Oncology 1 (Introduction, Lymphoma, Dx)
1/199
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
200 Terms
What are the goals of veterinary oncology?
- Provide care to animals diagnosed with cancer (often palliative vs. curative)
- Inform client of disease progression and clinical signs
- Discuss plan for end-of-life care
Why does veterinary medicine not have the same remission/cure rates as human oncology?
- We do not use the same doses of chemotherapy or intensity of multi-drug protocols because we cannot ask Fido if they want to go through it
True or false: Cancer patient co-morbidities can affect monitoring, therapy side effects, safe chemotherapeutics to administer, and contribute to caregiver burden.
- True
There is likely an ____________ of studies related to veterinary oncology where beneficial effects were not seen or deleterious effects occurred.
- Underreporting
Cancer growth follows an ______________ model.
- Sigmoidal
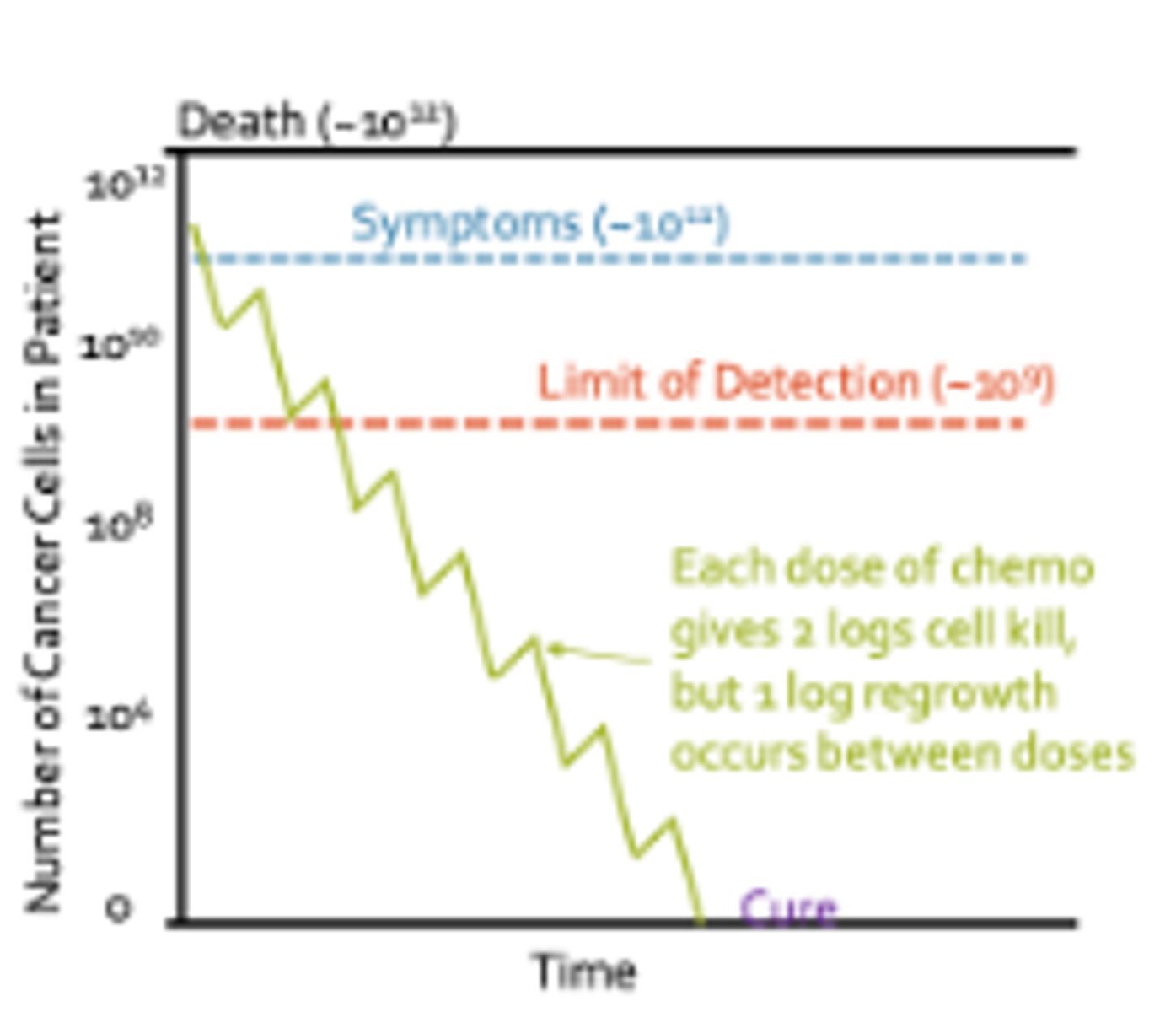
What is the limit of detection for cancer cells? What about the point in which symptoms develop?
- Limit of detection: 10^9 cells
- Symptoms: 10^11 cells
(Death: 10^12 cells)
What cancer treatment options are available for local disease control?
- Surgery
- Radiation
What cancer treatment options are available for systemic disease control?
- Chemotherapy
- Immunotherapy (i.e., prednisone)
Chemotherapy is rarely used with much success on solid tumors with the exception of _____________________.
- Lymphoma
Define the following terms as they relate to veterinary oncology.
A. Adjuvant
B. Neoadjuvant
C. Induction therapy
D. Rescue therapy
A. Adjuvant: Treatment with chemotherapeutic agent after achieving control of the primary tumor with surgical resection or radiation therapy
B. Neoadjuvant: Chemotherapy used prior to treatment with other modalities for local tumor control, with the intent of decreasing the tumor size
C. Induction Therapy: Chemotherapy treatment with the intent of a cure; Initial protocol
D. Rescue Therapy: Use of chemotherapy after a tumor fails to respond to a previous therapy or after tumor recurrence
Each dose of chemotherapy kills _____________"logs" of cells, but there is ~________ "log" of cell regrowth between doses.
- 2
- 1
Define the following terms.
A. Maximum tolerated dose
B. Biologically effective dose
C. Metronomic dose
A. MTD: Highest dose of a given drug that can be administered in the absence of unacceptable or irreversible side effects; Most chemotherapy protocols
B. BED: Response at a putative target that is related to the mechanism of action of the agent; Targeted therapies like Palladia
C. Low-dose chemotherapy given on daily to every-otherday schedule. Aimed to slow progression of tumor through multiple mechanisms (angiogenesis, tumor immunology)
Define the following terms:
A. Complete remission/response
B. Partial remission/response
C. Stable disease
D. Progressive disease
E. Progression-free interval/survival
F. Disease-free interval/survival
A. CR: Complete disappearance of tumor(s) and symptoms of disease
B. PR: At least 30% reduction in the sum of diameters of target lesions
C. SD: Less than 30% reduction or 20% increase in the sum of diameters of target lesions
D. PD: Either the appearance of one or more new lesions or at least a 20% increase in the sum of diameters of target lesions
E. PFI: The amount of time elapsed without evidence of progressive tumor growth or death
F. DFI: The amount of time that elapses without disease recurrence
In studies, what does overall response rate encompass? What about biological response rate?
- ORR: Complete remission and partial response
- BRR: Complete remission, partial response, and stable disease
What is an adverse event in veterinary oncology?
- Any unfavorable and unintended clinical sign or disease temporally associated with the use of a medical treatment that may or may not be considered related to the medical treatment
What is the grading scale for adverse events in veterinary oncology?
Grade 1 - mild
Grade 2 - moderate
Grade 3 - severe or medically significant
Grade 4 - life-threatening
Grade 5 - death
Chemotherapy targets which cells in the body? How does this relate to side effects?
- All rapidly dividing cells, including normal cells that are always replicating like bone marrow, GI, and hair follicle cells
- This non-selectivity can result in side effects
What is a nadir?
- The lowest point in bone marrow suppression following chemotherapy, usually 5-7 days post-dose
What is the half life of the following cells?
A. Neutrophils
B. Platelets
C. RBCs
A. Neutrophils: Hours to 1 day (shortest - why we monitor them closely)
B. Platelets: 7-10 days
C. RBCs: 100-120 days (dogs); 70-80 days (cats)
Note: 1, 10, 100 rule
What monitoring should be performed while a patient is undergoing chemotherapy to evaluate bone marrow suppression?
- CBC
- Slide reviews for platelet estimates
What GI side effects are associated with chemotherapy and when do they typically occur?
- Nausea, vomiting, diarrhea
- 3-5 days post-treatment for most patients
What prophylactic treatments can be used to prevent/minimize GI side effects in patients undergoing chemotherapy?
- Anti-nausea medications
- Fasting? (Noted in people that fasting for personal reasons before chemo resulted in less side effects, specifically nausea and vomiting)
- Microbiome?
When patients experience neutropenia secondary to chemotherapy, when should antibiotics be utilized? When should they be hospitalized?
- PO ABX with a repeat CBC in 2-3 days if patient is normothermic and neutrophils are between 500-1000
- IV ABX if neutrophils <500 with repeat CBC in 24 hours and hospitalize if the patient is febrile
What is the focus of palliative supportive care?
- Focusing on alleviating symptoms related to cancer diagnosis (Pain management, nutritional management, supportive medications)
What tumors are known to be particularly painful?
- Bone
- CNS
- Oral cavity
- GI
- Nasal
- Urogenital
What pain management options are available for cancer patients undergoing palliative care?
- Medications: NSAIDs, Gabapentin, Opioids, Amantadine
- Bisphosphonates: Controversial
- Acupuncture
- Radiation
Why is it sometimes recommended that cancer patients be on a diet which is low in CHOs and high in protein +/- fat
- "Warburg Effect"- glycolysis is the primary pathway for energy production in cancer cells -> Neoplastic cells propagate better in high glucose media
True or false: Anorexia and cachexia are common clinical signs in cancer patients.
- False; Can occur, but not as commonly as in human medicine; Patients are often obese
True or false: If a patient is eating, then their caloric needs are being met.
- False; Just because a patient is eating does not mean they are eating enough
True or false: Energy requirement equations have a 50% variability in accuracy and may not meet a patient's caloric needs.
- True
What are scoring metrics for nutritional management/support in cancer patients?
- BCS
- Muscle condition score
What are some clinical tips for cancer patients with hyporexia or anorexia?
- Different flavors, formulations, toppers, broths
- Paper plates: Dogs and cats have way better sensory olfactory - smell things in tupperware, steel
- Feeding tubes
What supportive medications can be used in cancer patients undergoing palliative care?
- Anti-nausea: Maropitant, Ondansetron, Metoclopramide
- Gastroprotectants: Sucralfate, Omeprazole, Famotidine
- Anti-diarrheal: Metronidazole, Tylosin, Loperamide Immodium, Crofelemer Canalevia (FDA approved specifically for chemotherapy-induced diarrhea)
- Appetite Stimulant: Capromorelin Entyce/Elura, Mirtazapine
In what forms of neoplasia might you want to use NSAIDs over steroids?
- Cases of pain and inflammation
- Carcinomas (have high COX-2 expression)
In what forms of neoplasia might you want to use steroids over NSAIDs?
- Round cell tumors
- Consider steroid side effects
Define the following terms:
A. Caregiver burden
B. QOL
C. Grief
A. Strain owing to caregiving due to subjective (emotional) + objective (physical) demands of caregiving
B. Sense of life's "goodness"; Client's subjective evaluation of positive and negative aspects of own life
C. Bereavement reaction involving feelings of sadness and despair owing to a loss of anticipated loss
What are some steps veterinarians can take to minimize caregiver burden on clients?
- Treat every client as an individual
- Avoid minimizing the feelings of burden
- Share the power of knowledge (www.petcaregiverburden.com)
- Create a collaborative care plan (i.e., streamline medications, help appetite, etc.)
- Help client problem solve
- Offer words of encouragement
What are some tips/tricks for assessing QOL?
- Complete at different times of day (mobility may change throughout the day)
- Request multiple members of family to complete and compare observations
- Take periodic photos to help
What is the incidence of neoplasia in cats and dogs?
- 1:3 Dogs
- 1:4 Cats
Cancer describes a large number of diseases whose common feature is...
- Uncontrolled growth
Briefly describe the following classifications of tumors:
A. Benign
B. In-situ
C. Cancer
A. Benign: Tumors which can arise in any body tissue and grow locally but do NOT metastasize, though they can still result in morbidity/mortality
B. Often small tumors that arise in epithelium which histologically appear to contain cancer cells that have not invaded the basement membrane and could develop into malignancy
C. Malignant tumor with the capacity for both local and distant invasion
What are some factors which may contribute to the "cause" of cancer?
- Lifestyle/habits
- Genetics
- Chemical carcinogens
- Ionizing or UV radiation
- Viruses/bacteria/parasites
- Environmental factors
True or false: Cancer is a genetic disease and is always heritable
- False; Cancer is a genetic disease, however it is not always heritable
Tumors can arise from an accumulation of mutations that...
- Eliminate normal constraints on proliferation and genetic integrity
What is "mutagen"?
What are some vet med examples of the multifactorial causes of cancer?
- Rural vs. urban area
- Radiation exposure resulting in nasal planum/cutaneous SCC
- Pesticides/herbicides/insecticides increasing occurrence of bladder cancer
- Hormonal exposure
Which breeds are predisposed to TCC?
- Beagles (x3), Scotties (x21), West Highland white terriers (x6)
What are the three stages of carcinogenesis?
1) Initiation
2) Promotion
3) Progression
What is initiation?
- Interaction of the carcinogen with cellular DNA in which DNA damage may remain undetected for life unless further events stimulate the tumor environment
True or false: An initiated cell is NOT a cancer cell, yet
- True
True or false: Initiation is irreversible.
- False
What is promotion? Can tumors develop from promotion without initiation?
- Clonal expansion of an initiated cell to produce a larger population of cells at risk of further genetic change
- Tumors cannot develop if only the promoter is applied, or if promoter is applied before initiation occurs
What is progression?
- Tumor obtains ability to invade tissues and metastasize to distant locations
What are hallmarks of tumor progression?
- Increased genetic instability
- Nuclear alterations
What are the hallmarks of cancer?
1) Sustaining proliferative signaling
2) Evading growth suppressors
3) Resisting cell death
4) Inducing angiogenesis
5) Enabling replicative immortality
6) Activating invasion and metastasis
How do cancer cells differ from normal cells in regards to proliferative signaling?
- Normal cells require mitogenic stimuli for growth and proliferation
- Cancer cells produce growth factor ligands, and induce expression of the corresponding receptors → resulting in autocrine stimulation and proliferation
- Cancer cells may disrupt negative-feedback mechanisms that normally attenuate/inhibit growth
How do cancer cells differ from normal cells in regards to growth suppression?
- In normal cells, multiple anti-proliferative signals operate to maintain homeostasis and push the cell either into G0 or post-mitotic state
- Cancer cells evade these signals to continue proliferating
What are some examples of growth/tumor suppressor proteins?
- Retinoblastoma (Rb)
- P53
What is angiogenesis?
- New blood vessel growth from existing blood vessels
Normally, angiogenesis is suppressed with exceptions including female reproduction, inflammation and wound healing. How do cancer cells change this?
- Angiogenic switch -> Shift in balance between angiogenic factors and anti-angiogenic factors to induce formation of new vessels by recruiting progenitor cells, pericytes and smooth muscle cells
Cancer cells > ____________ from the blood vessel become hypoxic and start to release ______________ factors.
- 2 mm
- Proangiogenic
What is the Hayflick limit?
- Normal genetic programming limits the number of times a cell is able to replicate -> When reached, replicative senescence
How do tumors develop limitless replicative potential?
- Activating telomerase activity and continued maintenance of telomeres
Most cancer related deaths are due to the primary tumor or metastasis?
- Metastasis
How does metastasis occur?
- Metastasis occurs via lymphatic vessels and/or blood vessels and is generally an inefficient process, though it is made more efficient when the cancer is of cells which already have the capability to move between tissues and blood/lymphatics (i.e., lymphoma)
What is lymphoma?
- Diverse group of malignancies with origin in lymphoreticular cells arising in lymphoid organs (lymph nodes, spleen, tonsils)
What is the typical signalment of canine patients which develop lymphoma?
- Large to giant breed dogs (Golden Retrievers, Boxers, Basset hounds, Rotties, Mastiffs, St. Bernard, Bulldogs, Airedales) with a median age of 6-9 YO

What are various ways to classify lymphoma?
- Histologic grade (low, mid, high) and histologic subtypes (~25 subtypes of canine lymphoma)
- Immunophenotype (B cell vs. T cell lymphocyte origin)
- Anatomic site
B cell lymphomas make up about ___________% of canine lymphoma while T cell lymphomas make up about _______________% of canine lymphoma.
- 70
- 30
At which anatomic sites does canine lymphoma commonly occur?
- Multicentric (multiple lymph nodes) = 80-84% of total cases
- Gastrointestinal = 5-7%
- Mediastinal = 5%
- Cutaneous
- Hepatosplenic
- Other extranodal sites - nasal, bone, CNS, ocular, etc.

For most multicentric lymphoma patients, what signs do they present with?
- None (substage a)
Clinical symptoms are noted in approximately ______________% of canine lymphoma patients.
- 20-40
Patients with which type of lymphoma are more likely to be substage b?
- High grade, T cell lymphoma
For those patients with multicentric canine lymphoma that do present with clinical signs, what signs are common?
- Lymphadenopathy primary sign
- Hepatosplenomegaly
- Weight loss, anorexia, fever, etc.
- PUPD (can be associated with hypercalcemia)
What are some DDx for lymphadenopathy?
- Immune-mediated disorders
- Disseminated infection (bacteria, viral, rickettsial, fungal)
- Other forms of neoplasia
What are some clinical signs associated with GIT lymphoma?
- V/D
- Malabsorption
- Weight loss
- ER signs: Perforation/obstruction
What are some clinical signs associated with mediastinal lymphoma in dogs?
- Respiratory signs: Cough, Dyspnea, Pleural fluid
- Regurgitation
- Pre-caval syndrome (Compression of the cranial vena cava -> Reduced venous return) -> pitting edema of head, neck, forelims
- Will look edematous
- Hypercalcemia
- PUPD

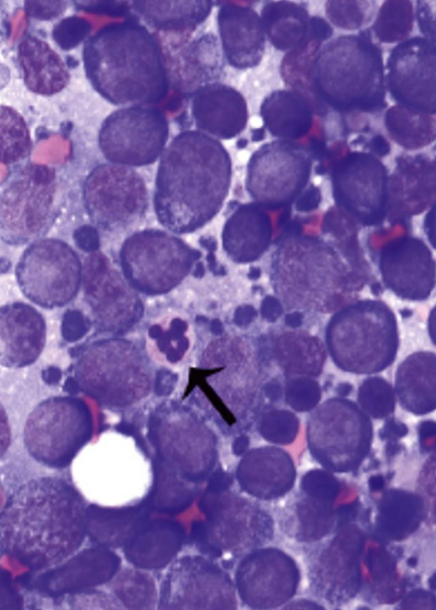
What are options for LN sampling and the testing which can be done with the samples?
- FNA -> Cytology, flow cytometry, PARR
- Biopsy -> Histopath, grading, sub-classification
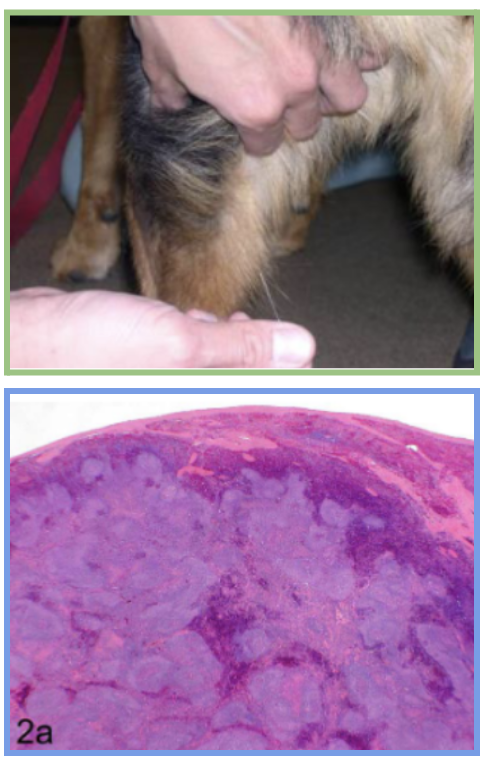
If possible, avoid sampling the _________________ lymph node. Why?
- Mandibular
- Drains oral cavity; may represent inflammatory/reactive lymph node vs. lymphoma
What are some lymphoma-associated paraneoplastic syndromes?
- Anemia (most common in dogs/cats; Mild and non-regenerative)
- Fever
- Thrombocytopenia
- Hypercalcemia (15% of patients (30-40% of patients with mediastinal); More common with T cell)
- Monoclonal gammopathy (More common with B cell)
- Cachexia
What diagnostics are useful for staging of lymphoma?
- CBC/Chem/UA
- +/- thoracic rads, AUS, bone marrow aspirate
_____________ of lymphoma patients are stage ___________________.
- 80%
- 3 and 4
Describe the stages of lymphoma.
1) Involvement limited to a single node or lymphoid tissue in a single organ
2) Involvement of many lymph nodes in a regional area (+/- tonsils)
3) Generalized lymph node involvement
4) Liver and/or spleen involvement (+/- stage III)
5) Manifestation in the blood and involvement of bone marrow and/or other organ systems (+/- stage 1-4)
Each stage can be subclassified into:
- a. Without systemic signs
- b. With systemic signs
What are treatment options for canine lymphoma?
- Prednisone alone (MST 60 days)
- Chemotherapy
- Surgery (consider with obstructive or solitary lesions)
- Radiation (local treatment vs. whole body)
- Bone marrow transplant
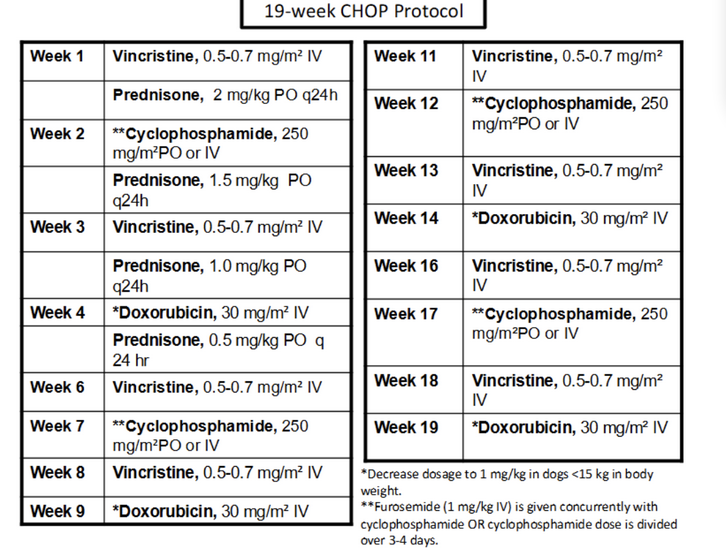
What is the "best" treatment for lymphoma? It induces remission in _______________% of patients with MSTs of _________________.
- CHOP-based Chemotherapy
- 80-95%
- 10 - 14 months
What drugs are used in the CHOP protocol?
- C = cyclophosphamide
- H = doxorubicin (hydroxydaunorubicin)
- O = vincristine (Oncovin)
- P = prednisone
What are some additional options for chemotherapy for lymphoma?
- Doxorubicin (Adramycin); 60-85% ORR
- Rabacfosadine (Tanovea); 55-75% ORR
- Rabacfosadine + doxorubicin combination; 85% ORR

What is the MST of high-grade lymphoma treated with doxorubicin only? Rabacfosadine only? Rabacfosadine + Doxorubicin combo?
Doxorubicin - 6-9 month MST, 4-5 month median remission
Rabacfosadine (Tanovea) - 3-6 month median remission, B- cell disease significantly improved response
Rabacfosadine + Doxorubicin combo - 6.5 month median progression free survival
What can be considered for rescue chemotherapy for canine lymphoma?
- If patient successfully finished CHOP protocol initially, consider re-induction of CHOP protocol
- Know cumulative dose of doxorubicin and do not go over!
Is chemotherapy/treatment needed for low grade/indolent lymphoma (i.e., T zone lymphoma, follicular lymphoma)?
- Not yet; Start with monitoring only
- When it is time for treatment (i.e. lymphocytosis becomes more moderate to severe), can utilize less aggressive options (Prednisone and Chlorambucil)
For palliative care, Prednisone used at immunosuppressive doses can kill lymphoma cells, resulting in a _______________ ORR and MST of ______________.
- 50%
- 60 days

What are some prognostic factors associated with lymphoma?
- Histologic Grade
- Histologic Subtype
- Stage of Disease (WHO)
- Substage
- Anatomic Location
- Immunophenotype (within context of grade and subtype)
- Flow cytometry features
- Response to Treatment
- Chemotherapy-induced hematologic toxicity
- Prolonged steroid pretreatment
True or false: Lymphoma is very sensitive to radiation
- True
Hematopoietic tumors accounts for _______ of all feline tumors.
- 1/3
Prior to the development of FeLV vaccines, what was the most common presentation of cats with lymphoma?
- Younger cats (4-6 years old) which were 70% FeLV positive and most commonly had mediastinal, multicentric and spinal lymphoma
After the development of FeLV vaccines, what is the most common presentation of cats with lymphoma?
- Older cats (10 YO) which are 25% FeLV positive and most commonly have GI lymphoma
Describe how FeLV is related to tumor-genesis.
- They have a direct role in tumor-genesis and are associated with lymphoma, leukemia, and anemia
- T-cell lymphoma being more common
Describe how FIV is related to tumor-genesis.
- They have an indirect role based on immunosuppressive effects of FIV with B-cell lymphoma developing more commonly in FIV-positive cats.
FIV positive cats have a ________ increased risk of lymphoma.
- 5x
What are some other factors (aside from retroviral status) which can predispose a cat to lymphoma?
- Tobacco smoke exposure (increases risk 2.4x with duration and quantity of exposure)
- Immunosuppression (I.e. increases risk 6x renal transplant cases with long term cyclosporine administration)