Kidney Dysfunction: Conditions like chronic kidney disease may lead to fluid retention because the kidneys can't effectively filter excess fluid.
Heart Failure: The heart cannot pump effectively, causing blood to pool, especially in the venous system, and leading to fluid retention.
Hormonal Imbalances: Overproduction of antidiuretic hormone (ADH) or aldosterone can increase fluid retention.
Effects of Increased Blood Volume:
Increased Blood Pressure: Higher blood volume raises blood pressure, as there is more fluid in the vascular system.
Edema: Excess fluid can move into tissues, causing swelling, especially in extremities (hands, feet).
Heart Strain: The heart must work harder to pump the extra volume, potentially worsening heart failure or leading to heart strain.
Reduced Blood Volume - Hypovolemia (causes and effects)
Causes of Hypovolemia:
Dehydration: Lack of fluid intake or excessive fluid loss from vomiting, diarrhea, sweating, or fever.
Hemorrhage: Loss of blood through bleeding, whether internal or external.
Severe Burns: Fluid loss through damaged skin can deplete blood volume.
Diuretics and Kidney Disease: Certain medications or kidney dysfunction can lead to excessive fluid loss.
Effects of Reduced Blood Volume:
Low Blood Pressure (Hypotension): Reduced blood volume lowers pressure in blood vessels, potentially leading to dizziness and fainting.
Poor Circulation: Reduced blood flow can deprive organs and tissues of oxygen and nutrients, risking tissue damage.
Shock: Severe hypovolemia can lead to hypovolemic shock, a life-threatening condition where the organs can no longer get enough blood and oxygen.
Regulation of Blood Volume
The body regulates blood volume through several mechanisms that adjust fluid intake, output, and redistribution to maintain homeostasis:
Kidneys:
Renin-Angiotensin-Aldosterone System (RAAS): When blood volume drops, kidneys release renin, triggering a cascade that eventually releases aldosterone. Aldosterone increases sodium and water reabsorption, expanding blood volume.
Antidiuretic Hormone (ADH): The hypothalamus detects low blood volume and signals the release of ADH, which promotes water retention in the kidneys to increase blood volume.
Thirst Mechanism:
Controlled by the hypothalamus, this mechanism is triggered by increased plasma osmolarity (high solute concentration) or decreased blood volume, stimulating thirst and encouraging fluid intake.
Atrial Natriuretic Peptide (ANP):
Released by the heart's atria in response to increased blood volume, ANP promotes sodium and water excretion by the kidneys, reducing blood volume and lowering blood pressure.
Capillary Fluid Shift:
If blood volume decreases, fluid shifts from tissues into the capillaries to help stabilize blood pressure. Conversely, excess fluid in the vascular system can shift into tissues, which helps reduce blood volume.
Baroreceptor Reflex:
Specialized pressure sensors (baroreceptors) in the aorta and carotid arteries sense changes in blood pressure and send signals to adjust heart rate, blood vessel diameter, and blood volume accordingly.
List the major blood reservoirs in the body
veins
spleen
liver
skin
lungs
heart
Veins as a major blood reservoir in the body
Primary Reservoir: Veins, especially in the liver, spleen, and skin, act as the main blood reservoirs, holding about 60-70% of the total blood volume at any given time.
High Capacity, Low Pressure: Veins have a high capacity to hold blood because they are more distensible (stretchable) than arteries and operate at a lower pressure. This flexibility allows them to store or release blood as needed.
Venous Constriction: In situations like blood loss or exercise, sympathetic nervous system activation can cause venous constriction, pushing stored blood back into the circulation to maintain blood pressure and increase cardiac output.
Spleen as a major blood reservoir in the body
Red Pulp: The spleen has a specialized region called the red pulp, where a significant amount of blood is stored, particularly red blood cells. This region can hold up to 100-300 mL of blood that can be quickly released in response to blood loss or increased demand.
Blood Filtering and Recycling: The spleen also filters blood, removes aged or damaged red blood cells, and plays a role in immune response by producing white blood cells.
Liver as a major blood reservoir in the body
Large Venous Sinuses: The liver contains large venous sinuses that store about 10-15% of the body's blood volume. These sinuses can expand or contract to release or store blood as needed, making the liver a flexible blood reservoir.
Function in Blood Volume Regulation: In response to reduced blood volume or pressure, blood stored in the liver can be released back into circulation to support vital functions.
Skin as a major blood reservoir in the body
Vascular Network: The skin has a large network of blood vessels that can store or release blood in response to temperature changes. When body temperature rises, more blood flows to the skin to release heat. In cold conditions, blood flow to the skin decreases to conserve heat and maintain core body temperature.
Role in Blood Pressure: By adjusting blood flow, the skin can help regulate blood pressure, particularly during physical activity or environmental temperature changes.
Lungs as a major blood reservoir in the body
Pulmonary Circulation: The lungs hold a considerable amount of blood, around 450 mL, and can serve as a reservoir. Blood in the lungs is easily accessible for oxygenation and can be mobilized in response to physical demands.
Capacity for Redistribution: In response to changes in posture or pressure, the lungs can adjust their blood volume to accommodate changes in the systemic circulation, helping maintain cardiac output.
Heart as a major blood reservoir in the body
Right and Left Atria: The atria of the heart can also serve as temporary reservoirs. The right atrium, in particular, receives venous blood and holds it before passing it to the ventricles.
Response to Demand: When demand increases, such as during exercise, the atria can help by adjusting blood volume, ensuring a more efficient blood flow and cardiac output.
Role of Blood Reservoirs in Physiological Regulation
Hemorrhage: When blood volume is lost due to injury or bleeding, blood reservoirs release stored blood to help maintain blood pressure and supply oxygen to vital organs.
Exercise: During physical activity, blood stored in the veins and spleen can be mobilized to increase circulation to muscles.
Stress and Shock: In stress or shock, reservoirs help compensate for sudden demands, allowing blood pressure and tissue perfusion to be maintained temporarily.
These reservoirs, especially under control of the autonomic nervous system, help ensure that the body can respond dynamically to changes in activity level, blood volume, and environmental conditions
Define hematocrit
Hematocrit (HCT) is the volume percentage of whole blood that is made up of red blood cells (RBCs) in the total blood volume.
It is an important measure of blood’s ability to carry oxygen, and abnormal hematocrit levels can indicate various health conditions.
How is haematocrit measured?
Hematocrit is usually measured as part of a complete blood count (CBC) test. A blood sample is spun in a centrifuge, causing the heavier red blood cells to settle at the bottom of the tube, with the plasma (liquid component of blood) on top. Hematocrit is calculated as the percentage of RBCs in relation to total blood volume.
Reference Values for Hematocrit
Normal hematocrit values vary based on age, sex, and sometimes altitude:
Adult Men: 0.40-0.54 L/L (40-54%)
Adult Women: 0.36-0.47 L/L (36-48%)
Newborns: 55-68% (higher than adults but decreases after birth)
Children (varies by age): Typically 30-44%
These ranges can vary slightly depending on the laboratory standards and geographic location, as people living at higher altitudes may naturally have higher hematocrit values to compensate for lower oxygen levels.
Increased Hematocrit (Polycythemia) - causes, effects and thresholds
Causes of Increased Hematocrit:
Dehydration: Loss of fluid increases the concentration of red blood cells in blood.
Chronic Hypoxia: Conditions that lower blood oxygen (e.g., chronic obstructive pulmonary disease, living at high altitudes) can stimulate red blood cell production to increase oxygen transport.
Polycythemia Vera: A bone marrow disorder causing excessive red blood cell production.
Anabolic Steroid Use: Can stimulate RBC production and increase hematocrit.
Effects of Increased Hematocrit:
Thicker Blood: Higher hematocrit makes blood more viscous, which can slow circulation and increase the risk of blood clots.
Increased Blood Pressure: Thicker blood requires more force to circulate, which can increase blood pressure and strain the heart.
Thresholds: In general, hematocrit values above 52% in men and 48% in women are considered elevated and may require further investigation.
Reduced Hematocrit (Anemia) - causes, effects and thresholds
Causes of Reduced Hematocrit:
Blood Loss: Acute or chronic bleeding, from injuries, surgery, or internal conditions (e.g., gastrointestinal bleeding), can reduce hematocrit.
Nutritional Deficiencies: Low iron, vitamin B12, or folic acid levels can impair red blood cell production, reducing hematocrit.
Bone Marrow Disorders: Conditions like aplastic anemia or certain cancers can decrease red blood cell production.
Chronic Disease: Kidney disease, liver disease, or chronic inflammatory conditions can lead to low hematocrit.
Overhydration: Excessive fluid dilutes the blood, reducing hematocrit.
Effects of Reduced Hematocrit:
Reduced Oxygen Carrying Capacity: Lower hematocrit reduces the amount of oxygen that can be transported to tissues, potentially causing fatigue, weakness, and shortness of breath.
Potential Heart Strain: To compensate for reduced oxygen-carrying capacity, the heart may work harder to circulate blood, which can strain the cardiovascular system over time.
Thresholds: Hematocrit values below 39% in men and 35% in women are generally considered low and may indicate anemia or other underlying issues.
Clinical Importance of Monitoring Hematocrit
Monitoring hematocrit is important for diagnosing and managing various health conditions:
Anemia: Low hematocrit often points to anemia, prompting further investigation into causes like iron deficiency or chronic disease.
Polycythemia: High hematocrit may indicate polycythemia or a compensatory response to hypoxia, particularly in smokers or those with lung disease.
Hydration Status: Hematocrit can also give clues about a person’s hydration, helping guide treatment in dehydration or overhydration cases.
Regular monitoring of hematocrit, especially in patients with chronic conditions or those undergoing certain treatments, helps detect changes in red blood cell levels and assess overall health.
Define blood plasma
Blood plasma, the liquid component of blood, is about 90% water but contains a variety of organic and inorganic substances.
The organic constituents of blood plasma are crucial for physiological functions, supporting cellular metabolism, immune defense, blood clotting, and nutrient transport.
List the components of the blood plasma
plasma proteins
lipoproteins
glucose
amino acids
nitrogenous waste products
hormones
enzymes
vitamins
organic acids and buffers
Plasma Proteins in the blood plasma - types (with reference values)
Plasma proteins are the most abundant organic constituents in blood plasma, constituting 6-8% of plasma by weight (60-83g.l-1). They are essential for maintaining blood pressure, coagulation, osmotic pressure, immune defense, blood clotting, and transporting molecules.
Albumin - 35-55g.l-1
Globulins - Alpha-1 (1-3g.l-1), Alpha-2 (6-10g.l-1), Beta (7-14g.l-1), Gamma (7-16g.l-1)
Immunoglobulins: IgG (8-18g.l-1), IgA (0.7-4.5g.l-1), IgM (men 0.6-2.5g.l-1, women 0.7-2.8g.l-1), IgD (0.03-0.4g.l-1), IgE (0.017-0.45g.l-1)
Fibrinogen - 2-4g.l-1
Clotting Factors
Complement Proteins
Regulatory Proteins (e.g., Hormones, Enzymes)
Albumin - plasma protein - concentration, production, functions
Concentration: Albumin is the most abundant plasma protein, comprising approximately 55-60% of total plasma proteins, with a concentration of 35-55g.l-1.
Produced by: Liver
Functions:
Maintains Oncotic Pressure: Albumin plays a critical role in maintaining colloid osmotic pressure, which helps retain water within blood vessels and prevents excessive fluid from leaking into tissues.
Transporter: Albumin binds and transports various substances in the blood, including hormones (like thyroid hormones), fatty acids, bilirubin, calcium, and drugs. It facilitates their solubility and availability to tissues.
Nutrient Source: During starvation or malnutrition, albumin can be broken down to provide amino acids for protein synthesis.
Globulins - plasma protein - concentration, types, production, functions
Concentration: Globulins account for about 35-40% of plasma proteins, with concentrations ranging from Alpha-1 (1-3g.l-1), Alpha-2 (6-10g.l-1), Beta (7-14g.l-1), Gamma (7-16g.l-1) They are further divided into alpha, beta, and gamma globulins, each with different functions.
Types: Alpha, beta, and gamma globulins
Alpha Globulins:
Produced mainly by the liver.
Include proteins like alpha-1 antitrypsin (protects tissues from enzymes of inflammatory cells) and thyroxine-binding globulin (transports thyroid hormone).
Beta Globulins:
Also produced by the liver.
Includes proteins like transferrin (transports iron), plasminogen (involved in blood clot breakdown), and lipoproteins (carry fats and cholesterol in the blood).
Gamma Globulins (Immunoglobulins):
Produced by B lymphocytes and plasma cells.
Includes antibodies (IgG, IgA, IgM, IgE, IgD), which play a central role in immune defense by recognizing and neutralizing pathogens like bacteria, viruses, and toxins.
Immunoglobulins: IgG (8-18g.l-1), IgA (0.7-4.5g.l-1), IgM (men 0.6-2.5g.l-1, women 0.7-2.8g.l-1), IgD (0.03-0.4g.l-1), IgE (0.017-0.45g.l-1).
Fibrinogen - plasma protein - concentration, production, functions
Concentration: Fibrinogen makes up about 4-6% of plasma proteins, with a concentration of approximately 0.2-0.4 g/dL.
Produced by: Liver
Function: Fibrinogen is essential for blood clotting. During injury, fibrinogen is converted to fibrin, which forms a mesh-like structure that stabilizes blood clots and prevents excessive blood loss.
Blood Clotting: Fibrinogen is an essential clotting protein. In response to vessel injury, fibrinogen is converted by the enzyme thrombin into fibrin, which forms a mesh-like network that stabilizes blood clots and prevents blood loss.
Acute Phase Reactant: Fibrinogen levels can increase during inflammation, as it is part of the body's acute-phase response to injury or infection.
Clotting factors - plasma protein - examples, functions
Examples: Prothrombin, factor VIII, and factor IX
Function: These proteins, produced mainly by the liver, are involved in the complex cascade that leads to blood clot formation, an essential process for stopping bleeding and healing wounds.
Complement Proteins - plasma protein - concentration and functions
Concentration: A variety of complement proteins are present in plasma in smaller amounts.
Function: Complement proteins (e.g., C3, C4) are part of the immune system. They work with antibodies and phagocytic cells to destroy pathogens, enhance inflammation, and promote immune responses.
Regulatory Proteins (e.g., Hormones, Enzymes) - plasma protein - concentration and functions
Concentration: These proteins are typically present in trace amounts.
Function: Hormones and enzymes regulate many metabolic and physiological processes. For example, enzymes like coagulation factors (prothrombin, factor VIII) are vital for blood clotting, while hormones regulate cellular functions, growth, and metabolism.
Lipoproteins in the blood plasma - types with reference values
Lipoproteins are complexes of lipids and proteins that allow lipids to be transported in the bloodstream.
Types:
Chylomicrons: Transport dietary lipids (mainly triglycerides) from the intestines to other tissues.
Low-Density Lipoprotein (LDL): Known as "bad cholesterol," it carries cholesterol to tissues but can contribute to plaque formation in arteries. (up to 3.0 mmol.l-1)
High-Density Lipoprotein (HDL): Known as "good cholesterol," it transports cholesterol from tissues back to the liver for excretion or reuse. (above 1.0 mmol.l-1)
Very Low-Density Lipoprotein (VLDL): Transports triglycerides synthesized by the liver to adipose and muscle tissue.
Functions: Lipoproteins are essential for lipid transport and metabolism. They provide energy storage (triglycerides) and structural components for cell membranes (cholesterol).
Glucose in blood plasma - with reference values
Glucose is the primary energy source for cells, especially the brain and red blood cells, which rely almost entirely on glucose for their energy needs. It is transported in plasma and regulated by hormones like insulin and glucagon to maintain blood glucose levels within a narrow range.
blood sugar (fasting): 2.8-6.1 mmol.l-1
glycated hemoglobin HbA1c: up to 6.4%
Amino acids in blood plasma
Source: Derived from dietary proteins or protein breakdown in the body.
Function: Amino acids serve as building blocks for protein synthesis, supporting cell repair, growth, and maintenance. They are also involved in neurotransmitter synthesis and other metabolic functions.
Nitrogenous Waste Products in the blood plasma
Examples: Urea, uric acid, and creatinine
Function: These are metabolic waste products derived from protein and nucleic acid breakdown. They are transported in plasma to the kidneys for excretion, playing a role in detoxifying the blood and maintaining metabolic balance.
Hormones in the blood plasma
Source: Endocrine glands, including the thyroid, adrenal glands, pancreas, and pituitary.
Function: Hormones regulate various physiological processes, including metabolism (e.g., insulin, thyroid hormones), growth and development (e.g., growth hormone), stress responses (e.g., cortisol, adrenaline), and reproductive functions (e.g., estrogen, testosterone).
Enzymes in the blood plasma
Although enzymes are usually present in low amounts in plasma, they are involved in metabolic processes, including breaking down nutrients, aiding in blood clotting, and helping with immune responses. Some enzymes serve as markers of tissue damage (e.g., creatine kinase for muscle damage).
Vitamins in the blood plasma
Types: Fat-soluble (A, D, E, K) and water-soluble (B-complex, C)
Function: Vitamins are crucial for cellular metabolism, immune function, blood clotting (e.g., vitamin K), and antioxidant protection (e.g., vitamin C, vitamin E). They act as cofactors in enzyme reactions and are essential for many biochemical pathways.
Organic acids and buffers in blood plasma
Examples: Lactate, bicarbonate
Function: These organic molecules help in maintaining acid-base balance in the blood. Bicarbonate acts as a primary buffer, helping to regulate pH, while lactate levels increase in anaerobic conditions (e.g., strenuous exercise), indicating energy production under low oxygen.
Summary of Functions of Organic Constituents in Blood Plasma
Transport: Plasma proteins, glucose, lipoproteins, and amino acids help transport nutrients, waste products, and other molecules.
Regulation: Hormones and vitamins play roles in regulatory processes, while enzymes and buffers help maintain homeostasis.
Protection: Immunoglobulins and clotting factors protect against infection and prevent blood loss.
Energy and Nutrition: Glucose and lipoproteins serve as energy sources, while amino acids support tissue repair and growth.