Circulation disturbances - Hemostasis
1/92
Earn XP
Description and Tags
Pathology - Lec 12 - Exam 2
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
93 Terms
hemostasis
arrest of bleeding → physiologic response to vascular damage & a mechanism to seal an injured vessel to prevent blood loss
Normal hemostasis is the result of what?
a series of complex, well-regulated processes that have 2 main functions
What is the main function of hemostasis under normal conditions?
maintains blood in fluid state
What is the main function of hemostasis under abnormal conditions?
rapid formation of a local hemostatic plug at a site of vascular damage
What is the big picture process of hemostasis?
transient vasoconstriction (brief reflex)
platelet aggregation
formation of platelet plug (1o hemostasis)
formation of a fibrin-platelet aggregate (2o hemostasis)
dissolution of fibrin-platelet aggregate (thrombolysis/ fibrinolysis)
What causes the brief reflex vasoconstriction at the initial site of vascular injury?
endothelin release from damaged endothelial cells
serotonin & TXA2 from platelets
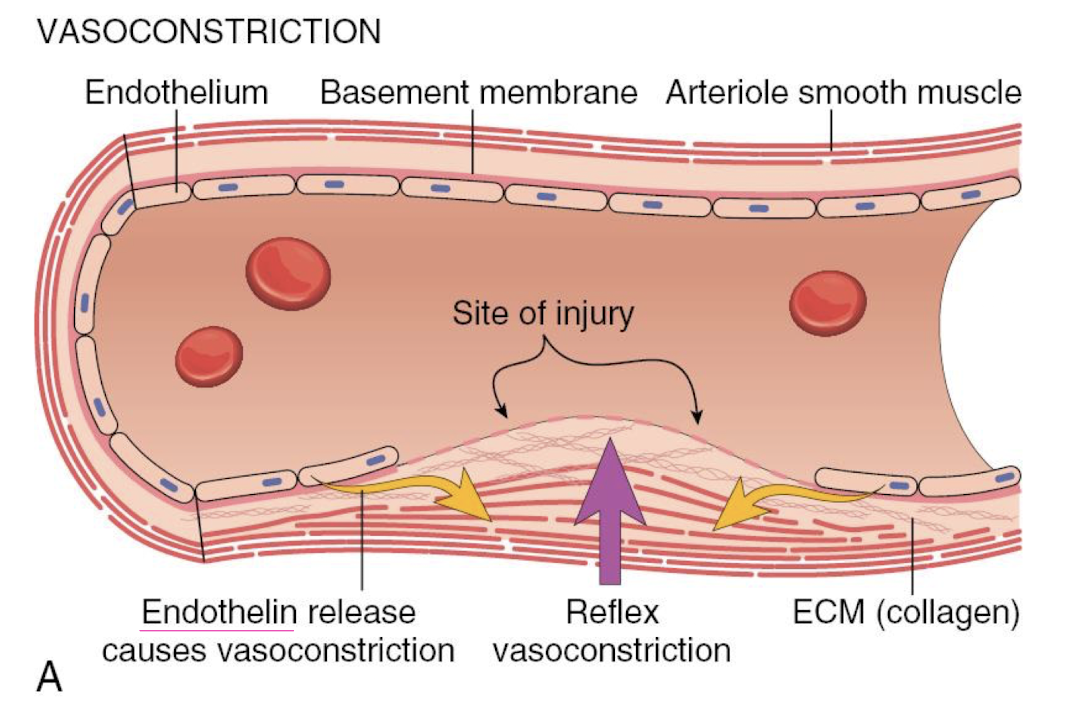
What are the physiologic goals of transient vasoconstriction?
reduce volume of blood flowing through the affected area
bring opposing endothelial surfaces closer together
Disruption of the endothelium exposes what?
collagen, fibronectin, & other ECM glycoproteins & proteoglycans
subendothelial von Willebrand factor (vWF)
What releases von Willebrand Factor and what does it do?
activated endothelial cells & platelets
coats subendothelial collagen
What is vWF necessary for?
firm platelet adhesion
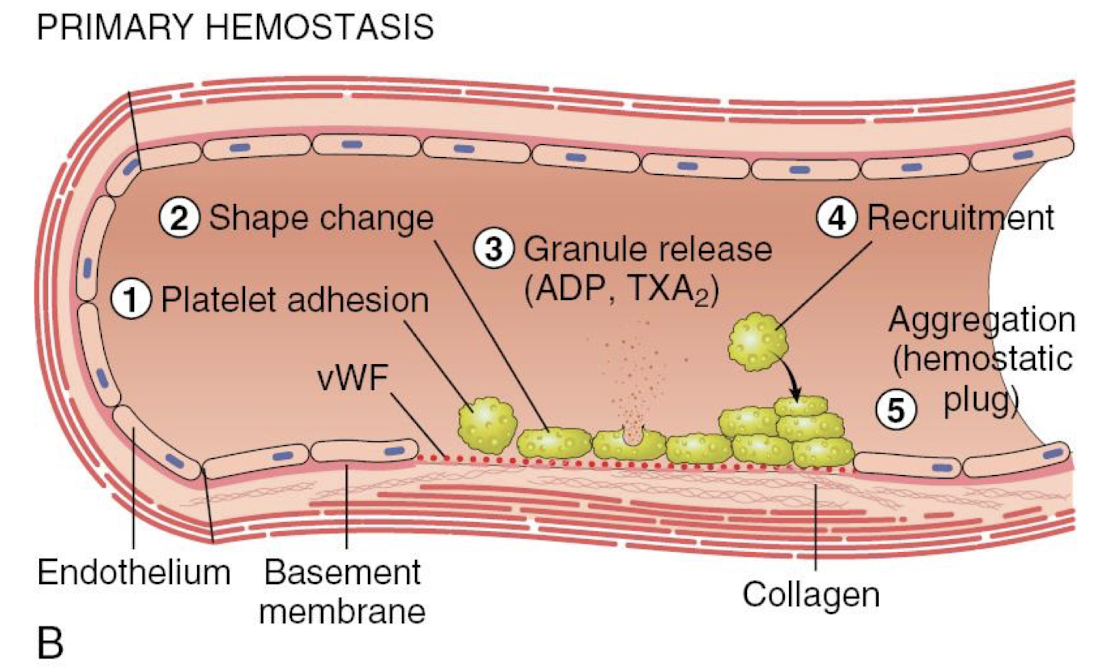
What are the 5 main steps of 1o hemostasis?
platelet adhesion (vWF attracts)
shape change
granule release (ADP, TXA2)
recruitment
aggregation (hemostatic plug)
What are the 4 main steps of 2o hemostasis?
tissue factor stimulates CoAg cascade
phospholipid complex expression
thrombin activation
fibrin polymerization
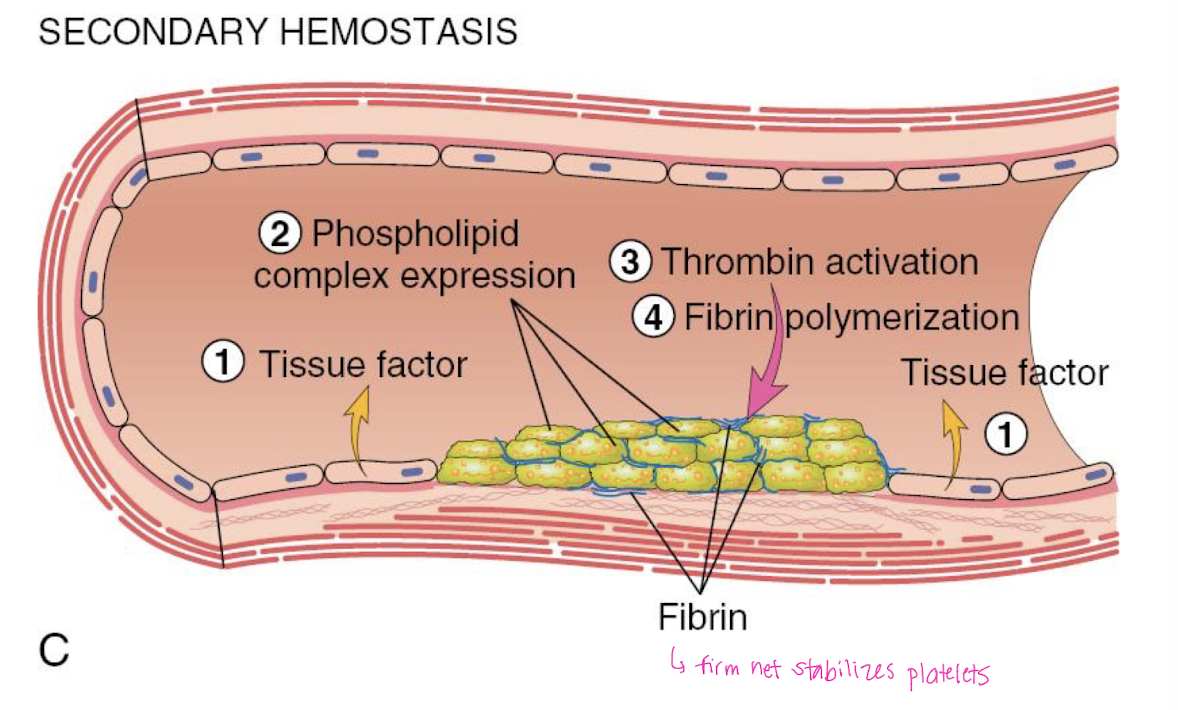
What function does fibrin serve in 2o hemostasis?
creates a firm net that stabilizes platelets
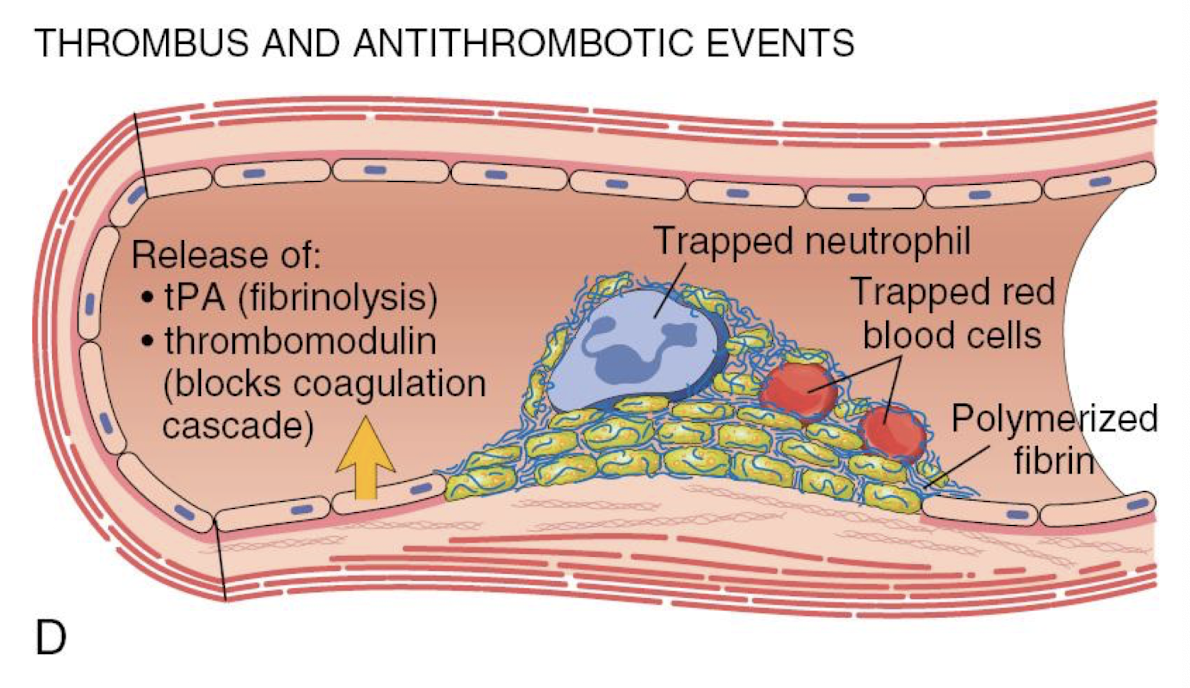
What 2 substances initiate antithrombotic events?
tPA → fibrinolysis
thrombomodulin → blocks CoAg cascade
T/F: Endothelium is a dynamic interface during hemostasis.
TRUE
A normal endothelium promotes what? How?
smooth, non-turbulent blood flow
vasodilation, antithrombotic & profibrinolytic (prevent clotting)
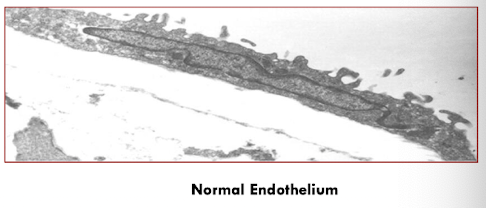
What types of injury activates the endothelium?
oxidative stress, hypoxia, inflammation, infectious agents, and tissue injury
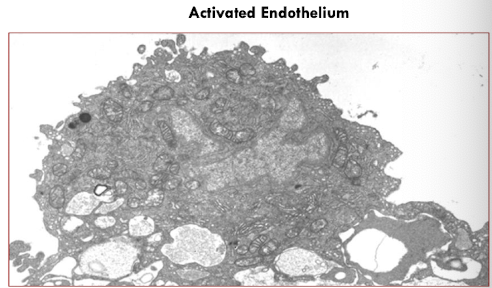
An injured (activated) endothelium promotes what?
vasoconstriction
enhance platelet adhesion & aggregation
stimulate coagulation
prothrombotic & antifibrinolytic (avoid breakdown)
What are platelets?
annucleate cell fragments derived from megakaryocytes circulating in blood
What do platelets adhere to?
exposed subendothelial collagen, laminin, fibronectin, etc
What are the membrane receptors that various glycoproteins bind to?
collagen, vWF, thrombin, fibrin, etc
T/F: An intact endothelium promotes interaction.
FALSE - prevents interaction
Platelets provide a surface for the assembly of what?
coagulation factors → IX & X
What are the 2 types of cytoplasmic granules?
alpha → growth factors, CoAg factors
dense → adenine nucleotides, Ca2+, inorganic phosphates, serotonin
coagulation
process by which blood changes from a liquid to a gel, forming a blood clot
What are the 3 classical coagulation pathways?
intrinsic
extrinsic
common
Coagulation factors can be:
serine protease proenzymes
non-enzymatic proteins
platelet phospholipids
transmembrane cell surface receptors
calcium
What are serine protease proenzymes?
enzymatic factors → vitamin K dependent factors (2,7,9,10)
What synthesizes serine protease proenzymes?
the liver
T/F: The circulating ½ life of serine protease proenzymes is long.
FALSE - short = hours to days
Which factor has the shortest ½ life?
factor VII → 4-6 hours
T/F: Serine protease proenzymes require activation to become proenzymes or zymogens
TRUE
The vitamin K dependent factors are activated by what?
vit K dependent carboxylation of glutamic acid residues on the factors
T/F: The vitamin K dependent factors are only found in the intrinsic and common pathways.
FALSE - found in all 3
The intrinsic pathway involves which substances?
high molecular weight kininogen, prekallikrein, & factors XII, XI, IX, VIII
T/F: The intrinsic pathway exhibits contact activation.
TRUE - HMWK, prekallikrein, XII, & XI
What activates the intrinsic pathway?
negatively charged substances → collagen, activated platelets, endotoxin
The intrinsic pathway is a series of activation events:
factors IX & VIII activate factor X → start of the common pathway
Which pathway usually initiates coagulation in vivo?
the extrinsic pathway
Explain the initiation of coagulation in vivo.
tissue factor (factor III) contacts & complexes w/ factor VII (or VIIa) → factor III-VIIa complex can activate factor IX (intrinsic) and factor X (common)
What is tissue factor?
CoAg factor III → cell surface glycoprotein expressed on subendothelial tissue
T/F: Factor X can be activated by either the intrisic or extrinsic pathway.
TRUE - binds to factor V
Where can factor V be found?
circulating in plasma
within platelet alpha granules
Factor X binds to what to form the prothrombinase complex?
Factor X-V-Ca2+ (10,5,4)
What does prothrombinase complex converts what?
prothrombin (factor II) to thrombin (factor IIa)
Thrombin converts what?
fibrinogen (Factor I) to fibrin (Ia)
Which factor cross-links fibrin?
factor XIII (fibrin stabilizing factor)
T/F: The extrinsic, intrinsic, and common pathways happen in a stepwise mannor.
FALSE - all pathways occur simultaneously
What are the 3 main platelet events in 1o hemostasis?
platelets recognize endothelial damage
platelets become activated
recruitment & aggregation of additional platelets to form platelet plug
How do platelets recognize endothelial damage?
change in blood flow
attracted to negatively charged ECM matrix
adhere to exposed vWF
What happens after platelets become activated?
results in shape change → increase surface area
release of secretory granules
phospholipid activiation/ phosphatidylserine exposure → binds CoAg factors
What are the 2 main steps of platelet aggregation?
fibrinogen (circulating plasma glycoprotein) bridges loosely link platelets → form loose aggregate
platelet contraction & polymerization of fibrinogen to fibrin consolidates aggregate to a dense plug
T/F: In many cases, fibrin is necessary for complete hemostasis.
TRUE - mediators from endothelial cells, activated platelets, and the ECM trigger activation of the CoAg cascade & the formation of fibrin for 2o hemostasis
The initiation of blood coagulation… (sorry this is the big bolded statement on slide 28)
occurs via the extrinsic tenase (VII, X) complex following tissue injury. However, sustained generation of factor Xa is dependent upon the intrinsic tenase (VIII, IX, X) complex which is 50x more efficient and not as susceptible to inhibition.
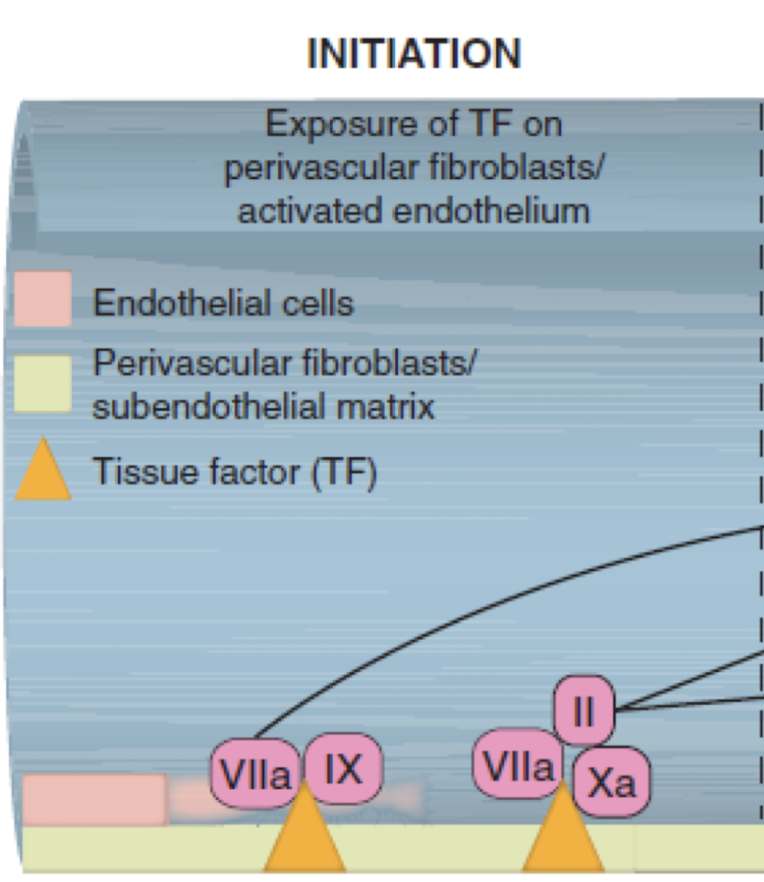
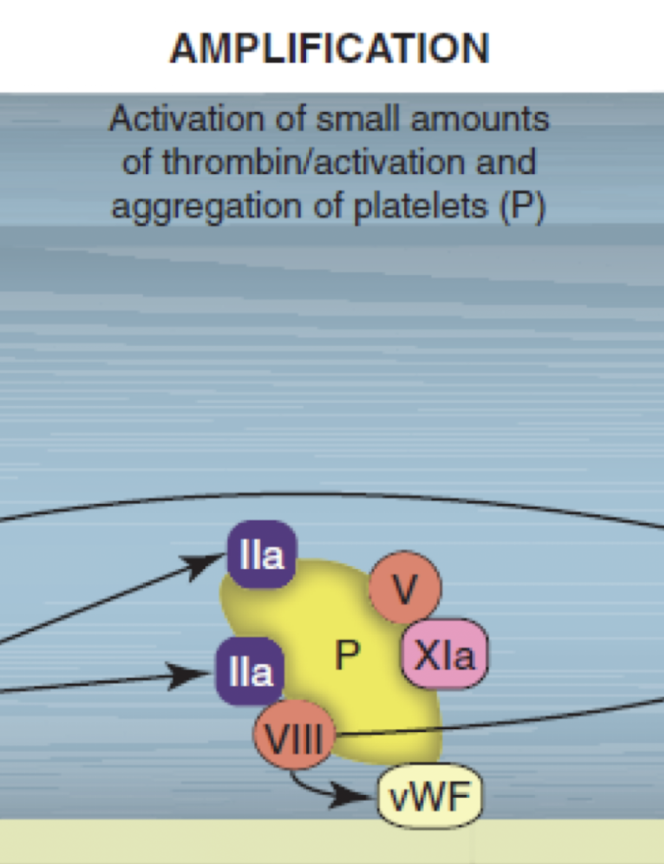
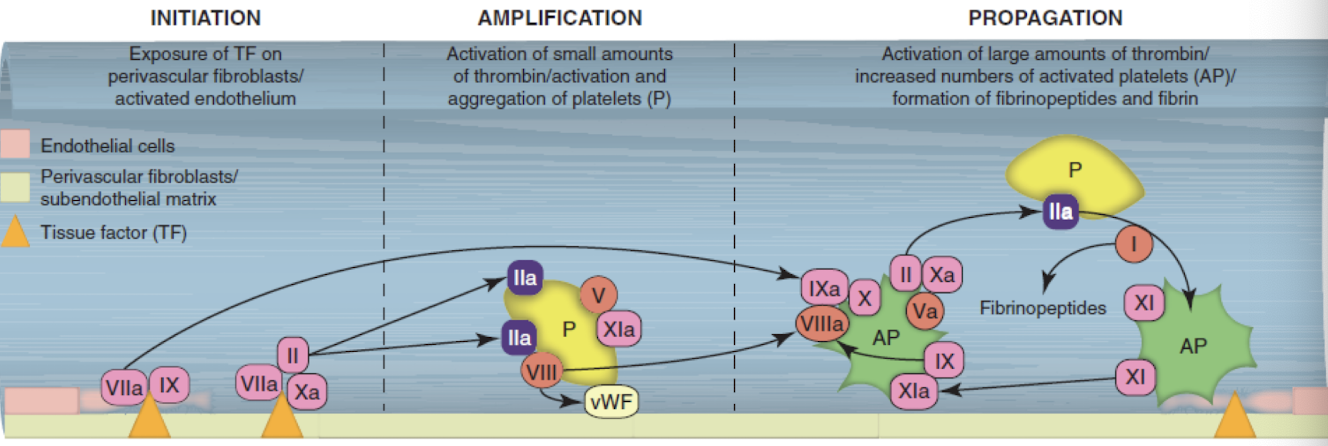
What are the 3 steps of the cell-based model of coagulation?
initiation
amplification
propagation
Cell-based model of coagulation: initiation
exposure of tissue factor (III) on perivascular fibroblasts/ activated endothelium
Cell-based model of coagulation: amplification
activation of small amounts of thrombin/ activation & aggregation of platelets (P)
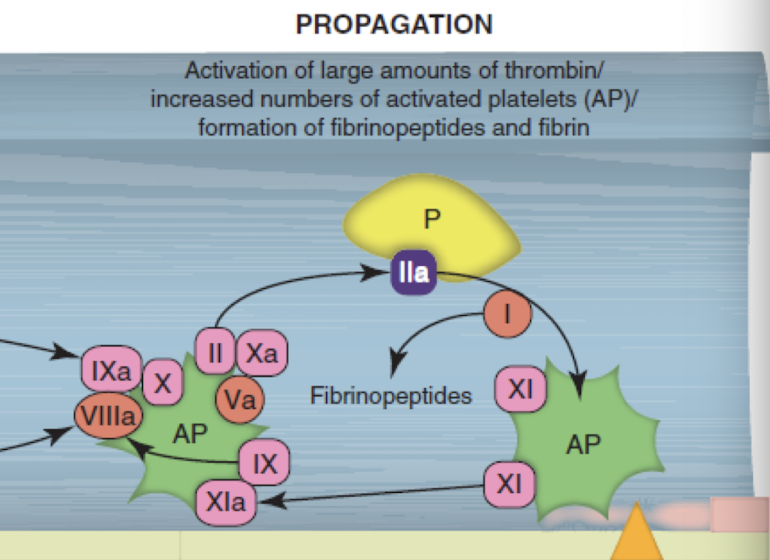
Cell-based model of coagulation: propagation
activation of large amounts of thrombin/ increased numbers of activated platelets (AP)/ formation of fibrinopeptides and fibrin
Cell-based model of coagulation: written out fully (sorry for the word vomit) - slide 29
Vascular damage results in tissue factor (TF) exposure and production of thrombin and factor IXa via the extrinsic pathway (initiation). The small amounts of thrombin formed during initiation cleave von Willebrand factor (vWF) from factor VIII, enhancing platelet adhesion to the damaged site. Thrombin activates platelets (P), which result in degranulation and the aggregation of additional platelets. Thrombin also results in the generation of factors Va, VIIIa, and XIa (amplification). During propagation, activated platelet (AP) membranes support assembly of intrinsic tenase complex (IXa/VIIIa) that is rapidly induced from factor XIa. Factor Xa and its coreactants form prothrombinase to generate large amounts of thrombin, which is released directly onto platelets to cleave fibrinogen into fibrinopeptides, which cross-link to form fibrin.
What is the stimuli of extrinsic coagulation?
release of tissue factor (III)
What releases tissue factor (III) thus stimulating extrinsic coagulation?
activated endothelium, activated platelets, perivascular cells, ECM
What is the stimuli for intrinsic coagulation?
binding of factor XII to negatively charged surfaces
What are the negatively charged surfaces that can trigger intrinsic coagulation via binding of factor XII?
ECM, activated platelets, endotoxin
Initiation of coagulation via the extrinsic pathway:
release of tissue factor
factor VII circulates in blood plasma (1% active VIIa)
factor VII, with Ca2+ forms a TF:VII complex on the surface of the injured area (phosphatidylserine helps with orientation)
TF:VII is activated toTF:VIIa (may be autoactivated or activated by many factors)
TF:VIIa activates factors X and IX
Amplification of coagulation via the common pathway:
active factor X (Xa) binds to factor V, Ca2+, and phospholipids to form prothrombinase complex
factor Xa cleaves prothrombin (II) into thrombin (IIa)
thrombin converts fibrinogen (I) to fibrin (Ia), activates platelets and factors XI, VIII, V, and XIII
Propagation of coagulation via the intrinsic pathway:
contact activation of factor XII - also activation of factors XI & VIII by thrombin (factor XII can autoactivate)
conversion of proenzymes to active enzymes occurs on platelet surface
activation cascade of XII → XI → IX
factor IX complexes with factor VIII = intrinsic tenase complex (+ Ca2+ & phospholipids)
intrinsic tenase complex activates factor X
T/F: It is harder to stop the intrinsic pathway.
TRUE
Explain the formation of fibrin.
factor Xa converts prothrombin (II) to thrombin (IIa)
thrombin cleaves fibrinogen (I) into fibrin (Ia)
factor XIII is activated by thrombin (& Xa)
factor XIIIa cross-links & stabilizes fibrin
T/F: Cross-linked fibrin is soluble.
FALSE - insoluble
Freshly formed fibrin threads are ________, causing them to adhere to ____________.
sticky
each other, platelets, blood cells, tissues, & foreign substances
Over time, fibrin ________.
contracts
The contraction of fibrin does what 2 things?
allows continued blood flow
brings edges of defect closer together
thrombolysis
removal/ dissolution of fibrin-platelet aggregate (thrombus) → fibrinolysis
What prevents permanent occlusion of the vessel after injury?
balance between formation of the fibrin-platelet aggregate for adequate hemostasis and removal of aggregate to allow for healing and return of normal blood flow
What is responsible for fibrinolysis?
plasminogen
Fibrinolysis is activated by what?
tissue plasminogen activator (tPA)
urokinases
factor XIIa
Fibrinolysis is inactivated by what?
a2-antiplasmin
a2-macroglobin
Fibrinolysis is regulated by what?
thrombin activatable fibrinolysis inhibitor (TAFI)
plasminogen activator inhibitors (PAIs)
T/F: Coagulation factors are only activated when needed.
FALSE - continuously activated, primed for rapid response
What helps limit the hemostatic reactions?
proteins that inhibit or degrade CoAg factors that circulate in the plasma & are released at sites of vascular injury
Coagulation regulation is the balance between which 3 pathways?
hemostatic
fibrinolytic
anticoagulant
How does blood flow contribute to the regulation of coagulation?
dilution → molecules removed from the site and from circulation by the liver and spleen
What is the most potent and most significant coagulation inhibitor?
antithrombin III
What are the other anticoagulant molecules?
heparan sulfate
tissue factor pathway inhibitor
protein C - protein S - thrombomodulin system
Protein C and protein S are _________ dependent.
vitamin K
What is the function of the anticoagulant system?
inactivate or inhibit factors involved in coagulation
Wha are the endothelial surface members of the anticoagulant system?
heparan sulfate
thrombomodulin
What are the circulating members of the anticoagulant system?
antithrombin III
tissue factor pathway inhibitor
protein C
protein S
What is the end result of the anticoagulant system?
conversion of thrombin (IIa) from procoagulant to anticoagulant
Which factors are inhibited as a result of the anticoagulant system?
Xa, VIIa, VIIIa, V
Regulation of coagulation requires the integration between pathways. An example of this is thrombin. Explain how thrombin can be both a procoagulant and anticoagulant.
procoagulant:
cleaves fibrinogen (I) to fibrin (Ia)
activates factors V, VIII, XI, and XIII
activates platelets
anticoagulant:
high concentrations destroys factors V and VIII
activates protein C when bound to thrombomodulin
A prothrombotic event is also ___________.
proinflammatory
T/F: There is no overlap between coagulation and inflammation.
FALSE - large overlaps → complement cascade