Traumatic Brain Injury
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
Alteration in brain function, or other evidence of brain pathology, caused by an external force
Alteration in brain function, or other evidence of brain pathology, caused by an external force
leading cause of injury-related death and disability in the US
1.7 million people visit emergency departments for TBI annualy
50,000 people die as a result of the injury
300,000 require hospitalization
True incidence likely underestimated
does not include military, non-ED visits, or many sports-related injury
Prevalence of TBI
Falls – 32%
Motor vehicle/traffic accidents – 19%
Struck by/against events – 18%
Assaults – 10%
Leading Causes of TBI
Children (0–4 years) - Most common population affected.
Adolescents & young adults (<25 years)
Older adults (65+ years)
Hospitalization and death as a result of TBI is most common.
High-risk groups:
5.3 million people in the U.S. live with TBI-related disability.
1 year after injury:
40% not working
33% struggle with social integration
• 25% need help with ADLs
• ~40% report poor physical & mental health
Long Term Impact of TBI
Traumatic brain injury is a heterogenous injury, with a wide variety of pathophysiological mechanisms.
The brain damage results from external forces that cause brain tissue to make direct contact with an object (bony skull or penetrating object), rapid acceleration or deceleration forces, or blast waves from an explosion.
Mechanism of Injury and Pathophysiology
Primary Injury
Due to direct trauma to the parenchyma
Secondary Injury
Results from a cascade of biochemical, cellular, and molecular events that evolve over time due to the initial injury and injury-related hypoxia, edema, and elevated intracranial pressure (ICP).
Brain tissue damage can be categorized as follows:
Caused by direct trauma to brain tissue.
TBI: Primary Injury
Contact injuries (e.g., contusions, lacerations, hematomas)
Acceleration/deceleration injuries (e.g., diffuse axonal injury - DAI)
Main types of Primary Injury
Anterior temporal poles
Frontal poles
Lateral and inferior temporal cortices
Orbital frontal cortices.
Primary Injury: Common areas of focal injury
Diffuse axonal injury (DAI)
Predominant mechanism of injury in most individuals with severe to moderate TBI.
Parasagittal white matter of the cerebral cortex
Corpus callosum
Pontine-mesencephalic junction adjacent to the superior cerebellar peduncles.
Diffuse axonal injury (DAI): Often occurs in discrete areas:
False: Mechanism is microscopic, so often there are minimal initial findings on CT & MRI.
True/False: Diffuse axonal injuries are often obvious in initial findings on CT & MRI
Common in high-speed motor vehicle accidents (MVAs) and can be seen in some sports-related TBIs.
Common in high-speed motor vehicle accidents (MVAs) and can be seen in some sports- related TBIs.
Diffuse axonal injury (DAI) pathophysiology & MOI
Blast Injury
Signature injury of the U.S. military conflicts in the Middle East.
Brain Injury
When an explosive device detonates a transient shock wave is produced, which can cause brain damage.
Primary Blast Injury
Direct effect of blast overpressure on organs (in this case the brain).
Secondary Blast Injury
Shrapnel and other objects being hurled at the individual.
Tertiary Blast Injury
Occurs when the victim is flung backward and strikes an object.
Types of Blast Injuries:
Direct transcranial blast wave propagation.
Transfer of kinetic energy from the blast wave through the vasculature, which triggers pressure oscillations in the blood vessels leading to the brain.
Elevations in cerebrospinal fluid (CSF) or venous pressure caused by compression of the thorax and abdomen and by propagation of a shock wave through the blood vessels or CSF.
Three mechanisms by which primary blast brain injury may occur:
Occurs hours to days after initial trauma.
Secondary Injury
Hypoxia, hypotension, ischemia, edema,
↑ ICP
Secondary Injury: Triggered by?
Glutamate toxicity
Calcium influx
Free radical release
Inflammatory cytokines
Secondary Injury: Cellular-level changes include:
Brain swelling, hematoma, CSF imbalance
Elevated Intracranial Pressure (ICP) is caused by?
ICP: 5–20 cm H2O
Normal ICP
Brain herniation (uncal, central, tonsillar)
Requires emergency treatment
High ICP can lead to:
Cushing Triad
Altered level of consciousness
Headache
Vomiting
Papilledema
Behavioral Changes
Elevated Intracranial Pressure Clinical Features
Irregular breathing
Widened pulse pressure
Bradycardia
Cushing Triad
macrocephaly
bulging fontanels
sunset sign
Elevated intracranial Pressure Clinical features in infants
Impaired motor function:
Upper extremity (UE) and lower extremity (LE) paresis.
Impaired coordination
Impaired postural control
Abnormal tone
Abnormal gait
*may be present as life-long impairments.
Abnormal, involuntary movements (tremors, chorea and dystonic movements) are less common.
Patients may also present with impaired somatosensory function, depending on the location of the lesion.
Sequelae of Traumatic Brain Injury: Neuromuscular
Involves arousal, attention, concentration, memory, learning, and executive functions (Categories: planning, cognitive flexibility, initiation and self-generation, response inhibition, and serial ordering and sequencing).
Mainly controlled by the frontal lobes, making them vulnerable in TBI.
Altered levels of consciousness are commonly seen.
Disordered arousal states seen after severe brain injury:
Coma
Vegetative State
Minimally Conscious State
Sequelae of Traumatic Brain Injury: Cognitive
Cognition
The mental process of knowing and applying information.
The arousal system is not functioning.
The patient’s eyes are closed.
No sleep/wake cycles.
Patient is ventilator dependent.
No auditory or visual function.
No cognitive or communicative function.
Abnormal motor and postural reflexes may be present.
Usually not permanent.
Patients may become brain dead, enter a vegetative or minimally conscious state, or go onto full recovery.
Cognitive Impairments: Coma
Disassociation between wakefulness and awareness.
Higher CNS centers are not integrated with the brainstem.
patient can be weaned off the ventilator.
Present sleep/wake cycles.
Eyes may be open though awareness of surroundings is absent.
Patients may startle to visual or auditory stimuli and briefly orient to sound or visual stimuli.
Meaningful cognitive and communication function is absent.
Reflexive smiling/crying may be present.
A withdraw response to noxious stimuli is present.
Although patients in a vegetative state may appear to have purposeful movement, these movements are non purposeful and reflexive in response to external stimuli.
Patients in a permanent vegetative state may have no meaningful motor or cognitive function and a complete absence of awareness of self or the environment for period greater than 1 year after TBI and greater than 3 months after anoxic brain injury.
Cognitive Impairments: Vegetative State
There is minimal evidence of self or environmental awareness.
Cognitively mediated behaviors occur inconsistently and are reproducible or sustained such that they can be differentiated from reflexive behaviors.
Present sleep/wake cycles.
Patients can localize to noxious stimuli, inconsistently reach for objects, may localize to sound location and demonstrate sustained visual fixation and visual pursuit.
Cognitive Impairments: Minimally Conscious State
an unresponsive state from which the patient can be aroused only briefly with vigorous, repeated sensory stimulation.
Cognitive Impairments: Stupor
the patient sleeps often and when aroused exhibits decreased alertness and interest in the environment and delayed reactions.
Cognitive Impairments: Obtunded
Patients can exhibit profound behavioral changes as they progress through recovery.
These impairments can be closely linked to cognitive impairments and are often more debilitating in the long run than physical disability.
Common behavioral sequelae:
Low frustration tolerance
Agitation
Disinhibition
Apathy
Emotional lability
Mental inflexibility
Aggression
Impulsivity
Irritability
Sequelae of Traumatic Brain Injury: Neurobehavioral
Language and communication deficits after brain injury are generally non-aphasic in nature and are related to cognitive impairment.
Common language and communication deficits include disorganized and tangential oral or written communication, imprecise language, word retrieval difficulties, and disinhibited and socially inappropriate language.
Patients may also exhibit difficulties communicating in distracting environments, reading social cues, and adjusting communication to meet the demands of the situation.
These communication deficits can affect employability, social integration, and quality of life.
Sequelae of Traumatic Brain Injury: Communciation
Paroxysmal Sympathetic Hyperactivity (PSH)
These episodes are paroxysmal, meaning they occur suddenly and unpredictably, and are usually triggered by external stimuli (like pain, suctioning, or repositioning).
is a clinical syndrome often seen after severe traumatic brain injury (TBI). It is characterized by sudden, episodic increases in sympathetic nervous system activity.
Tachycardia
Hypertension
Hyperthermia
Tachypnea
Sweating
Posturing
Key Features of Paroxysmal Sympathetic Hyperactivity (PSH)
Typically results from disruption of brain pathways that regulate the autonomic nervous system, especially following diffuse axonal injury or severe cortical/subcortical trauma.
It involves an imbalance between excitatory and inhibitory control of the sympathetic system.
Paroxysmal Sympathetic Hyperactivity (PSH): Causes and Pathophysiology:
Reducing external stimuli
Medications: beta-blockers, opioids, benzodiazepines, and others to control symptoms
Supportive care and close monitoring.
Paroxysmal Sympathetic Hyperactivity (PSH): Management
Seen in 12% and 50% of people with severe TBI.
Phenytoin (an anticonvulsant) is effective in decreasing the risk of early post-traumatic seizures.
Post-traumatic Seizures
DVT
Heterotropic ossification
Pressure olcer
Pneumonia
Chronic pain
Contractures
Decreased endurance
Muscle atrophy
Fracture
Peripheral nerve damage
Secondary Impairments and Medical Complications
Glasgow Coma Scale
The most widely used clinical scale that measures level of consciousness and helps define and classify the severity of injury.
Motor Response (6pts)
Verbal Response (5pts)
Eye Opening (4pts)
GCS is comprised of three response scores
• Mild: 13 to 15
• Moderate: 9 to 12
• Severe: ≤ 8
The scores from the separate responses are summed to provide a score between 3 and 15.
GCS Scoring
Mild TBI | |
LOC | 0-30 mins |
AOC | brief >24 hours |
PTA | 0-1 day |
GCS | 13-15 |
Neuroimaging | normal |
Characteristics of Mild TBI: LOC, AOC, PTA, GCS, Neuroimaging
Moderate TBI | |
LOC | >30 min and <24 hr |
AOC | >24 hours |
PTA | >1 and <7 days |
GCS | 9-12 |
Neuroimaging | normal or abnormal |
Characteristics of Moderate TBI: LOC, AOC, PTA, GCS, Neuroimaging
Severe TBI | |
LOC | >24 hours |
AOC | >24 hours |
PTA | >7 days |
GCS | <9 |
Neuroimaging | normal or abnormal |
Characteristics of Severe TBI: LOC, AOC, PTA, GCS, Neuroimaging
Factors that can be useful in estimating future outcomes:
Low initial scores on the GCS, particularly motor score and pupillary reactivity, have been identified as a predictor of poor recovery in patients with moderate to severe TBI.
Other factors associated with poor outcomes are age, race, and lower education level.
Petechial hemorrhages, subarachnoid bleed, obliteration of 3rd ventricle or basal cisterns, midline shift, and subdural hematoma findings on initial CT scan are also predictive of poor outcomes.
The Medical Research Council (MRC) CRASH (corticosteroid randomization after significant head injury) study
provides a Web-based calculator that allows clinicians to enter demographic and prognostic information and calculate the 14-day mortality risk and unfavorable outcome at 6 months, along with the 95% confidence interval.
Post-Traumatic Amnesia
Time between injury and consistent memory of ongoing events
Likely to be living without assistance.
PTA outcomes: <53 days
Higher Functional Independence Measure (FIM) scores at discharge from inpatient rehabilitation.
PTA outcomes: <48.5 days
Likely to have a good overall recovery (as measured by the GOS).
PTA outcomes:<34 days
Likely to be employed.
PTA outcomes:<27 days
Ensure patient is medically stable before contact.
Identify:
ICP monitoring
Ventilator status
ROM & weight-bearing precautions
Musculoskeletal injuries or open wounds
Understand contraindications and precautions.
Patient Examination: Step 1 medical Record
Patients in coma, vegetative, or minimally conscious states may exhibit:
Abnormal tone (e.g., spastic hypertonia)
Primitive postures:
Decorticate rigidity
Decerebrate rigidity
Patient Examination: Severe TBI
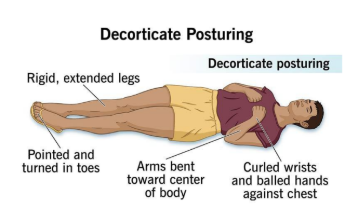
UE flexion, LE extension
Decorticate rigidity
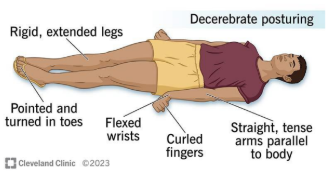
UE and LE Extension
Decerebrate rigidity
No Response
patient appears to be in deep sleep and is completely unresponsive to any stimuli
Rancho Los Amigos Levels of cognitive Functioning: I
Generalized Response
patient reacts to inconsistently and nonpurposefuly to stimuli in a nonspecific manner
responses are limited and often the same regardless of stimulus presented
responses may be physiological changes, gross body movements, and/or vocalization
Rancho Los Amigos Levels of cognitive Functioning: II
Localized Response
patient reacts specifically but inconsistently to stimuli
responses are directly related to the type of stimulus presented
may follow simple commands such as closing eyes or squeezing hand in an inconsistent, delayed manner
Rancho Los Amigos Levels of cognitive Functioning: III
Confused-Agitated
patient is in a heightened state of activity
behavior is bizzarre and nonpurposeful relative to immediate environment
Does not discriminate among persons or objects; is unable to cooperate directly with treatment efforts
Verbalizations frequently are incoherent and/or inappropriate to the environment; confabulation may be present
Gross attention to environment is very brief; selective attention is often nonexistent
patient lacks short and long-term recall
Rancho Los Amigos Levels of cognitive Functioning: IV
Confused-Inappropriate
patient is able to respond to simple commands fairly consistently
However, with increased complexity of commands or lack of any external structure, responses are nonpurposeful, random, or fragmented
Demonstrates gross attention to the environment but is highly distractible and lacks ability to focus attention on a specific task
With structure, may be able to converse on a social automatic level for short periods of time
Verbalization is often inappropriate and confabulatory
Memory is severely impaired; of often shows inappropriate use of objects; may perform previously learned tasks with structure but is unable to learn new information
Rancho Los Amigos Levels of cognitive Functioning: V
Confused-Appropriate
patient shows goal-directed behavior but is dependent on external input or direction
follows simple directions consistently and shows carryover for relearned tasks such as self-care
Responses may be incorrect due to memory problems, but they are appropriate to the situation
Past memories show more depth and detail than recent memory
Rancho Los Amigos Levels of cognitive Functioning: VI
Automatic Appropriate
patient appears appropriate and oriented within the hospital and home settings
goes through routine automatically, but frequently robot-like
Patient shows minimal to no confusion and has shallow recall of activities
Shows carryover for new learning but at a decreased rate
With structure is able to initiate social or recreational activities; judgement remains impaired
Rancho Los Amigos Levels of cognitive Functioning: VII
Purposeful-Appropriate
patient is able to recall and integrate past and recent events and is aware of and responsive to environment
Shows carryover for new learning and needs no supervision once activities are learned
May continue to show a decreased ability relative to premorbid abilities, abstract reasoning, tolerance for stress, and judgement in emergencies or unusual circumstances
Rancho Los Amigos Levels of cognitive Functioning: VIII

Basilar skull fracture following head trauma
Battle sign and racoon eyes are both late signs of?