Unit 7: Constipation and Diarrhea
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
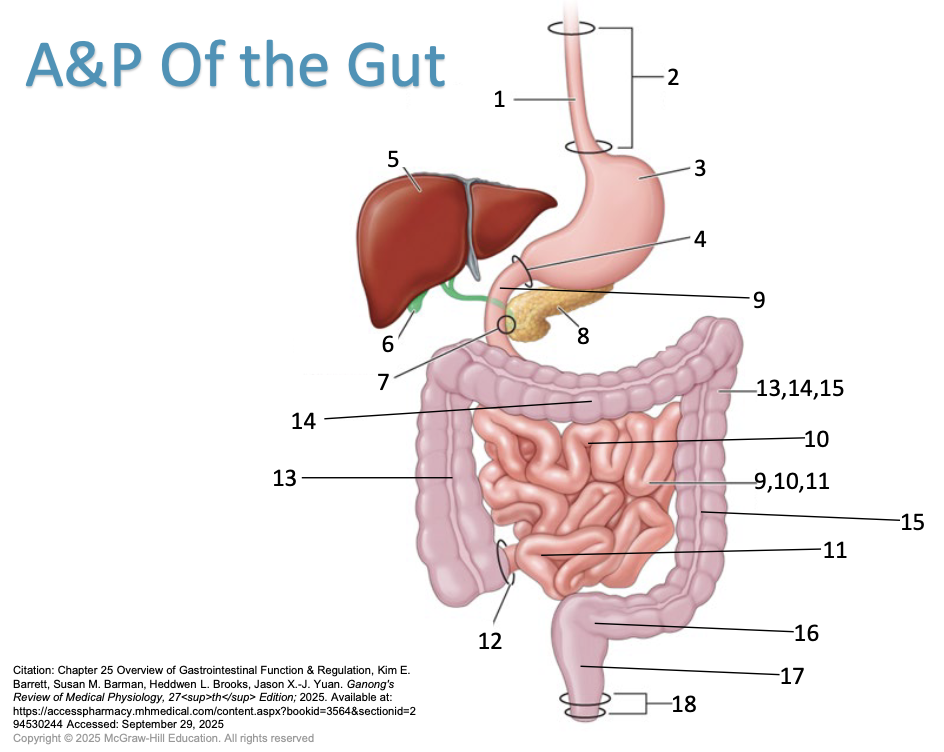
Describe the physiology associated with bowel transit.
Esophagus
Esophageal sphincters
Stomach
Pyloric sphincter - controls how much feed is let into the small intestines
Liver
Gallbladder
Sphincter of Oddi - Gallbladder enters into small intestines
Pancreas
Duodenum - Small intestines starts
9, 10, 11 - small intestines
Jejunum
Ileum
Ileocecal valve
13, 14, 15 - large intestines
Ascending colon
Traverse colon
Descending colon
Sigmoid colon (Pelvic colon)
Rectum
Anal sphincter
Timeline for digestion
0 hours - when you put food in your mouth
Esophagus: Takes 3 seconds to get from mouth to stomach
Stomach: food will hang out in stomach for 3-5 hours
Pyloric sphincter through small intestines to ileocecal valve: 4.5 hours
Ileocecal valve to ascending colon: another hour so 5.5 hours total now
Ascending colon to transverse colon: another hour so 6.5 hours total
Traverse colon to descending colon: another 3 hours so 9.5 hours total
Descending colon to sigmoid colon: could be another 2.5 to 14.5 hours for a total of 12-24 hours
How long does it take for food to get from the mouth to the small intestines?
6 hours
How long does food stay in the colon?
6-18 hours in the colon where stool is desiccated (water removed)
What is the purpose of the villi and where is it located?
lines the small intestines creating more surface area
villi are where we absorb more nutrients
What is the intrinsic innervation? (Physiology of bowel transit)
The intrinsic innervation of the gut is primarily carried out by the enteric nervous system (ENS); known as the “little brain”
It consists of two major networks of neurons called the myenteric (Auerbach's) plexus, located between the muscle layers and controlling gut motility, and the submucosal (Meissner's) plexus, found beneath the mucosa and involved in glandular secretion and monitoring the gut environment.
The ENS can function independently of the central nervous system, (can function without input from CNS)
What is the extrinsic innervation?
Extrinsic innervation of the gut refers to nerves originating outside the gastrointestinal (GI) tract that connect to and influence the gut's functions (autonomic nervous system).
These nerves, which include both sensory and motor fibers, transmit information from the gut to the central nervous system and provide signals from the brain to the gut via the vagus nerve (parasympathetic) and splanchnic nerves (sympathetic).
This communication helps regulate vital GI processes such as motility, secretion, and the detection of visceral pain, satiety, and nausea
What do the parasympathetic fibers do?
increase the activity of the intestinal smooth muscle and relax sphincters
What do the sympathetic fibers do?
decrease activity and cause sphincters to contract
What are the risk factors for constipation?
Women, older adults, inactivity, lower socioeconomic class, lower income, non-white race, symptoms of depression, history of physical or sexual abuse
What is the pathophysiology of constipation?
Primary (idiopathic): no identifiable cause
Categories:
normal transit or functional: most common type, Pts have normal GI motility and stool frequency, may experience signs/symptoms
slow transit: abnormality of the GI transit time
Dysfunction of the pelvic floor muscles
Pts may present with more than one type
Secondary: has an identifiable cause
What is the common clinical presentation of constipation?
Difficult or infrequent passage of stool
Straining or feeling of incomplete defecation
Decreased stool frequency
Chronic constipation: symptoms lasting for greater than or equal to 3 months
Estimated to be about 14% worldwide
Rome IV criteria:
At least 2 of the signs/symptoms apply to a minimum of 25% of BM:
Infrequent BM (<3 per week)
Stools that are hard, small, or dry
Difficulty or pain of defecation
Feeling of incomplete evacuation
Feeling of anorectal obstruction or blockage
Physical tactics needed for defecation
Loose stools are rarely occur without laxative use
1. Describe the role of nonpharmacologic strategies in the treatment of constipation (1d)
Diet
25-35 grams of fiber per day
whole grains, oats, fruits, vegetables
avoidance of constripating foods
processed cheese, concentrated sweets
adequate fluid intake
at least eight 8 ounce glasses of water per day
Physical Activity
increase exercise/activity level
Bowel Habits
do not ignore the urge to defecate
establish a regular pattern
allow adequate time
General emotional well being and avoidance of stressful situations
Identify drug classes used in the management of constipation. (2 general)
laxatives (bulk forming, saline, stimulant)
hyperosmotic agents
lubricant products
emollient agents (stool softeners)
Describe the mechanism of action for saline laxatives used for constipation.
MOA: create an osmotic gradient resulting in water being drawn into the lumen of the intestines and rectum, creating increased intraluminal pressure and stimulating peristalsis
Describe the mechanism of action for bulk forming laxatives used for constipation.
MOA: increased fiber intake, increases stool volume and may make stools softer
Describe the mechanism of action for stimulant laxatives used for constipation.
MOA: since these are old drugs, their MOA are not well understood
Appear to act locally by irritating the mucosa or stimulating the nerve plexus of the intestinal smooth muscle
May also stimulate secretion of water and electrolytes into the intestines
Describe the mechanism of action for hyperosmotic agents used for constipation.
MOA: create an osmotic gradient resulting in water being drawn into the lumen of the intestines and rectum, creating increased intraluminal pressure and stimulating peristalsis
Describe the mechanism of action for lubricant products used for constipation.
MOA: coats the stool and prevents reabsorption of fecal water. This results in a softer stool that is more easily eliminated
(used as enema in a hospital setting; other settings are not recommended)
Describe the mechanism of action for stool softeners used for constipation.
MOA: anionic surfactants that increase wetting efficiency (promote mixing of aqueous and fatty substances) so that intestinal fluid mixes with fecal material to create a softer fecal mass.
What is chronic constipation?
symptoms last at least 3 months or longer
estimated to be about 14% worldwide
1. Differentiate the timeframe of acute versus chronic diarrhea. (1c)
acute
last for less than 3 weeks
BM are fewer than 3 times per week
hard or dry stools
straining during BM
abdominal pain or bloating
caused by changes in diet, travel, dehydration, lack of exercise, certain meds
usually resolves within a few days or weeks
chronic
last for 3 months or longer
underlying medical condition: IBS, thyroid disorders, certain mediations; low fiber intake, sedentary lifestyle; ignoring the urge to defecate
symptoms similar to acute constipation but may be more persistent and accompanied by other symptoms such as fatigue, abdominal discomfort, or rectal bleeding
Bulk Forming Laxatives: ADRs and Onset of action?
ADRs: abdominal cramping and flatulence
12 to 72 hours
Hyperosmotic Agents: ADRs and Onset of Action?
ADRs: bloating, cramping, abdominal discomfort, flatulence, anal irritation due to leakage (suppositories)
Onset of action:
PEG 3350 & MiraLax 12 to 72 hours
Suppositories: 15 to 30 minutes
Saline Laxatives: ADRs and Onset of Action?
ADRs:
Bloating, cramping, abdominal discomfort, and flatulence
Diarrhea, dehydration, and related complications may occur, particularly with excessive use
Due to loss of electrolytes
Elevated magnesium levels, particularly in pts with kidney failure, infants and children, and older adults
Onset of Action:
oral - 30 minutes to 6 hours
enema - 2 to 15 minutes
Emollient Agents (Stool Softeners): ADRs and Onset of Action?
ADRs: diarrhea and mild cramping
onset of action: 12 to 72 hours but may be up to 5 days
Lubricant Products: ADRs and Onset of Action?
ADRs:
lipid pneumonia - of aspirated
Leakage of oil through anal sphincter
Absorption into intestinal mucosa, liver and spleen - foreign body reactions
onset of action:
oral - 6 to 8 hours
enema - 5 to 15 minutes
Stimulant Laxatives: ADRs and Onset of Action?
onset of action: generally 6 to 10 hours after oral use but may be up to 24 hours
Examples of bulk forming laxatives/efficacy
methylcellulose (meta-mucils), calcium polycarbophil, psyllium husk
work only in the gut (non-systemic product)
take with plenty of liquids to promote efficacy and prevent product swelling in throat or esophagus
separate other drugs and prevent absorption by separating by at least 2 hours
Examples of hyperosmotic agents
Polyethylene glycol 3350 )PEG 3350, MiraLax) - good recommendation (12 to 72 hour onset)
Glycerin Rectal Suppositories (occasional use; 15 to 30 minutes onset)
Examples of saline laxatives
Magnesium hydroxide (Milk of Magnesia) - liquid and tablets
Magnesium sulfate (epsom salts) - powder to be mixed in water or other liquid (do not use for laxative)
Magnesium citrate - 10 ounce bottles of liquid
Sodium phosphate salts - enemas (Fleet enema) - adult and pediatric products
onset: oral - 30 minutes to 6 hours; enema - 2 to 15 minutes
Examples of emollient agents (stool softeners)
docusate sodium (Colace); docusate calcium
these are not true laxatives because they do not stimulate a true BM
recommended to prevent stool straining and prevent painful defecation
onset: 12 to 72 hours but may take up to 5 days
drug interactions with emollient agents (stool softeners)
should not be used at the same time as mineral oil, as it can result in absorption of mineral oil from the GI tract
Examples of lubricant products
mineral oil (liquid), mineral oil (liquid emulsion), mineral oil (enema)
onset of action: oral 6 to 8 hours; enema 5 to 15 minutes
Drug interactions with lubricant products
reduced absorption of drugs and fat soluble vitamins A, D, E, K
Examples of stimulant laxatives (Bisacodyl)
Bisacodyl (Dulcolax):
Drug must be delivered to site of action in the colon
Suppositories - 10 mg, acts in 15 to 60 minutes
Enteric coated tablets - 5 and 10 mg
Rationale for enteric coated tablets
Tablet coating doesn’t dissolve in acidic environment of stomach, but does dissolve as the pH approaches neutral to alkaline in the small and large intestine
This allows bisacodyl to be delivered directly to the site of action
Severe ADRs may occur if administered with antacid products, H2-antagonists, or proton pump inhibitors. Elevated pH will allow enteric coating to dissolve and drug will be released in the upper portion of the GI tract.
Tablets cannot be crushed prior to administration
ADRs
Severe cramping, abdominal pain, diarrhea, fluid and electrolyte loss, intestinal protein loss
Example of stimulant laxative (Senna)
Available in a variety of oral products: tablets/pills, chocolate pieces, liquids
ADRs: melanosis coli - benign black pigment in the colon with prolonged use; may be seen in colonoscopy; discoloration of urine
example of stimulant laxative (castor oil)
(Do not recommend castor oil; there are safer and more effective options)
Stimulates small and large intestines
Do not want to stimulate small intestines because that is where medication is being absorbed
ADRs: severe cramping, nutrient loss, excessive fluid and electrolyte loss
What is an example of a combination product?
Senna and docusate: mush and push
Why do diuretic medications cause constipation?
decrease body water to decrease swelling
not enough water - stool becomes dry and hard
How do anticholinergic drugs cause constipation?
Block acetylcholine’s effect
acetylcholine is one of the primary neurotransmitters
acetylcholine primarily stimulates the gut
blocking acetylcholine will SLOW DOWN the gut
How do opioid medications cause constipation?
central stimulation of u-receptors - causes pain relief
stimulation SLOWS GI motility