Cardiology Unit
1/185
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
186 Terms
How does the blood move through the heart?
superior vena cava —> right atrium —> tricuspid valve —> right ventricle —> pulmonary valve (semilunar valve) —> pulmonary artery —> lungs —> pulmonary veins —> left atrium —> mitral/bicuspid valve —> left ventricle —> aortic valve (SL valve) —> aorta —> the body.
arteries
away from the heart = does not mean only oxygenated blood
vein
toward the heart = does not mean only deoxygenated blood
how does blood oxygen occur/the pathway?
oxygenated blood through the aorta/artery —> arteriole —> capillaries (where O2 exchange happens) —> venule (deoxygenated) —> vein cava vein
how does blood flow through the body?
gradients
what types of gradients are in neurophysiology?
electrochemical gradients
what types of gradients are in cardiovascular?
pressure gradients
what types of pressure are in the aorta and vena cava?
aorta = highest pressure
vena cava = lowest pressure
it’s how/why blood flows from aorta (oxygenated) to vena cava (deoxygenated)
what part has the largest pressure drop?
arterioles have the highest pressure drop b/c they have the highest resistance to blood flow due to their small diameter (decreased SA = increased flow)
what is the equation for flow (Q)
Q = change in pressure / resistance (R)
how is the magnitude of Q determined?
Determined by the size of the pressure difference (change in pressure)
how is the direction of Q determined?
determined by the pressure gradient (high to low)
what is poiseuille’s law?
Resistance = (8nl)/(pir4)
what do each of the variables in poiseuille’s law mean?
R = resistance
n = viscosity of blood (constant)
l = length of blood vessel (constant)
r4 = radius of blood vessel raised to the fourth power
what is the shortened version of poiseuille’s law/resistance?
R = 1/r4
when is viscosity relevant in determining resistance?
change in volume (such as dehydration)
change in # of cells (such as polycythemia)
how does dehydration (change in volume) effect viscosity and resistance?
decrease in water = decrease in plasma
decrease in plasma —> increase in blood viscosity —> thicker blood —> increased resistance —> decreased flow
how does polycythemia (change in # of cells) effect viscosity and resistance?
decrease in water = decrease in plasma
decrease in plasma —> increase in blood viscosity —> thicker blood —> increased resistance —> decreased flow
when is length relevant in determining resistance?
always constant
unless there is an amputation of blood vessel
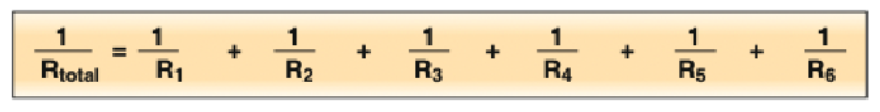
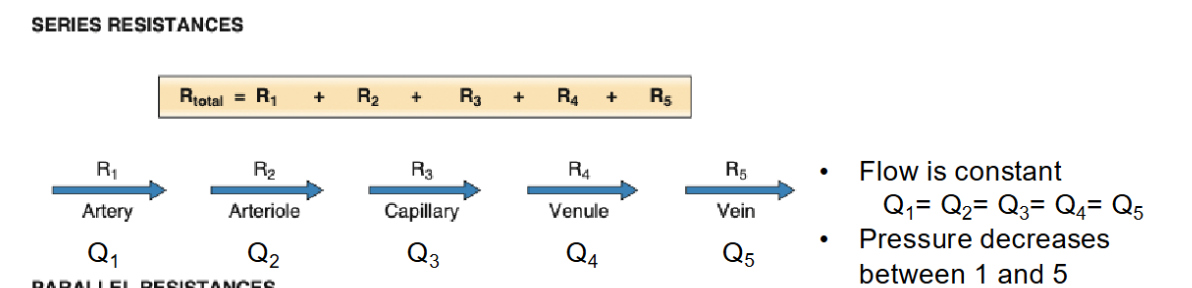
vessels in series
Rtotal = RA+Ra+Rc+Rc+Rv+RV
have to go sequentially through each category
vessels in parallel
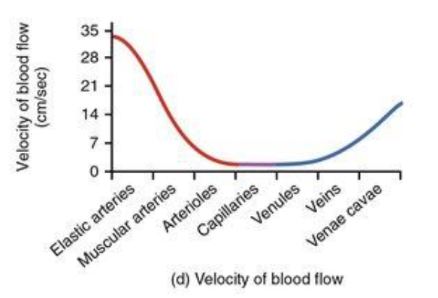
what is velocity (v)?
distance a given fluid moves within a unit of time (cm/sec)
how fast per time
rate of blood flow
what is flow (Q)?
quantity of a given fluid that passes by a certain point within a unit of time (mL/sec)
how much per time
when is flow preserved?
when the arteries/veins are in series —> blood is preserved should not change
what is the equation for velocity?
v = Q/A
what do the variables for velocity stand for?
v = velocity of blood flow (cm/sec)
Q = flow (mL/sec)
A = cross-sectional area (cm2) = total cross sectional area
what is the vessel diameter range?
capillaries have the lowest, arteries and venae cavae are the highest
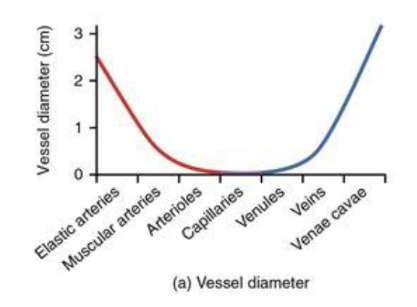
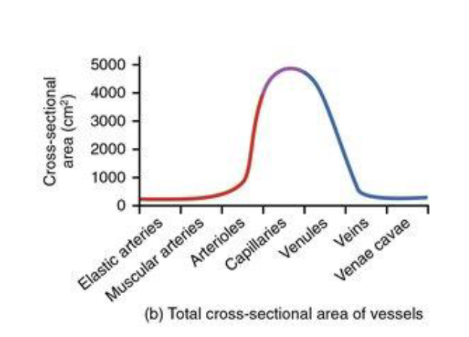
what is the total cross-sectional area of vessels range?
capillaries have the highest because it’s not individual, instead based on the cross-sectional area of all capillaries added together
what is the velocity of blood flows range?
the arteries have the highest velocity, the capillaries have the lowest velocity
higher total SA = slower
ICLICKER: radius plays the greatest role in determining resistance because…
correct: radius can be regulated —> when your being chased the blood gets rerouted
correct: length and viscosity are constants —> equation
correct: radius factors in the equation to the 4th power —> equation
when is flow constant?
when resistance is in series
pressure will still decrease between 1 and 5
what happens with parallel resistances?
they have the same pressure difference
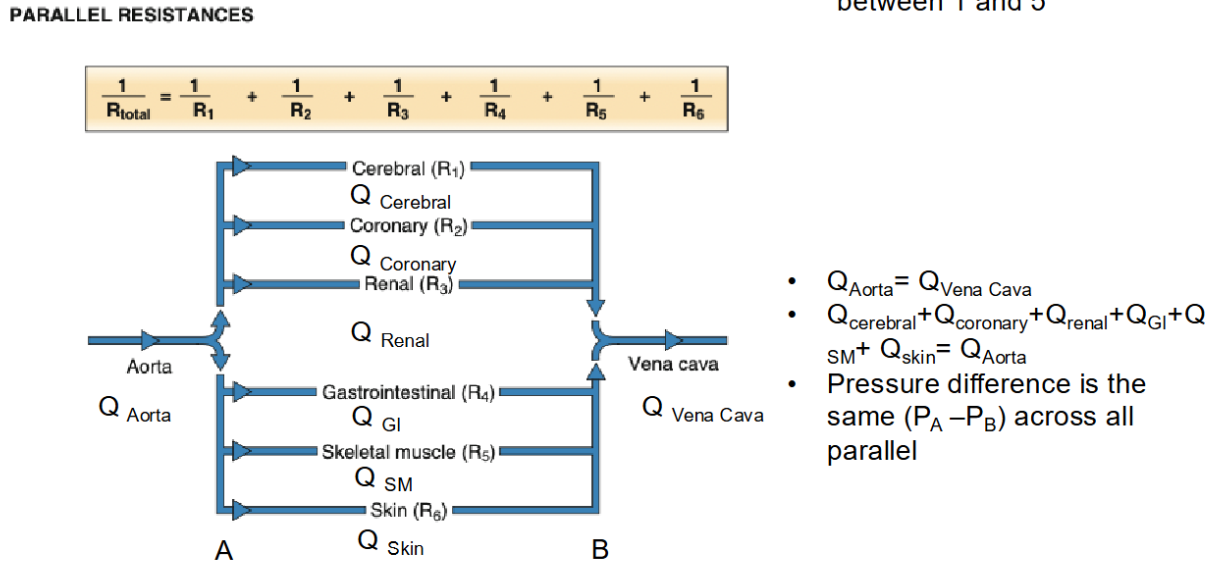
what is true about pressure for in parallel?
Arteriole 1 P3-P4 = Arteriole 10 P3-P4
what is true about pressure for in series?
Change in P3-P4 is NOT EQUAL to P2-P3
ICLICKER: are left and right sides of heart in series or in parallel?
correct: series
incorrect: parallel
incorrect: impossible to tell
everything needs to go into the right side of the heart to get into the lungs and so forth —> IN SERIES
as fluid moves through the branching system of pipes, what happens to the flow rate?
flow is constant because they are in parallel so the change in pressure is the same
as fluid moves through the branching system of pipes, what happens to the velocity of flow?
v=Q/A
don’t know how A changes
ICLICKER: which are true of flow and velocity of flow in the cardiovascular system?
correct: flow remains constant from aorta to capillaries
only the flow within the aorta is not constant = in parallel
in series = constant
correct: velocity is inversely proportional to total cross-sectional area
v=Q/A
correct: velocity of flow is lowest in the capillaries
we want a lot of exchange for oxygen
ICLICKER: a large artery branches into two arterioles. arteriole A is 2x longer than arteriole B, but the radius of arteriole B is ½ that of arteriole A. which arteriole offers less resistance to flow? explain using poiseuille’s equation.
WORK IT OUT
which has less resistance: A
ICLICKER: Suppose one dilates and the other constricts. what happens to flow in each arteriole?
WORK IT OUT
increases in A, decreases in B
is it in parallel or in series?
does all the blood need to go through A to go through B
no b/c they’re not connected in that way —> they’re parallel
if in parallel —> their pressure drop is the same
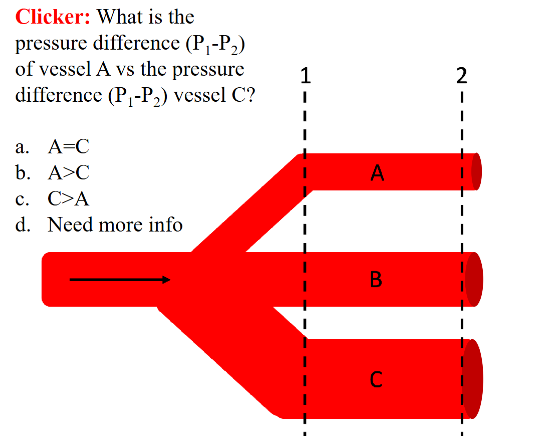
ICLICKER: what is the pressure difference (P1-P2) of vessel A vs the pressure difference (P1-P2) vessel C?
vessels are in parallel —> pressure drop is the same
A=C
how does asthma affect your airways?
for an asthmatic airway: decrease radius —> increase resistance = decrease of flow
what consistent of muscle cells?
contractile cells (99%)
conducting (1%)
what do contractile cells do?
produce force and contraction
what does conducting cells consist of?
autorhythmic cells
SA node
AV node
bundle of His
purkinje fibers
conducting fibers
internodal fibers
R and L bundle branch
conduct action potentials and/or initiate action potentials
what location is followed by the rhythm of the fastest node?
the sinoatrial node (SA node)
location of the nodes
sinoatrial node (SA node) = 70-80 impulses/min
atrioventricular node (AV node) = 40-60 impulses/min
bundle of His = 40 impulses/min
purkinje fibers = 15-20 impulses/min
how do pacemaker and contractile cells compare?
pacemaker cells = conduct action potentials and/or initiate action potentials
contractile cells = produce force and contraction
ICLICKER: pacemaker cells are BLANK in origin
muscle cells
muscles cells that have electrical properties
pacemaker cells
does NOT have a true RMP
have a calcium ion action potential
If channels open at -60 mV
contractile cells
have a RMP —> -90 mV
spread signals via gap junctions
have a plateau —> K+ leave is equal to Ca2+ coming in
what are funny channels?
non-specific, can let in Na+ and K+, but hey favor Na+
Can be activated when the cell’s hyperpolarize
activated at -60 mV hyperpolarized-activated
If can produde a signal w/o a stimulus for pacemaker cells
Important parts of the pacemaker cell figure:
If channels are activated at -60mV - hyperpolarized-activated.
when If channels open, increase permeability of BOTH Na+ and K+
However, Na+ going in the cell is greater than K+ going out of the cell (Na+ into the cell > K+ out of the cell).
At -50mV, T Type Ca2+ channels activated
At -40mV, voltage gated Ca2+ channels activated called L Type Ca2+ channels.
T type Ca2+ channels
activated at -50 mV
only activate during this time
role = help the funny channel out in bringing the membrane potential more positive —> easier to achieve the threshold faster.
L type Ca2+ channels
voltage-gated Ca2+ channels
activated at -40 mV
all pacemakers have ______ properties
similar
pacemakers are origin of ______ heartbeat
myogenic
SA node sets the pace because
it is the node w/ the fastest rhythm
if a pacemaker other than the SA node is setting the pace, then…
it is an ectopic pacemaker
the SA node is likely damaged
this is when you know something is wrong
contractile myocardium mV graph
threshold for v-gated Na+ channels = -60 mV
threshold for v-gated L type Ca2+ channel = -40 mV
threshold for V-gated K+ channels = -20 mV
what is the RMP of contractile myocardium?
-90 mV
what is the reasoning behind the plateau of the contractile myocardium cell?
the amount of K+ going out of the cell is balanced by the amount of Ca2+ coming into the cell
which cell has an absolute and relative refractory period?
the contractile myocardium
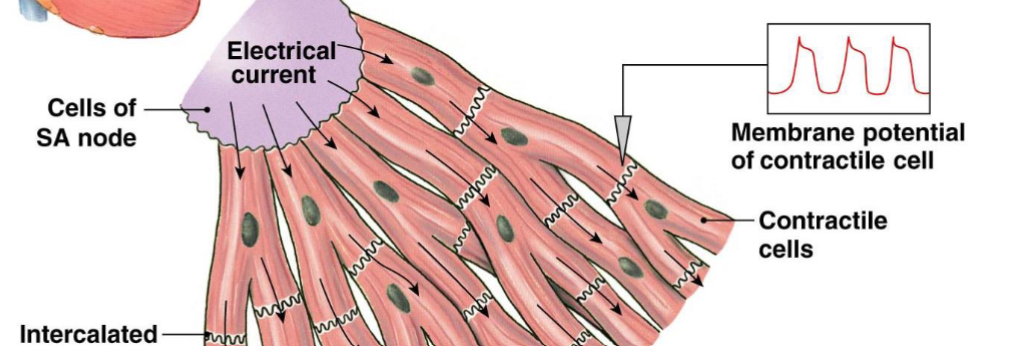
what is the structure of the myocardial muscle cells?
branched
have a single nucleus
attached by specialized junctions (intercalated disks)
what do gap junctions do in contractile cells?
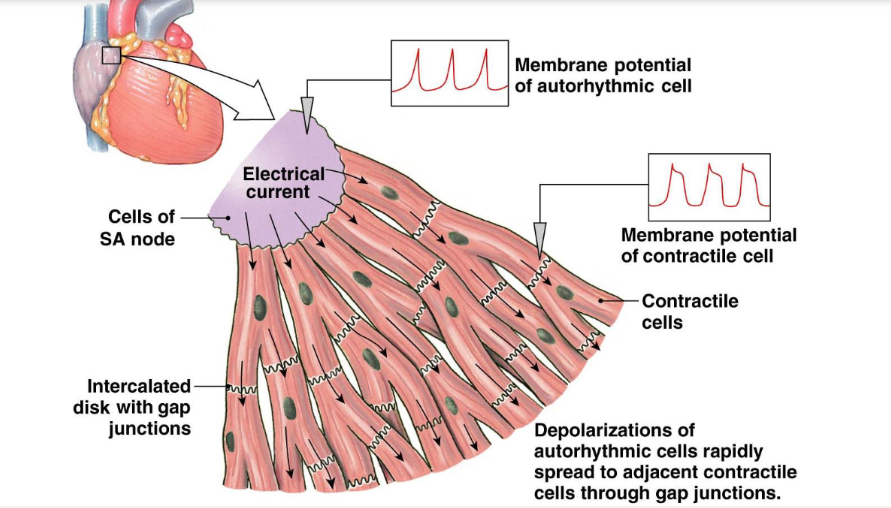
depolarizations of autorhythmic cells (pacemaker cells) rapidly spread to adjacent contractile cells through gap junctions.
what is a syncytium?
organ that is made up of different cells but because of gap junctions they act like one big cell
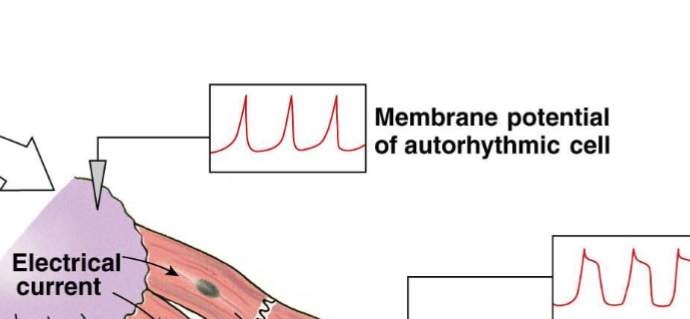
what does the membrane potential of pacemaker cells look like?
what is the membrane potential of contractile cells?
how do the pacemaker cells and contractile cells connect?
depolarizations of autorhythmic cells rapidly spread to adjacent contractile cells through gap junctions
which cell type controls force of contraction?
contractile cells
which controls rate of contraction?
pacemaker cells
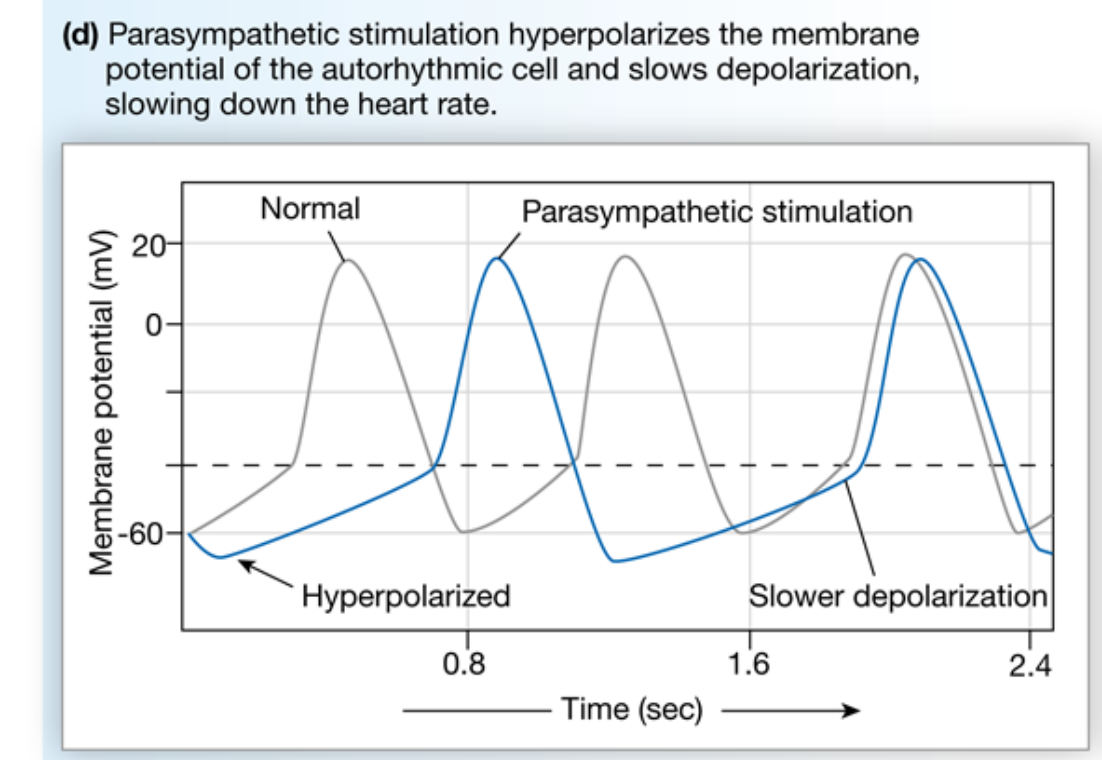
stimulation by parasympathetic nerves ____ heart rate
decreases
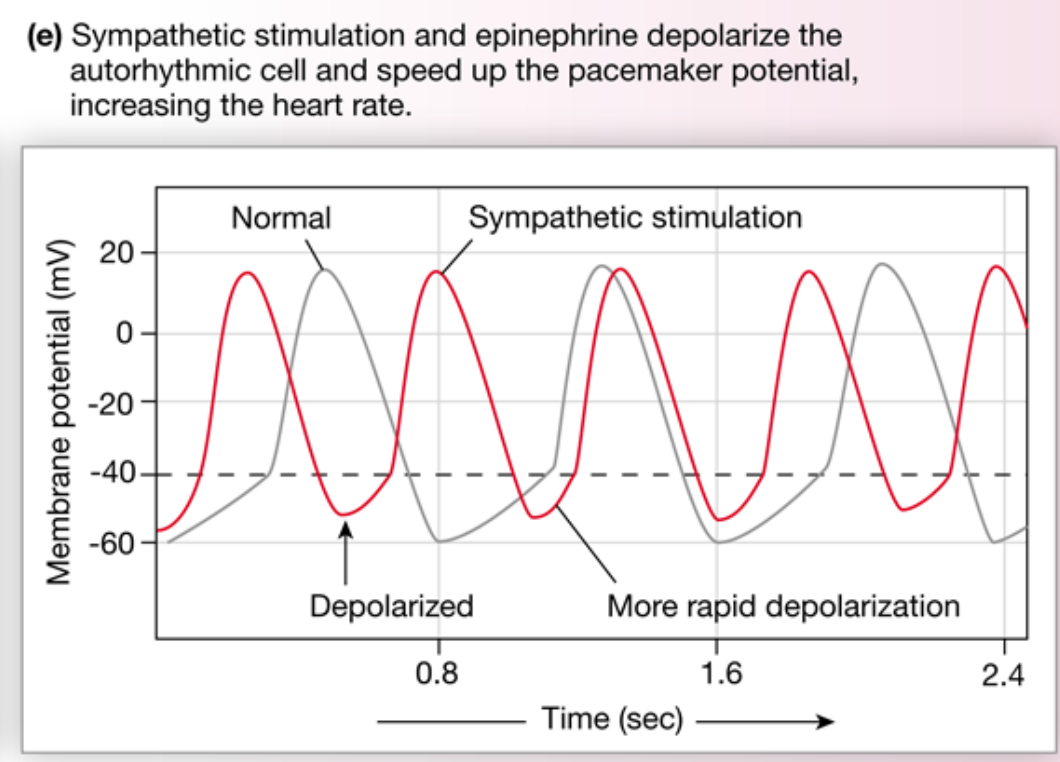
stimulation by sympathetic nerves ______ heart rate
increases
parasympathetic neuron (ACh on Muscarinic receptor) steps
cardiovascular control center in medulla oblongata
parasympathetic neurons (ACh)
muscarinic receptors of autorhythmic cells
increase K+ efflux; decrease Ca2+ influx
hyperpolarizes cell and decreases rate of depolarization
decrease heart rate
why did the parasympathetic neurons (ACh) lead to a decreased heart rate?
led to a decrease in cAMP —> increase K+ permeability and decrease Ca2+ permeability
this makes it harder to make threshold —> decrease HR
sympathetic neurons (NE)
cardiovascular control center in medulla oblongata
sympathetic neurons (NE)
B1-receptors autorhythmic cells
increase Na+ and Ca2+ influx
increase rate of depolarization
increase heart rate
why did the sympathetic neurons (NE) lead to a increased heart rate?
The sympathetic neuron leads to an increased cAMP —> increase in Na and Ca into cell
more positive —> easier to meet threshold
dec polymerization rate
increase HR
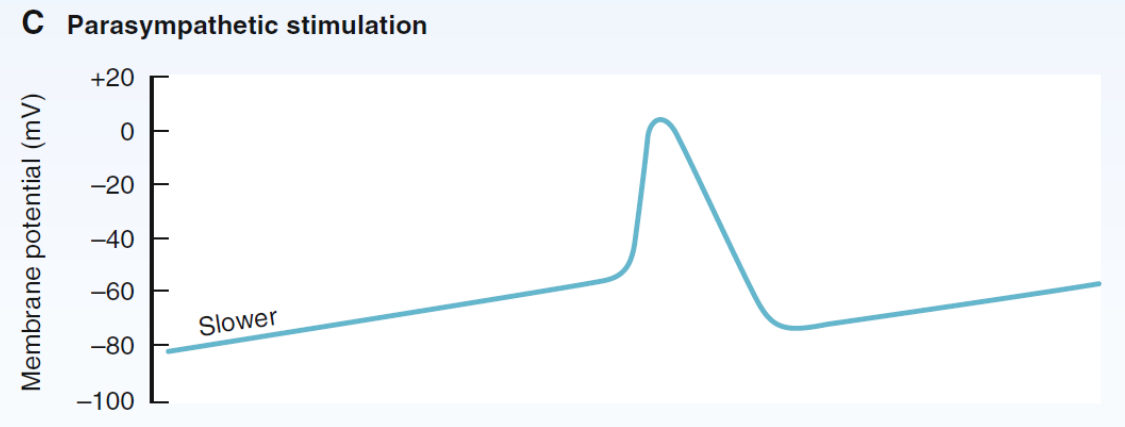
parasympathetic stimulation mV graph
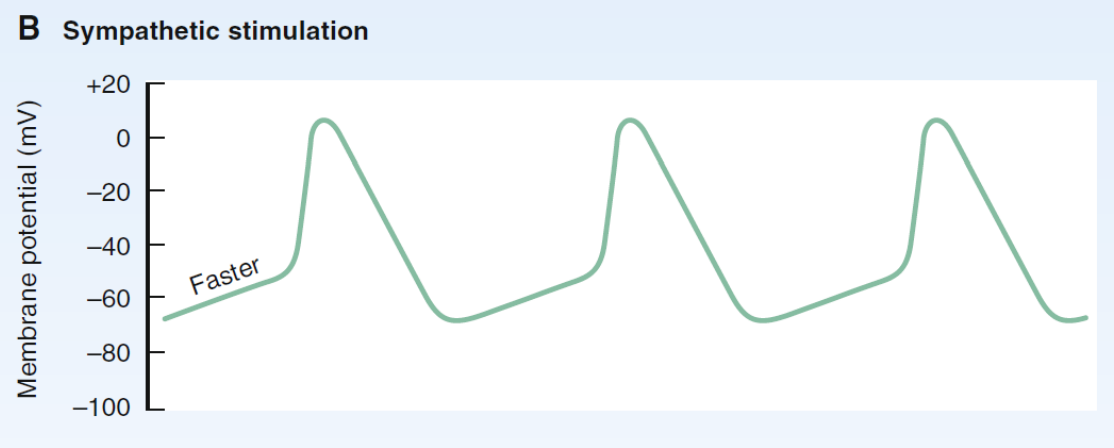
sympathetic stimulation mV graph
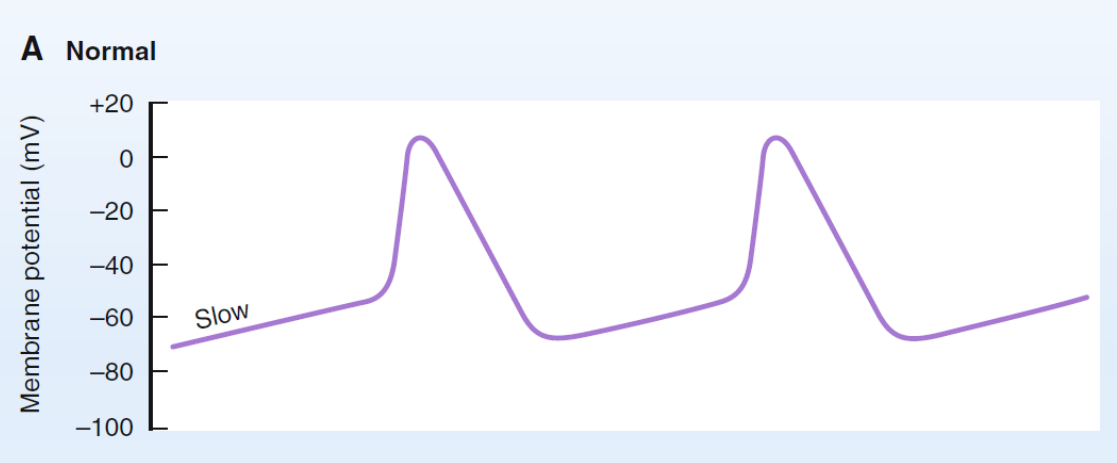
what does a normal mV graph look like?
what does a sympathetic stimulation look like?
what does parasympathetic stimulation look like?
ICLICKER: the internodal pathways take the signal to the:
Atrial muscle (atrial contractile cells)
AV node
what is the typical signal pathway?
SA node
internodal pathways
AV node
AV bundle (bundle of His)
bundle branches
purkinje fibers
ventricular contractile cells (cells in the ventricle)
how did the small local current flow in ECF reflect the ICF?
the ECF mirrors what is happening in the ICF of the cardiac contractile cells
what is the direction of the current flowing in the heart / electrical axis of the heart?
from the Right Atrium to the Left Ventricle
average value of 60 degrees from horizontal
electrocardiography
process of recording potential changes at skin surface
electrocardiogram (ECG or EKG)
record of potential changes
SUM of electrical activity
Not an action potential
action potential
a single cell recording ICF reading
lead I
right arm —> left arm
lead II
right arm —> left leg
lead III
left arm —> left leg
what lead most represents the heart?
lead two —> it is parallel to the heart
depolarization wave towards POS
upward deflection
repolarization wave towards NEG
upward deflection
depolarization wave toward NEG
downward deflection
repolarization wave towards POS
downward deflection
depolarization wave = 90 degrees / parallel
no deflection
repolarization wave = 90 degrees / parallel
no deflection
ICLICKER: overall strongest upward deflections produced by:
lead II