ENT: Inner Ear
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
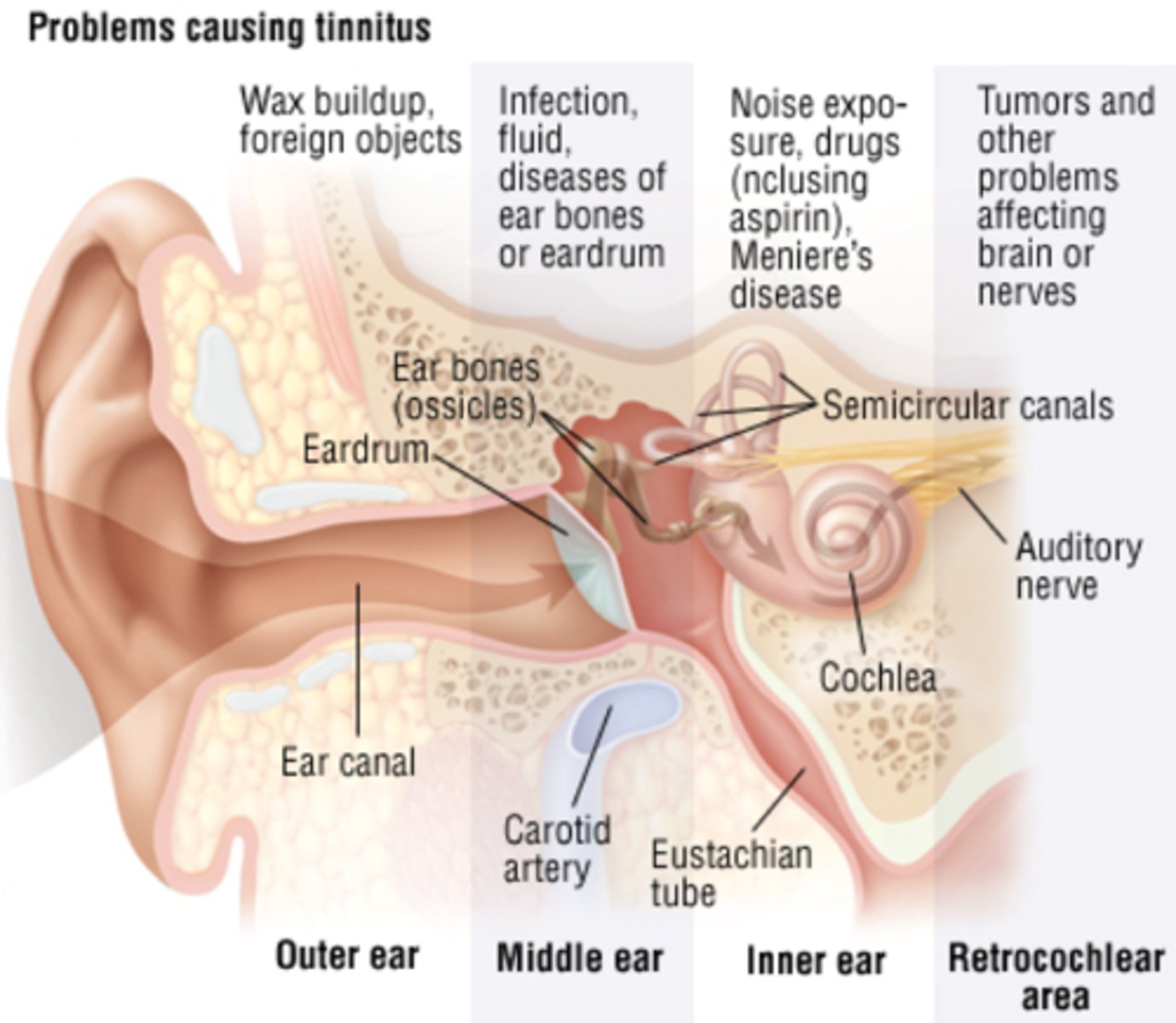
Tinnitus
Perception of non verbal sound in ears without a stimulus
Note that this is a SYMPTOM
The sound could be (whistling, hissing, buzzing, ringing, pulsating)
It can be unilateral or bilateral, acute or chronic, and intermittent or constant.
Frequently is associated with hearing loss and presbyacusis
Tinnitus is more common in which patients?
Men
Smokers
Objective vs subjective tinnitus
Objective tinnitus: tinnitus that can perceived by others, which is due to sounds created by the body (e.g., carotid artery stenosis, stapedial myoclonus). You would be able to auscultate this on a stethoscope
Subjective tinnitus: tinnitus that is only perceived by the affected individual, which can be due to a wide range of etiologies (e.g., otosclerosis, tumor, infections)
Outline the VASCULAR causes of tinnitus
- carotid artery stenosis
- carotid artery dissection
- gloms jugglers tumours, pulsatile tinnitus
Ototoxic drugs
Aspirin
Loop diuretics
Aminoglycosides
Chemotherapy e.g. cisplatin
Antimalarial drugs e.g. quinine
Tetracyclines
Slidenafil
ALACATS
Outline the otological, conductive causes of tinnitus
Cerumen impaction, otosclerosis, otitis media, infection, fluid
This mostly affects the middle ear and external ear
Outline the otological, sensorineural causes of tinnitus
This usually affects the inner ear and includes DRUGS, NOISE EXPOSURE, MENIERES DISEASE
Also presbyacusis
Metabolic causes of tinnitus
Hyperthyroid
Zinc
What tumour can cause tinnitus?
Acoustic neuroma
Neurological condition which can cause tinnitus
Multiple sclerosis
MSK causes of tinnitus
STAPEDIUS MYOCLONUS - objective tinnitus
TMJ joint dysfunction
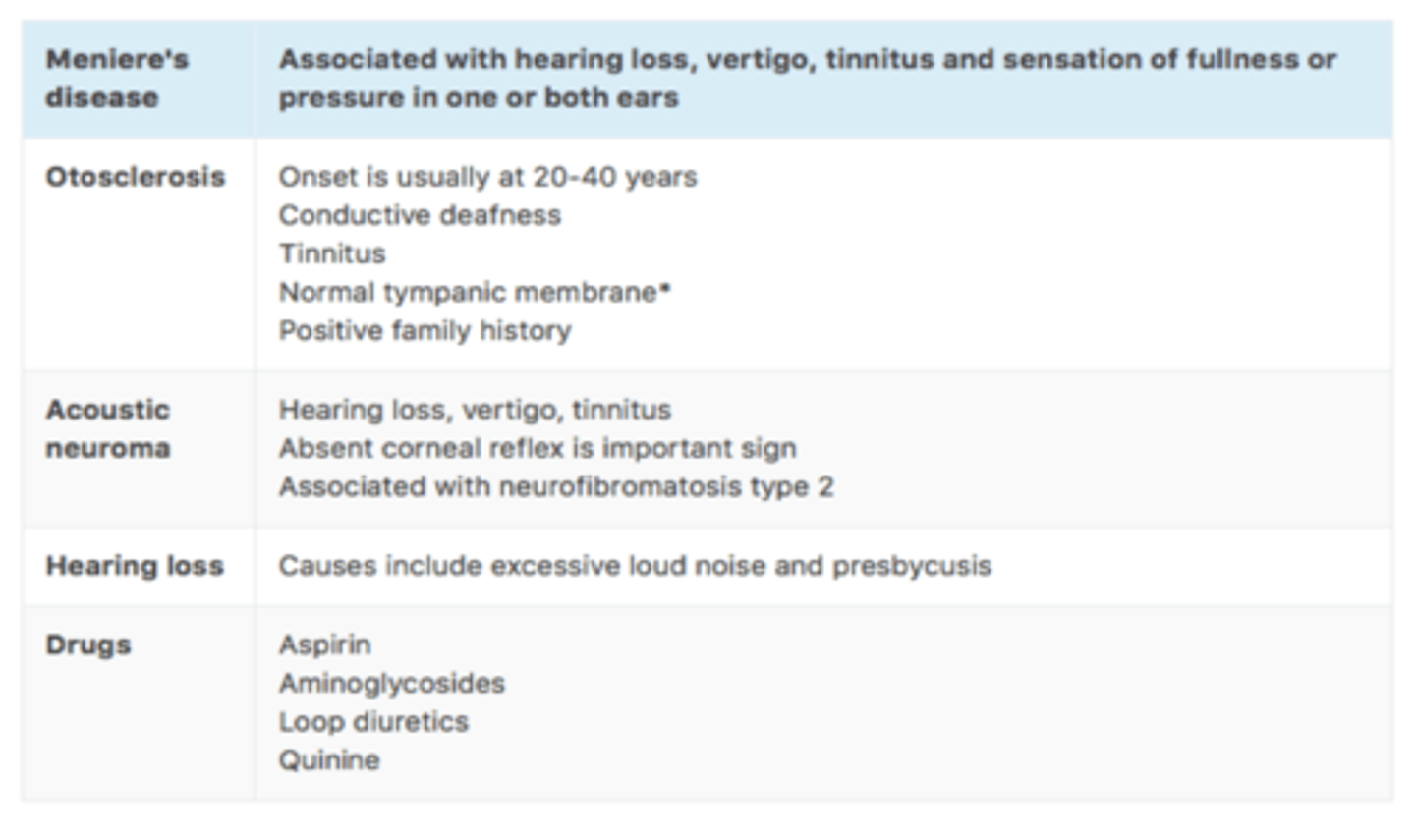
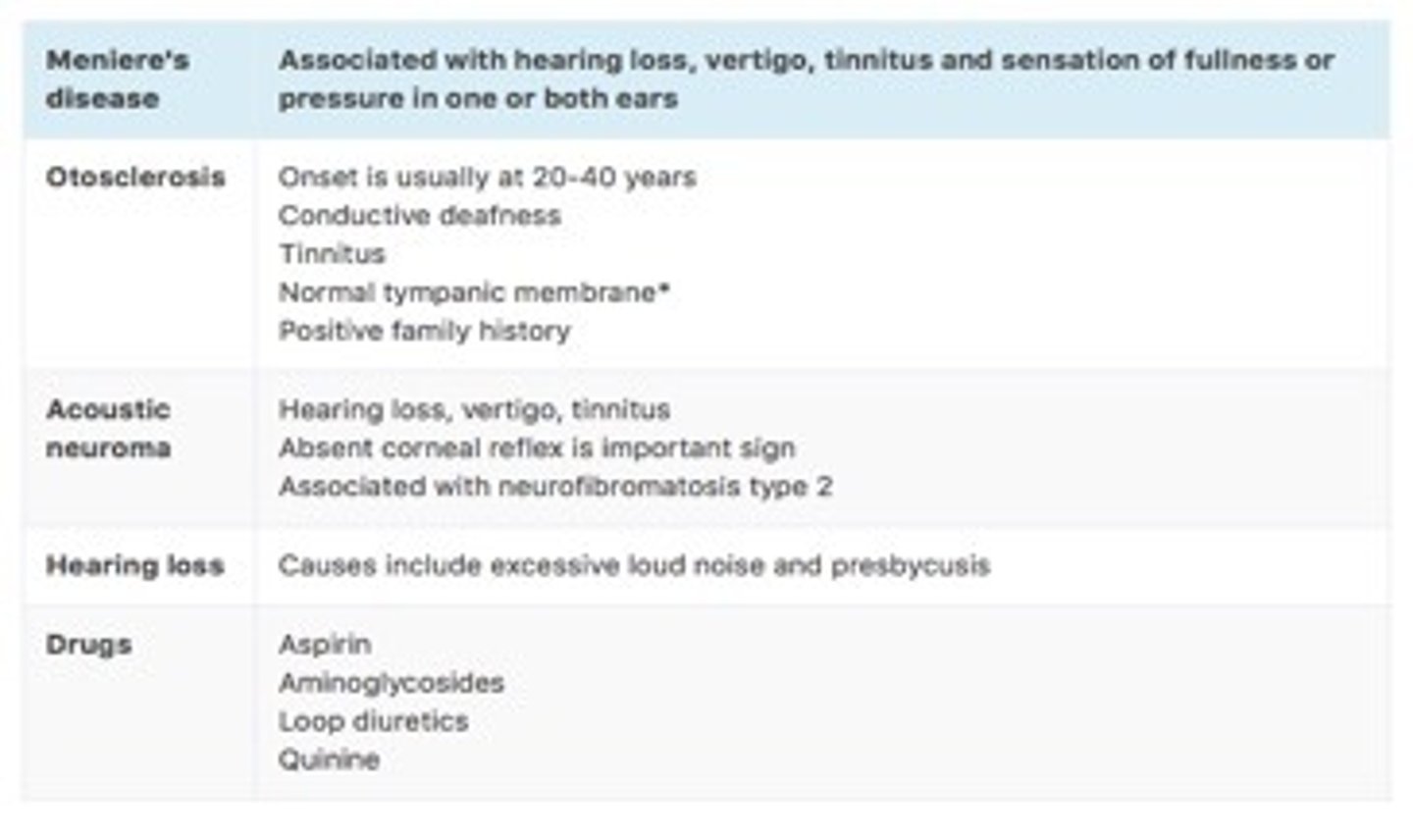
Outline the most common, important causes of tinnitus
MOHAD
M - menieres disease
O - otosclerosis
H - hearing loss, chronic noise exposure, presbyacusis
A - acoustic neuroma
D - drugs: ALACATS
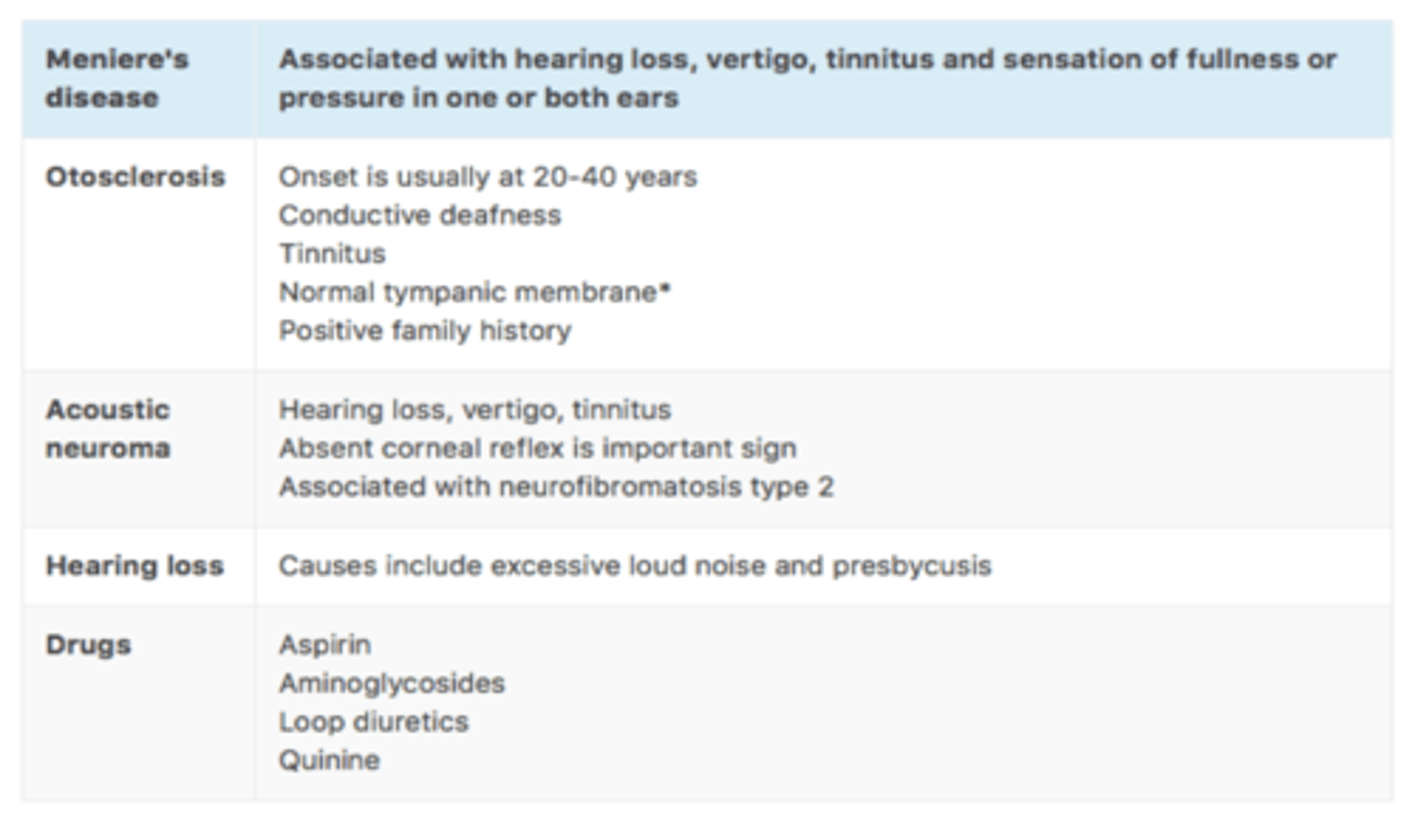
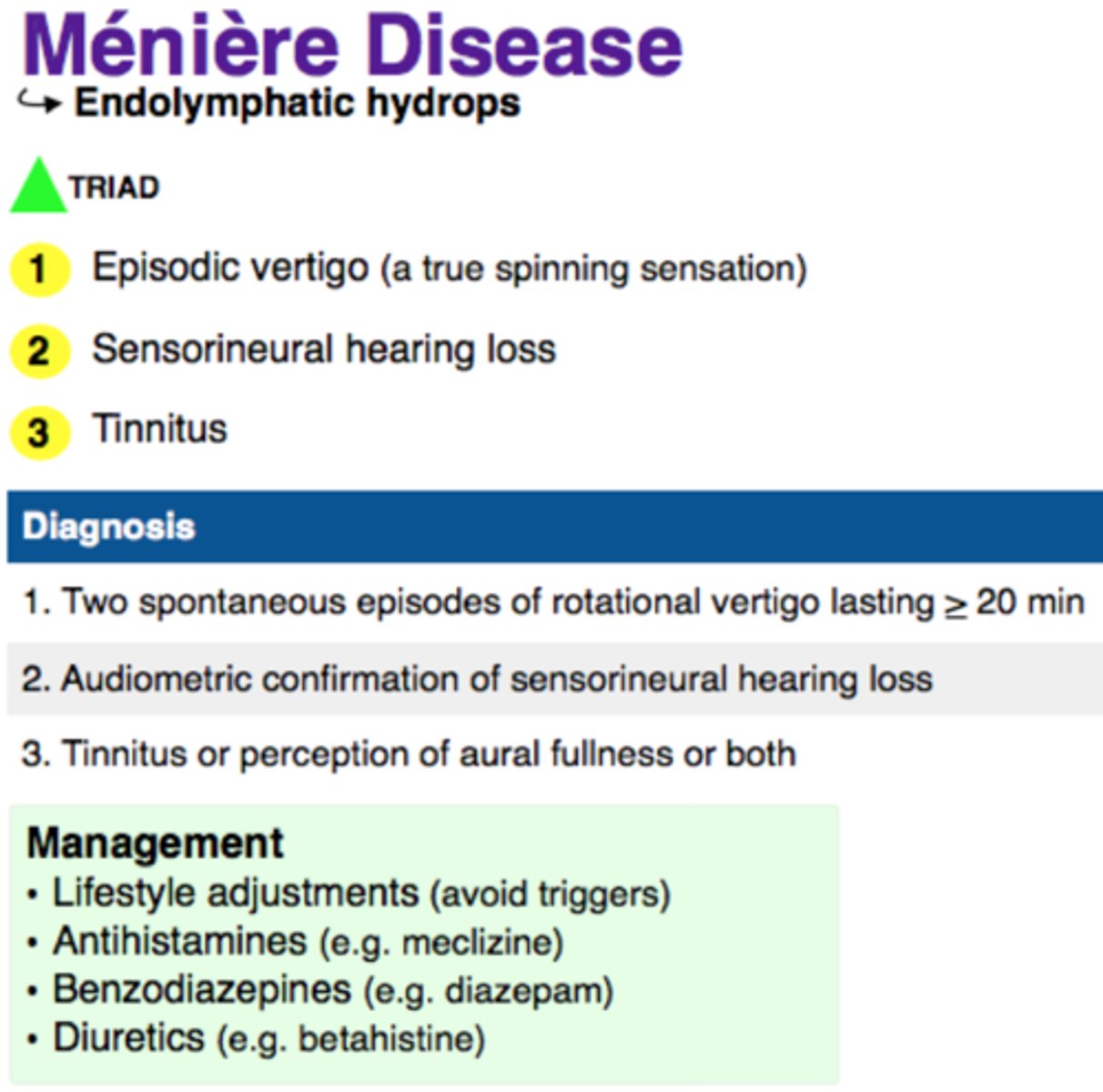
Meniere's disease
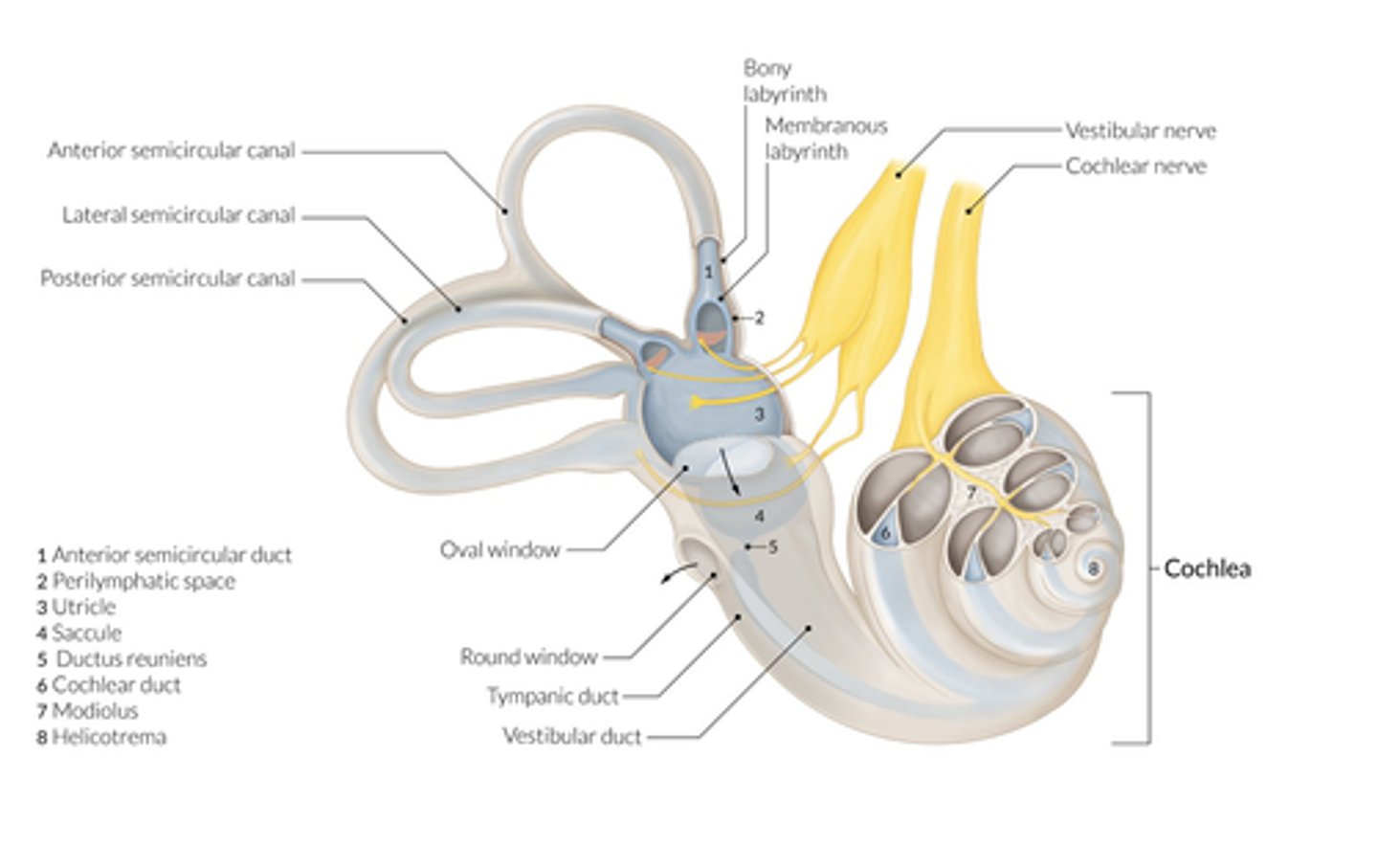
Idiopathic condition affecting the inner ear, in which impaired resorption of endolymphatic fluid causes it to accumulate in the membranous labyrinth (endolymphatic hydrops)
This leads to excessive pressure and dilation of the endolymphatic system
More common in females
Peak incidence: 40–60 years
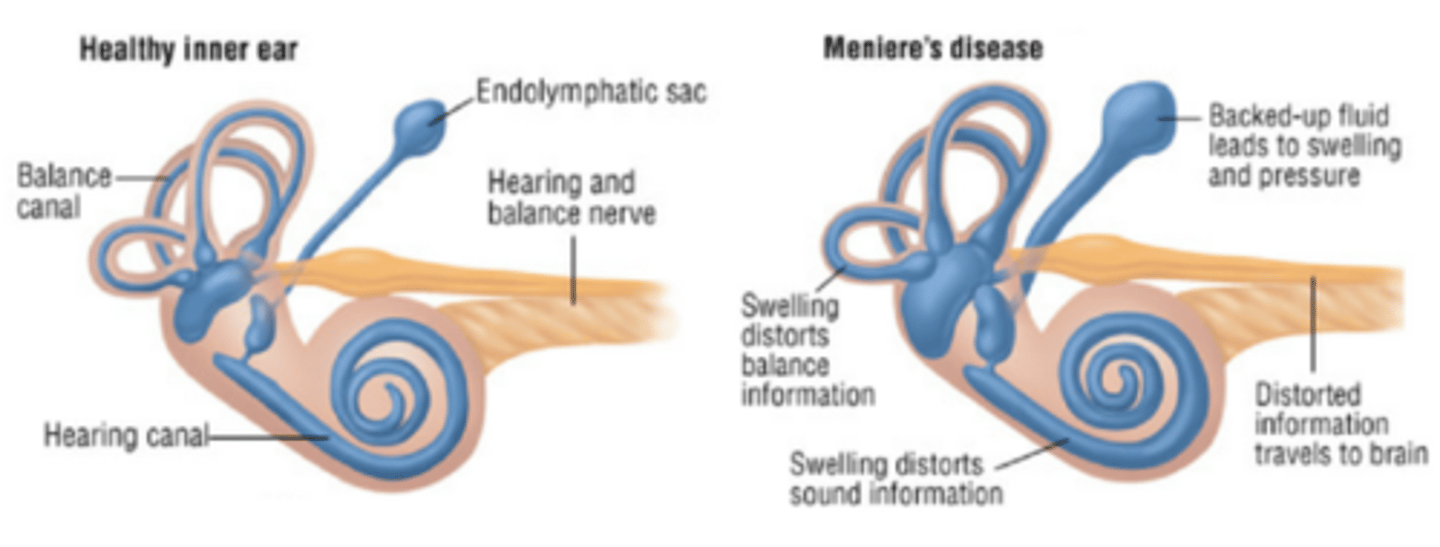
Triad of symptoms in Menieres disease
Tinnitus
Vertigo
Sensorineural hearing loss - fluctuating, low-frequency loss increases with each episode that may lead to deafness after several years.
KEY SYMPTOM: AURAL FULLNESS
Also nausea and committing, HORIZONTAL NYSTAGMUS
Positive Romberg test
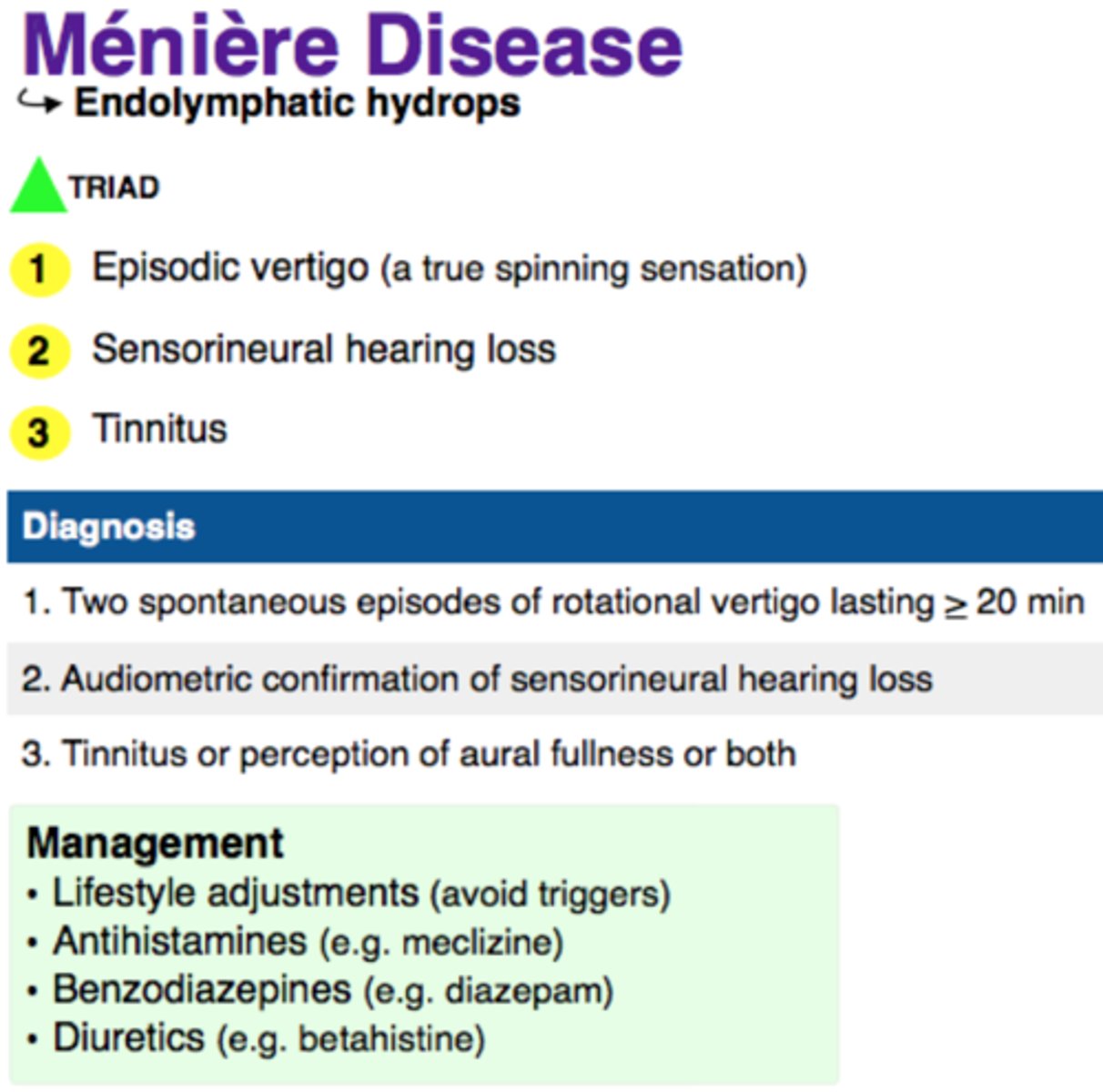
Describe the pattern of symptoms associated with meniere disease
Episodes are acute and recurrent
Acute attacks typically last minutes-hours, often 2-3 hours.
Acute episodes may occur in clusters of about 6-11 per year.
Remission of symptoms may last several months.
Most begin unilaterally and then develop into a bilateral pattern
Describe the nystagmus that is associated with menieres disease
The pattern of nystagmus in Ménière disease typically reverses during the course of an attack.
An initial brief period of irritative nystagmus towards the affected ear is usually followed by a period (20–30 minutes) of nystagmus towards the healthy ear or absence of nystagmus, which is then followed by a longer period (hours to days) of irritative nystagmus towards the affected ear (recovery nystagmus).
Nystagmus may also be absent during clinical examination.
Name the three key features required to confirm a diagnosis of Menieres disease
Two or more episodes of vertigo that last 20 minutes to 12 hours
Low-frequency to mid-frequency sensorineural hearing loss on audiometry
Fluctuating tinnitus or ear fullness
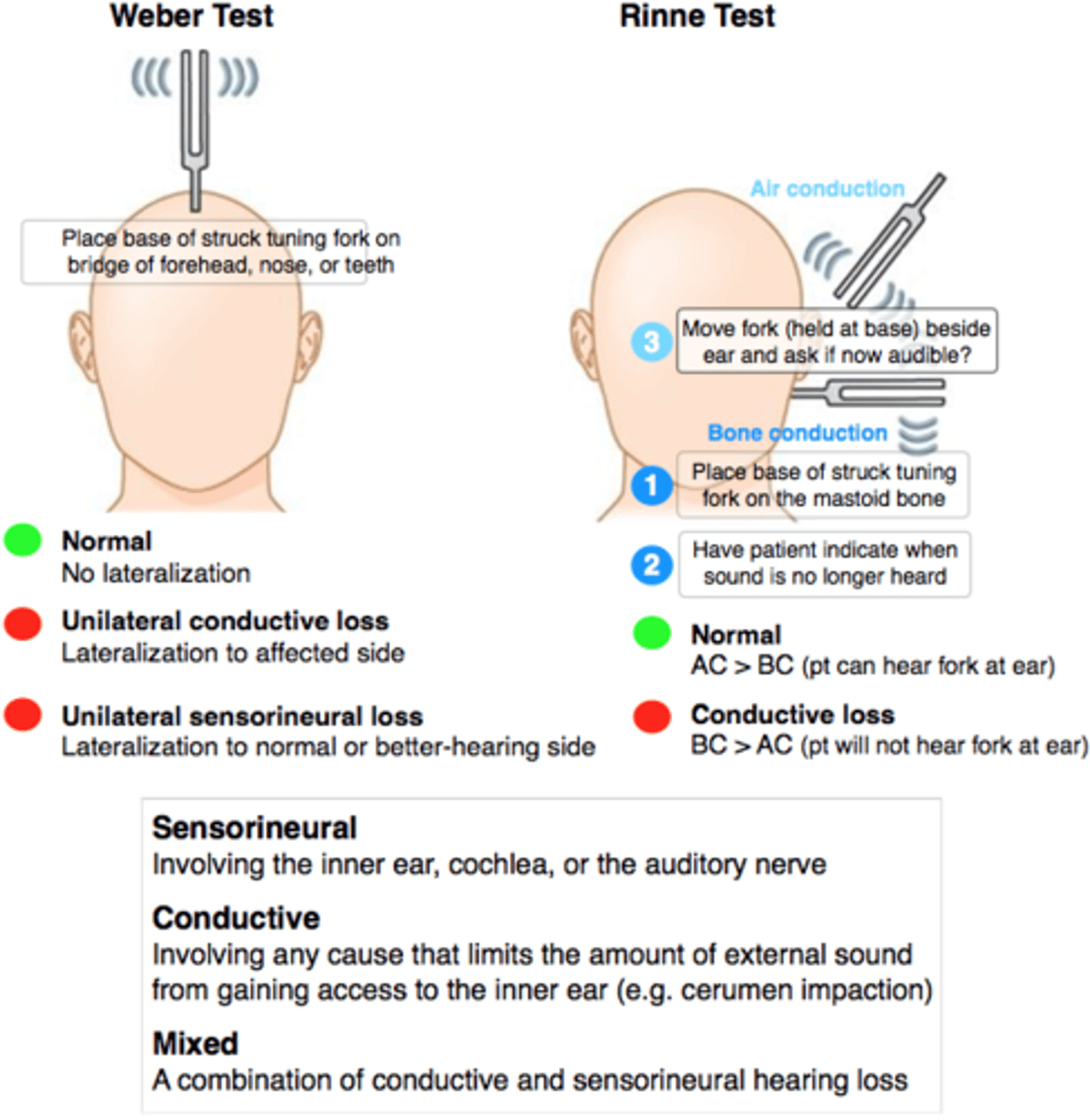
Describe the tuning fork results associated with Menieres disease
Weber test: lateralization to the healthy ear - Indicates sensorineural hearing loss in the opposite ear
Rinne test: bilaterally positive, normal conductive hearing.
DDX Meniere's disease
Other ENT causes:
Exclude acoustic neuroma in anyone with unilateral deafness, tinnitus and/or facial nerve palsy.
Otitis media.
Earwax.
Ototoxic drugs.
Intracranial pathology
Vertebrobasilar insufficiency, transient ischaemic attack (TIA), stroke, thrombosis of labyrinthine artery.
Intracranial tumours.
Migraine.
Systemic illness:
Anaemia
Hypothyroidism
Diabetes mellitus
Autoimmune disease
Syphilis
What blood tests would be important to perform when investigating a patient presenting with menieres disease?
Blood tests to exclude systemic illness
FBC, ESR, thyroid function, syphilis screen, fasting glucose, renal function, lipids.
Non pharmacological management of Meniere disease
- Patient must inform DVLA, - cease driving until satisfactory control can be achieved
- Avoid dietary and environmental triggers (caffeine, alcohol, smoking and stress).
- Low-sodium diet
- Vestibular rehabilitation therapy in patients with persistent disequilibrium symptoms between attacks, the programmes involve exercises such as learning to bring on the symptoms to 'desensitise' the vestibular system; learning to improve balance, co-ordination and coping skills.
- Hearing aids may be needed
- Safety - if prone to sudden vertigo, consider safety and risks with activities involving heights, dangerous machinery, swimming, etc
- Maintain mobility, After an acute attack of vertigo, patients naturally tend to sit still. Encourage them to move around to promote central compensation, where the brain uses vision and other senses to compensate for the loss of vestibular function.
Acute attack of Meniere disease management
Vertigo and nausea can be alleviated by prochlorperazine, cinnarizine, cyclizine, or VESTIBULAR SUPPRESSANT
Anti emetic: promethazine, ondansetron
Consider patient preference for both choice of drug and route of administration.
For severe symptoms, hospital admission may be needed to maintain hydration.
Drug prophylaxis for Meniere Disease
Trial of BETAHISTINE (initially 16 mg three times a day) to reduce the frequency and severity of attacks - note that this is a histamine analogue
Diuretics may be helpful but are not usually recommended for use in primary care e.g: (hydrochlorothiazide or triamterene)
NOTE: Betahistine is preferred over diuretics because diureticsrequire regular monitoring of blood pressure, kidneyfunction, and electrolytes.
What interventional/surgical treatment options are there for Meniere disease?
Intratympanic gentamicin injection: repeated application of gentamicin to the middle ear cavity through a small incision in the eardrum (paracentesis), damaging action of gentamicin on the sensorineural epithelium and labyrinthine cells to reduce vertigo, while preserving hearing (although there may be a risk of sensorineural hearing loss)
Local steroid injection - this is transtympanic or intratympanic dexamethasone injection
Sacculotomy: The endolymphatic sac and duct (part of the vestibular organ) are surgically exposed in order to promote drainage of endolymph, decompression of the endolymphatic sac and sigmoid sinus.
Vestibular neurectomy: Surgical lysis of the vestibular bundle entering the internal auditory canal. In some cases, the procedure is associated with hearing loss
Labyrinthectomy - this is a last option, as hearing in that ear would also be lost.
Prognosis of Meniere disease
There is no cure but most patients can be helped by the above treatments.
The Ménière's Society suggests that 80% of patients will have their symptoms alleviated by non-invasive treatments.
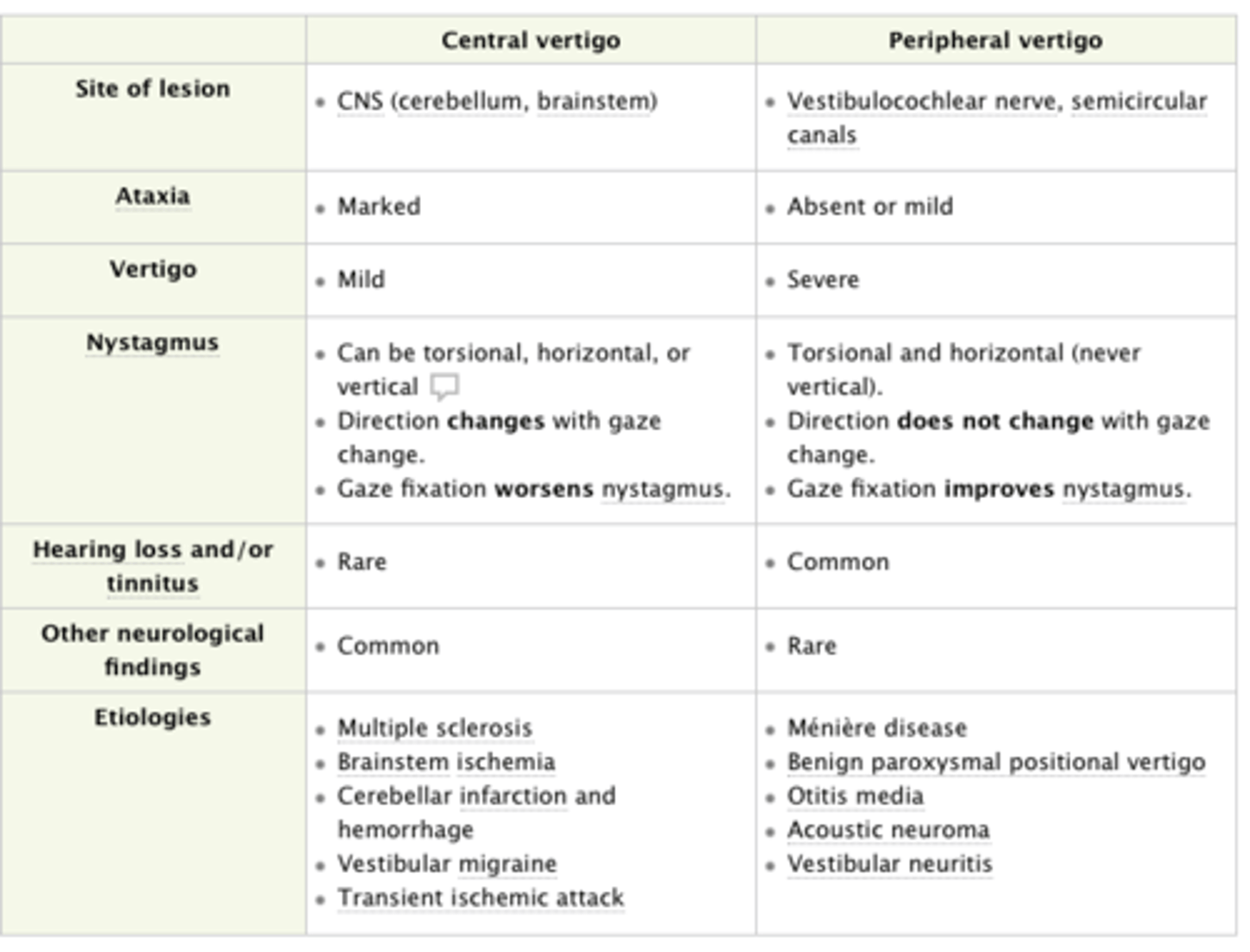
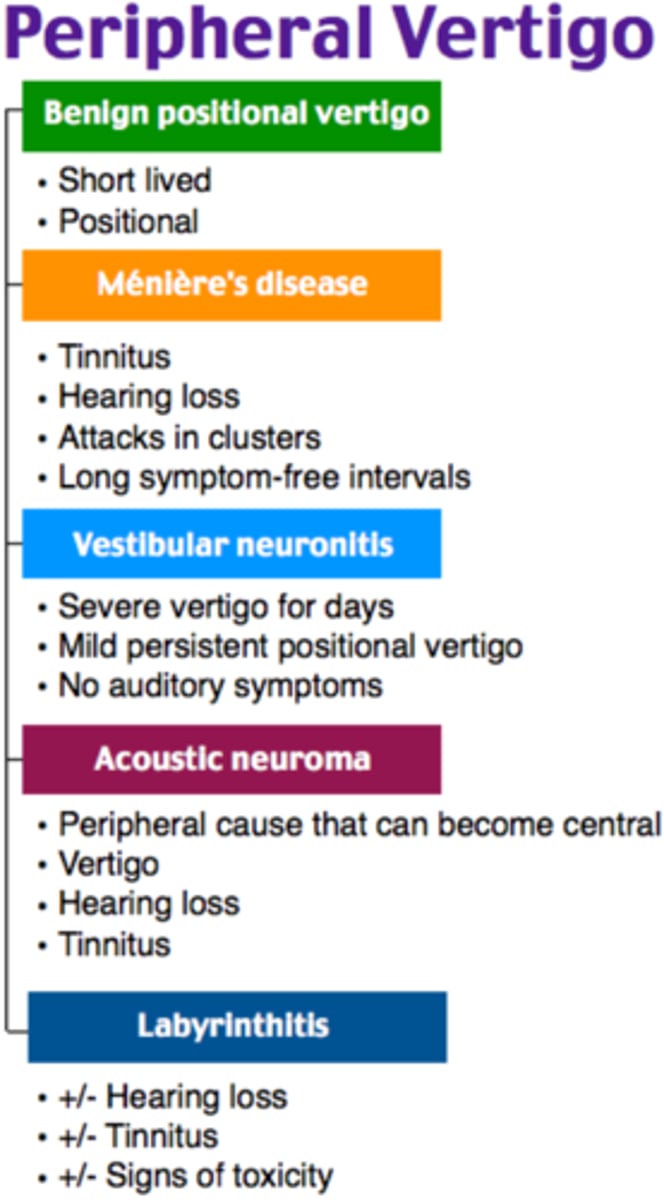
Vertigo
False sensation that you or environment is moving
Mismatch between the vestibular system as well as other sensory inputs such as vision and proprioception
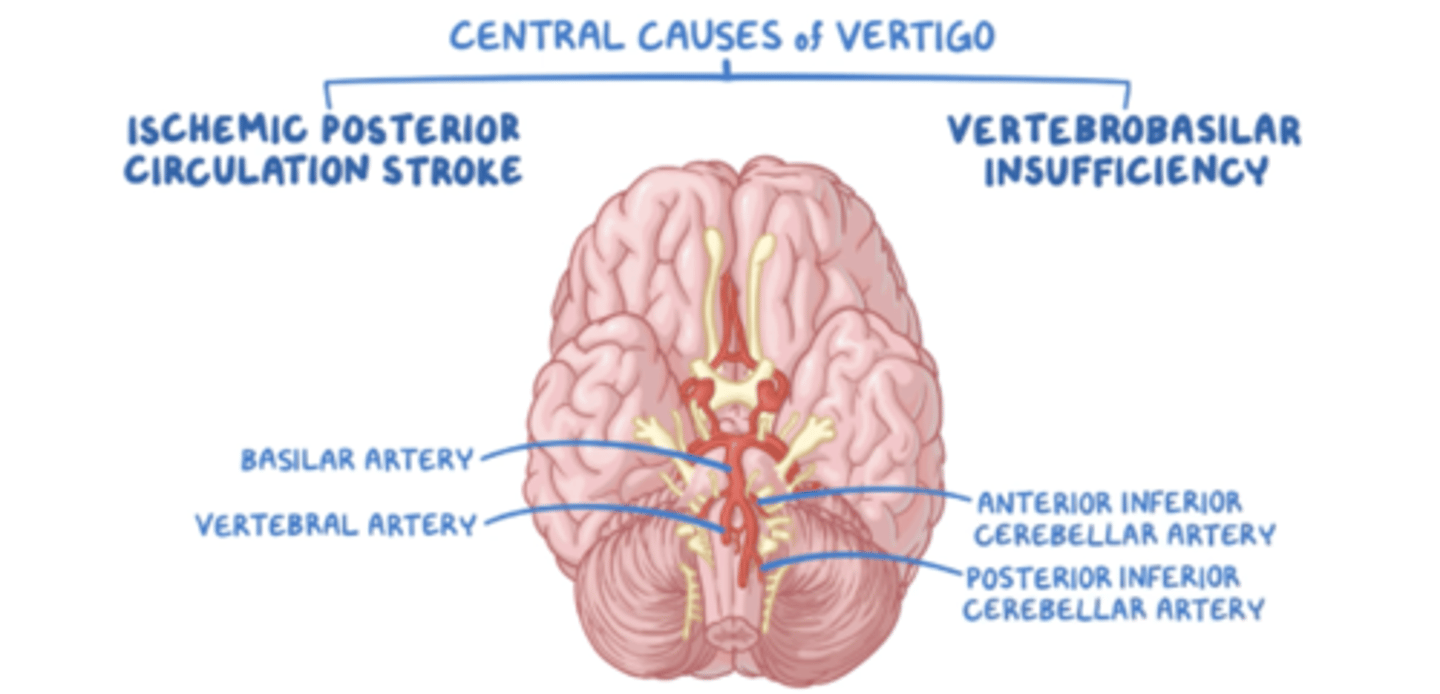
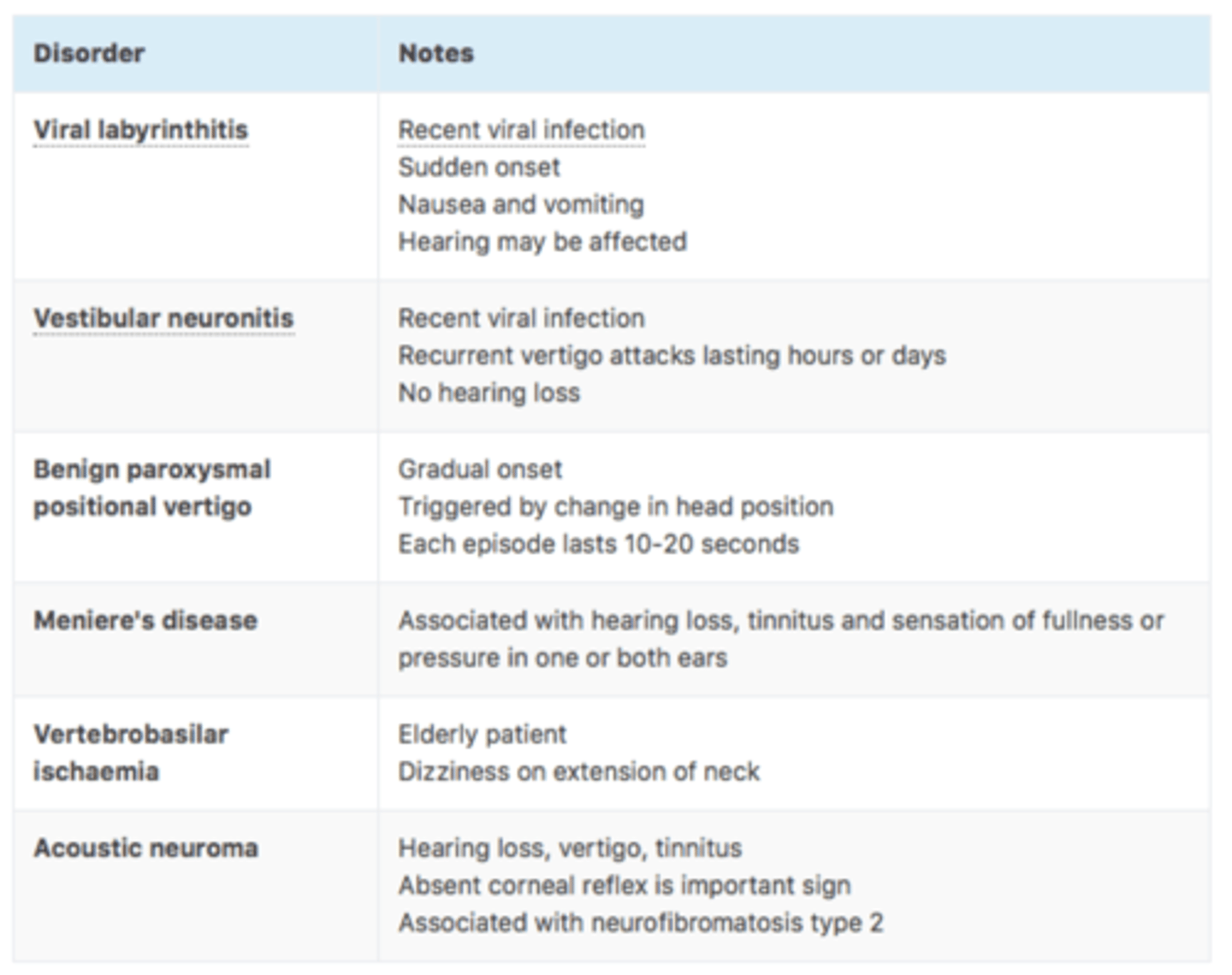
Central causes of vertigo
Due to damage of the vestibular structures in the brainstem or cerebellum
- Infection
- Vertebral basilar artery insufficiency
- Subclavian steal syndrome
- Cerebellar hemorrhage or infarction
- Vertebral basilar migraine
- Post-traumatic injury
- Post-concussive syndrome
- Temporal lobe epilepsy
- Brainstem tumour eg pilocystic astrocytoma which can compress on vestibular structures of brainstem
- Multiple sclerosis
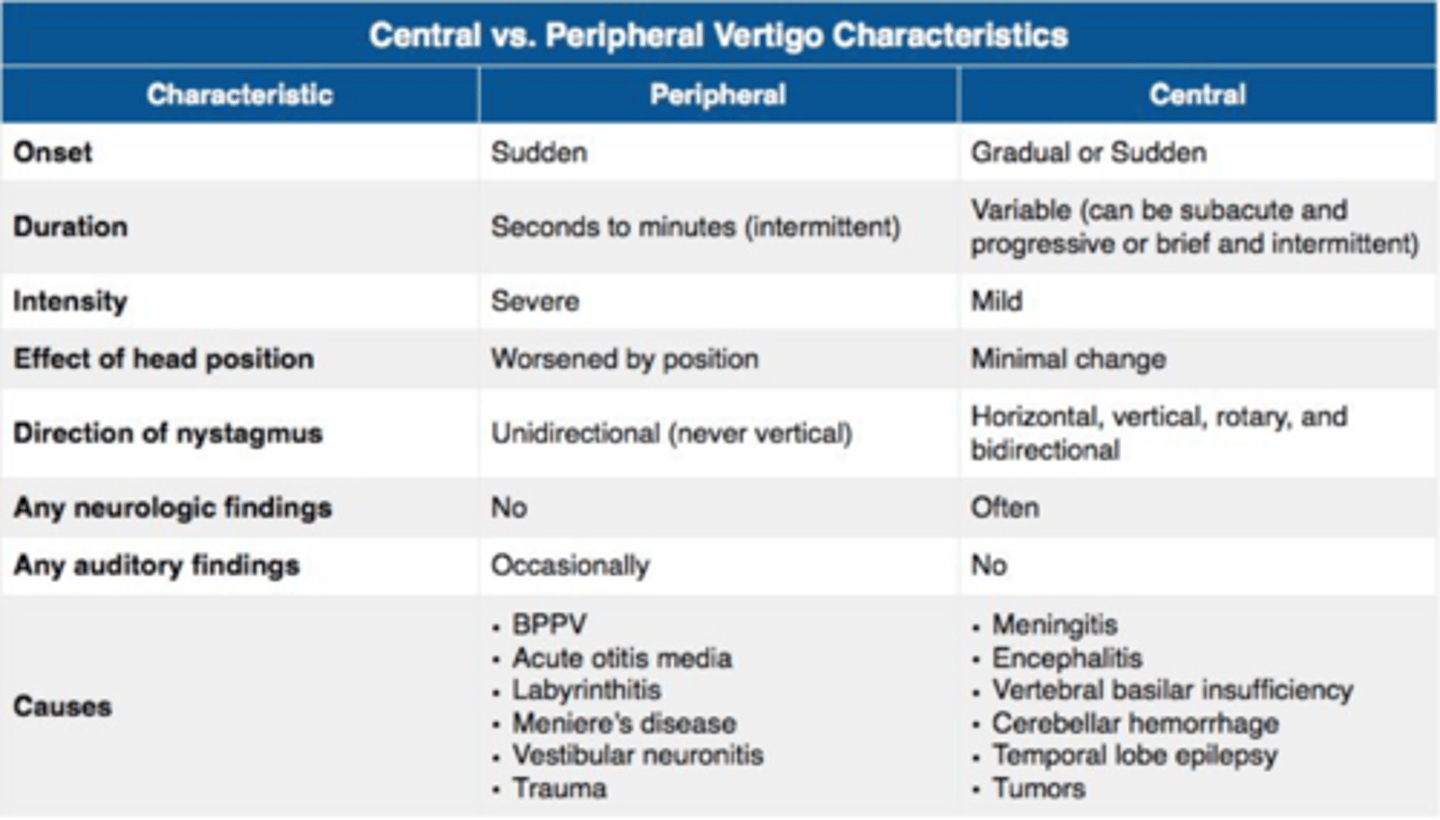
Peripheral causes of vertigo
This is due to damage of the vestibular apparatus/vestibular nerve
Benign paroxysmal positional vertigo (BPPV)
Meniere's disease
Labyrinthitis
Vestibular migraine
Choleasteatoma
What symptoms help indicate that vertigo is being caused by a central pathology?
The 4 Ds - DILPOLPIA, DYSPHAGIA, DYSARTHRIA or DYSMETRIA INDICATES CENTRAL VERTIGO
Loss of consciousness
Constant, unremitting
Vertical nystagmus
Cerebrovascular disease
Neurological symptoms eg hemiparesis, numbness, dysphagia, ataxia
Note that central causes of vertigo should be considered in any ELDERLY PATIENT WITH NEW ONSET OF ACUTE VERTIGO WITH NO OBVIOSU CAUSE
If there is vertigo with neurological signs, do MRI as this is sensitive for stroke
HINTS exam
Test which helps differentiate central vertigo from peripheral
If 1 of 3 parts of the exam are present than it indicates a central cause an a BRAIN MRI should be done to identify a posterior circulation stroke
- Head impulse test
- Nystagmus
- Test of skew
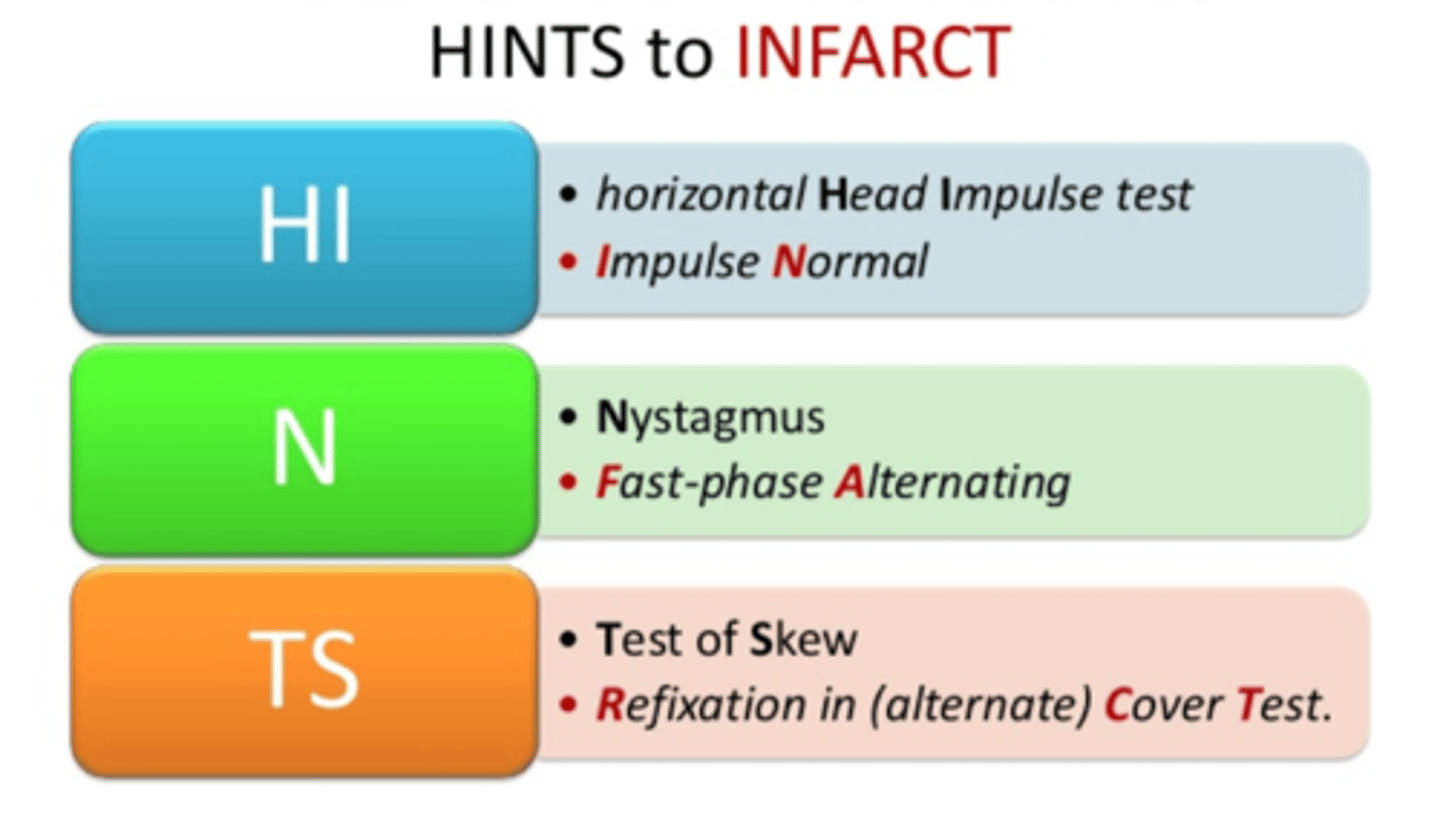
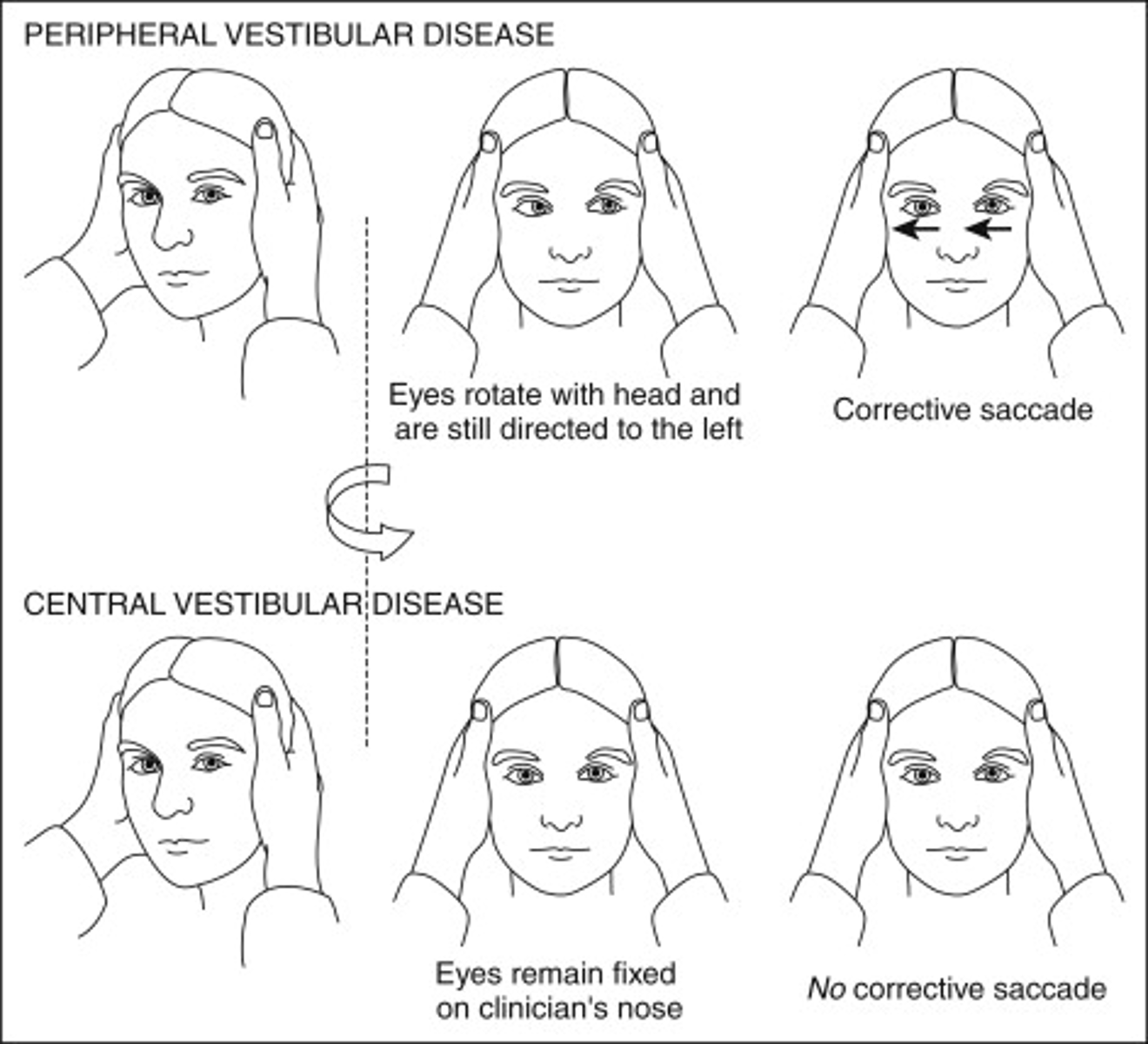
Head Impulse Test (HIT)
· Head impulse test, is there a lag time between when eyes remain fixed on your nose? A positive test indicates a peripheral cause of vertigo, normal, negative test indicates central cause eg stroke
· Tests vestibulo ocular reflex, checking if the nerve has been affected so if it is normal it means the nerve isn't affected, more indicative of a central cause of vertigo
Can peripheral vertigo cause vertical nystagmus?
No - BIDIRECTIONAL NYSTAGMUS IS HIGHLY SPECIFIC FOR A CENTRAL CAUSE OF VERTIGO & STROKE
Benign postional paroxysmal vertigo (BPPV)
VERTIGO LASTS SECONDS TO MINUTES
The presence of debris in the semicircular canals of the ears causes vertigo upon head movement.
BPPV is caused by semicircular canal dysfunction.
Dislodged particles (otoliths) disrupt the endolymph → stimulation of the hair cells on cupulas → signal sent to the brain through the vestibulocochlear nerve that is disproportional to current positioning and movement → severe vertigo attacks lasting several seconds
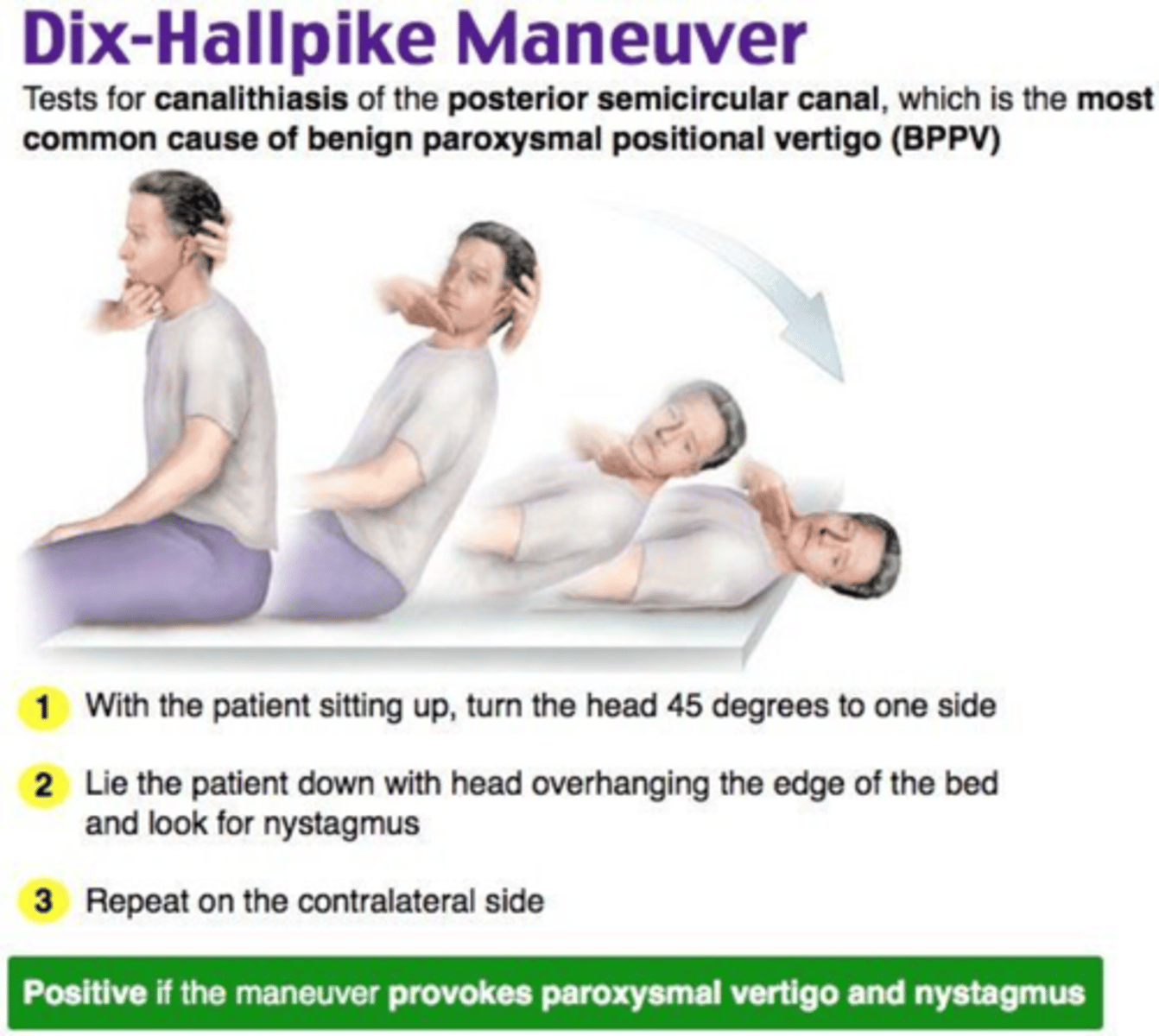
Features of BPPV
vertigo triggered by change in head position (e.g. rolling over in bed or gazing upwards)
nystagmus towards the affected side
may be associated with nausea
no hearing or neurological symptoms
each episode typically lasts 10-20 seconds
positive Dix-Hallpike manoeuvre
Triggers of BPPV
Rolling over in bed, lying down quickly
Quick rotation of the head, reclining, etc.
Vertigo occurs with a latency of a few seconds
Diagnostic test for BPPV
DIX HALLPIKE MAOUVRE
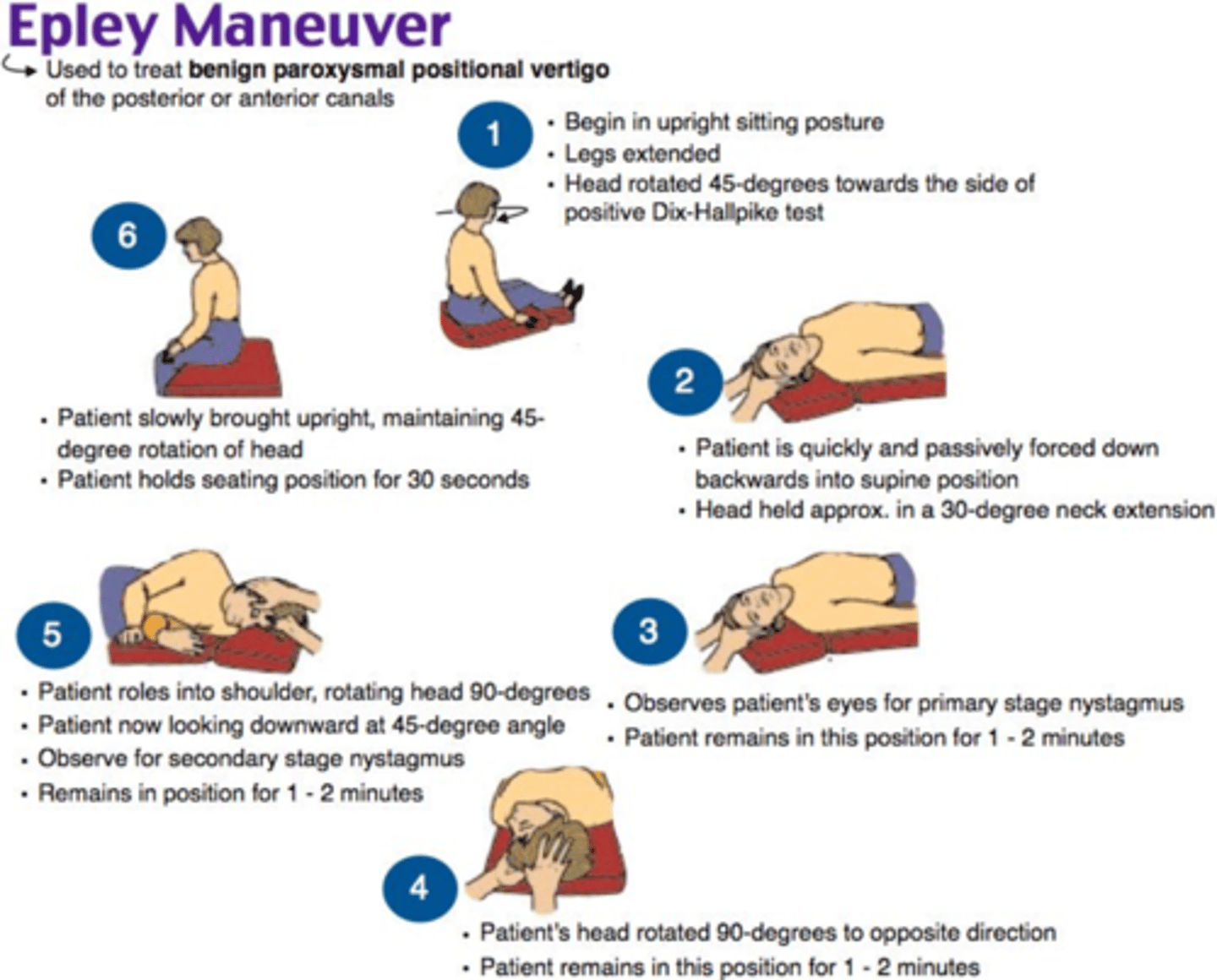
Management of BPPV
Usually resolves spontaneously within a few weeks or months
Epley manoeuvre (successful in around 80% of cases)
Teaching the patient exercises they can do themselves at home, termed vestibular rehabilitation, for example Brandt-Daroff exercises
Medication is often prescribed (e.g. Betahistine) but it tends to be of limited value.
Around half of people with BPPV will have a recurrence of symptoms 3–5 years after their diagnosis
NOTE: Chronic use of antivertigo drugs (e.g., dimenhydrinate) are contraindicated in BPPV because they may exacerbate unsteadiness by inhibiting central compensation!
Labrynthitis
Inflammation of inner ear canals
Can be viral, bacterial or systemic but VIRAL IS THE MOST COMMON
It is often associated with a recent viral illness or a vascular lesion, in which case it may involve other cranial nerve deficits.
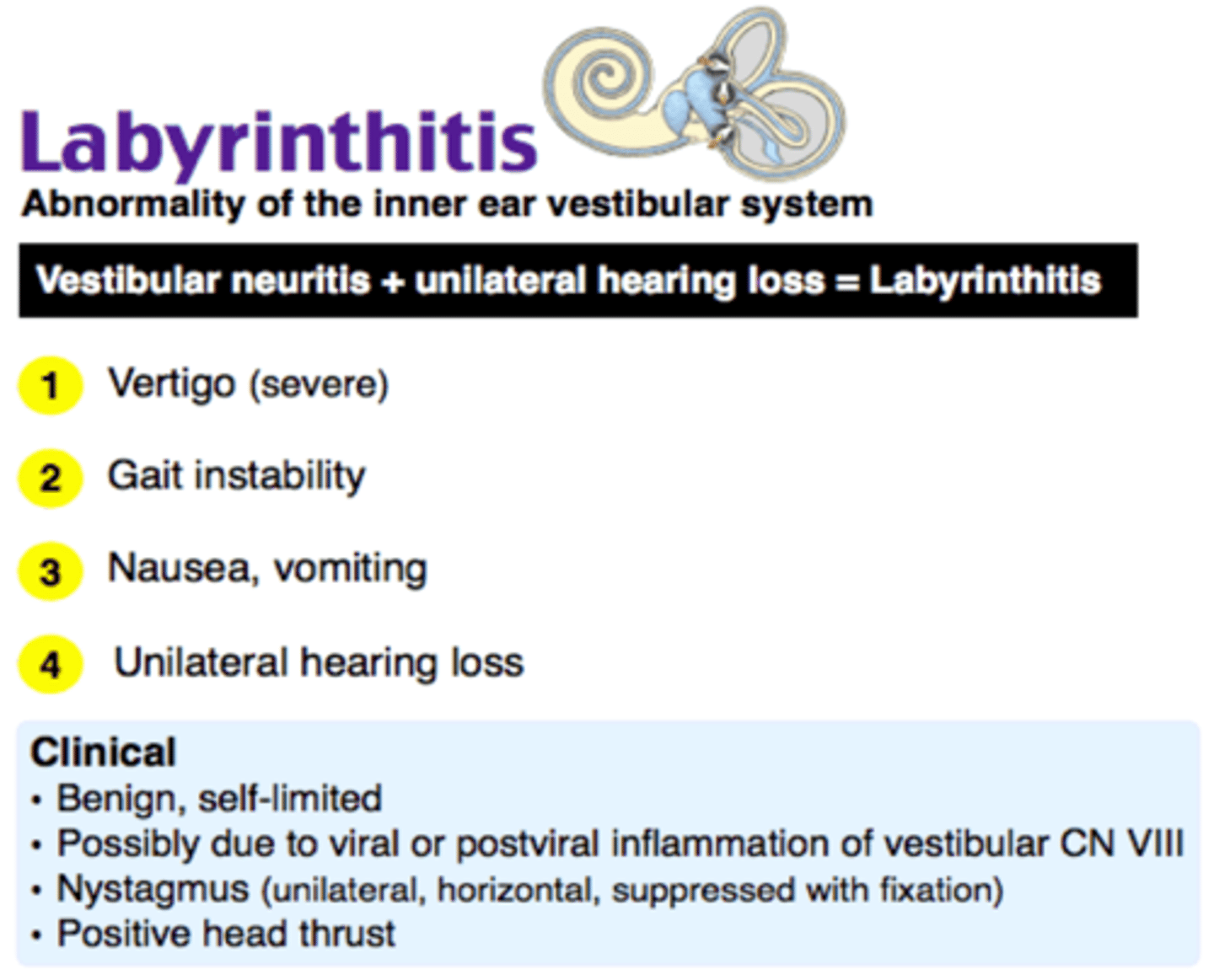
Clinical features of Labyrinthitis
- Acute onset
- Vertigo: not triggered by movement but exacerbated by movement
- N+V
- Hearing Loss
- Tinnitus
- Preceding or concurrent symptoms of upper respiratory tract infection
- Patient may fall towards affected side
- spontaneous unidirectional horizontal nystagmus towards the unaffected side
What type of hearing loss is associated with Labrynthitis ?
sensorineural hearing loss: shown by Rinne's test and Weber test
Head impulse test would reveal what in Labrynthitis?
abnormal head impulse test: signifies an impaired vestibule-ocular reflex but normal skew test (?)
What may you see in inspection of the ear canal in Labrynthitis?
abnormality on inspection of the external ear canal and the tympanic membrane e.g. vesicles in herpes simplex infection
Investigations in labrynthitis?
pure tone audiometry can be done to assess hearing loss
full blood count and blood culture: if systemic infection suspected
culture and sensitivity testing if any middle ear effusion
temporal bone CT scan: indicated if suspecting mastoiditis or cholesteatoma
MRI scan: helpful to rule out causes such as suppurative labyrinthitis or central causes of vertigo
vestibular function testing: may be helpful in difficult cases and/or determining prognosis
Treatment of Labrynthitis
It often resolves completely over a month, so treatment is conservative, although sedatives may help in severe cases.
Most common cause of labrynhtitis
VIRAL INFECTION
Vestibular Neuritis
Inflammation of the vestibular nerve which most commonly occurs after a viral infection (URTI)
Cause vertigo which can last for days
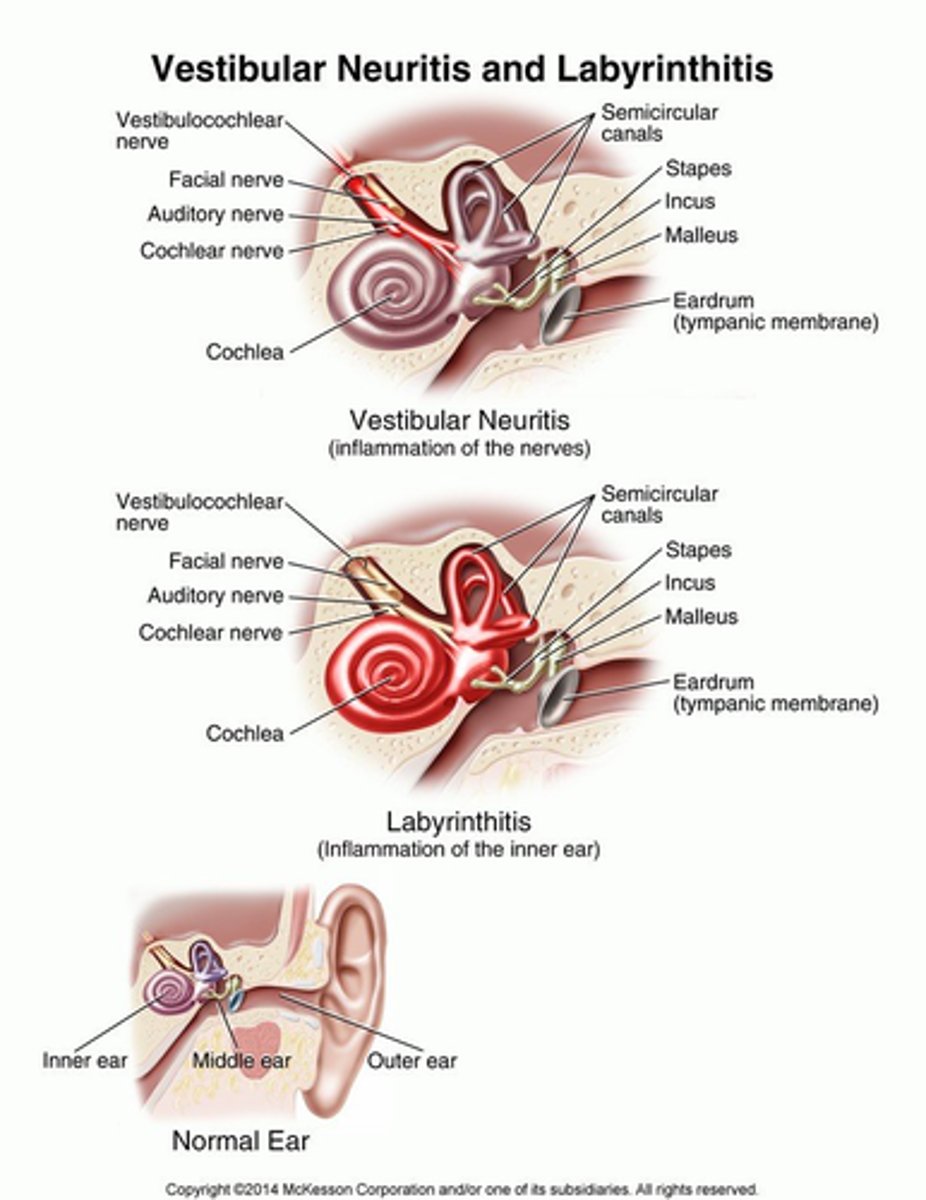
Clinical features of vestibular neuritis
recurrent vertigo attacks lasting hours or days
nausea and vomiting may be present
horizontal nystagmus is usually present
no hearing loss or tinnitus
NOTE: vestibular neuritis is used to define cases in which only the vestibular nerve is involved, hence there is no hearing impairment; Labyrinthitis is used when both the vestibular nerve and the labyrinth are involved, usually resulting in both vertigo and hearing impairment.
Investigations for vestibular neuritis
CLINICAL DIAGNOSIS
Imaging studies are indicated in patients older than 60 years, as well as those with persistent vestibular symptoms, headache, vascular risk factors, or focal neurologic symptoms to rule out a lateral medullary/cerebellar stroke - these include MRI, MRA, CT
Management of vestibular neuritis
Vestibular rehabilitation exercises are the preferred treatment for patients who experience chronic symptoms
Buccal or intramuscular prochlorperazine is often used to provide rapid relief for severe cases
A short oral course of prochlorperazine, or an antihistamine (cinnarizine, cyclizine, or promethazine) may be used to alleviate less severe cases
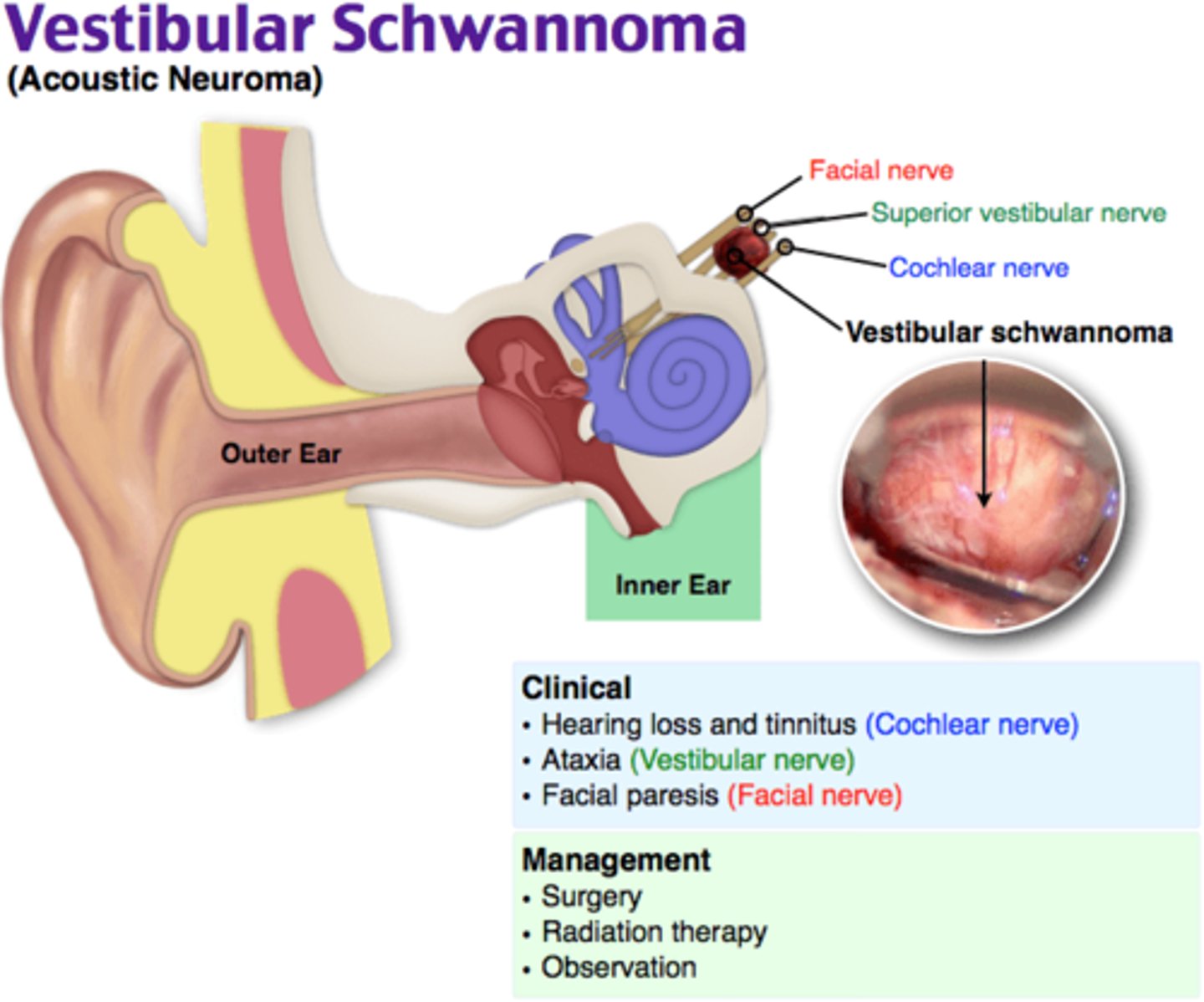
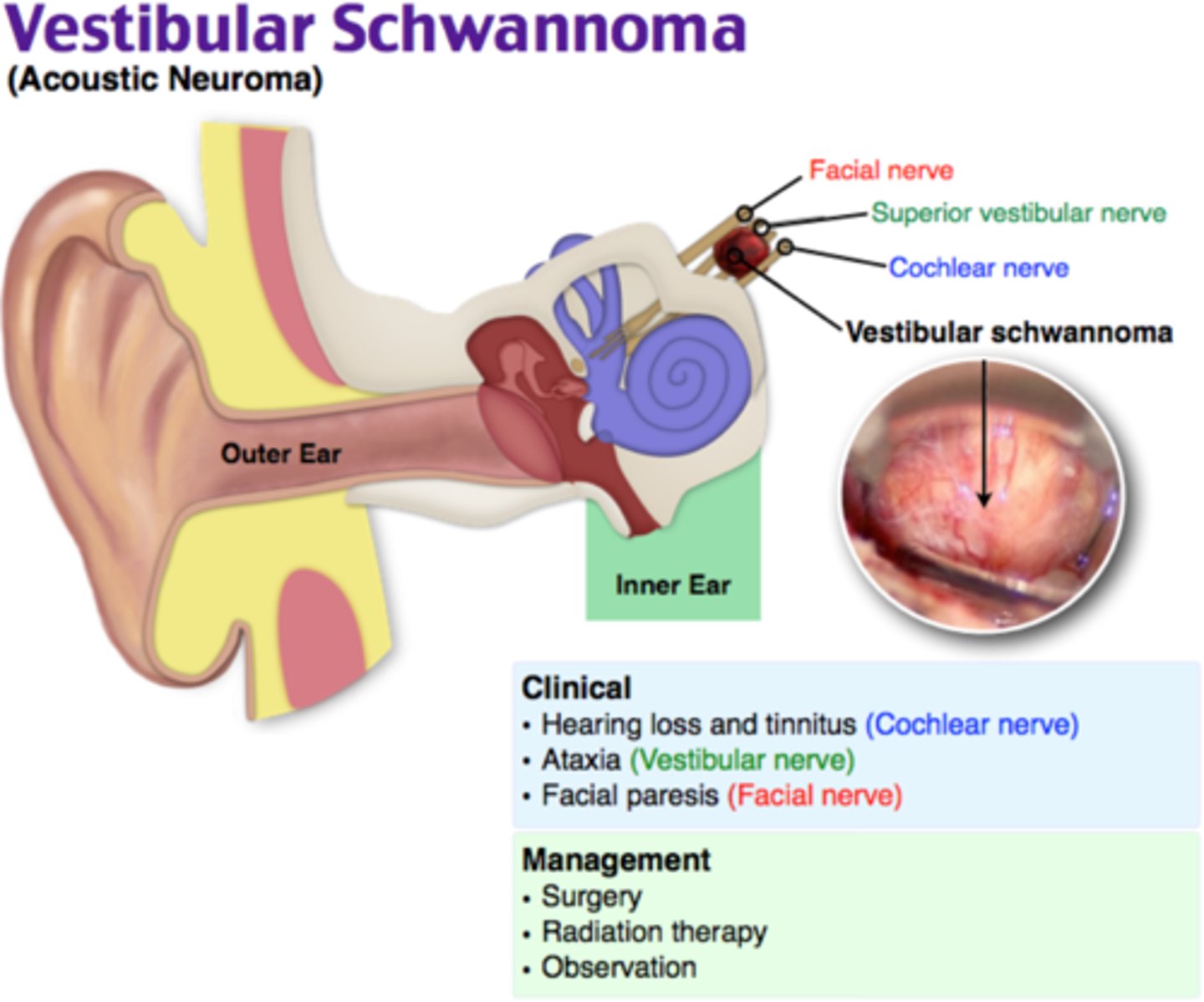
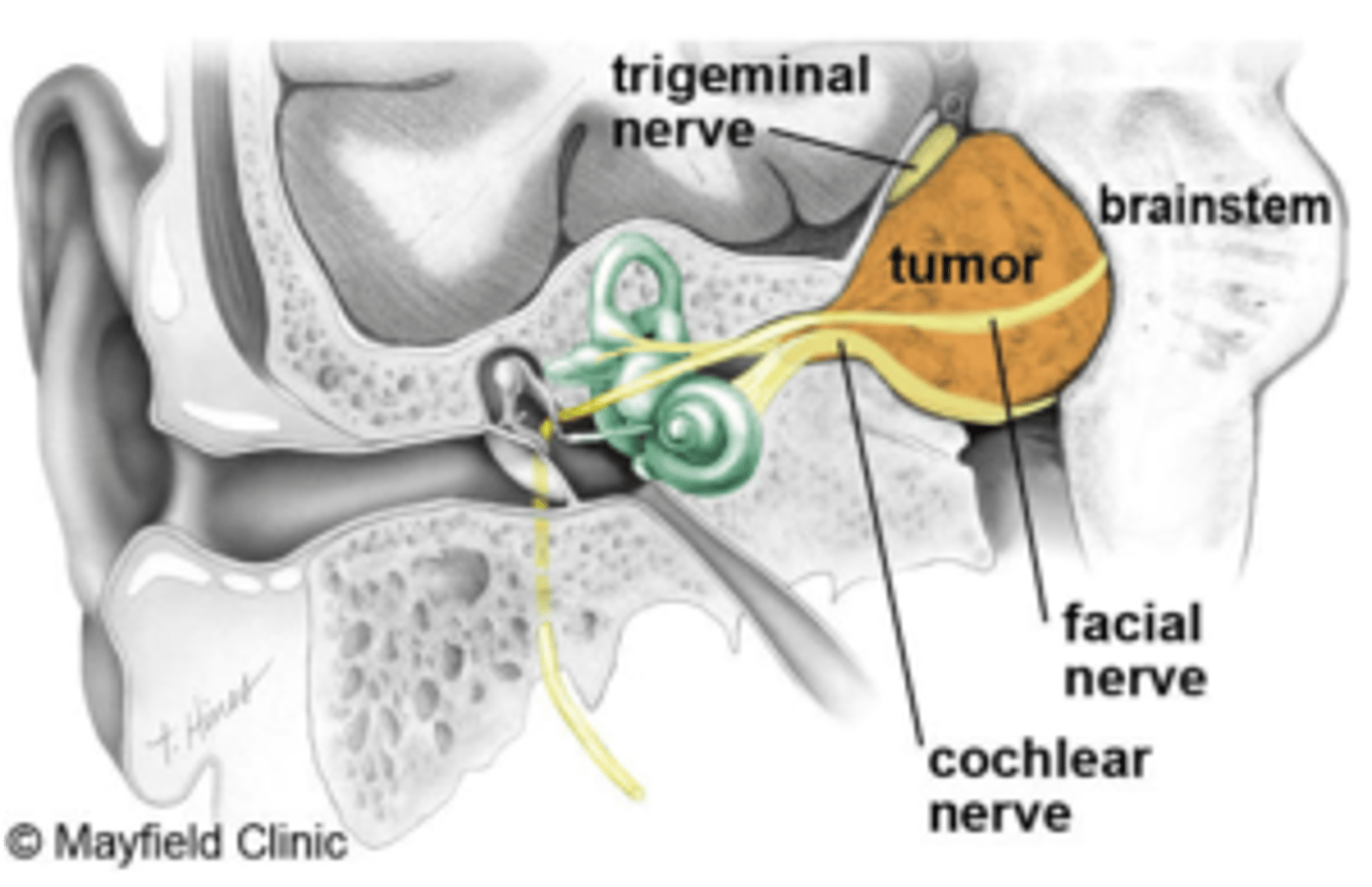
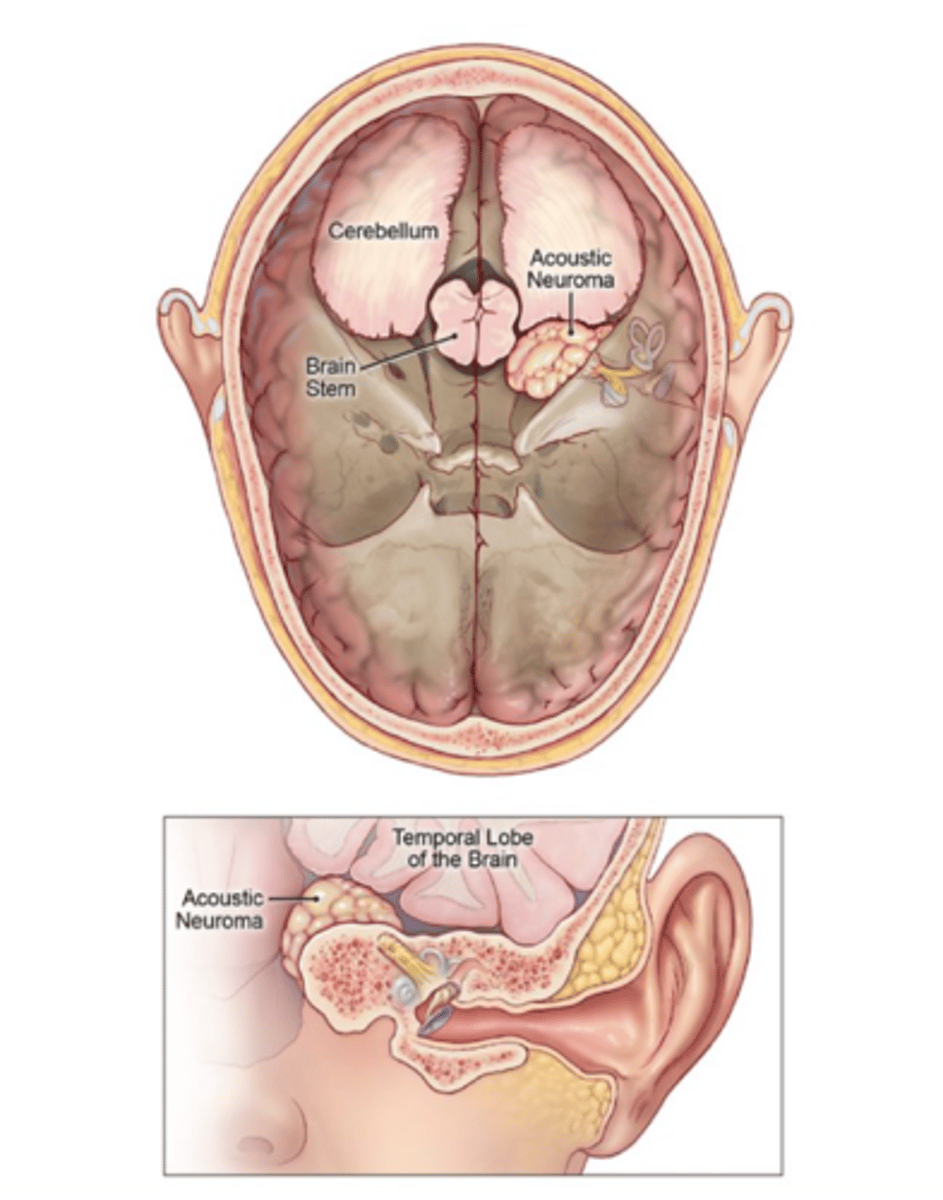
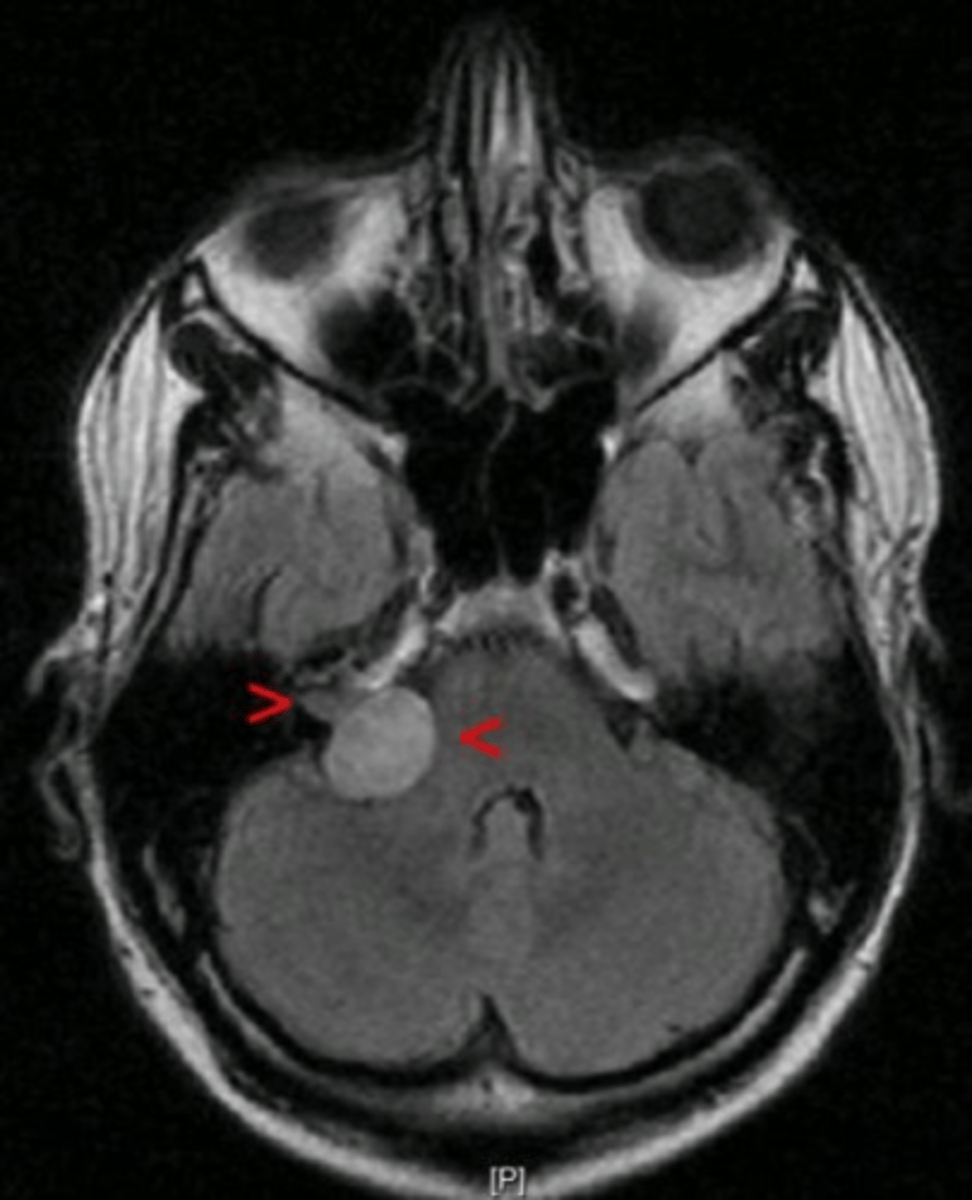
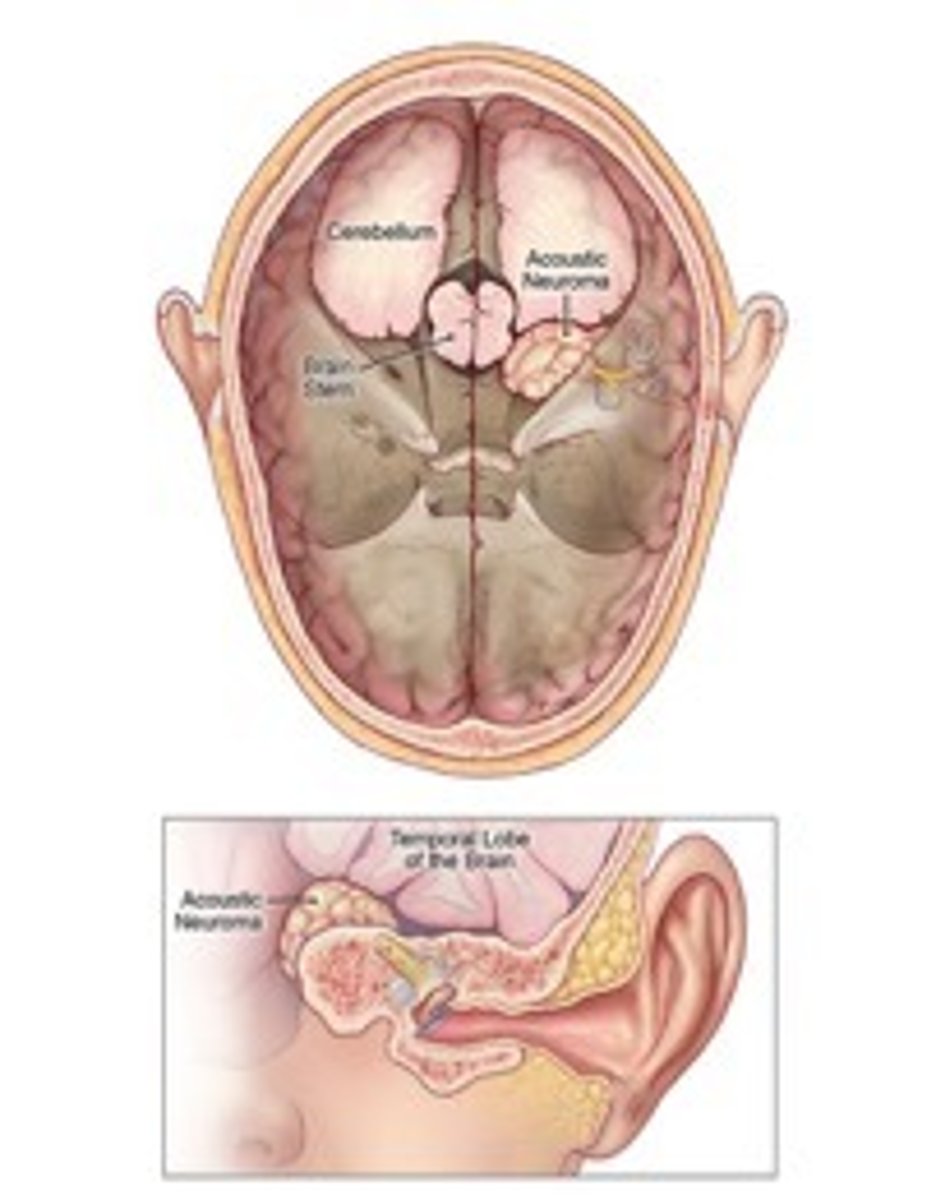
Acoustic Neuroma (Vestibular Schwannoma)
Benign, slow-growing tumor of nerve sheath (schwan cells) of acoustic nerve.
Thery account for 90% of cerebellopointine angle tumours
Cerebellopontine angle
The junction at the base of the brain where the cerebellum, medulla, and pons communicate
CN 5,6,9,10

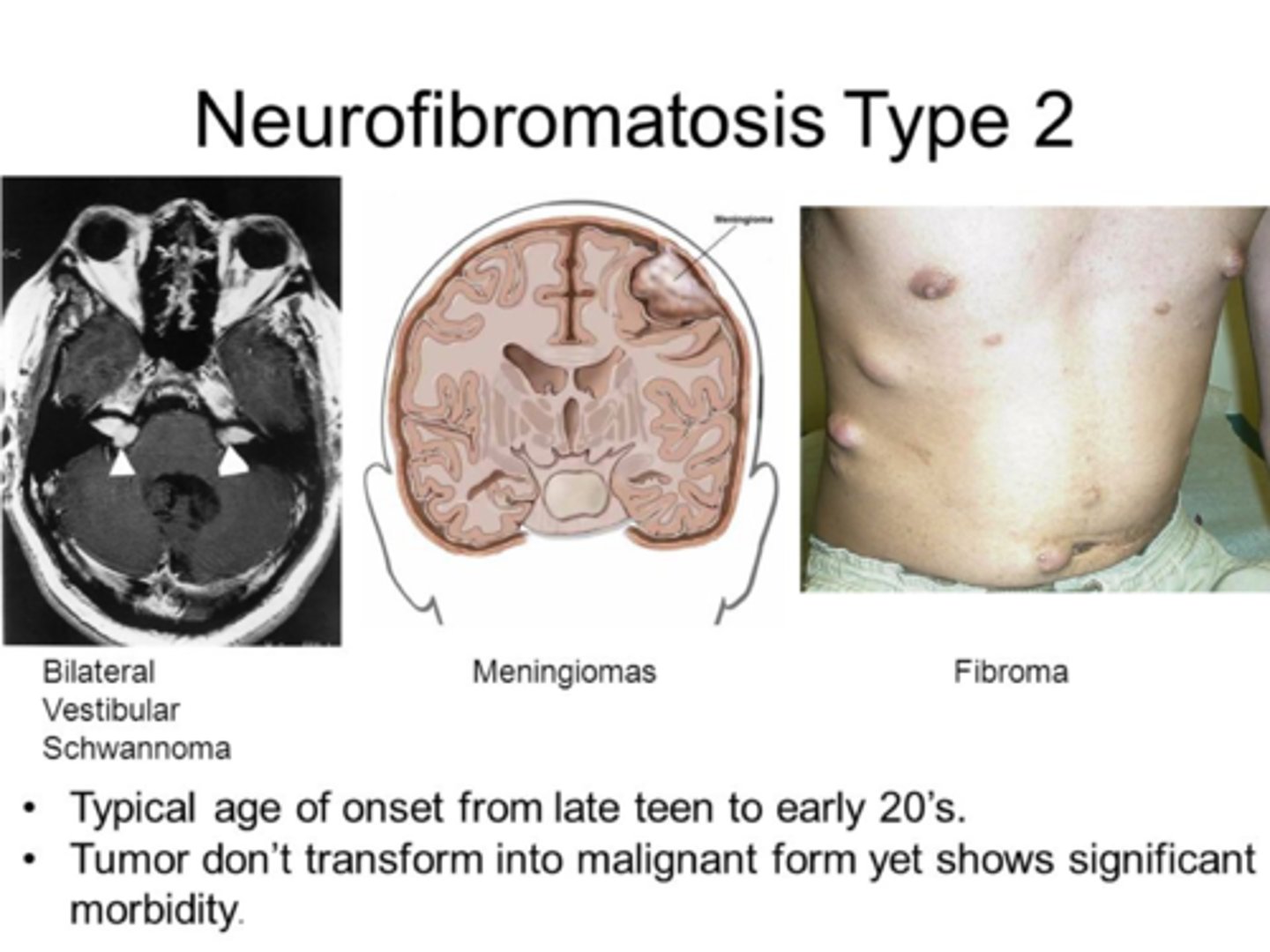
Bilateral acoustic neuromas are strongly associated with?
Bilateral vestibular schwannomas are seen in neurofibromatosis type 2, SCHWANN CELLS EXPRESS A GENE CALELD NEUROFIBROMIN 2 ENCODING A PROTEIN CALLED MERLIN WHICH IS A TUMOUR SUPRESSOR GENE) and in neurobromatosis there is deletion on chromosome 22 leading to mutation of in NF2 which inactivates merlin àuncontrollable division
But majority of tumours (90%) are unilateral
Clinical features of acoustic neuroma
Cochlear nerve involvement
- Unilateral sensorineural hearing loss (most common symptom)
- Tinnitus
Vestibular nerve involvement
- Dizziness
- Unsteady gait and disequilibrium
Later symptoms are caused by pressure of the tumour on adjacent structures of the cerebellopontine angle
Trigeminal nerve (CN V) involvement: paresthesia (numbness), hypoesthesia (decreased sensation), and/or unilateral facial pain, absent corneal reflex
Facial nerve (CN VII) involvement: peripheral, unilateral facial weakness that can progress to paralysis
Cerebellum: ataxia
Fourth ventricle: hydrocephalus
Management of Acoustic Neuroma
Patients with a suspected vestibular schwannoma should be referred urgently to ENT.
It should be noted though that the tumours are often slow growing, benign and often observed initially.
What is the investigation of choice for acoustic neuroma?
CONTRAST MRI as well as Audiometry as only 5% of patients will have a normal audiogram
Management options for acoustic neuroma
Management is with either surgery, radiotherapy or observation.
Observation of the tumor can be considered in patients with small tumors or minimal hearing loss, or if they are of advanced age. These patients should undergo MRI surveillance every 6-12 months.
Ramsay Hunt Syndrome (Herpes Zoster Oticus)
Caused by reactivation of Varicella in the GENTICULATE GANGLION OF CN 7 + 8
Essentially there is a herpetic infection of these cranial nerves
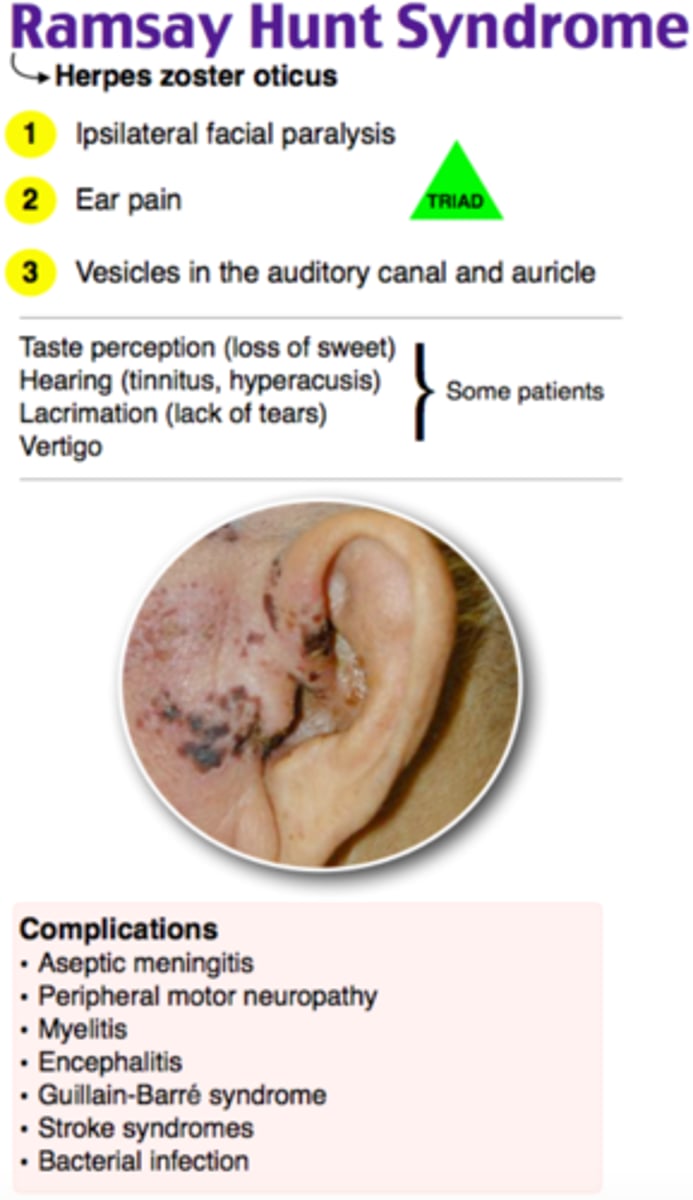
Clinical features of Ramsay Hunt Syndrome
- Auricular pain
- Facial nerve palsy
- Vestibular rash around the ear
- Vertigo
- Tinnitus
- Fever
Management of Ramsay Hunt Syndrome
ORAL ACICLOVIR + CORTICOSTEROIDS

Vestibular sedative drugs
Prochlorperazine - D2 antagonist
SE of prochlorperazine
QT prolongation
Parkinsonism
Tardive dyskinesia
Restlessness
Respiratory depression
Drug induced cholestasis
Causes of vertigo
Meniere's, vestibular neuritis, acoustic neuroma, MS, CN 8 lesions, brainstem or cerebellar tumors or bleeding
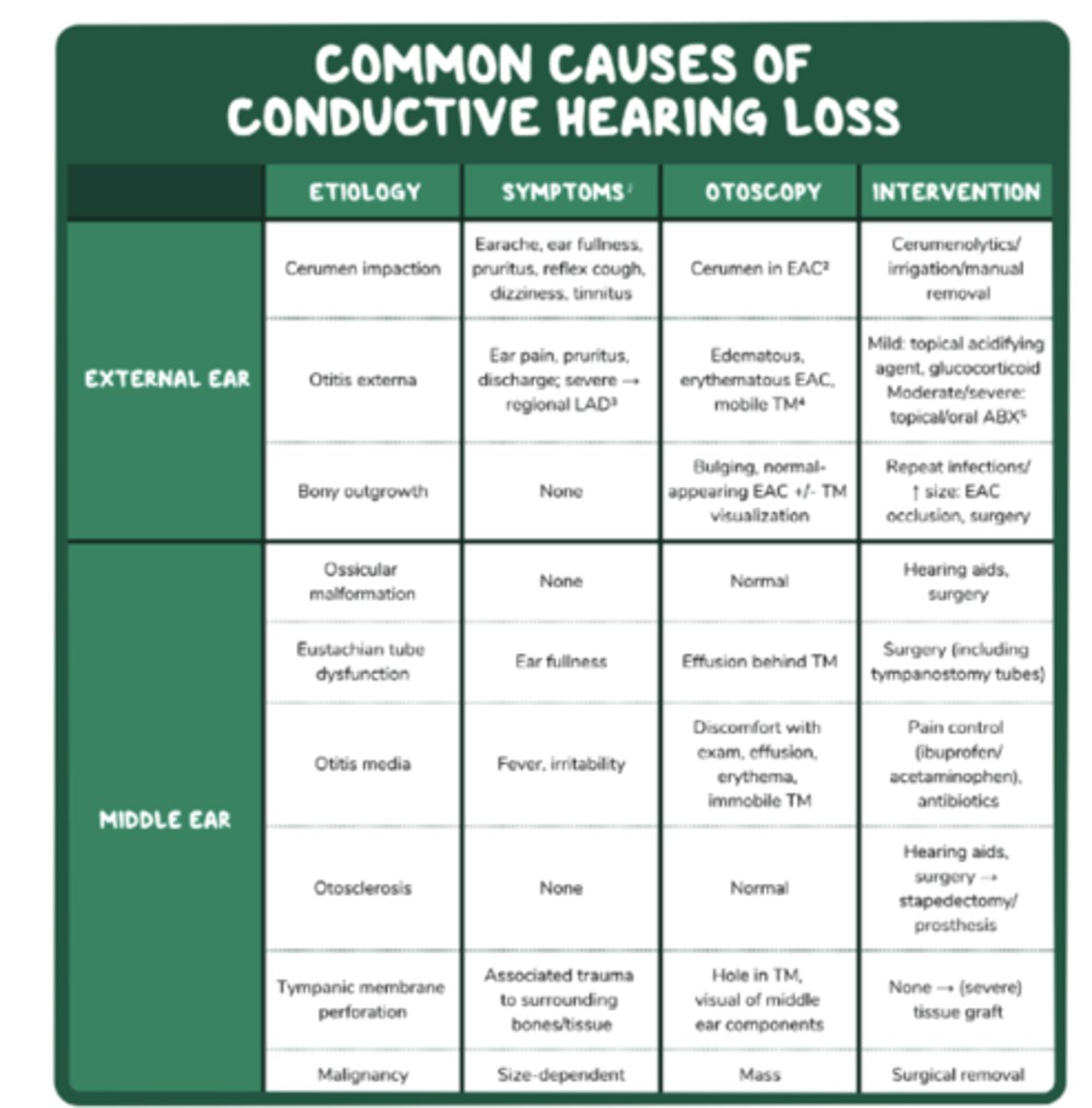
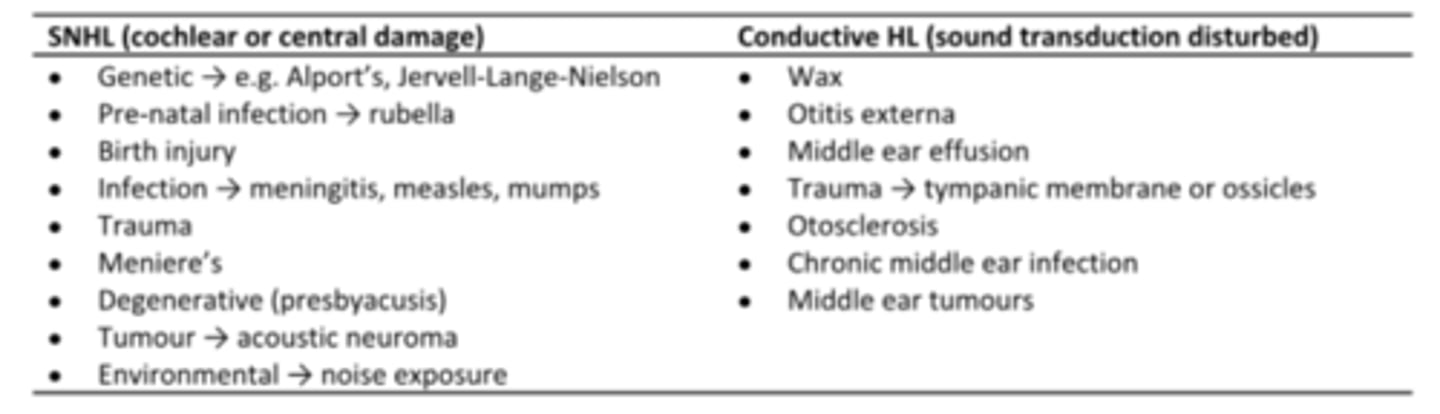
Conductive hearing loss
Hearing impairment caused by interference with sound or vibratory energy in the external canal, middle ear, or ossicles
BETWEEN OUTER EAR AND FOOT PLATE OF STAPES IN MIDDLE EAR
1) EXTERNAL CANAL OBSTRUCTION
· Wax impaction
· Discharge from otitis externa
· Glue ear (otitis media with effusion)
· Foreign bodies
· Developmental abnormalities (DOWNS SYNDROME)
2) PERFORATION OF EAR DRUM
· Trauma
· Barotrauma
· Infection – ear infections, otitis media with effusion (glue ear), chronic suppuratve otitis media (SECRETORY OTITIS MEDIA)
3) PROBLEMS WITH OSCULAR CHAIN
· Osteosclerosis - CARHARTS NOTCH WHERE THERE IS AN APPARENT LOSS OF BONE CONDUCTION AT 2000HZ (characteristic audiometric sign)
· Infection
· Trauma
4) INADEQUATE EUSTACHIAN TUBE VENTILATION
· With/without effusion
· Eg secondary to nasopharyngeal carcinoma
· Large adenoids
· Eustachian tube dysfunction
Sensorineural hearing loss
Hearing loss caused by damage to the cochlea's receptor cells or to the auditory nerves; also called nerve deafness
THERE IS A POBLEM IN THE COHLEAR OR AUDITORY NERVE
Presbycusis
Noise-induced hearing loss
Congenital infections (e.g. rubella, CMV)
Neonatal complications (e.g. kernicterus or meningitis)
Drugs (aminoglycosides)
Post infection due to meningitis, measles, mumps, flu, herpes, syphillis
Vascular pathology (stroke, transient ischaemic attacks)
Rare causes: acoustic neuroma, vitamin B12 deficiency, multiple sclerosis, brain mets.
Noise-induced hearing loss (NIHL)
Condition caused by the destruction of hair cells due to exposure to loud noise
Workers in heavy industry are particularly at risk
Hearing loss is bilateral and typically is worse at frequencies of 3000-6000 Hz
This could be one time, called acoustic trauma (sounds greater than 180dB) – may cause ear drum rupture and ossicles fracture
Or this could be gradually over time for example at work that over time causes hearing loss – 8 hours of sound at 85dB is typically enough to cause damage
Symptoms:
- Bilateral, symmetrical
- Sensorineural hearing loss
- +/- tinnitus
- may be noise induced temporary threshold shift
- audiometry shows a notch at 3,4 or 6kHz with recovery at 8
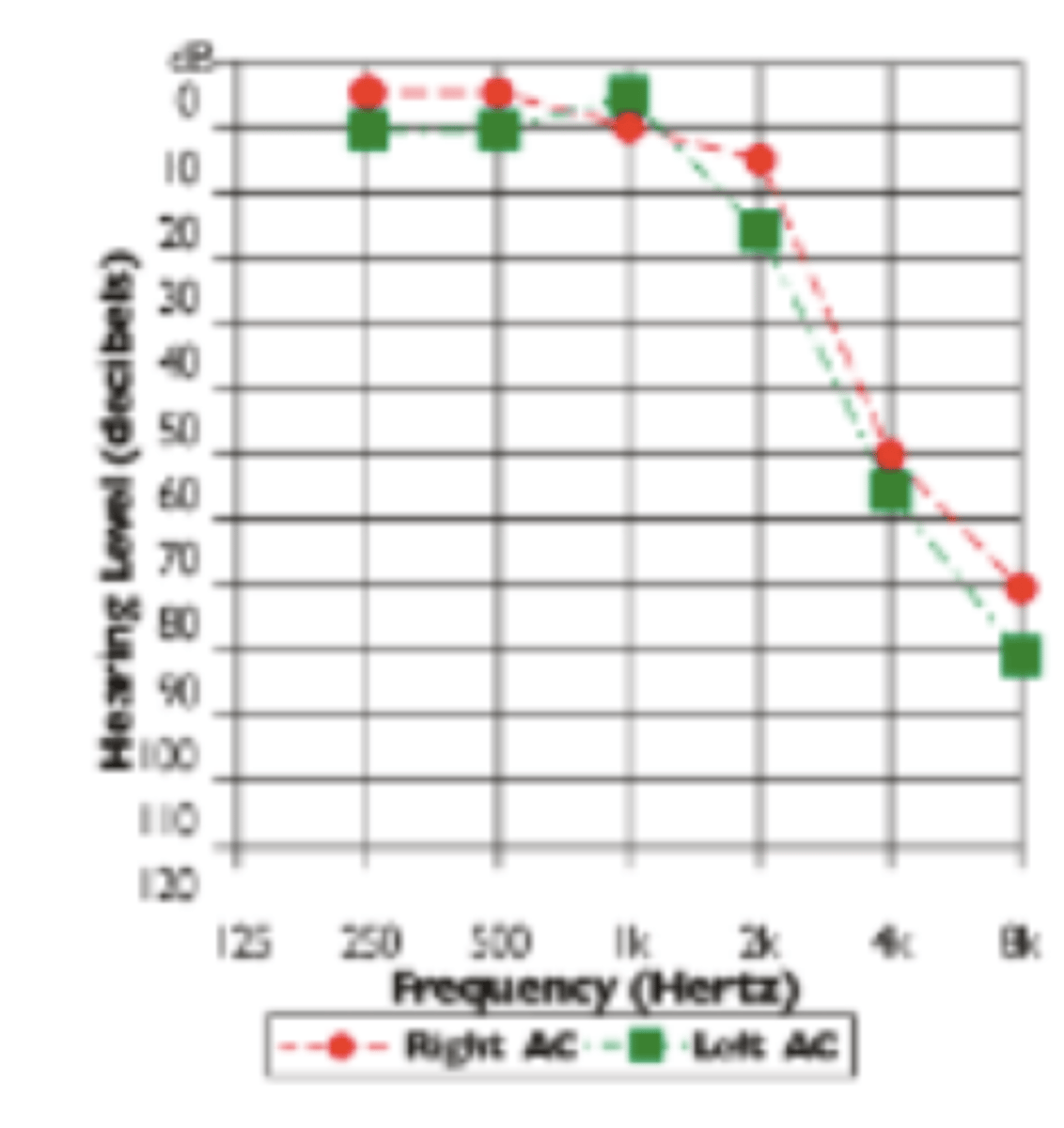
Presbyacusis
Age related, bilateral sensorineural hearing loss
High frequency hearing is affected bilaterally -conversational difficulties in noisy environments (hearing is most affected in the presence of background noise)
Audiometry shows bilateral high-frequency hearing loss
Precise cause is unknown, is multifactorial
- Arteriosclerosis – diminished perfusion and oxygenation of cochlea, damage to inner ear structures
- Diabetes – accelerates arteriosclerosis
- Accumulated exposure to noise
- Drugs – salicylates, chemotherapy
- Stress
- Genetics
Outline how you would go about investigating a patient with hearing loss
BEDSIDE
- Whispered voice test and finger rub test: screening to determine the extent of hearing loss
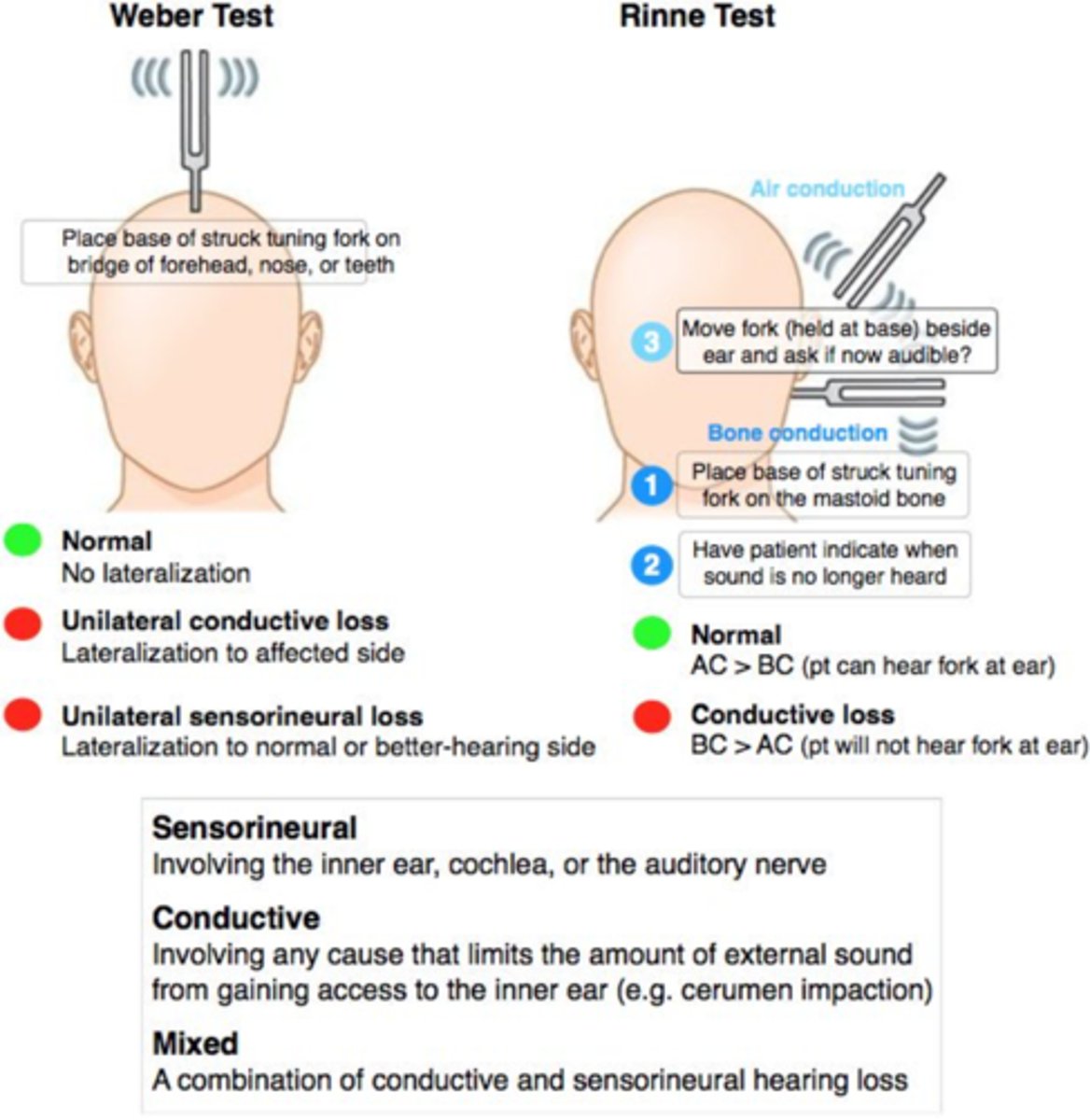
- Rinne test and Weber test: to classify hearing loss as conductive or sensorineural
- Otoscopy: allows for visual assessment of the external ear and tympanic membrane
BLOODS
- FBC
- Glucose
- TSH
- Syphillis testing
IMAGING
- MRI or CT
AUDIOMETRY!!
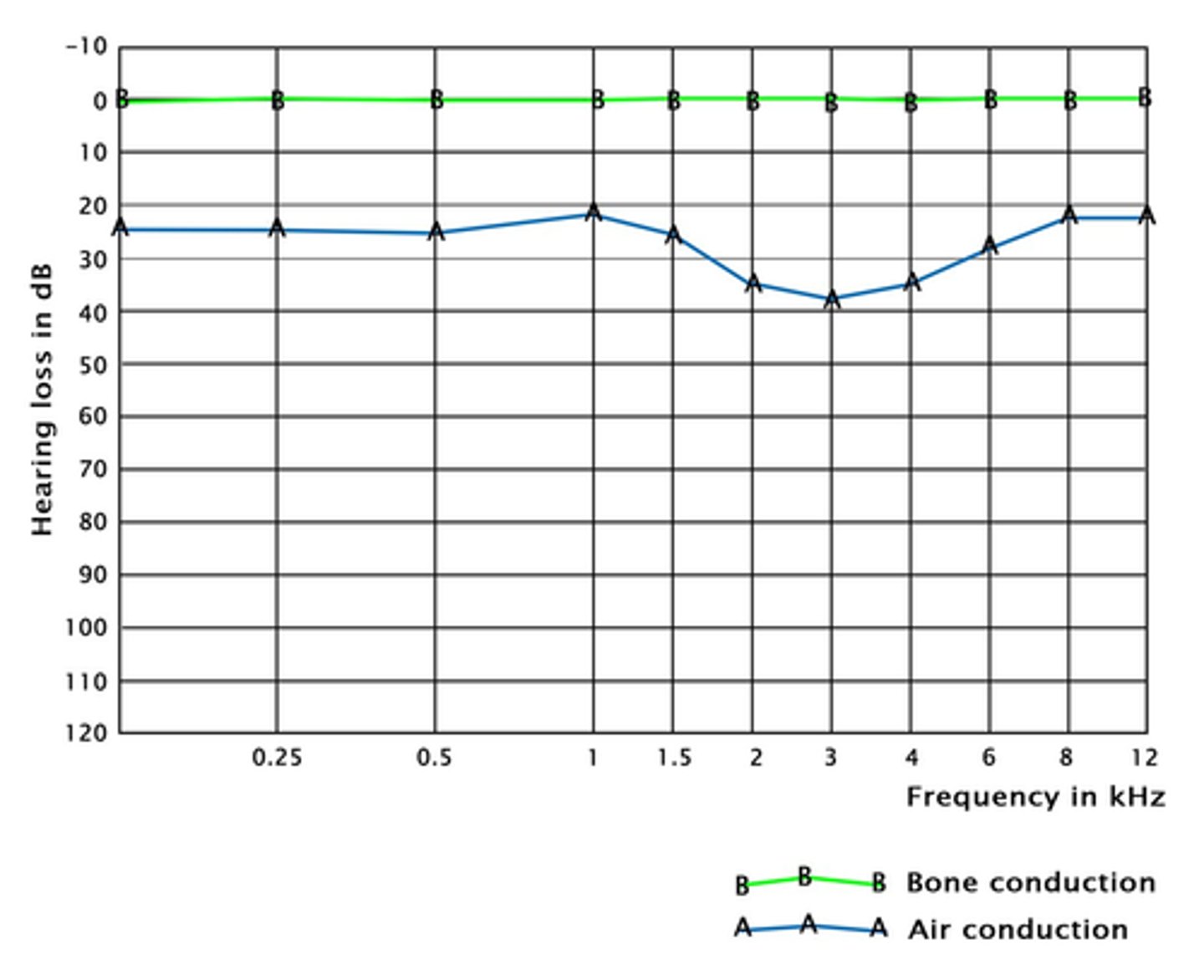
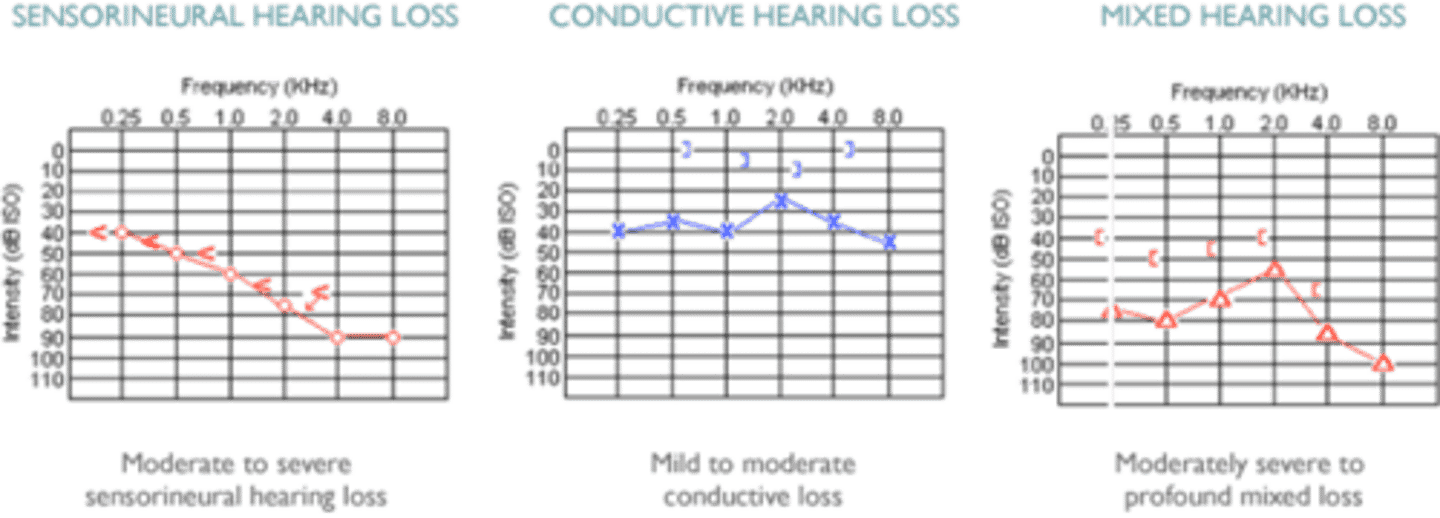
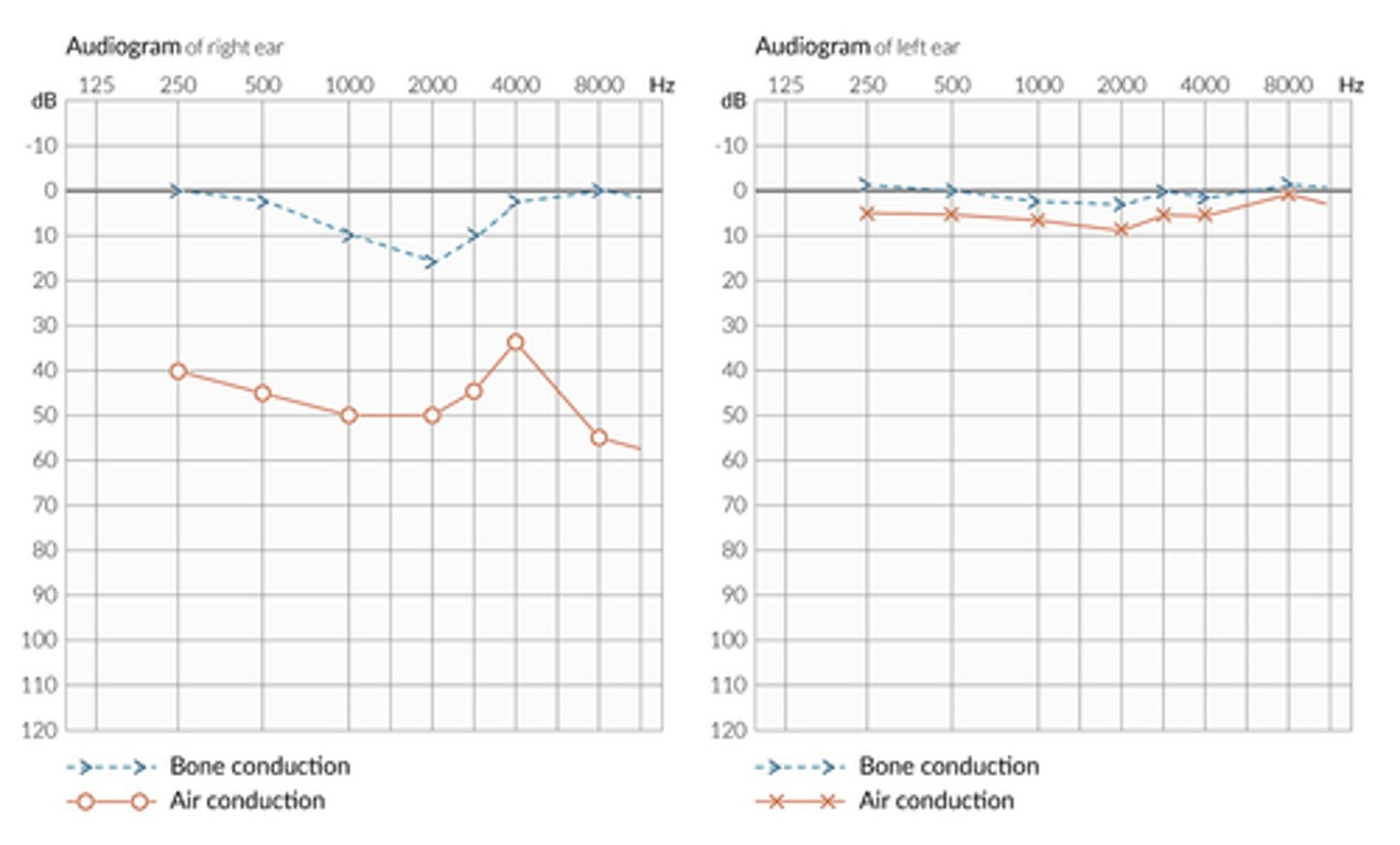
Audiometry interpretation conductive hearing loss
In conductive hearing loss (damage to the middle or external ear) AIR CONDUCTION IS IMPAIRED
So the auditory threshold is increased in air conduction; however, the auditory threshold is normal in bone conduction
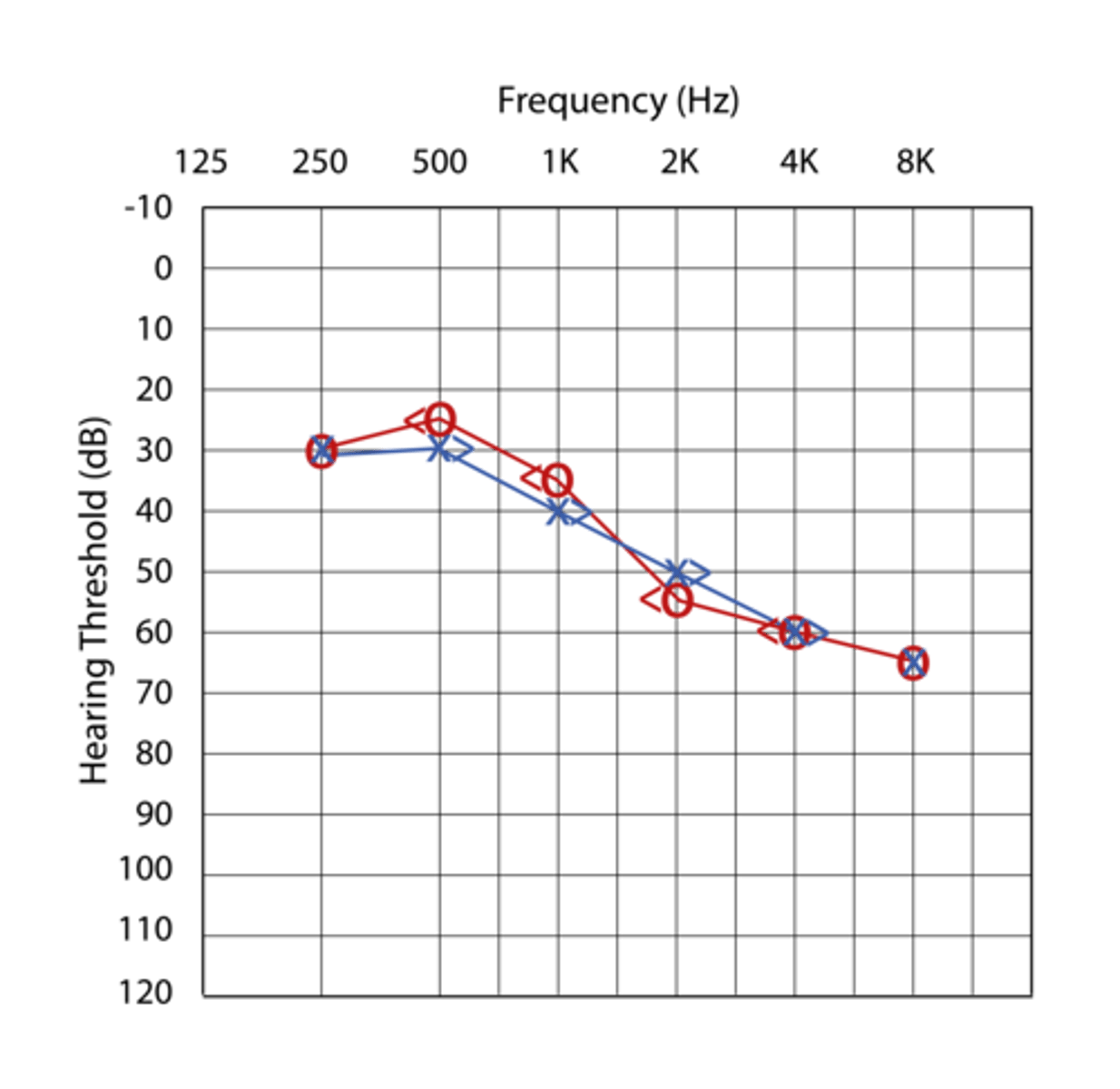
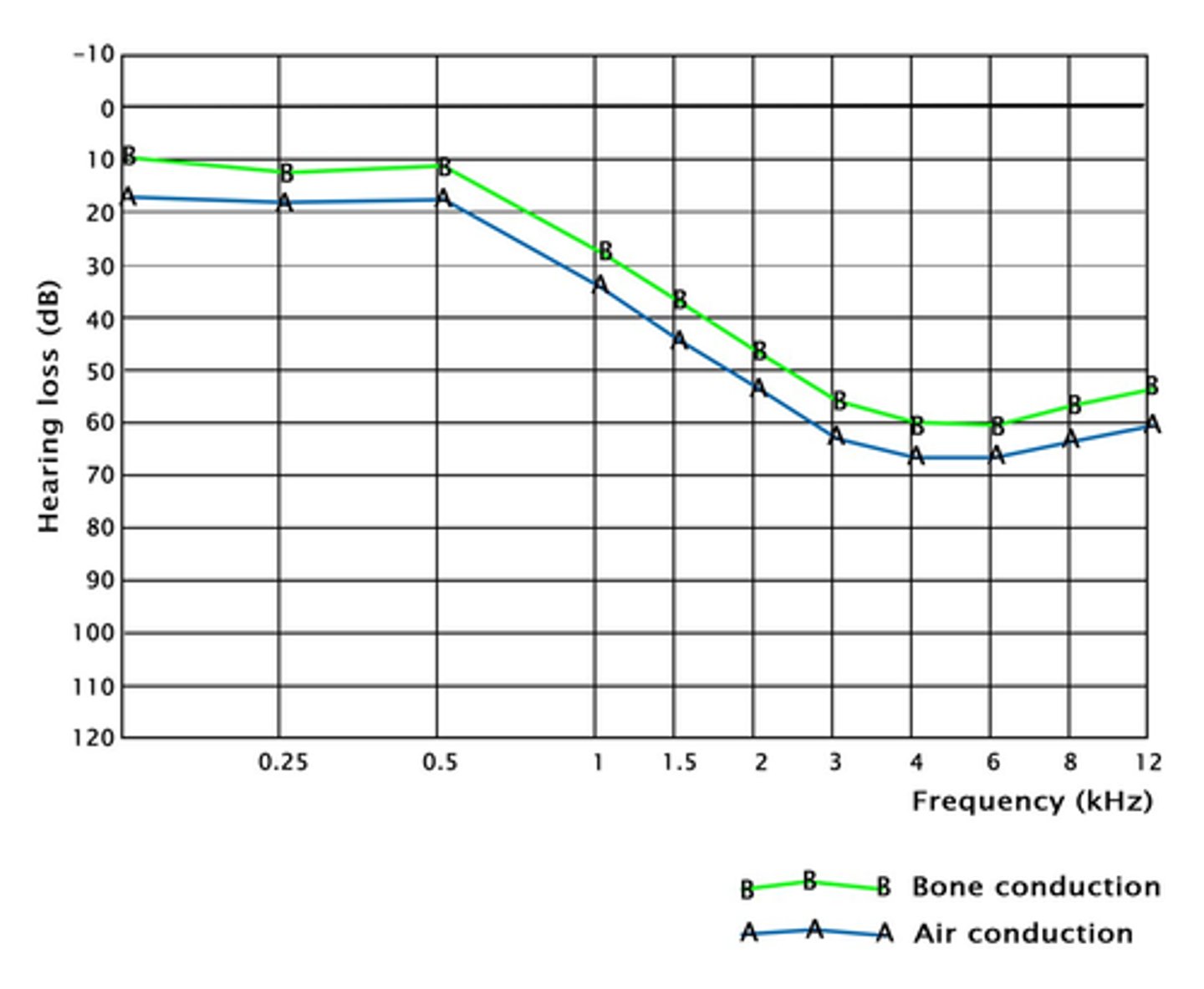
Audiometry interpretation in sensorineural hearing loss
Both air and bone conduction are impaired so hearing threshold increases for both
Mixed hearing loss audiogram
In mixed hearing loss both air and bone conduction are impaired, with air conduction often being 'worse' than bone
Audiogram in presbycusis
Increasingly deafer at high frequencies
They struggle to hear higher frequencies in both air and bone conduction
Otosclerosis audiogram
Carhart notch - notched hearing loss at 2000Hz with CONDUCTIVE HEARING LOSS so air conduction is impaired
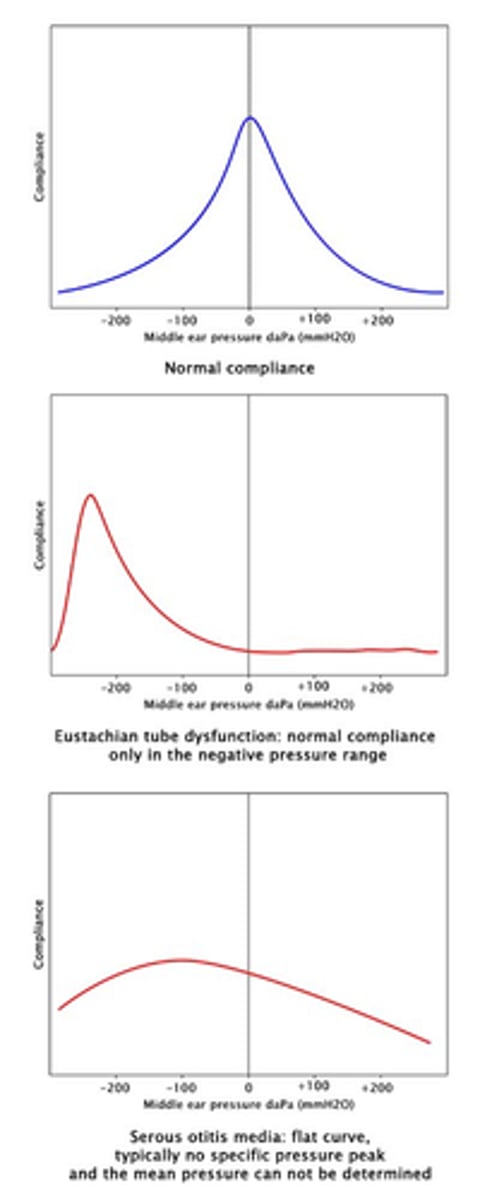
Tympanometry finding in secretory otitis media
Normal middle ear function: maximum compliance of ∼0 Pa
Eustachian tube dysfunction: displacement of normal compliance in the region of negative pressure
Secretory otitis media: flat tympanometry curve without an identifiable maximum
Rinne and weber test
Rinne test: tuning fork on mastoid, then near ear
Weber test: tuning fork on top of head, then near ear
Normal: AC > BC in both ears
Abnormal Rinne test
• Right bone conduction problem => BC > AC on right (lateralization to right side)
• Left neural problem => AC > BC on both sides (lateralize to right side)
REMEMBER WITH WEBER TEST THE SOUND SHOULD NOT LATERALISE ! (if it does it means you either have sensorineural in other ear or conductive in that ear)
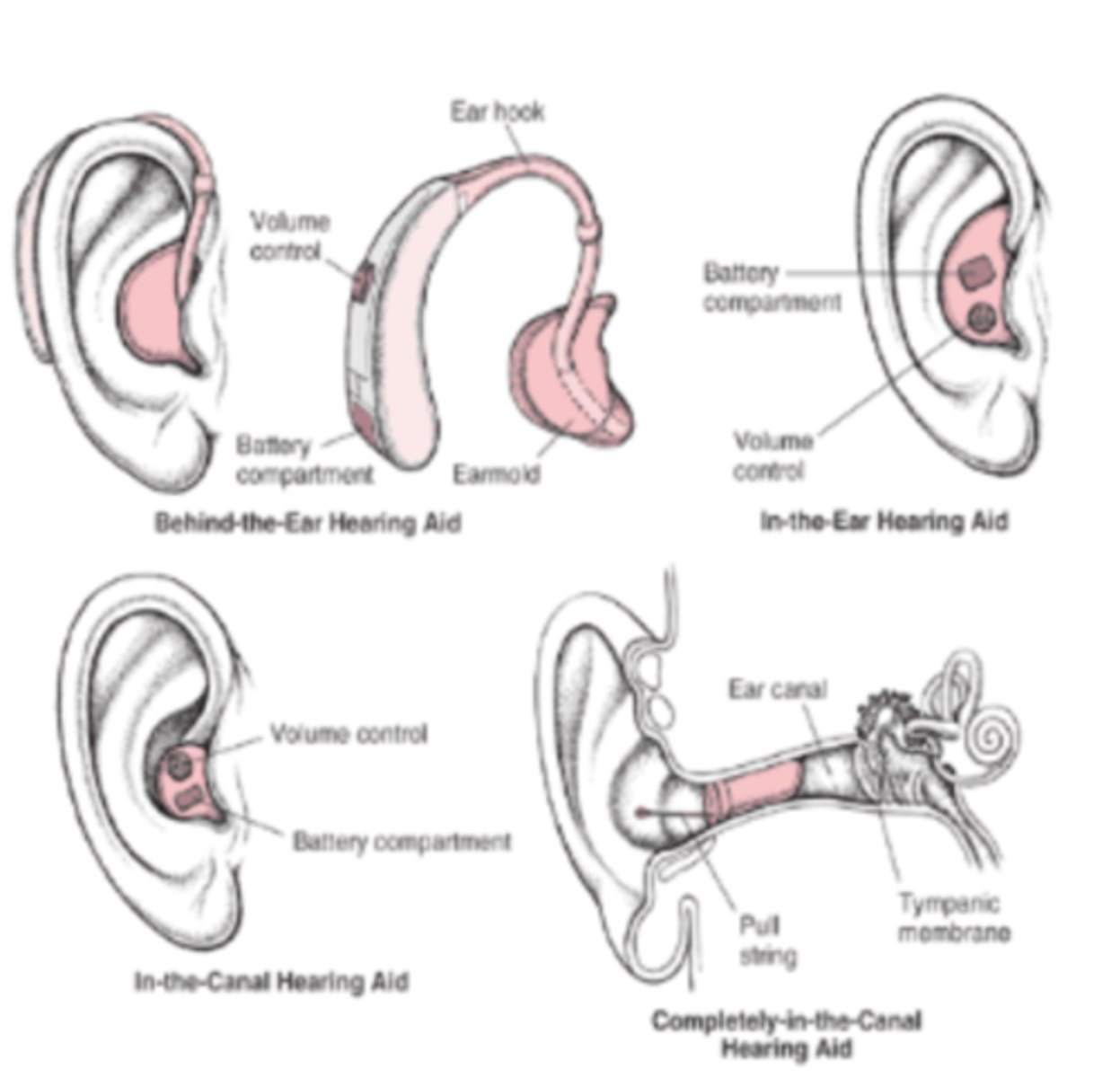
Types of hearing aids
HEARING AIDS
Behind the ear or in the ear
Low to high power amplification
Analogue/digital
BONE ANCHORED HEARING AIDS (BAHA)
This is for significant conducting hearing loss
Surgically implanted (mastoid) titanium base
Electronic amplification device attachment
Allows bone transmission of sound
Indications for this include:
- Significant conductive hearing loss
- Intolerance of hearing aids
- Congenital malformations
Single sided deafness
COCHLEAR IMPLANTS
For profound hearing loss
Electrically stimulates auditory nerve directly
NICE recommends implants for adults or children with PROFOUND SENSORINEURAL HEARING LOSS who do not benefit from traditional hearing aid
Electrode is inserted surgically into cochlea which will directly stimulate the auditory nerve when electrical signals are applied
Electrode is attached to external auditory processor through skin with magnetic coupler
Note that the signal is not normal sound which is why intensive therapy is needed to understand new sounds
The implants will help with lip reading, provision and recognition of environmental sounds and help relief isolation
Outer ear causes of otalgia
Perichondritis
Otitis externa
Furuncle
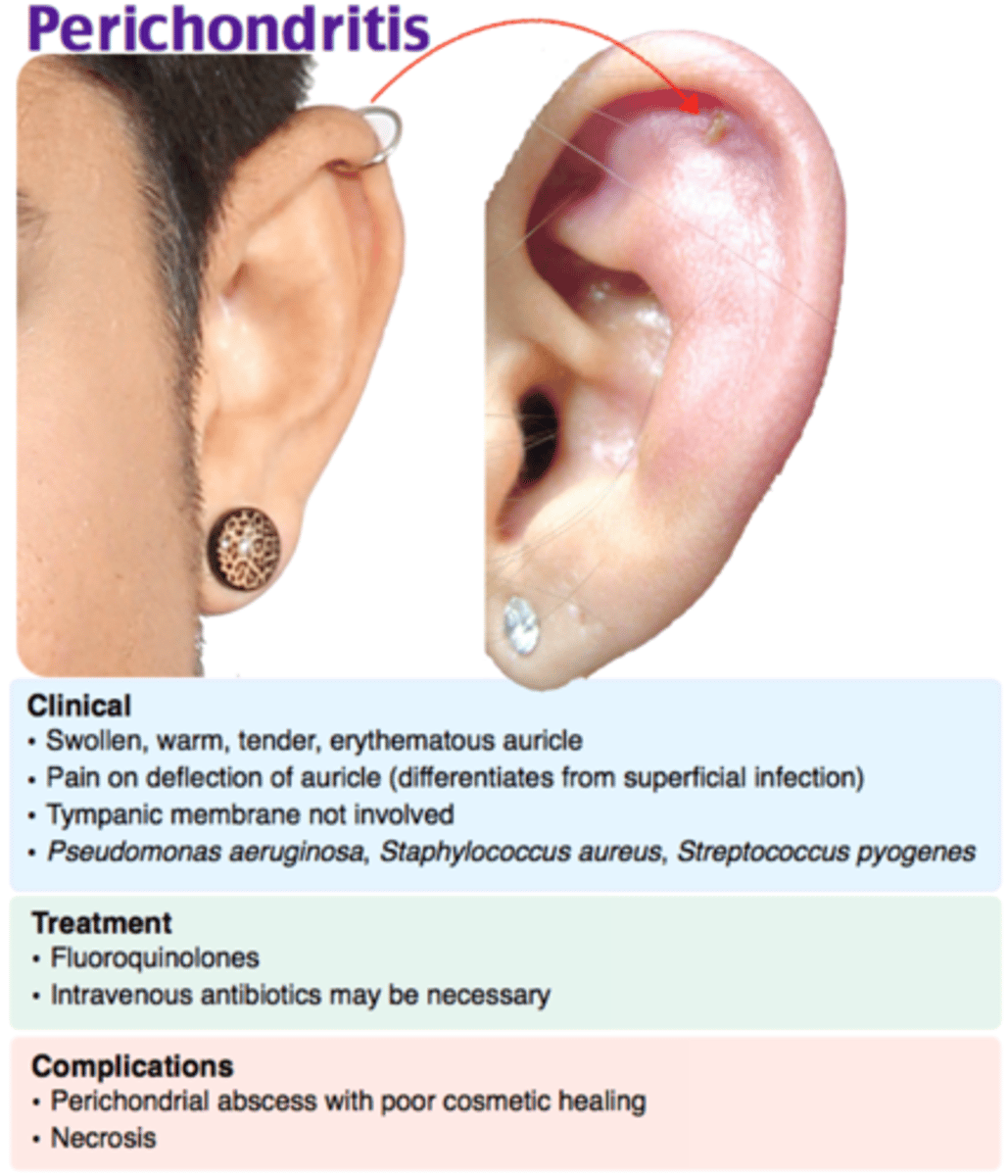
Causes of otalgia
50% have spontaneous resolution with no underlying detectable cause.
External ear causes:
- otitis externa
- foreign body
- trauma
- impacted cerumen (earwax)
- furuncle
- herpes zoster
- neoplasm
- otomycosis
- perichondritis of pinna
- Sjogren's syndrome
Middle ear causes:
- otitis media
- acute mastoiditis
- barotrauma
- acute Eustachian tube obstruction
- neoplasm
- trauma
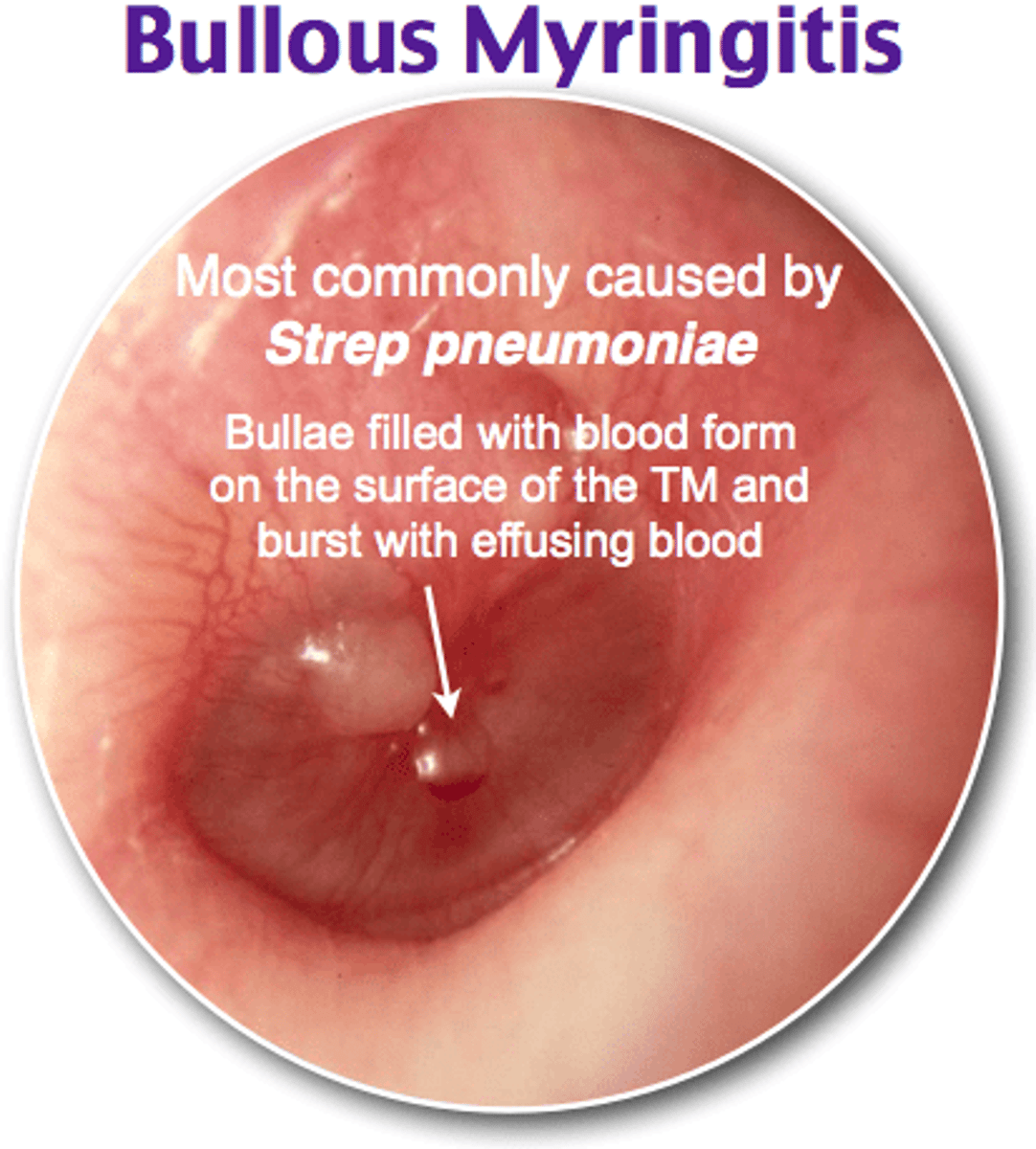
- bullous myringitis
- furunculosis
Referred ear pain
- nasopharynx: adenoidectomy, infection, neoplasm
- salivary gland infection or calculi
- from teeth, jaw, oesophagus, larynx, oropharynx, tongue, cervical spine, cranial nerves, temporomandibular joints
- tonsillitis
- GCA
- thyroiditis
TMJ dysfunction
Temporomandibular joint; abnormality of joint where lower jaw hinges to upper jaw
· Ear ache
· Facial pain
· Joint clicking/popping related to teeth grinding
· Stress - makes it a biopsychological disorder which may lead to chronic pain syndrome
· Joint tenderness which is made worse by lateral movement of the jaw or trigger points in the pterygoids
Bullous Myringitis
Small vesicles containing blood on the drum; accompany mycoplasma pneumonia and virus infections
PAINFUL HAEMORRHAGIC BLISTERS OF TYMPANIC MEMBRANE
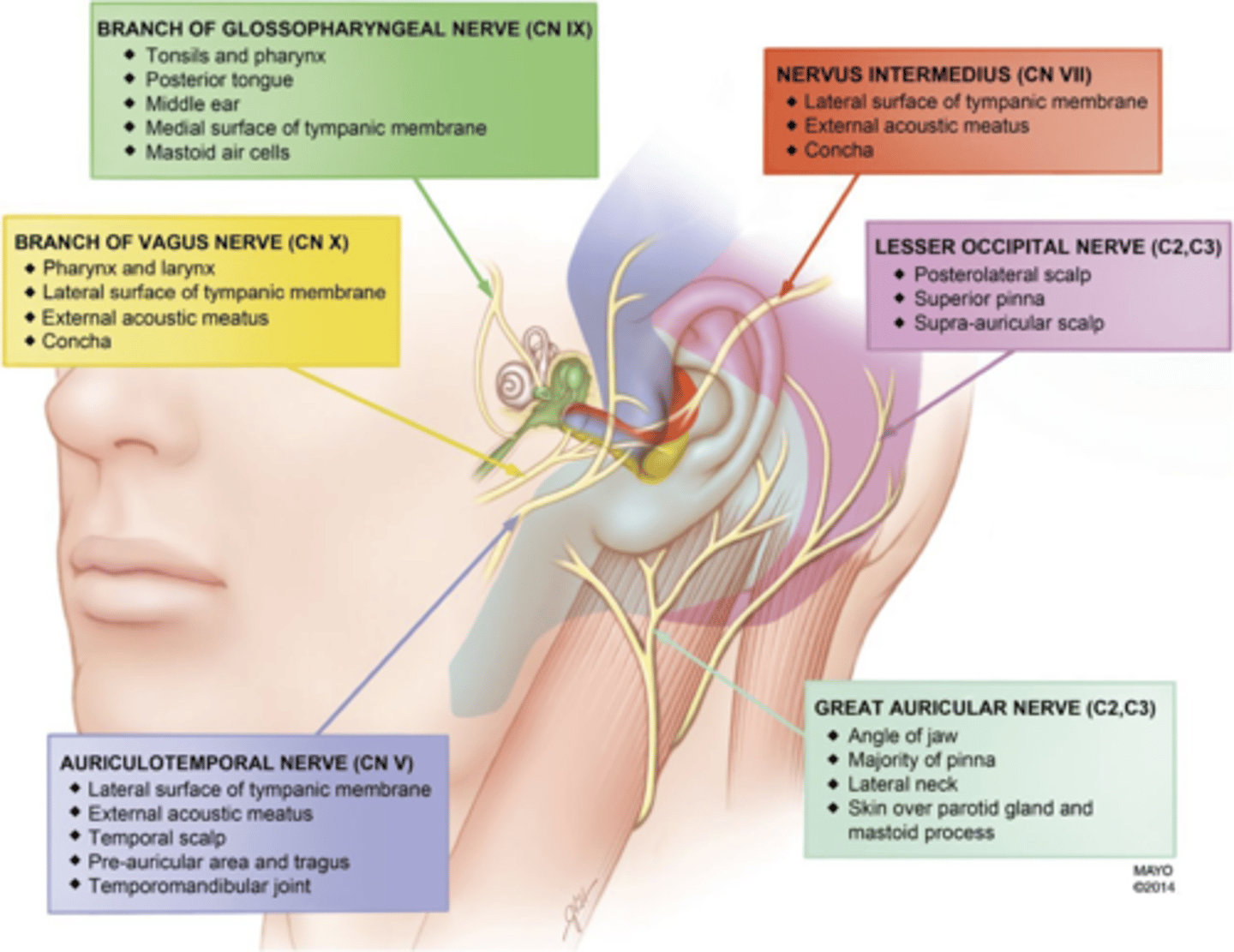
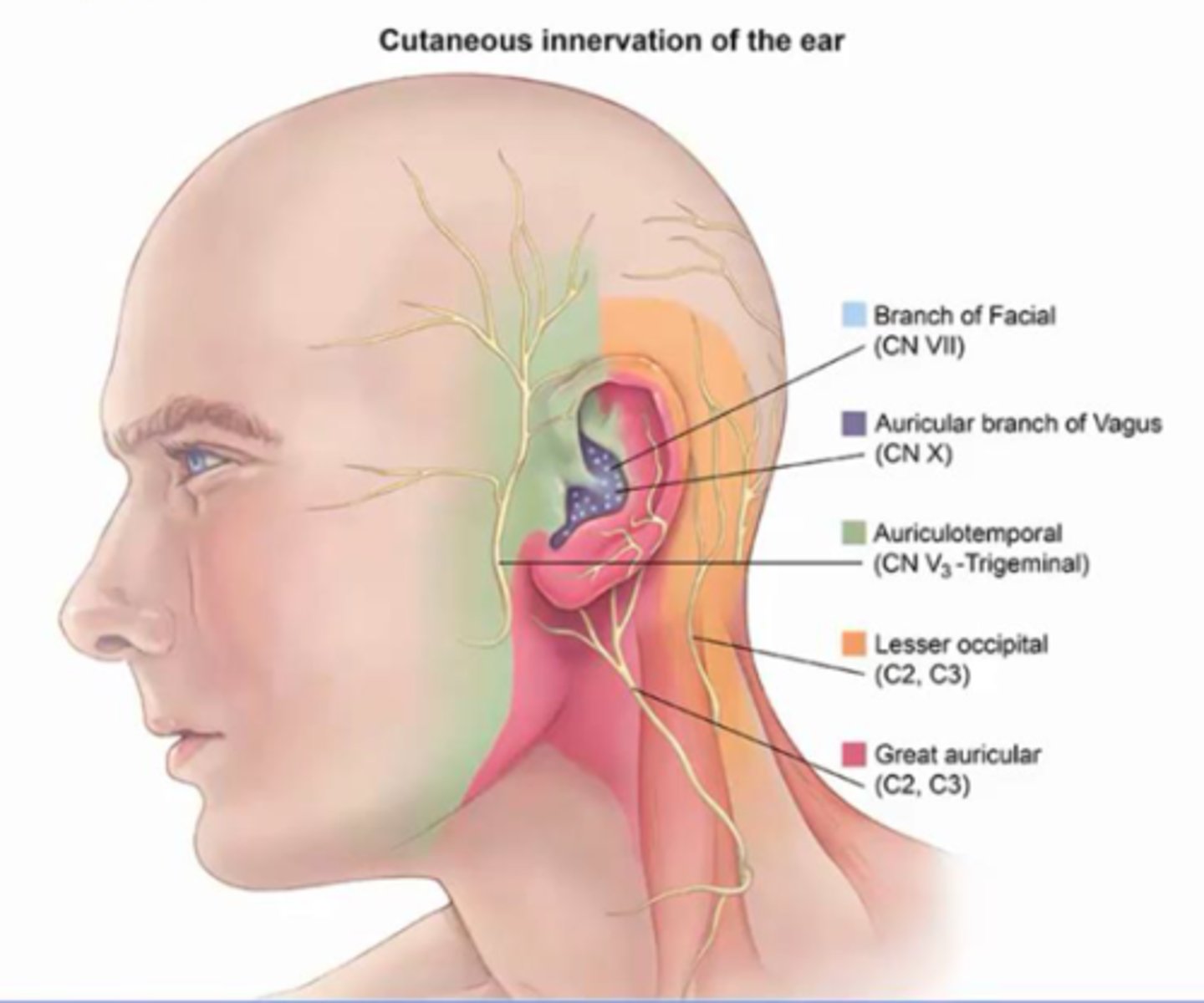
Which nerves are involved in referred ear pain?
Trigeminal nerve
Facial nerve
Glosopharyngeal nerve
Vagus nerve
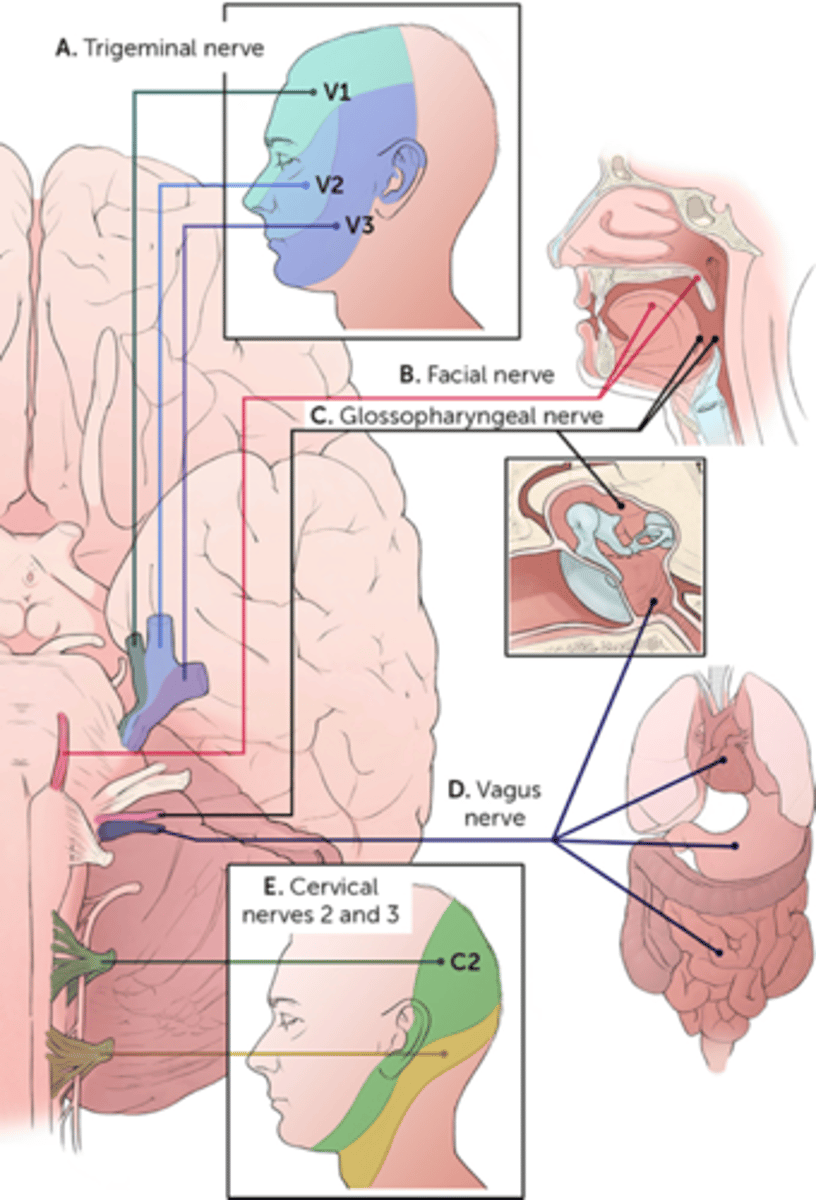
Auricotemporal nerve is a branch of?
V3 of trigeminal
Supplies lateral upper half of pinna
May refer from dental disease or TMJ dysfunction, parotid, tongue, nose, sinuses
Pathologies:
- trigeminal neuralgia
- dental disease
- TMJ dysfunction
- parotid infection/tumour
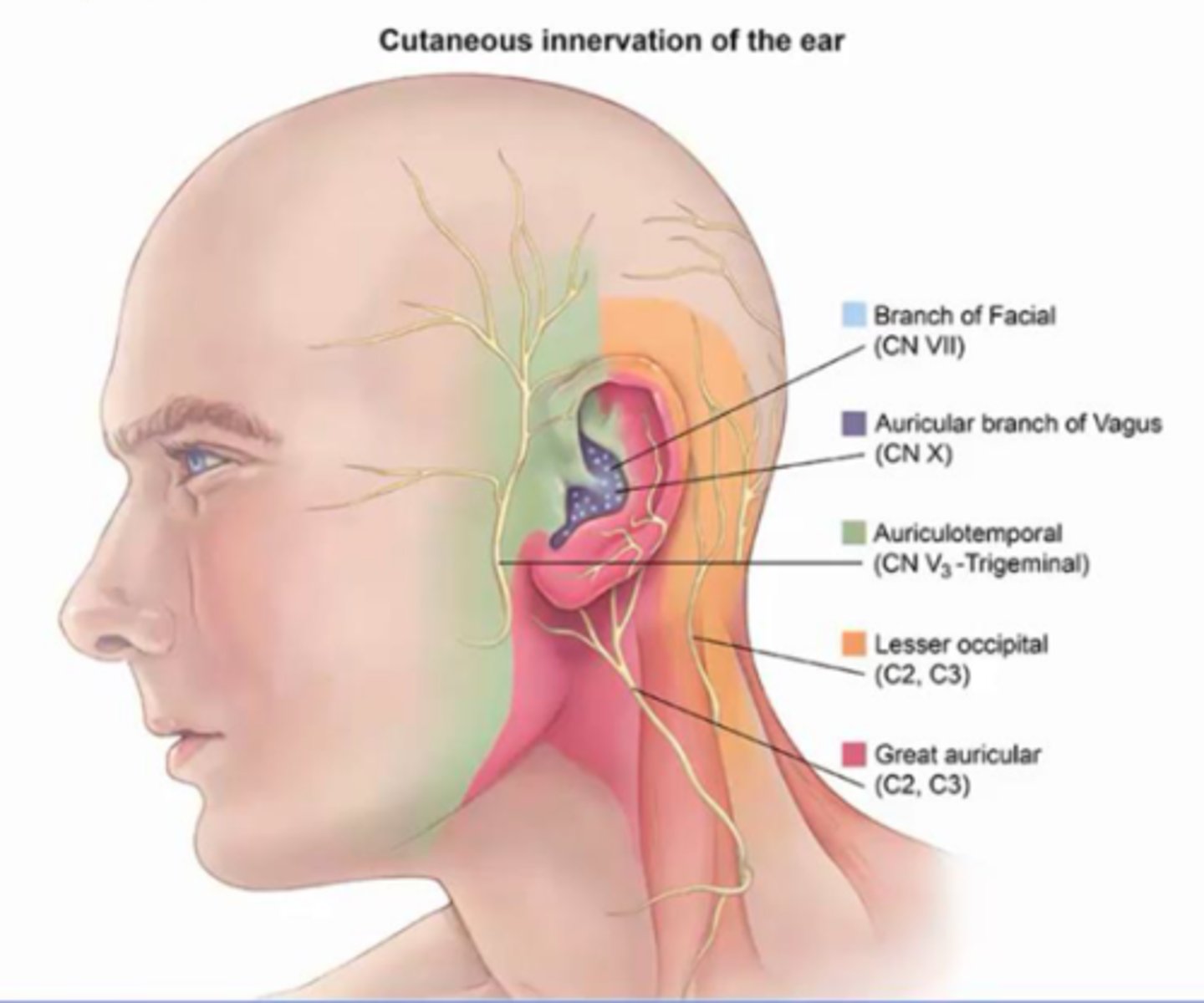
What nerve supples external auditory meatus?
Auricular branch of the facial nerve
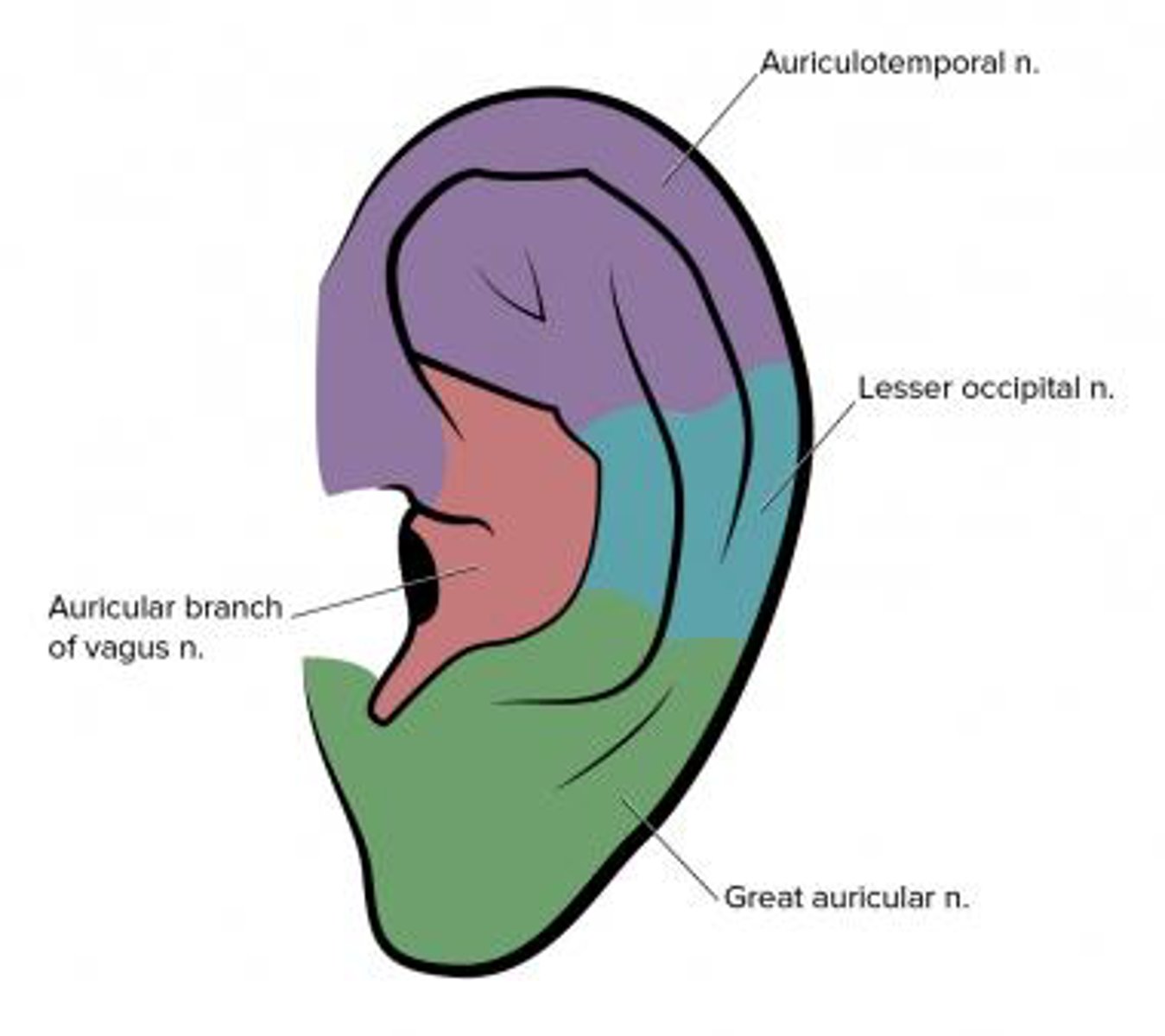
What nerve innervates the posterior auricle as well as skin overlying mastoid ?
GREAT AURICULAR NERVE C2,C3
think cervical spine pathology
- cervical spine degenerative disease: Osteoarthritis• Cervical facette disease• Spondylosis• Disc herniation• Spinal stenosis
- Whiplash (2%)• Cervical meningioma• Arnold-Chiari type I (1%)• Vascular (1%)• Fibromyalgia (1%)• Cervical nerve root cysts
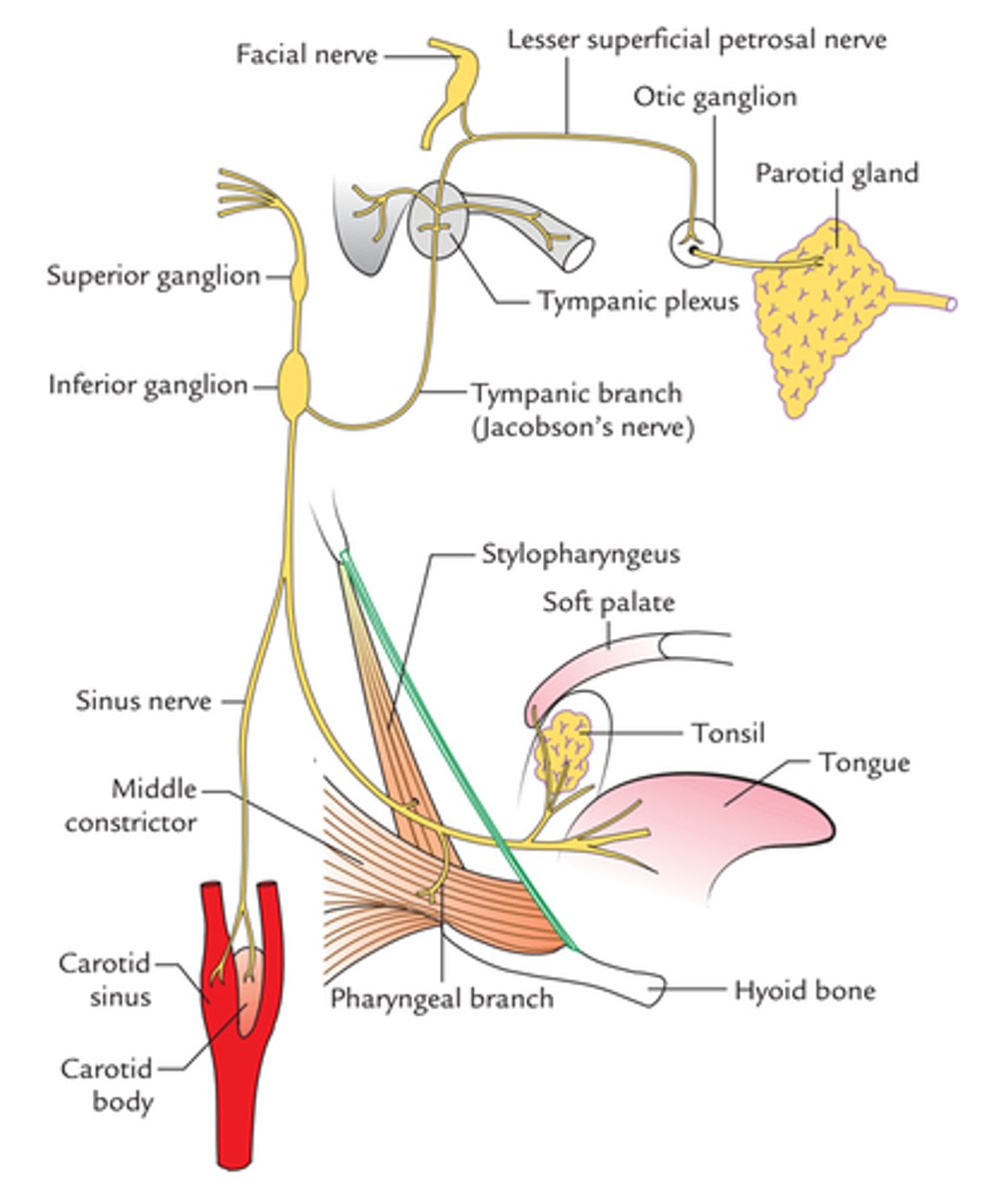
What nerve innervates Middle ear• Upper Eustachian tube• Medial surface of tympanic membrane?
TYMPANIC BRANCH OF GLOSSOPHARYNGEAL NERVE , and arises from the inferior ganglion of the glossopharyngeal nerve. It also carries preganglionic parasympathetic fibres, from the inferior salivary nucleus, which eventually enter the otic ganglion.
Pathology:
- sinusitis
- tonsilitis
- pharyngitis
- pharyngeal tumour
- glossopharyngeal neuroma
Innervates
Nasal cavity
Nasopharynx
Paranasal sinuses
Palatine tonsils
Tonsillar fossa
Soft palate
Oropharynx
Posterior one-third of tongue
Infratemporal fossa
Posterior auricular nerve
Branch of the seventh cranial nerve that affects the muscles behind the ear at the base of the skull
Branch of facial nerve
Innervates:
Posterior wall of external auditory canal
Posterior lateral surface of tympanic membrane Posterior skin of auricle
Pathology
RAMSAY HUNT SYNDROME
Vestibular Schwannoma
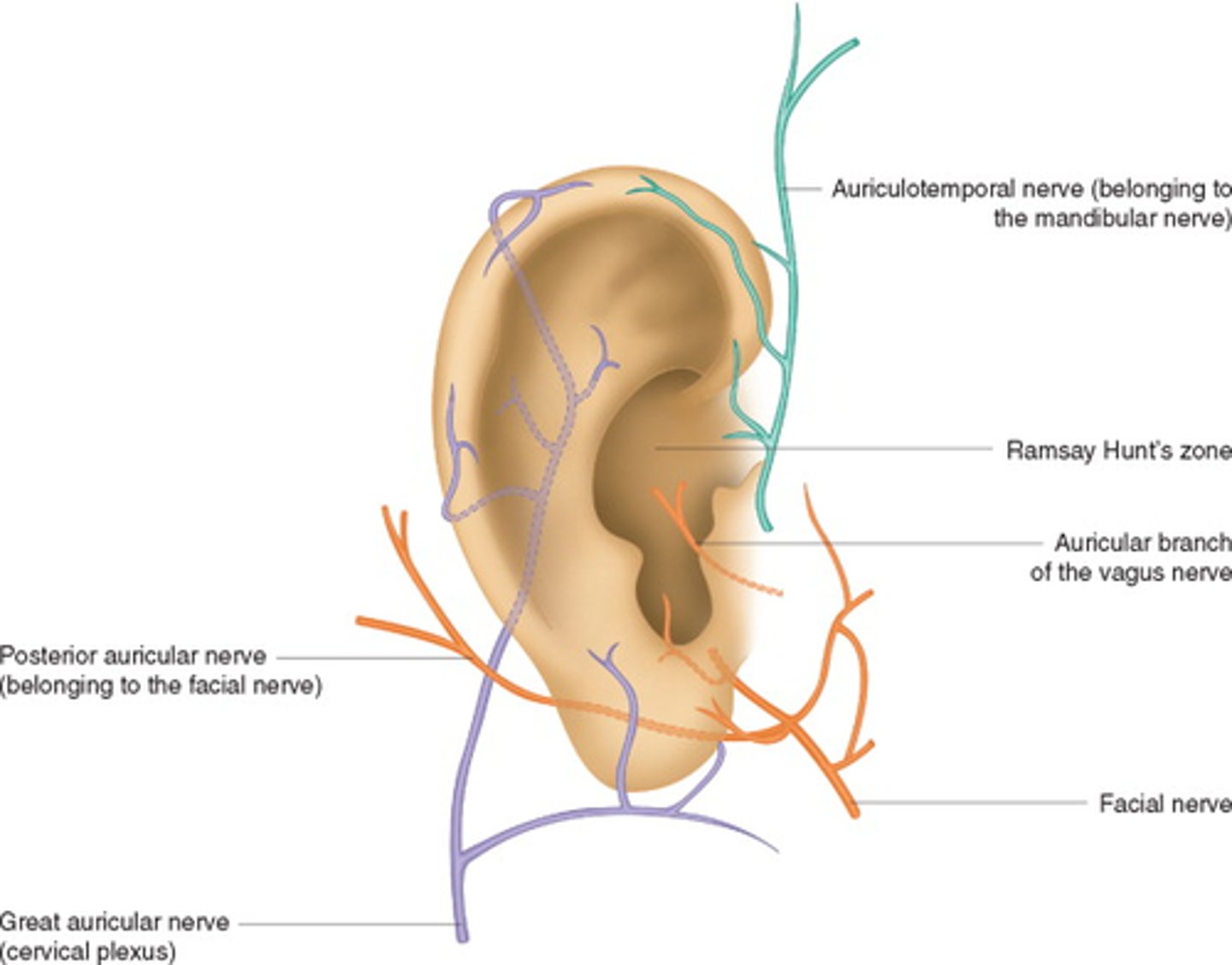
Auricular innervation