Clinical Oncology - Leukemias and Lymphomas
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
What are the major lymph nodes involved in lymphomas?
1. Waldeyer Ring: nasopharynx, oropharynx, cervical, preauricular, occipital
2. Supra and infraclavicular
3. Axillary
4. Thorax: hilar and mediastinal
5. Abdominal: para-aortic
6. Pelvic cavity: iliac and Peyer patches
7. Inguinal and femoral
Where do B and T cells develop and mature?
B and T cells develop in bone marrow and mature in lymphatic organs
What age group is Hodgkin lymphoma more common in?
20 to 34 years old, and < 17 years old
What gender is Hodgkin lymphoma more common in?
Males
What race is Hodgkin lymphoma more common in?
White and black people have a higher incidence
Is Hodgkin or non-Hodgkin lymphoma more common?
Non-Hodgkin (80% of all lymphomas)
What is the etiology of Hodgkin lymphoma?
Largely unknown
Family history, Epstein-Barr (Reed-Sternberg), HIV
What is the clinical presentation of Hodgkin lymphoma?
Most common is painless lymphadenopathy and is often asymptomatic
What is common in extensive disease of lymphoma?
B-symptoms:
Unexpected weight loss of > 10% of body weight in 6 months
Night sweats
Fevers
What is the clinical presentation of advanced lymphoma?
Enlarged spleen, tender abdomen, pleural effusion, achy bones
What is the hallmark of Hodgkin lymphoma?
Reed-Sternberg, which is a large lymphoid cell with multiple nuclei
What are the most common pathologies of Hodgkin lymphoma?
Classical HL (95%) and nodular lymphocyte (5%)
What are the most common subtypes of classical HL?
Nodular scleorsing (80%) and mixed cellularity (15%)
Describe the natural history of Hodgkin lymphoma
Most often arises above diaphragm
Continuous and predictable spread (cervical > supraclavicular > mediastinal)
What staging system is used for lymphoma?
Ann Arbor System
A - no B symptoms
B - B symptoms
E - extranodal disease
S - spleen involvment
What is a prognostic indicator for lymphoma?
Bulky disease, mass > 10 cm
What is the treatment for Hodgkin lymphoma?
Chemotherapy (primary; for stage I and II) and adjuvant RT (stage III and IV) to treat subclinical or residual disease
What chemotherapy drugs are used in Hodgkin lymphoma?
4 cycles of ABVD (Adriamycin), can use MOPD instead due to risk of heart damage from Adriamycin
What are mantle fields used to treat?
Cervical, submandibular, axillary, supraclavicular, mediastinal and hilar lymph nodes
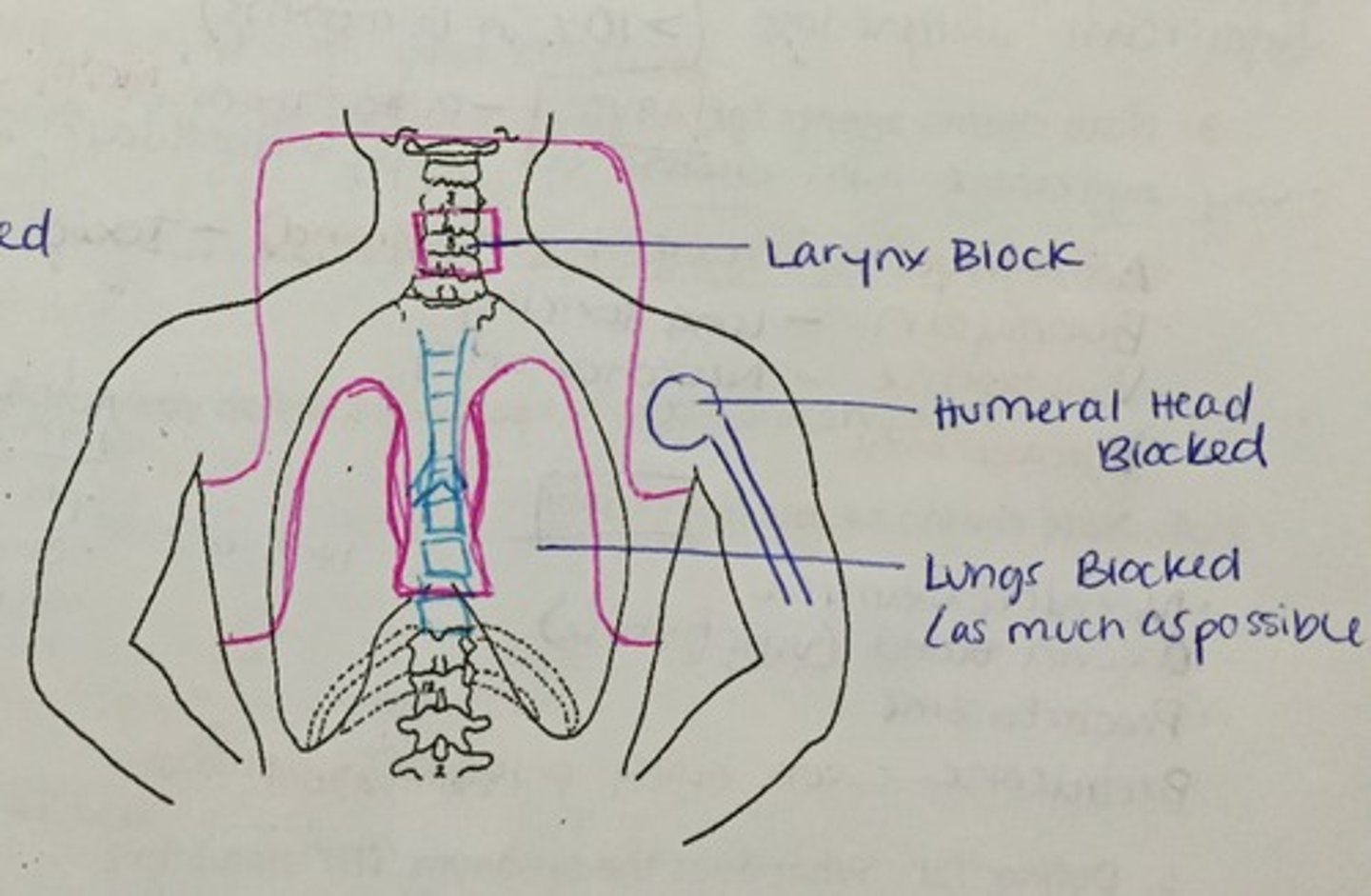
Describe the mantle field technique and simulation
Large field size with AP/PA
Supine, hands above head and akimbo position, chin extended
May use body molds to decrease movement
What are the field borders for mantle field?
Superior: below mandible and mastoid tips
Inferior: T9 to T10
Lateral: flash above axillary nodes
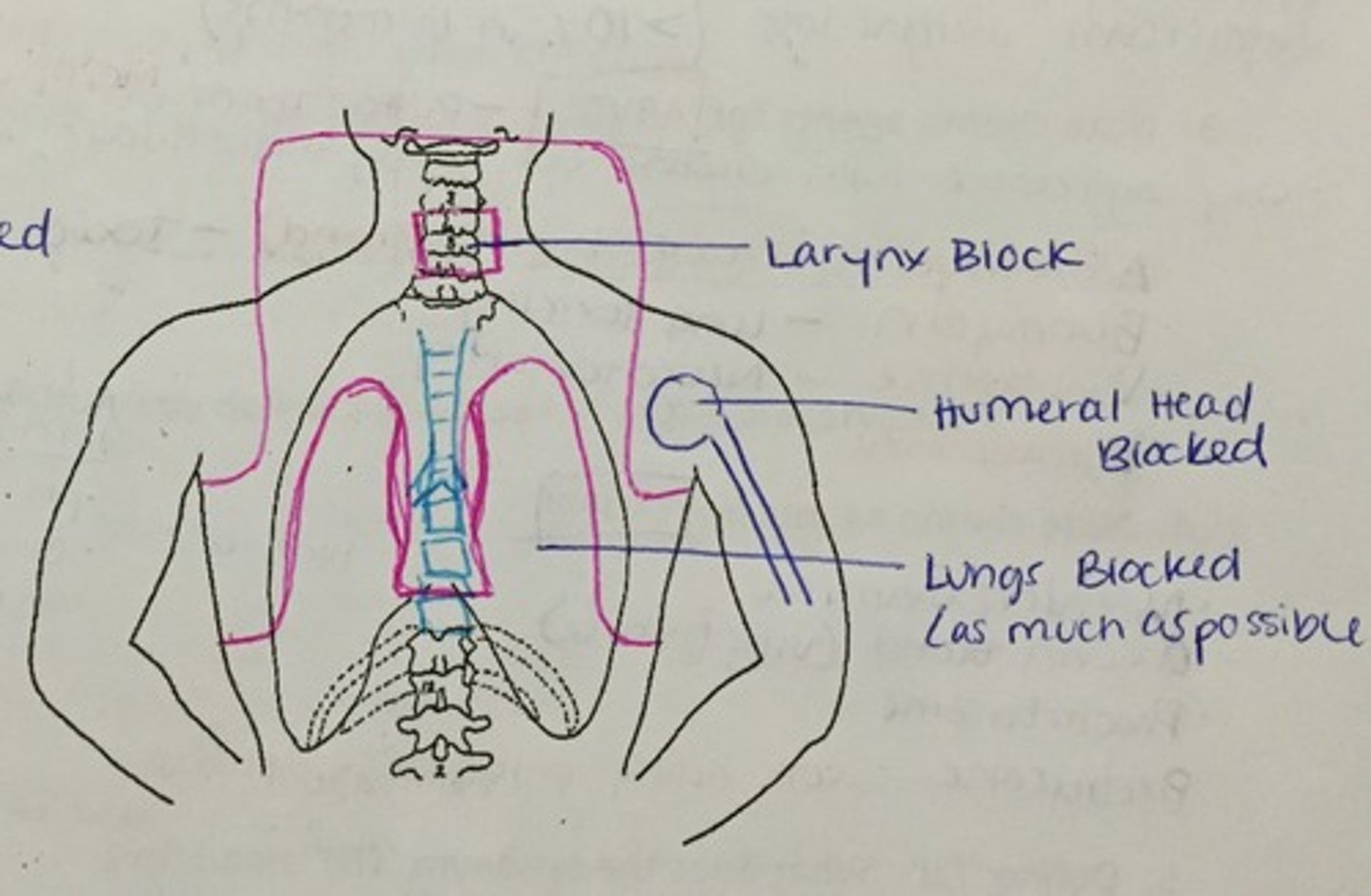
What is the inverted Y?
Pelvis and para-aortic
What is an involved field radiation?
Only encompass areas of known disease
What is an extended field?
Areas of known disease and contiguous uninvolved lymph nodes
What if chemotherapy and RT fail?
Autologous bone marrow or blood stem cell transplant
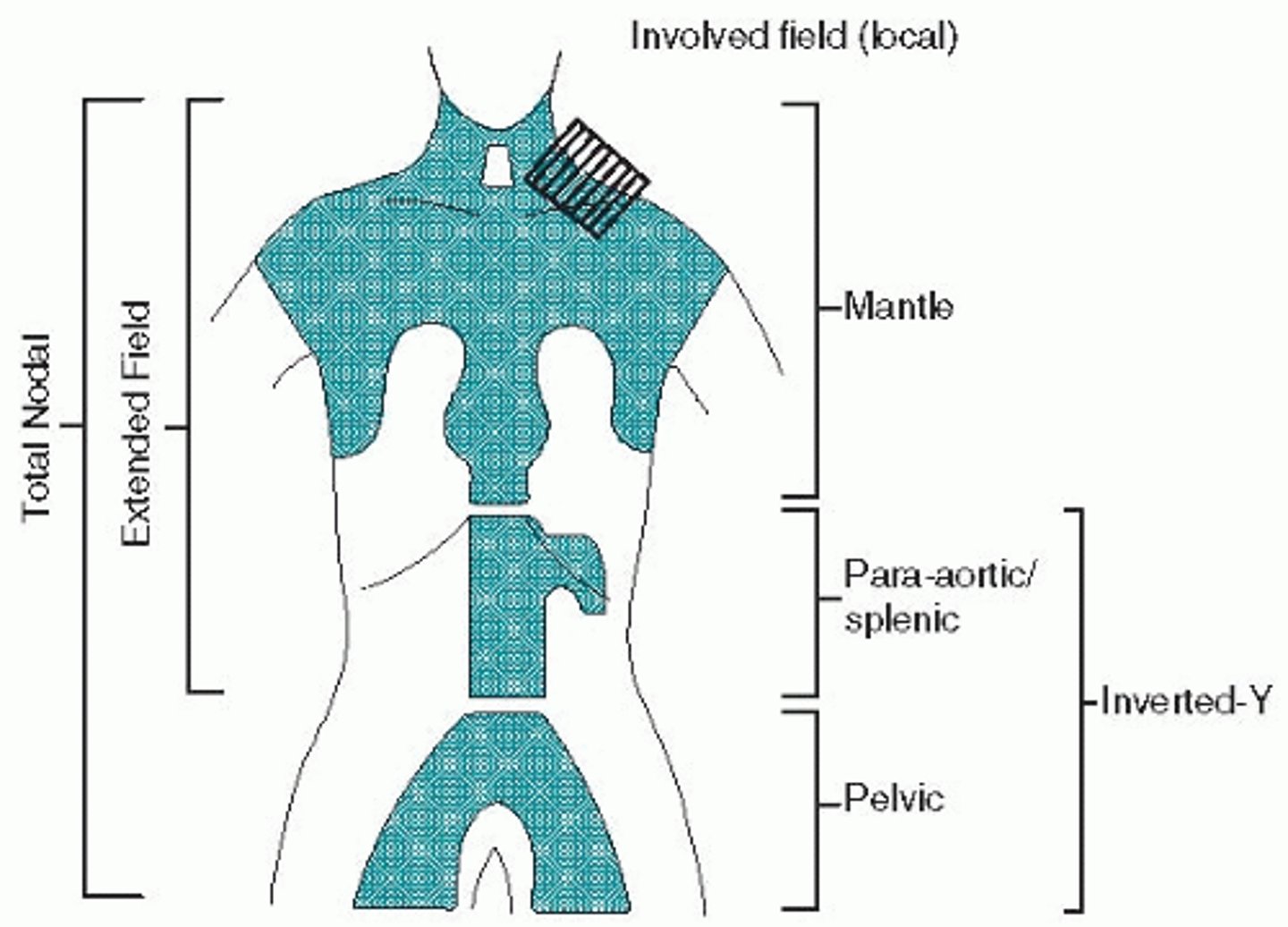
What is the abdominal/para-aortic field used to treatment in lymphoma?
Spleen, para-aortic and retroperitoneal nodes
Describe the treatment technique for the abdominal/para-aortic field
AP/PA field
What needs to be shielded with the abdominal/para-aortic field?
Spine and kidneys
Describe the field borders for the abdominal/para-aortic field
Superior: mid T10-T11
Inferior: L4-L5
Lateral: 9 to 10 cm wide
Describe the treatment technique for the pelvic field for lymphoma
AP/PA field with shielding of bone marrow, bowel and bladder - could be shielding for fertility
Describe the field borders for the pelvic field for lymphoma
Superior: L5
Inferior: 2 cm below ischial tuberosity
Lateral: 2 cm from pelvic inlet
What dose is used for RT for Hodgkin lymphoma?
35 to 44 Gy for RT alone
20 Gy for chemo + RT
What age group is Non-Hodgkin lymphoma more common in?
65 to 74 years old, median age at 67 years old
What gender is Non-Hodgkin lymphoma more common in?
Males
What is the etiology of Non-Hodgkin lymphoma?
Largely unknown
Immunosuppression, viruses (Epstein-Barr, HIV/AIDS, Hep. C, HTVL-1), radiation, chemotherapy
What is the most common site for extranodal disease in Non-Hodgkin lymphoma?
GI system (stomach)
What is the natural history of Non-Hodgkin lymphoma?
Lymphatic spread is not contiguous or predictable
What are the two groups of Non-Hodgkin lymphoma?
B-cell (diffuse large B-cell) (85%)
T-cell and cutaneous T-cell (15%)
*Non-Hodgkin lymphoma can be indolent or aggressive, and indolent can change to aggressive within 2 years after treatment. Not all cells make transition - diagnosed with both indolent and aggressive.
What is the treatment for indolent and early stage (I and II) Non-Hodgkin lymphoma?
Radiation alone
What is the treatment for aggressive Non-Hodgkin lymphoma?
Chemotherapy + RT
What dose is used for Non-Hodgkin lymphoma?
35 to 44 Gy to involved site and related drainage
What is the clinical presentation of leukemia?
Fatigue
Bruise easily
Bleed easily
Consistent infections that are hard to clear
*RBC, WBC, and platelets are low
What is the most common leukemia in children?
Acute lymphocytic leukemia (ALL)
What is the most common leukemia in adults?
Chronic lymphocytic leukemia (CLL)
What is the etiology of acute lymphocytic leukemia (ALL)?
Radiation, benzene, HTVL-1
What treatment is available for acute lymphocytic leukemia?
Chemotherapy
TBI
Targeted therapy for Philadelphia chromosome
Describe acute myeloid leukemia (AML)
Age: 68 years old
Etiology: radiation, benzene, smoking
Treatment: chemotherapy
*Worse prognosis than ALL as patients are older and may not tolerate chemotherapy toxicities
What is the clinical presentation for chronic lymphocytic leukemia (CLL)?
Asymptomatic until spread to LNs, spleen, liver
What is the etiology for chronic lymphocytic leukemia?
Agent orange, age, family history
What is the treatment for chronic lymphocytic leukemia?
Chemotherapy, TBI, rituxamab
What is the average age of diagnosis for chronic myeloid leukemia (CML)?
64 tears old
What is involved in detection of chronic myeloid leukemia (CML)?
Usually found incidentally
Need genetic testing for Philadelphia chromosome and BCR-ABL gene (mutation of myeloid cell) for diagnosis
What is the treatment for chronic myeloid leukemia?
Chemotherapy and targeted therapy (tyrosine-kinase inhibitor taken for rest of patient's life)