Pediatrics
0.0(0)
Card Sorting
1/139
There's no tags or description
Looks like no tags are added yet.
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
140 Terms
1
New cards
Newborn Assessment
1\. APGAR
2\. Work of breathing
3\. Vital signs (including temperature!)
4\. Weight
5\. Length
6\. Head circumference
7\. Chest circumference
8\. Abdominal girth
9\. Head to toe assessment
2\. Work of breathing
3\. Vital signs (including temperature!)
4\. Weight
5\. Length
6\. Head circumference
7\. Chest circumference
8\. Abdominal girth
9\. Head to toe assessment
2
New cards
Work of Breathing
● Retrations?
○ Note the severity and location
● Respiratory rate and depth
● Secretions?
○ Note the color, odor, consistency, and amount.
● Nasal flaring
● Grunting
○ Note the severity and location
● Respiratory rate and depth
● Secretions?
○ Note the color, odor, consistency, and amount.
● Nasal flaring
● Grunting
3
New cards
4
New cards
5
New cards
Pulse
● Check brachial pulse
● Check for no longer than 10 seconds
○ If you don’t feel it - start resuscitation!
● Count for a full minute when obtaining vital signs
● Check for no longer than 10 seconds
○ If you don’t feel it - start resuscitation!
● Count for a full minute when obtaining vital signs
6
New cards
Temperature
● Newborns can’t maintain their own temperature very well
● They’re wet!
○ Evaporative heat loss!
● To keep them warm:
○ Dry them off
○ Place them skin to skin
○ Bundle
○ Radiant warmer
○ Incubator
● They’re wet!
○ Evaporative heat loss!
● To keep them warm:
○ Dry them off
○ Place them skin to skin
○ Bundle
○ Radiant warmer
○ Incubator
7
New cards
Neurological
● Level of consciousness
● Infant behavior
● Cry
● Tone
● Pupils
○ Size
○ Shape
○ Reaction to light
● Any seizure activity
● Infant behavior
● Cry
● Tone
● Pupils
○ Size
○ Shape
○ Reaction to light
● Any seizure activity
8
New cards
Reflexes
● Reflexes, or lack thereof, can indicate abnormalities with the nervous system
● Many present as newborns (normal) and diminish at expected ages
● Abnormalities in newborn period:
○ Absent developmental reflexes
○ Asymmetric
○ Persist beyond anticipated age at which they should diminish
***Rooting reflex, palmar grasp reflex, Babinski reflex, moro reflex***
● Many present as newborns (normal) and diminish at expected ages
● Abnormalities in newborn period:
○ Absent developmental reflexes
○ Asymmetric
○ Persist beyond anticipated age at which they should diminish
***Rooting reflex, palmar grasp reflex, Babinski reflex, moro reflex***
9
New cards
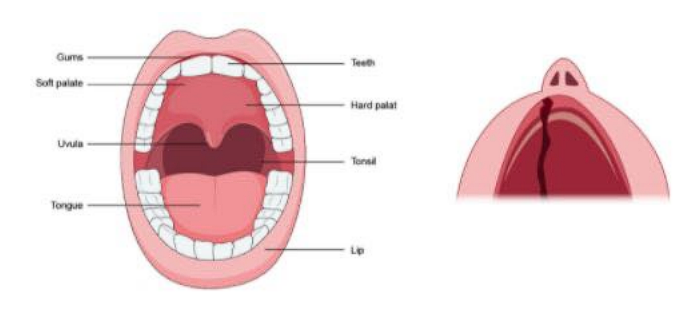
Head, Ears, Eyes, Nose, Throat (HEENT)
● Eyes
● Ears
● Nose
● Lips
● Mouth
● Throat
● Tongue
● Oral mucous membranes
● Neck
● Cranial sutures
● Anterior and posterior fontanelles
● Ears
● Nose
● Lips
● Mouth
● Throat
● Tongue
● Oral mucous membranes
● Neck
● Cranial sutures
● Anterior and posterior fontanelles
10
New cards
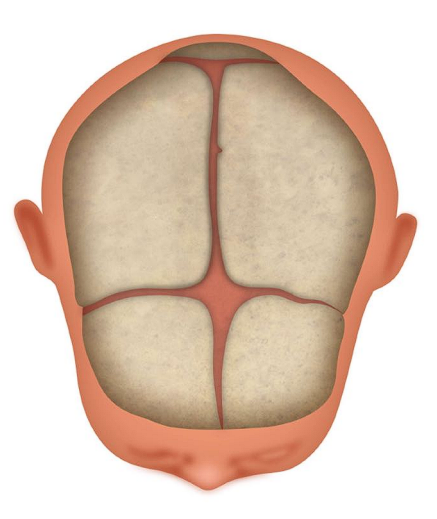
Fontanelles
● Soft/flat
○ Anterior
■ Closes between 6 and 18 mo
○ Posterior
■ Closes by 2 months
○ Anterior
■ Closes between 6 and 18 mo
○ Posterior
■ Closes by 2 months
11
New cards
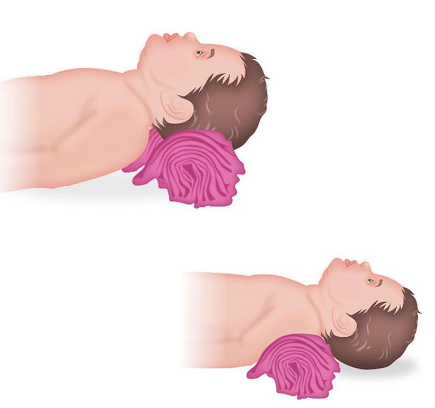
Respiratory
\
__**● Airway patency**__
○ Kids have a large occiput
■ Shoulder roll - ‘sniffing position’
■ Avoid supine position
○ Secretions
■ They can’t get their own boogers out!
■ Have suction ready
○ Swelling can occlude airway quickly
■ Tongue is bigger
■ Airway is smaller and less rigid
__**● Breathing**__
○ “Kids compensate until they fall off a cliff”
○ Lower lung capacity
○ Trend their vital signs! If they start to look bad…. Often, they are about to look __***really bad***__
__**● Airway patency**__
○ Kids have a large occiput
■ Shoulder roll - ‘sniffing position’
■ Avoid supine position
○ Secretions
■ They can’t get their own boogers out!
■ Have suction ready
○ Swelling can occlude airway quickly
■ Tongue is bigger
■ Airway is smaller and less rigid
__**● Breathing**__
○ “Kids compensate until they fall off a cliff”
○ Lower lung capacity
○ Trend their vital signs! If they start to look bad…. Often, they are about to look __***really bad***__
12
New cards
Cardiac
● Rate, rhythm, regularity
● Heart sounds
○ S1, S2
○ Murmur
■ Extra ‘whooshing’ heart sound
● Cyanosis
● Pulses
● Cap refill
● Edema
○ Location, severity
● Heart sounds
○ S1, S2
○ Murmur
■ Extra ‘whooshing’ heart sound
● Cyanosis
● Pulses
● Cap refill
● Edema
○ Location, severity
13
New cards
Musculoskeletal
● Weakness
● Any abnormalities
○ Contractures
○ Club foot
● Splints or devices
● Any abnormalities
○ Contractures
○ Club foot
● Splints or devices
14
New cards
Integumentary
● Skin color
● Moisture
● Integrity
● Wounds
● Rashes
● Lanugo
● Milia
● Mongolian spots
● Vernix caseosa
● Moisture
● Integrity
● Wounds
● Rashes
● Lanugo
● Milia
● Mongolian spots
● Vernix caseosa
15
New cards
Gastrointestinal
● Bowel sounds
● Abdominal girth
● Palpation
● Hernias
● Emesis
● Stools
● Anus/rectum
● Tone
● Abdominal girth
● Palpation
● Hernias
● Emesis
● Stools
● Anus/rectum
● Tone
16
New cards
Genitourinary
● Urine
○ Color
○ Odor
○ Amount
● Genitalia
● Check for sacral dimple (or a tuft of hair)
● Male - circumcised?
○ Color
○ Odor
○ Amount
● Genitalia
● Check for sacral dimple (or a tuft of hair)
● Male - circumcised?
17
New cards
Meconium Aspiration
Meconium is the first stool of the newborn.
When the meconium is passed before delivery, the fetus is at risk for meconium aspiration.
The aspiration can occur in utero, or just after delivery when the infant takes their first breath and starts to cry.
Meconium in the lungs causes very serious illness; pneumonia, pulmonary hypertension, and sepsis are all common. These infants become critically ill very quickly.
When the meconium is passed before delivery, the fetus is at risk for meconium aspiration.
The aspiration can occur in utero, or just after delivery when the infant takes their first breath and starts to cry.
Meconium in the lungs causes very serious illness; pneumonia, pulmonary hypertension, and sepsis are all common. These infants become critically ill very quickly.
18
New cards
Meconium Aspiration Assessment
__**If meconium aspiration is suspected, pertinent assessment will include:**__
● Respiratory status:
○ Accessory muscle use
○ Breath sounds
○ Grunting
○ Nasal flaring
__**Assessment to determine if meconium has been passed in utero:**__
● Visible meconium in fluid/on infant
● Discolored or foul smelling amniotic fluid
● Discoloration of the cord
● Discoloration of the nails/tonge on the infant
● Respiratory status:
○ Accessory muscle use
○ Breath sounds
○ Grunting
○ Nasal flaring
__**Assessment to determine if meconium has been passed in utero:**__
● Visible meconium in fluid/on infant
● Discolored or foul smelling amniotic fluid
● Discoloration of the cord
● Discoloration of the nails/tonge on the infant
19
New cards
Meconium Aspiration Interventions
Very quick action is essential to the outcome.
● Suction immediately after birth - before they take their first breath.
● Intubation
\
● IV antibiotics
● IV fluids
● Suction immediately after birth - before they take their first breath.
● Intubation
\
● IV antibiotics
● IV fluids
20
New cards
Jaundice
● Jaundice - elevated bilirubin level resulting in yellowing of the sclera, skin, and mucous membranes.
● Bilirubin - waste product produced during breakdown of red blood cells.
○ **Unconjugated (indirect)** - The heme that is released from hemoglobin in the process of red blood cell breakdown is converted to unconjugated bilirubin. It is transported to the liver.
○ **Conjugated (direct)** - Unconjugated bilirubin is converted to conjugated bilirubin in the liver. It is excreted in the stool.
● Bilirubin - waste product produced during breakdown of red blood cells.
○ **Unconjugated (indirect)** - The heme that is released from hemoglobin in the process of red blood cell breakdown is converted to unconjugated bilirubin. It is transported to the liver.
○ **Conjugated (direct)** - Unconjugated bilirubin is converted to conjugated bilirubin in the liver. It is excreted in the stool.
21
New cards
Physiological Jaundice
Jaundice that appears on day 2 or 3 of life.
This is expected and not considered pathologic unless other issues arise.
This is simply due to the normal transition from the placenta removing bilirubin, to the infant's liver doing the work.
Followed up outpatient with pediatrician.
This is expected and not considered pathologic unless other issues arise.
This is simply due to the normal transition from the placenta removing bilirubin, to the infant's liver doing the work.
Followed up outpatient with pediatrician.
22
New cards
Pathological Jaundice
Jaundice that occurs within the first 24 hours of life.
Serum bilirubin will be compared to normal value based on hours of life.
Jaundice appearing in the first 24 hours indicates some problem or disease process that needs addressed.
Could be an issue with the liver, or an ABO incompatibility
Serum bilirubin will be compared to normal value based on hours of life.
Jaundice appearing in the first 24 hours indicates some problem or disease process that needs addressed.
Could be an issue with the liver, or an ABO incompatibility
23
New cards
Kernicterus
Kernicterus is a type of brain damage that can result from high levels of bilirubin in the blood.
Complications of kernicterus:
● Cerebral palsy
● Hearing loss
● Problems with vision
● Problems with teeth
● Intellectual disabilities
Kernicterus is completely preventable! We must monitor for signs and symptoms of jaundice early and treat promptly.
Complications of kernicterus:
● Cerebral palsy
● Hearing loss
● Problems with vision
● Problems with teeth
● Intellectual disabilities
Kernicterus is completely preventable! We must monitor for signs and symptoms of jaundice early and treat promptly.
24
New cards
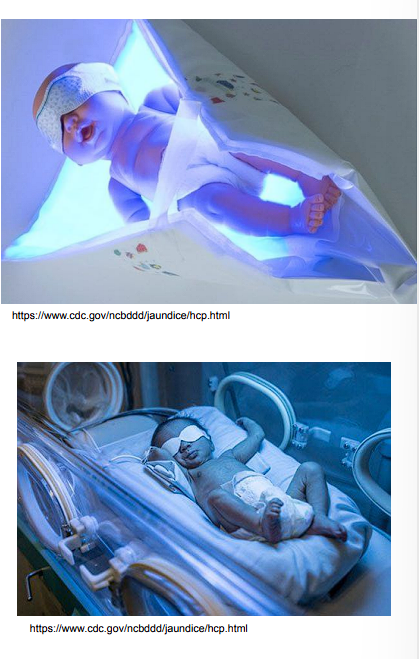
Treatment - phototherapy
● Helps break down bilirubin so it may be excreted in the feces.
● Must ensure the eyes and genitals are covered.
● Monitor the level and distance from the light if overhead therapy being used.
● Double, triple, and quadruple therapy depending on severity.
● Must ensure the eyes and genitals are covered.
● Monitor the level and distance from the light if overhead therapy being used.
● Double, triple, and quadruple therapy depending on severity.
25
New cards
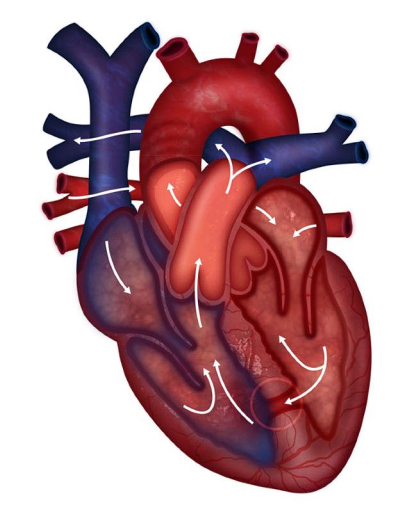
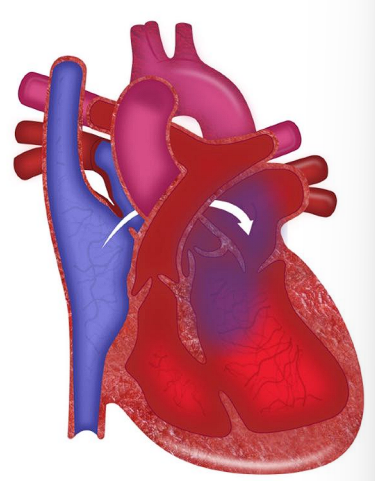
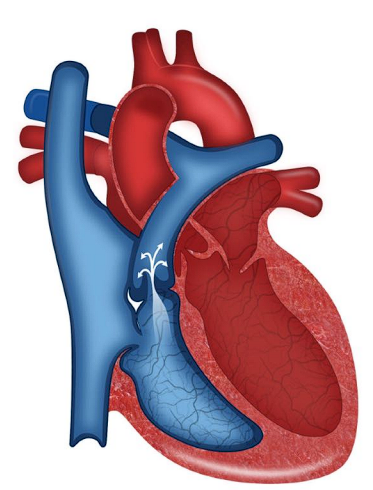
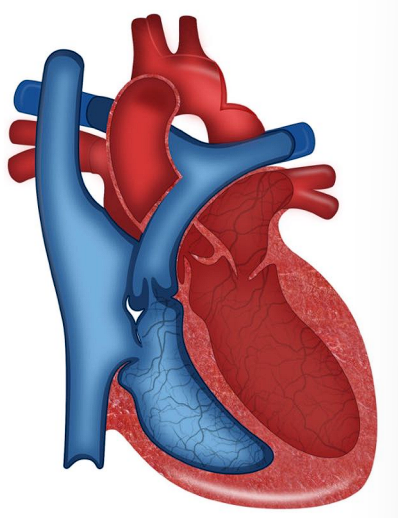
Fetal Circulation
● Fetal circulation bypasses the lungs
○ Mom is doing the oxygenation
■ No need for blood to to the lungs
○ Uses three shunts
■ Foramen ovale - opening between the atria
■ Ductus arteriosus - opening between the pulmonary artery and the aorta
■ Ductus venosus - Vessel connecting the inferior vena cava to the umbilical vein
● Umbilical vein
○ Carries oxygenated, nutrient-rich blood from the placenta to the fetus
● Umbilical arteries
○ Carry deoxygenated, nutrient-depleted blood from the fetus to the placenta
○ Mom is doing the oxygenation
■ No need for blood to to the lungs
○ Uses three shunts
■ Foramen ovale - opening between the atria
■ Ductus arteriosus - opening between the pulmonary artery and the aorta
■ Ductus venosus - Vessel connecting the inferior vena cava to the umbilical vein
● Umbilical vein
○ Carries oxygenated, nutrient-rich blood from the placenta to the fetus
● Umbilical arteries
○ Carry deoxygenated, nutrient-depleted blood from the fetus to the placenta
26
New cards
Foramen ovale
An opening between the right and left atrium present in fetal circulation
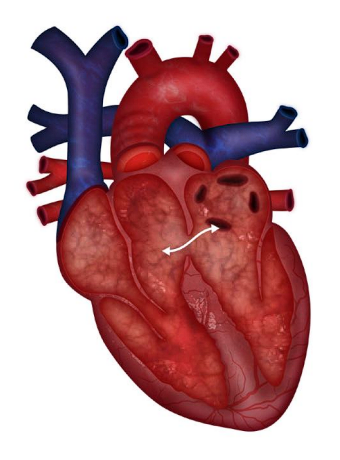
27
New cards
Ductus arteriosus
An opening between the pulmonary artery and aorta present in fetal circulation.
28
New cards
Defects
● Abnormalities in the structure of the heart
__**● Risk factors:**__
○ Maternal viral infections
○ Maternal diabetes
○ Drug and alcohol use
○ Advanced maternal age
__**● Commonly occur with chromosomal abnormalities and syndromes such as:**__
○ Trisomy 21
○ Trisomy 18
○ Turners syndrome
○ DiGeorge syndrome
__**● Risk factors:**__
○ Maternal viral infections
○ Maternal diabetes
○ Drug and alcohol use
○ Advanced maternal age
__**● Commonly occur with chromosomal abnormalities and syndromes such as:**__
○ Trisomy 21
○ Trisomy 18
○ Turners syndrome
○ DiGeorge syndrome
29
New cards
Stenosis
stiffening or thickening
30
New cards
Atresia
does not develop
31
New cards
Hypoplasia
underdeveloped
32
New cards
Hyperplasia
overdeveloped/grown
33
New cards
Coarctation
narrowing or stricture
34
New cards
Mixing
deoxygenated and oxygenated blood mixing together
○ “Purple blood”
○ “Purple blood”
35
New cards
Ductal dependent
dependent on the ductus arteriosus for mixing of blood
36
New cards
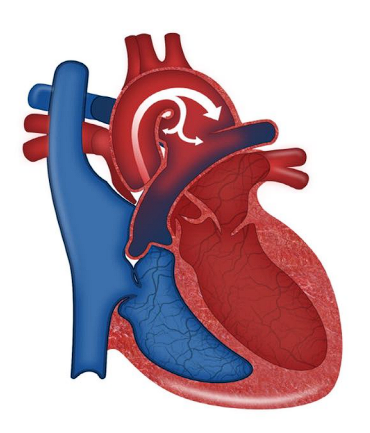
Shunting
***The movement of blood from one area to another (Blood will ALWAYS move from areas of high pressure, to areas of low pressure)***
__**● Right to left shunt**__
○ Blood from the right side of the heart moves to the left side of the heart.
○ Blood on the right side is deoxygenated
○ Blood in the left side of the heart moves out to the body
○ Deoxygenated blood is getting out to the body!
○ This shunt therefore causes cyanosis
__**● Left to right shunt**__
○ Blood from the left side of the heart moves to the right side of the heart.
○ Blood on the left side is oxygenated
○ Blood in the left side of the heart moves out to the lungs
○ MORE oxygenated blood is going to the lungs
○ This shunts causes pulmonary overcirculation - but NO cyanosis
__**● Right to left shunt**__
○ Blood from the right side of the heart moves to the left side of the heart.
○ Blood on the right side is deoxygenated
○ Blood in the left side of the heart moves out to the body
○ Deoxygenated blood is getting out to the body!
○ This shunt therefore causes cyanosis
__**● Left to right shunt**__
○ Blood from the left side of the heart moves to the right side of the heart.
○ Blood on the left side is oxygenated
○ Blood in the left side of the heart moves out to the lungs
○ MORE oxygenated blood is going to the lungs
○ This shunts causes pulmonary overcirculation - but NO cyanosis
37
New cards
Congenital Heart Defects: Acyanotic
__**Increase pulmonary blood flow L→ R shunt**__
1\. Patent Ductus Arteriosus (PDA)
2\. Atrial Septal Defect (ASD)
3\. Ventricular Septal Defect (VSD)
4\. Atrioventricular canal
__**Obstructive**__
1\. Coarctation of the aorta
2\. Aortic stenosis
3\. Pulmonic stenosis
1\. Patent Ductus Arteriosus (PDA)
2\. Atrial Septal Defect (ASD)
3\. Ventricular Septal Defect (VSD)
4\. Atrioventricular canal
__**Obstructive**__
1\. Coarctation of the aorta
2\. Aortic stenosis
3\. Pulmonic stenosis
38
New cards
Congenital Heart Defects: Cyanotic
__**Decrease pulmonary blood flow R→L shunt**__
1\. Tetralogy of Fallot
2\. Tricuspid atresia
__**Ductal Dependent: mixed**__
1\. Transposition of the great arteries (TGA)
2\. Hypoplastic Left Heart Syndrome (HLHS)
1\. Tetralogy of Fallot
2\. Tricuspid atresia
__**Ductal Dependent: mixed**__
1\. Transposition of the great arteries (TGA)
2\. Hypoplastic Left Heart Syndrome (HLHS)
39
New cards
Acyanotic-Patent ductus arteriosus (PDA)
__**● Defect**__
○ Failure of the ductus arteriosus to close
○ Should close 12 to 72 hours after birth
__**● Specific assessment findings**__
○ Machine-like murmur
__**● Treatment:**__
○ Small: often close spontaneously
○ Indomethacin or ibuprofen
○ Surgically closed
__**● Alprostadil (Prostaglandins/PGE)**__
○ Medication that can be administered to keep the PDA open in certain heart defects.
○ This can allow blood to get out to the body when it otherwise couldn’t.
○ Failure of the ductus arteriosus to close
○ Should close 12 to 72 hours after birth
__**● Specific assessment findings**__
○ Machine-like murmur
__**● Treatment:**__
○ Small: often close spontaneously
○ Indomethacin or ibuprofen
○ Surgically closed
__**● Alprostadil (Prostaglandins/PGE)**__
○ Medication that can be administered to keep the PDA open in certain heart defects.
○ This can allow blood to get out to the body when it otherwise couldn’t.
40
New cards
Acyanotic-Atrial Septal Defect
__**● Defect:**__
○ Opening between the atria
__**● Shunt:**__
○ Left to Right. Acyanotic
__**● History:**__
○ Is often asymptomatic until later in childhood.
○ Child fatigues easily, DOE, poor weight gain
__**● Assessment findings:**__
○ Murmur
__**● Treatment**__
○ Small - often close spontaneously
○ Large - Surgical closure
○ Opening between the atria
__**● Shunt:**__
○ Left to Right. Acyanotic
__**● History:**__
○ Is often asymptomatic until later in childhood.
○ Child fatigues easily, DOE, poor weight gain
__**● Assessment findings:**__
○ Murmur
__**● Treatment**__
○ Small - often close spontaneously
○ Large - Surgical closure
41
New cards
Acyanotic-Ventricular Septal Defect
__**● Defect:**__
○ Opening between the ventricles
__**● Shunt:**__
○ Left to right. Acyanotic
__**● History:**__
○ Typical for s/s of HF to begin at 2-8 weeks
__**● Assessment findings:**__
○ Loud murmur ○ CHF
__**● Treatment**__
○ CHF management: Diuretics, ACE inhibitors, β-blockers
○ Nutrition
○ Surgical closure
■ Bacterial endocarditis prophylaxis
○ Opening between the ventricles
__**● Shunt:**__
○ Left to right. Acyanotic
__**● History:**__
○ Typical for s/s of HF to begin at 2-8 weeks
__**● Assessment findings:**__
○ Loud murmur ○ CHF
__**● Treatment**__
○ CHF management: Diuretics, ACE inhibitors, β-blockers
○ Nutrition
○ Surgical closure
■ Bacterial endocarditis prophylaxis
42
New cards
Acyanotic-Atrioventricular Canal Defect
__**● Defect:**__
○ Opening between the atria AND the ventricles
○ ASD + VSD + Single AV Valve
__**● Shunt:**__
○ Left to right. Acyanotic
__**● History:**__
○ Heart failure s/s and failure to thrive
__**● Assessment findings:**__
○ Murmur
○ \*High risk for heart failure
__**● Treatment**__
○ CHF management: Digoxin, diuretics, ACE inhibitors, and β-blockers
○ Nutrition
○ Complete surgical repair at 3-6 months
■ Bacterial endocarditis prophylaxis
○ Opening between the atria AND the ventricles
○ ASD + VSD + Single AV Valve
__**● Shunt:**__
○ Left to right. Acyanotic
__**● History:**__
○ Heart failure s/s and failure to thrive
__**● Assessment findings:**__
○ Murmur
○ \*High risk for heart failure
__**● Treatment**__
○ CHF management: Digoxin, diuretics, ACE inhibitors, and β-blockers
○ Nutrition
○ Complete surgical repair at 3-6 months
■ Bacterial endocarditis prophylaxis
43
New cards
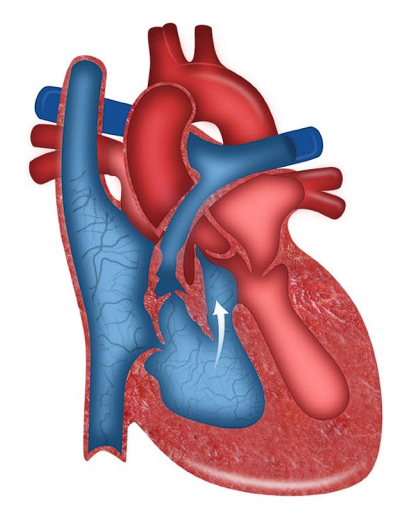
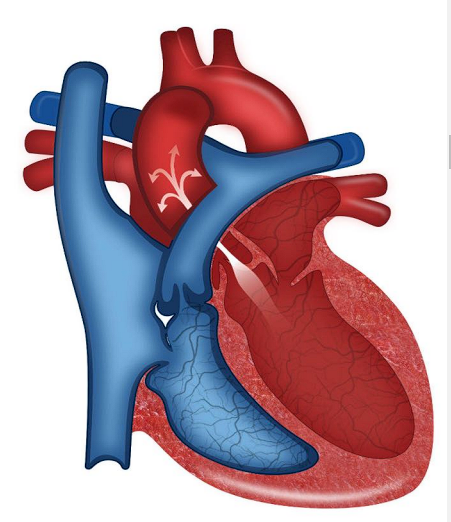
Cyanotic-Tetralogy of Fallot
__**● Four defects:**__
○ Large VSD
○ Pulmonary stenosis
○ Right ventricular hypertrophy
○ Overriding aorta
__**● History**__
○ Cyanosis
○ Dyspnea
○ Poor feeding and weight gain
__**● Specific assessment findings:**__
○ Tet spells
○ Large VSD
○ Pulmonary stenosis
○ Right ventricular hypertrophy
○ Overriding aorta
__**● History**__
○ Cyanosis
○ Dyspnea
○ Poor feeding and weight gain
__**● Specific assessment findings:**__
○ Tet spells
44
New cards
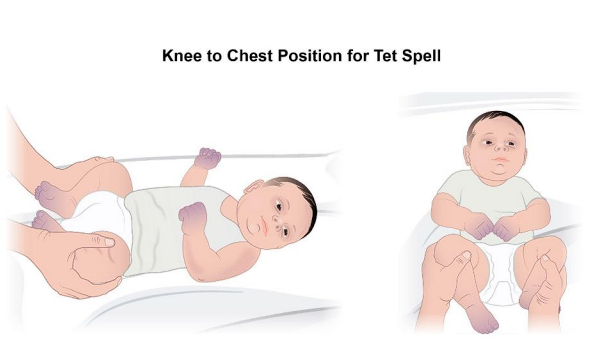
Cyanotic-Tet Spells
● Hypoxic spells that occur in TOF.
● Begins with irritability and hyperpnea and followed by a prolonged period of intense cyanosis leading to syncope.
● A drop in systemic vascular resistance increases the right to left shunt and decreases pulmonary blood flow.
● More right to left shunting → more deoxygenated blood out to the body.
● Begins with irritability and hyperpnea and followed by a prolonged period of intense cyanosis leading to syncope.
● A drop in systemic vascular resistance increases the right to left shunt and decreases pulmonary blood flow.
● More right to left shunting → more deoxygenated blood out to the body.

45
New cards
Tet Spell Interventions
Comfort and calm
Knee-to-chest position
Supplemental oxygen
Sedation - morphine
Volume
Knee-to-chest position
Supplemental oxygen
Sedation - morphine
Volume
46
New cards
Tet Spell Management
● If mild - can go home and grow until ready for surgery
● If critically ill with severe hypoxia - surgery is required in the neonatal period.
● Ideally, complete repair around 6 months of age.
● Can be earlier depending on signs and symptoms.
● Surgery - “Tet repair”
○ BT shunt
○ Repair of pulmonary valve
○ Patch VSD
● Bacterial endocarditis prophylaxis
● If critically ill with severe hypoxia - surgery is required in the neonatal period.
● Ideally, complete repair around 6 months of age.
● Can be earlier depending on signs and symptoms.
● Surgery - “Tet repair”
○ BT shunt
○ Repair of pulmonary valve
○ Patch VSD
● Bacterial endocarditis prophylaxis
47
New cards
Cyanotic-Tricuspid Atresia
__**● Defect:**__
○ Tricuspid valve does not grow
○ Leaves no communication between the right atrium and the right ventricle
○ VSD/ASD
○ Hypoplastic right ventricle
○ Enlarged mitral valve and left ventricle
__**● Specific assessment findings:**__
○ Cyanosis
__**● Treatment**__
○ Prostaglandins
○ Surgical repair - BT shunt, Rashkind procedure
○ Tricuspid valve does not grow
○ Leaves no communication between the right atrium and the right ventricle
○ VSD/ASD
○ Hypoplastic right ventricle
○ Enlarged mitral valve and left ventricle
__**● Specific assessment findings:**__
○ Cyanosis
__**● Treatment**__
○ Prostaglandins
○ Surgical repair - BT shunt, Rashkind procedure
48
New cards
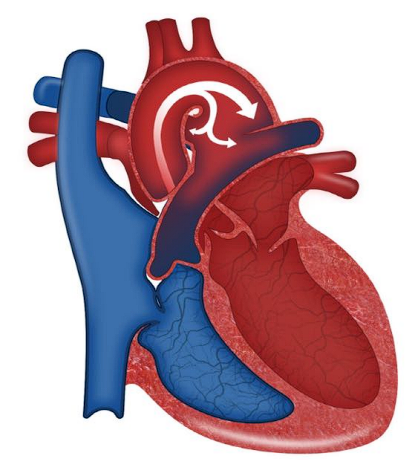
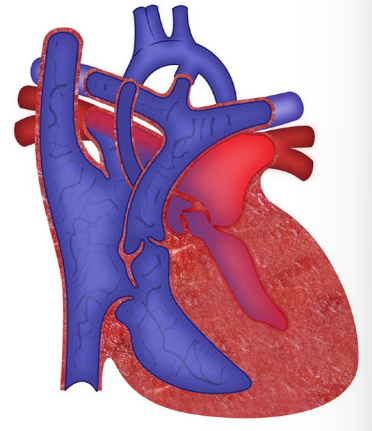
Transposition of the Great Arteries
__**● Defect:**__
○ The aorta and the pulmonary artery are switched
○ Two parallel circuits
■ Oxygenated blood continuously circulating through the pulmonary circuit
■ Deoxygenated blood continuously circulating through the systemic circuit
__**● Specific assessment findings:**__
○ Cyanosis within 1 hour of first
__**● Treatment**__
○ Prostaglandins
○ Balloon atrial septostomy
○ Surgical repair: arterial switch
○ Bacterial endocarditis prophylaxis for life
○ The aorta and the pulmonary artery are switched
○ Two parallel circuits
■ Oxygenated blood continuously circulating through the pulmonary circuit
■ Deoxygenated blood continuously circulating through the systemic circuit
__**● Specific assessment findings:**__
○ Cyanosis within 1 hour of first
__**● Treatment**__
○ Prostaglandins
○ Balloon atrial septostomy
○ Surgical repair: arterial switch
○ Bacterial endocarditis prophylaxis for life
49
New cards
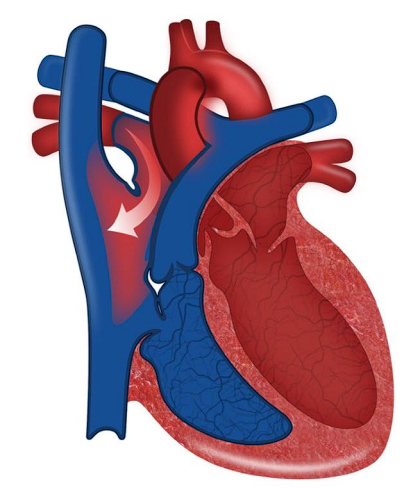
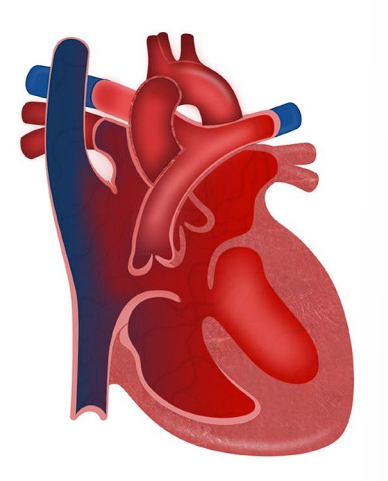
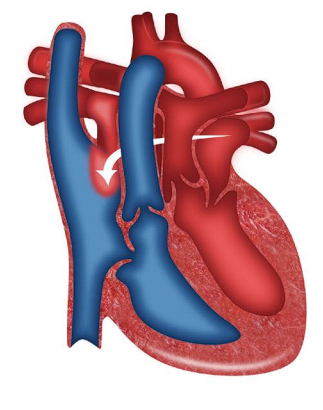
Hypoplastic Left Heart Syndrome (HLHS)
__**● Defect:**__
○ Left-sided structures don’t develop normally
○ Aorta is small
○ Left atria/ventricle are hypoplastic
○ Mitral valve is atretic
○ When the ductus arteriosus closes, very little blood will be able to get out to the body
__**● History:**__
○ Cyanosis when DA closes
○ Increased RR, fatigue - Can lead to obstructive cardiogenic shock
__**● Specific assessment findings:**__
○ Hepatomegaly
○ Murmur
○ Left-sided structures don’t develop normally
○ Aorta is small
○ Left atria/ventricle are hypoplastic
○ Mitral valve is atretic
○ When the ductus arteriosus closes, very little blood will be able to get out to the body
__**● History:**__
○ Cyanosis when DA closes
○ Increased RR, fatigue - Can lead to obstructive cardiogenic shock
__**● Specific assessment findings:**__
○ Hepatomegaly
○ Murmur
50
New cards
Hypoplastic Left Heart Syndrome (HLHS) Management
__**● Immediate treatment:**__
○ Prostaglandins
○ Correct acidemia
○ Inotropes
○ Plan for surgery
__**● Palliative Surgery:**__
○ Norwood at birth
○ Glenn at 2 months old
○ Fontan at 2 years old
__**● Possible cardiac transplantation**__
○ Prostaglandins
○ Correct acidemia
○ Inotropes
○ Plan for surgery
__**● Palliative Surgery:**__
○ Norwood at birth
○ Glenn at 2 months old
○ Fontan at 2 years old
__**● Possible cardiac transplantation**__
51
New cards
Aortic Stenosis
__**● Defect:**__
○ Narrowing of the aorta
○ Harder for the left ventricle to eject blood
__**● History:**__
○ Activity intolerance, fatigue, chest pain
○ Sudden death due to ventricular arrhythmias
__**● Specific assessment findings:**__
○ Exercise intolerance and syncopal episodes
○ Narrow pulse pressure
○ Pronounced apical impulse ○ Thrill
__**● Treatment**__
○ Critical
■ Balloon valvuloplasty asap! Prevent shock!
○ Ross procedure
○ Surgical valve replacement. If mechanical valve - will need anticoagulated!
○ Severe: needs to avoid contact sports.
○ Narrowing of the aorta
○ Harder for the left ventricle to eject blood
__**● History:**__
○ Activity intolerance, fatigue, chest pain
○ Sudden death due to ventricular arrhythmias
__**● Specific assessment findings:**__
○ Exercise intolerance and syncopal episodes
○ Narrow pulse pressure
○ Pronounced apical impulse ○ Thrill
__**● Treatment**__
○ Critical
■ Balloon valvuloplasty asap! Prevent shock!
○ Ross procedure
○ Surgical valve replacement. If mechanical valve - will need anticoagulated!
○ Severe: needs to avoid contact sports.
52
New cards
Pulmonary Stenosis
__**● Defect:**__
○ Narrowing of the pulmonary artery
○ Makes it harder for the RV to pump, causes hypertrophy
__**● History:**__
○ Often asymptomatic; as progressed DOE and fatigue develop
__**● Specific assessment findings**__
○ Dyspnea on exertion
○ Murmur
__**● Treatment**__
○ Pulmonary valvotomy
○ Moderate to severe stenosis: child should avoid high intensity activities.
○ Narrowing of the pulmonary artery
○ Makes it harder for the RV to pump, causes hypertrophy
__**● History:**__
○ Often asymptomatic; as progressed DOE and fatigue develop
__**● Specific assessment findings**__
○ Dyspnea on exertion
○ Murmur
__**● Treatment**__
○ Pulmonary valvotomy
○ Moderate to severe stenosis: child should avoid high intensity activities.
53
New cards
Coarctation of the Aorta
__**● Defect:**__
○ Narrowing of the aorta
○ Impedes blood flow to the lower half of the body
__**● History:**__
○ Symptoms appear quickly
■ When ductus arteriosus closes can rapidly progress to hypotension, acidosis, shock, and death.
○ Narrowing of the aorta
○ Impedes blood flow to the lower half of the body
__**● History:**__
○ Symptoms appear quickly
■ When ductus arteriosus closes can rapidly progress to hypotension, acidosis, shock, and death.
54
New cards
Coarctation of the Aorta-Specific findings
__**● Upper extremities**__
○ Bounding pulses
○ Hypertensive
○ Warm
○ Pink
__**● Lower extremities**__
○ Weak or absent pulses
○ Hypotensive
○ Pale
○ Cool
__**● Management**__
○ Critical coarctation - think shock!!
■ Prostaglandins
■ Surgical repair
○ Lifelong follow up
■ High risk for recoractation or aortic aneurysm
○ Bounding pulses
○ Hypertensive
○ Warm
○ Pink
__**● Lower extremities**__
○ Weak or absent pulses
○ Hypotensive
○ Pale
○ Cool
__**● Management**__
○ Critical coarctation - think shock!!
■ Prostaglandins
■ Surgical repair
○ Lifelong follow up
■ High risk for recoractation or aortic aneurysm
55
New cards
Which of the following assessment findings would lead the nurse to believe their client could have a coarctation of the aorta? Select all that apply.
a. +1 radial pulses and +3 femoral pulses
b. Pale, cool feet and legs with warm pink hands and arms
c. Hypertensive brachial blood pressure
d. >4 second capillary refill on the hands
e. Hypotensive popliteal blood pressure
a. +1 radial pulses and +3 femoral pulses
b. Pale, cool feet and legs with warm pink hands and arms
c. Hypertensive brachial blood pressure
d. >4 second capillary refill on the hands
e. Hypotensive popliteal blood pressure
Answer: B, C, and E
A is incorrect. In coarctation of the aorta, there is a stricture in the aorta preventing blood flow out of the left ventricle. It usually occurs beyond the blood vessels that branch off to your upper body and before the blood vessels that lead to your lower body. So blood flow to the upper body is abundant, but hardly any can make it to the lower part of the body. Therefore, there are decreased lower extremity pulses, and increased upper extremity pulses. So the nurse would expect to palpate bounding +3 or +4 pulses in the radial pulse, but weak +1 or even absent femoral pulses. This is all due to the stricture in the aorta preventing blood flow from getting to the lower extremities.
B is correct. Pale, cool feet and legs with warm pink hands and arms would be expected in a client with coarctation of the aorta due to the stricture in the aorta preventing blood flow from getting to the lower extremities.
C is correct. A hypertensive brachial blood pressure would be expected in a client with coarctation of the aorta due to the stricture in the aorta preventing blood flow from getting to the lower extremities.
D is incorrect. A normal capillary refill time is
A is incorrect. In coarctation of the aorta, there is a stricture in the aorta preventing blood flow out of the left ventricle. It usually occurs beyond the blood vessels that branch off to your upper body and before the blood vessels that lead to your lower body. So blood flow to the upper body is abundant, but hardly any can make it to the lower part of the body. Therefore, there are decreased lower extremity pulses, and increased upper extremity pulses. So the nurse would expect to palpate bounding +3 or +4 pulses in the radial pulse, but weak +1 or even absent femoral pulses. This is all due to the stricture in the aorta preventing blood flow from getting to the lower extremities.
B is correct. Pale, cool feet and legs with warm pink hands and arms would be expected in a client with coarctation of the aorta due to the stricture in the aorta preventing blood flow from getting to the lower extremities.
C is correct. A hypertensive brachial blood pressure would be expected in a client with coarctation of the aorta due to the stricture in the aorta preventing blood flow from getting to the lower extremities.
D is incorrect. A normal capillary refill time is
56
New cards
Epiglottitis
● Inflammation of the epiglottis
● Epiglottis
○ A leaf-shaped flap in the throat that prevents food from entering the windpipe and the lungs. It stands open during breathing, allowing air into the larynx
● Inflammation restricts the airway
● Caused by an infection
○ Bacterial
● Haemophilus influenzae type b
● Medical emergency
● Epiglottis
○ A leaf-shaped flap in the throat that prevents food from entering the windpipe and the lungs. It stands open during breathing, allowing air into the larynx
● Inflammation restricts the airway
● Caused by an infection
○ Bacterial
● Haemophilus influenzae type b
● Medical emergency
57
New cards
Epiglottitis Assessment
● Fever
● Difficulty swallowing
● Drooling
● Stridor
● Tripoding
● No cough
● Change in LOC
● Cherry red epiglottis
__**The 4 D’s of epiglottitis**__
● Dysphagia
● Dysphonia
● Drooling
● Distress
● Difficulty swallowing
● Drooling
● Stridor
● Tripoding
● No cough
● Change in LOC
● Cherry red epiglottis
__**The 4 D’s of epiglottitis**__
● Dysphagia
● Dysphonia
● Drooling
● Distress
58
New cards
The nurse is assessing a 4 year old who was sent to the ED from urgent care. Assessment reveals tripod positioning, blue lips, mottled skin, inspiratory stridor, and excessive drooling. Vital signs are:
Temp: 39 C
HR: 188
RR: 46
O2: 82 %
Which of the following should the nurse do first?
a. Keep the child calm and call for emergency airway equipment
b. Obtain IV access
c. Assess the throat for a cherry red epiglottis
d. Place the child on a high flow nasal cannula at 100% FiO2
Temp: 39 C
HR: 188
RR: 46
O2: 82 %
Which of the following should the nurse do first?
a. Keep the child calm and call for emergency airway equipment
b. Obtain IV access
c. Assess the throat for a cherry red epiglottis
d. Place the child on a high flow nasal cannula at 100% FiO2
Answer: A
A is correct. Based on the presenting symptoms, the nurse suspects that this child has epiglottitis. Any child presenting with excessive drooling, distress, and stridor is highly suspicious for this medical emergency. In addition, this client is already showing signs of circulatory compromise including circumoral cyanosis and mottling. The priority nursing action in this emergency is keeping the child calm and calling for emergency airway equipment. The child is at risk of losing their airway, and airway is always the priority!
B is incorrect. It is inappropriate to attempt to obtain IV access on a child suspected of epiglottitis before emergency airway equipment is available. The priority action at this time is keeping the child calm and calling for emergency airway equipment.
C is incorrect. It is inappropriate to assess the throat for a cherry red epiglottis at this time. Although presence of a cherry red epiglottis would confirm the diagnosis of epiglottitis, this child is at risk of losing their airway. The priority action will be to protect that airway before assessing the throat. .
D is incorrect. Placing the child on a high flow nasal cannula at 100% FiO2 is not the priority at this time. This answer probably sounded right, because you see the O2 is 82% and they have circumoral cyanosis. Oxygen sounds like the right answer! But this intervention addresses the ‘C’ in your ABC’s - circulation. And the priority is always ‘A’, airway! This child is at risk of losing their airway, so all interventions need to wait until there is emergency airway equipment close by. If anything upsets the child their airway could spams and obstruct completely making it impossible to intubate them. That is why keeping the child calm and calling for emergency airway equipment is the priority in epiglottitis clients.
A is correct. Based on the presenting symptoms, the nurse suspects that this child has epiglottitis. Any child presenting with excessive drooling, distress, and stridor is highly suspicious for this medical emergency. In addition, this client is already showing signs of circulatory compromise including circumoral cyanosis and mottling. The priority nursing action in this emergency is keeping the child calm and calling for emergency airway equipment. The child is at risk of losing their airway, and airway is always the priority!
B is incorrect. It is inappropriate to attempt to obtain IV access on a child suspected of epiglottitis before emergency airway equipment is available. The priority action at this time is keeping the child calm and calling for emergency airway equipment.
C is incorrect. It is inappropriate to assess the throat for a cherry red epiglottis at this time. Although presence of a cherry red epiglottis would confirm the diagnosis of epiglottitis, this child is at risk of losing their airway. The priority action will be to protect that airway before assessing the throat. .
D is incorrect. Placing the child on a high flow nasal cannula at 100% FiO2 is not the priority at this time. This answer probably sounded right, because you see the O2 is 82% and they have circumoral cyanosis. Oxygen sounds like the right answer! But this intervention addresses the ‘C’ in your ABC’s - circulation. And the priority is always ‘A’, airway! This child is at risk of losing their airway, so all interventions need to wait until there is emergency airway equipment close by. If anything upsets the child their airway could spams and obstruct completely making it impossible to intubate them. That is why keeping the child calm and calling for emergency airway equipment is the priority in epiglottitis clients.
59
New cards
Epiglottitis Interventions
● IV antibiotics
● Humidified oxygen
● Intubation and mechanical ventilation
● Keep the child calm
● No interventions until airway is secure
● Do not irritate the throat
○ NO tongue depressor
○ NO oral thermometer
○ NO assessing the throat
● NPO
● Tripod position
● Avoid supine
● Hib vaccine has reduced incidence
● Encourage parents to vaccinate to prevent
● Humidified oxygen
● Intubation and mechanical ventilation
● Keep the child calm
● No interventions until airway is secure
● Do not irritate the throat
○ NO tongue depressor
○ NO oral thermometer
○ NO assessing the throat
● NPO
● Tripod position
● Avoid supine
● Hib vaccine has reduced incidence
● Encourage parents to vaccinate to prevent
60
New cards
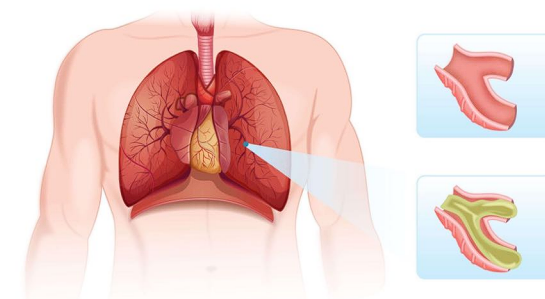
Bronchiolitis
● Inflammation of the bronchioles
● Bronchioles
○ Smallest branches of the airway
○ Lead to alveoli
● Alveoli
○ Air sacs
○ Location of gas exchange in the lungs
● Thick mucus clogs up the bronchioles
● Leads to decreased gas exchange in alveoli
○ Air trapping
○ Collapsed alveoli
● Most common in children under 2 years old
● Seasonal illness
○ Most common in winter
● Causative agent usually viral
○ Respiratory Syncytial Virus (RSV)
● Very contagious
● Worst on days 4-6
● Bronchioles
○ Smallest branches of the airway
○ Lead to alveoli
● Alveoli
○ Air sacs
○ Location of gas exchange in the lungs
● Thick mucus clogs up the bronchioles
● Leads to decreased gas exchange in alveoli
○ Air trapping
○ Collapsed alveoli
● Most common in children under 2 years old
● Seasonal illness
○ Most common in winter
● Causative agent usually viral
○ Respiratory Syncytial Virus (RSV)
● Very contagious
● Worst on days 4-6
61
New cards
Bronchiolitis Assessment
● Cough
● Fever
● Increased work of breathing
○ Retractions
■ Subcostal
■ Intracostal
■ Tracheal tug
○ Nasal flaring
○ Head bobbing
○ Tachypnea
● Lung sounds
○ Crackles
○ Wheezing
● Hypoxia
○ Circumoral cyanosis
○ Mottling
○ Delayed capillary refill
○ Decreased SpO2
● Changes in behavior
○ Irritability
○ Lethargy
○ Poor feeding
● Fever
● Increased work of breathing
○ Retractions
■ Subcostal
■ Intracostal
■ Tracheal tug
○ Nasal flaring
○ Head bobbing
○ Tachypnea
● Lung sounds
○ Crackles
○ Wheezing
● Hypoxia
○ Circumoral cyanosis
○ Mottling
○ Delayed capillary refill
○ Decreased SpO2
● Changes in behavior
○ Irritability
○ Lethargy
○ Poor feeding
62
New cards
Bronchiolitis Interventions
Supportive treatment
● Oxygenation
○ Nasal cannula - high flow nasal cannula
○ Always humidified
● Fluid & Nutrition
○ NGT
○ Enteral feedings ○ IVF
● Antipyretics
● Analgesics
● Oxygenation
○ Nasal cannula - high flow nasal cannula
○ Always humidified
● Fluid & Nutrition
○ NGT
○ Enteral feedings ○ IVF
● Antipyretics
● Analgesics
63
New cards
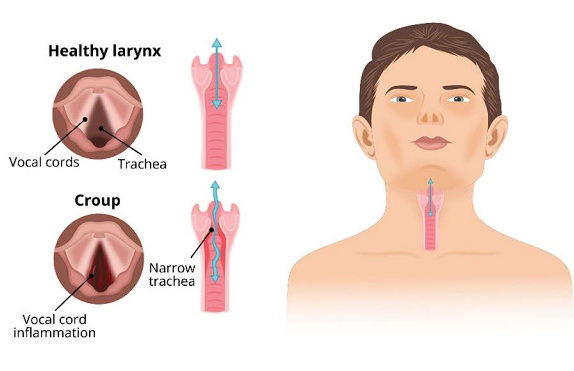
Croup
● Laryngotracheobronchitis (LTB)
● Viral respiratory tract illness
○ Results in inflammation and edema of the larynx and/or trachea
● Commonly affects pediatric population
● Viral respiratory tract illness
○ Results in inflammation and edema of the larynx and/or trachea
● Commonly affects pediatric population
64
New cards
Croup Assessment
● Hoarse, “bark-like” (or seal-like) cough
● Stridor
● Chest wall retractions
● Runny nose, fever
● Symptoms often worsen at night
● Stridor
● Chest wall retractions
● Runny nose, fever
● Symptoms often worsen at night
65
New cards
Croup Tx
● Corticosteroids
● Epinephrine via nebulizer
○ “Racemic epi”
● Keep patient calm and decrease anxiety levels
○ Agitation can lead to respiratory distress
● Epinephrine via nebulizer
○ “Racemic epi”
● Keep patient calm and decrease anxiety levels
○ Agitation can lead to respiratory distress
66
New cards
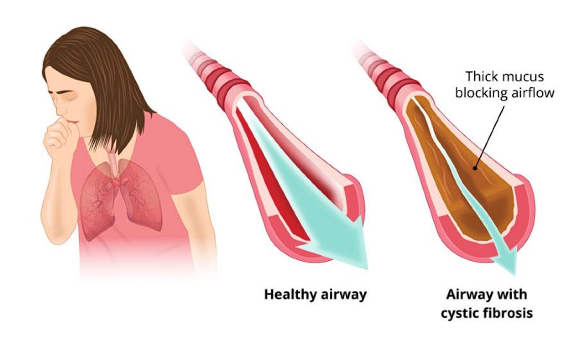
Cystic Fibrosis
● Autosomal recessive disorder
● Mutation leads to a buildup of excessive mucus in the airways
● Mucus leads to airway obstruction
● Mutation leads to a buildup of excessive mucus in the airways
● Mucus leads to airway obstruction
67
New cards
Cystic Fibrosis Pathophysiology
● Mucus is both excessive and very thick
● Causes mechanical obstructions throughout the body
○ Bronchi
○ Small intestines
○ Pancreatic ducts
○ Bile ducts
● Causes mechanical obstructions throughout the body
○ Bronchi
○ Small intestines
○ Pancreatic ducts
○ Bile ducts
68
New cards
Cystic Fibrosis Diagnosis
● Meconium ileus
○ Meconium is thicker and stickier than normal, creates a blockage and first stool doesn’t pass.
● Sweat chloride test
○ Sweat is collected and analyzed for increased levels of chloride ○ Sweat tastes salty
○ Meconium is thicker and stickier than normal, creates a blockage and first stool doesn’t pass.
● Sweat chloride test
○ Sweat is collected and analyzed for increased levels of chloride ○ Sweat tastes salty
69
New cards
Cystic Fibrosis Assessment
● Respiratory
○ Excessive mucus
○ Frequent respiratory infections
○ Hypoxemia
■ Clubbing
■ Cyanosis
■ Barrel chest
● Gastrointestinal
○ Intestinal obstruction
○ Meconium ileus
○ Large, bulky, frothy, foul smelling stool
○ Fat soluble vitamin deficiency
■ ADEK
■ Malnutrition
■ Failure to thrive
● Endocrine
○ Diabetes
● Integumentary
○ Salty tasting sweat
○ Elevated chloride in sweat
● Reproductive
○ Males are infertile
○ Excessive mucus
○ Frequent respiratory infections
○ Hypoxemia
■ Clubbing
■ Cyanosis
■ Barrel chest
● Gastrointestinal
○ Intestinal obstruction
○ Meconium ileus
○ Large, bulky, frothy, foul smelling stool
○ Fat soluble vitamin deficiency
■ ADEK
■ Malnutrition
■ Failure to thrive
● Endocrine
○ Diabetes
● Integumentary
○ Salty tasting sweat
○ Elevated chloride in sweat
● Reproductive
○ Males are infertile
70
New cards
Cystic Fibrosis Tx
● Airway clearance
○ Chest physiotherapy
○ Vest therapy
● Respiratory infections
○ Monitor for
○ Treat with IV antibiotics
○ Prevent!
● Respiratory support
○ Monitor work of breathing
○ Oxygen as needed
● Bronchodilators
● Promote nutrition and growth
○ High calorie, high protein diet
○ Increased fluid intake
○ Monitor serial weights
○ Pancreatic enzymes
■ Give within 30 min of eating every meal and snack
■ Sprinkle capsules on food
■ Fat soluble vitamin replacement
○ Chest physiotherapy
○ Vest therapy
● Respiratory infections
○ Monitor for
○ Treat with IV antibiotics
○ Prevent!
● Respiratory support
○ Monitor work of breathing
○ Oxygen as needed
● Bronchodilators
● Promote nutrition and growth
○ High calorie, high protein diet
○ Increased fluid intake
○ Monitor serial weights
○ Pancreatic enzymes
■ Give within 30 min of eating every meal and snack
■ Sprinkle capsules on food
■ Fat soluble vitamin replacement
71
New cards
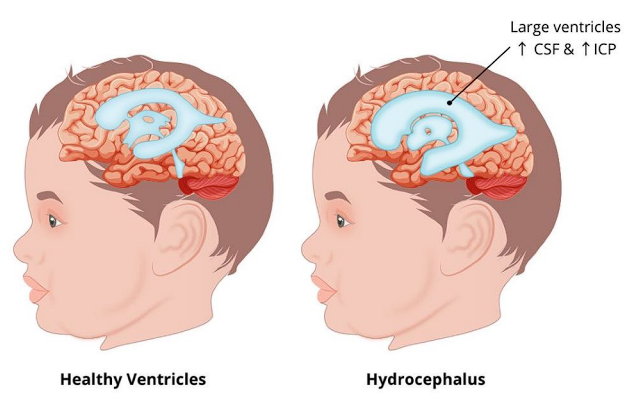
Hydrocephalus
● Increased accumulation of cerebrospinal fluid
● Increases ICP
● Causes:
○ Tumor
○ Hemorrhage
○ Infection
○ Congenital
● Increases ICP
● Causes:
○ Tumor
○ Hemorrhage
○ Infection
○ Congenital
72
New cards
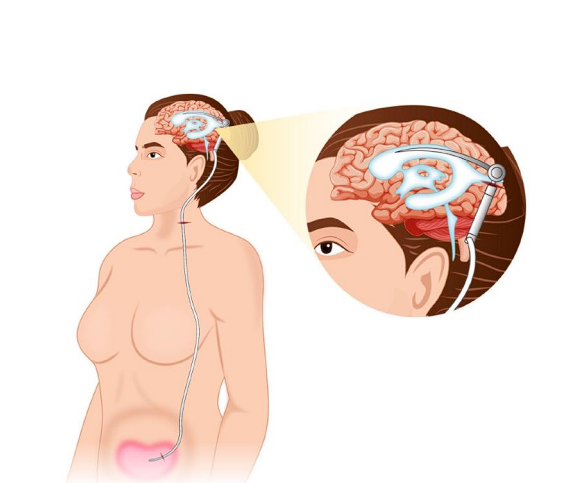
VP Shunt
○ Ventricle - Space in the brain
○ Peritoneum - Serous membrane lining the abdominal compartment
○ Shunt that drains extra CSF from brain to the abdomen, where it can then be excreted as urine.
○ Peritoneum - Serous membrane lining the abdominal compartment
○ Shunt that drains extra CSF from brain to the abdomen, where it can then be excreted as urine.
73
New cards
Cerebral Palsy
● Damage to immature brain- most often before birth
○ Pre/perinatal hypoxia or trauma
● Causes disorder in movement, muscle tone, and posture.
○ Pre/perinatal hypoxia or trauma
● Causes disorder in movement, muscle tone, and posture.
74
New cards
Cerebral Palsy Assessment Findings
● Movement/Coordination
○ Stiff muscles
○ Spasticity
○ Ataxia
○ Tremors
● Speech and Eating
○ Speech delays
○ Dysphagia
○ Difficulty speaking
○ Excessive drooling
● Development
○ Delayed motor skills
○ Intellectual disabilities
○ Delayed growth
○ Stiff muscles
○ Spasticity
○ Ataxia
○ Tremors
● Speech and Eating
○ Speech delays
○ Dysphagia
○ Difficulty speaking
○ Excessive drooling
● Development
○ Delayed motor skills
○ Intellectual disabilities
○ Delayed growth
75
New cards
Cerebral Palsy Tx
● No cure- focus is on symptom management
● Seizures
○ Anticonvulsants
● Spasticity
○ Muscle relaxants
● Growth + Development
○ PT
○ OT
○ SLP
● Seizures
○ Anticonvulsants
● Spasticity
○ Muscle relaxants
● Growth + Development
○ PT
○ OT
○ SLP
76
New cards
Defects in neural tube closure
● Development of the nervous system occurs early on in gestation
○ Develops from the neural tube
○ Low folic acid intake can impair neural tube development
__**● Spina Bifida**__
○ Failure of the vertebrae to close with protrusion of neural tube contents
***○ Meningocele (closed spina bifida)***
■ Protrusion of spinal fluid–filled meninges through a vertebral defect
***○ Myelomeningocele (open spina bifida)***
■ Protrusion of spinal fluid–filled meninges AND the spinal cord through a vertebral defect
○ Develops from the neural tube
○ Low folic acid intake can impair neural tube development
__**● Spina Bifida**__
○ Failure of the vertebrae to close with protrusion of neural tube contents
***○ Meningocele (closed spina bifida)***
■ Protrusion of spinal fluid–filled meninges through a vertebral defect
***○ Myelomeningocele (open spina bifida)***
■ Protrusion of spinal fluid–filled meninges AND the spinal cord through a vertebral defect
77
New cards
Defects in neural tube closure Assessment findings
● Paralysis possible
○ More likely the higher the defect is located on the spine
● Developmental delay
● Speech delay
● Intellectual disability
● Impaired coordination
● Sacral dimple or tuft of hair
○ More likely the higher the defect is located on the spine
● Developmental delay
● Speech delay
● Intellectual disability
● Impaired coordination
● Sacral dimple or tuft of hair
78
New cards
Defects in neural tube closure Tx
__**● Pre-op**__
○ Cover the sac with a moist, warm, sterile dressing
○ No diapering if defect is low- keep the sac clean with a protective barrier
○ Prophylactic antibiotics
○ Prone positioning
__**● Post-op**__
○ Remain prone until surgical site is healed
○ Family teaching
○ Cover the sac with a moist, warm, sterile dressing
○ No diapering if defect is low- keep the sac clean with a protective barrier
○ Prophylactic antibiotics
○ Prone positioning
__**● Post-op**__
○ Remain prone until surgical site is healed
○ Family teaching
79
New cards
Microcephaly
__**● Head circumference is smaller than normal**__
○ Brain did not develop properly or stopped growing.
__**● Causes**__
○ Genetic abnormalities
○ Drug or alcohol use during pregnancy
○ Virus during pregnancy
■ Cytomegalovirus
■ Rubella
■ Baricella
■ Zika
○ Brain did not develop properly or stopped growing.
__**● Causes**__
○ Genetic abnormalities
○ Drug or alcohol use during pregnancy
○ Virus during pregnancy
■ Cytomegalovirus
■ Rubella
■ Baricella
■ Zika
80
New cards
Microcephaly Assessment Findings
● Impaired cognitive development
● Delayed motor function
● Delayed speech development
● Facial distortion
● Dwarfism
● Hyperactivity
● Seizures
● Delayed motor function
● Delayed speech development
● Facial distortion
● Dwarfism
● Hyperactivity
● Seizures
81
New cards
Microcephaly TX
● Nothing will return the child’s head to normal size
● Focus: decrease impact of neurological complications
○ Physical therapy
○ Occupational therapy
○ Speech therapy
○ Control seizures with medications
● Focus: decrease impact of neurological complications
○ Physical therapy
○ Occupational therapy
○ Speech therapy
○ Control seizures with medications
82
New cards
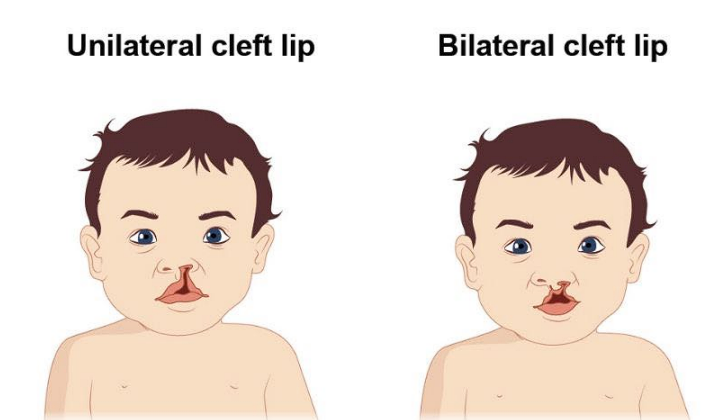
Cleft Lip
A congenital abnormality where there is a slip, or gap, in the upper lip on one or both sides.
83
New cards
Cleft Palate
A congenital abnormality where there is a split, or gap, in the hard palate (the roof of the mouth)
84
New cards
Cleft Palate Assessment
● Visible defect
● Monitor respiratory status
● Airway patency
● Nutritional status
● Weight gain
● Hydration
● Monitor respiratory status
● Airway patency
● Nutritional status
● Weight gain
● Hydration
85
New cards
Cleft Palate Management
● Surgically corrected
○ Cleft lip first at 3-6 months of age
○ Cleft palate second at 6-24 months of age
● Pre-operative care
○ Monitor for aspiration
○ Assess airway patency frequently
● Post-operative care
○ Positioning:
■ Position upright for feedings
■ Cleft palate - can be prone post op to help drain secretions
■ Cleft lip should NOT be prone as this could disturb the suture line
○ Protect suture line
○ Elbow restraints to avoid toddler putting things in the mouth that would compromise the sutures
○ No hard foods, straws, pacifiers, etc.
○ No oral or nasal suctioning
○ Cleft lip first at 3-6 months of age
○ Cleft palate second at 6-24 months of age
● Pre-operative care
○ Monitor for aspiration
○ Assess airway patency frequently
● Post-operative care
○ Positioning:
■ Position upright for feedings
■ Cleft palate - can be prone post op to help drain secretions
■ Cleft lip should NOT be prone as this could disturb the suture line
○ Protect suture line
○ Elbow restraints to avoid toddler putting things in the mouth that would compromise the sutures
○ No hard foods, straws, pacifiers, etc.
○ No oral or nasal suctioning
86
New cards
Feedings
● Specialized bottle to facilitate a good suction/latch
● Small, frequent feedings
● Upright position
● Burp frequently - will swallow a lot of air
● May take longer to feed than other children
● Monitor for aspiration
○ At risk for feeding to go out of their nose.
● Small, frequent feedings
● Upright position
● Burp frequently - will swallow a lot of air
● May take longer to feed than other children
● Monitor for aspiration
○ At risk for feeding to go out of their nose.
87
New cards
While assisting the intra-disciplinary team with interventions for a toddler who has just had a cleft palate repair, the nurse knows which of the following are appropriate? Select all that apply.
a. Pacifier with oral sucrose to reduce postoperative pain
b. Elbow restraints
c. Specialized bottle for feedings
d. Prone positioning
e. Oral suctioning
a. Pacifier with oral sucrose to reduce postoperative pain
b. Elbow restraints
c. Specialized bottle for feedings
d. Prone positioning
e. Oral suctioning
Answer: B, C, and D
A is incorrect. It is not appropriate to offer a toddler who is postoperative from a cleft palate repair a pacifier. This is because there is an incision with sutures in the palate of the mouth, and placing an object there could compromise the site. If the sutures break, the surgical site could open back up.
B is correct. Applying elbow restraints is an appropriate intervention for a toddler who has just had a cleft palate repair. Toddlers are often putting things in their mouths, and pulling on things. It is a priority to protect their sutures, and we do not want the toddler to be able to pull out the sutures or put anything in their mouth that would compromise the suture line. Therefore, elbow restraints are often needed and an appropriate intervention.
C is correct. Providing specialized bottles to the toddler who has completed their cleft palate repair will be very important for helping them establish feedings. It will be difficult for them to get good suction on a normal bottle, so specialized ones are needed.
D is correct. Prone positioning is appropriate for the infant with cleft palate repair post-operatively to aid in drainage of secretions and maintenance of a patent airway. E is incorrect. Oral suctioning should be avoided after a cleft palate repair as this could disturb the suture line.
A is incorrect. It is not appropriate to offer a toddler who is postoperative from a cleft palate repair a pacifier. This is because there is an incision with sutures in the palate of the mouth, and placing an object there could compromise the site. If the sutures break, the surgical site could open back up.
B is correct. Applying elbow restraints is an appropriate intervention for a toddler who has just had a cleft palate repair. Toddlers are often putting things in their mouths, and pulling on things. It is a priority to protect their sutures, and we do not want the toddler to be able to pull out the sutures or put anything in their mouth that would compromise the suture line. Therefore, elbow restraints are often needed and an appropriate intervention.
C is correct. Providing specialized bottles to the toddler who has completed their cleft palate repair will be very important for helping them establish feedings. It will be difficult for them to get good suction on a normal bottle, so specialized ones are needed.
D is correct. Prone positioning is appropriate for the infant with cleft palate repair post-operatively to aid in drainage of secretions and maintenance of a patent airway. E is incorrect. Oral suctioning should be avoided after a cleft palate repair as this could disturb the suture line.
88
New cards
Tracheoesophageal fistula (TEF)
A congenital abnormality in which there is an opening between the trachea and the esophagus
89
New cards
Esophageal atresia
Part of the esophagus does not form
90
New cards
Peds GI Tx
● Pre-operative
○ NPO
● Surgery
○ Repairs the opening
● Post-operative
○ Gradual oral nutrition
○ NPO
● Surgery
○ Repairs the opening
● Post-operative
○ Gradual oral nutrition
91
New cards
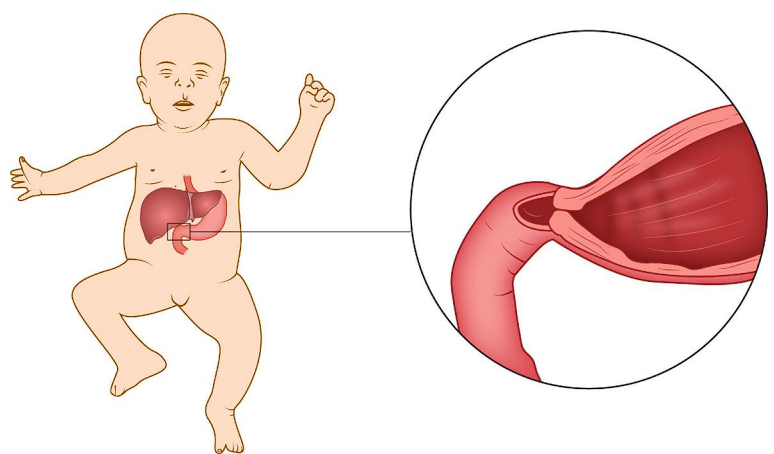
Pyloric stenosis
● Hypertrophy of the circular muscle fibers of the pylorus, with a severe narrowing of the lumen
92
New cards
Pyloric stenosis Assessment
● Vomiting
○ Non-bilious
○ Projectile
○ Right after feeding
○Infant is still hungry
● Dehydration
● Malnutrition
● Palpable pylorus
○ Non-bilious
○ Projectile
○ Right after feeding
○Infant is still hungry
● Dehydration
● Malnutrition
● Palpable pylorus
93
New cards
Pyloric stenosis Tx
● Correct dehydration
● Pyloromyotomy
● Nutrition after surgery
● Pyloromyotomy
● Nutrition after surgery
94
New cards
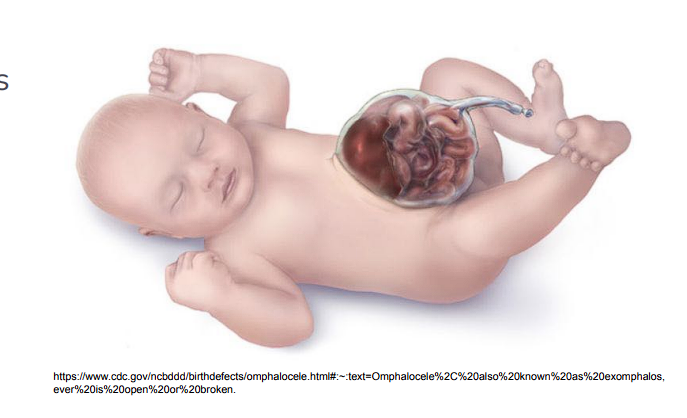
Omphalocele
● Congenital abnormality where the abdominal contents protrude through the umbilicus while remaining in the peritoneal sac.
● Occurs during weeks 9-10 of gestation.
● Usually diagnosed on a prenatal ultrasound.
● Occurs during weeks 9-10 of gestation.
● Usually diagnosed on a prenatal ultrasound.
95
New cards
Omphalocele Assessment
● Visible defect
● Some infants have only the omphalocele
● Some also have cardiac defects
● Lung size can be affected
● Some infants have only the omphalocele
● Some also have cardiac defects
● Lung size can be affected
96
New cards
Omphalocele Complications
● Hypothermia
● Dehydration
● Sepsis
● Dehydration
● Sepsis
97
New cards
Omphalocele Management
__**Pre-op**__
● Keep exposed intestines moist
● Cover with sterile gauze soaked in saline
● IV fluids
● IV antibiotics
● Thermoregulation
__**Post-op**__
● Parenteral feeds
● Trophic feeds started enterally very gradually
● Monitor weight
● Very long hospital stay
● Keep exposed intestines moist
● Cover with sterile gauze soaked in saline
● IV fluids
● IV antibiotics
● Thermoregulation
__**Post-op**__
● Parenteral feeds
● Trophic feeds started enterally very gradually
● Monitor weight
● Very long hospital stay
98
New cards
The nurse observes a parent swaddling their infant with an unrepaired omphalocele. Which of the following statements would be appropriate?
a. “Stop, you’ll kill your baby!!”
b. “That is a nice, tight swaddle. It will really help sooth your new baby”
c. “May I help you? We will need to be careful with their intestines, we do not want the swaddle to push them back inside.”
d. “Swaddling is not allowed for these babies, please stop.”
a. “Stop, you’ll kill your baby!!”
b. “That is a nice, tight swaddle. It will really help sooth your new baby”
c. “May I help you? We will need to be careful with their intestines, we do not want the swaddle to push them back inside.”
d. “Swaddling is not allowed for these babies, please stop.”
Answer: C
A is incorrect. This is inappropriate to say to a parent as it would cause panic and upset them. The nurse wants to promote the parent bonding with their infant, and phrases like this will scare the parent and make them afraid to touch the baby, which is not therapeutic.
B is incorrect. It is not appropriate to tightly swaddle an infant with an omphalocele. This would place pressure on their exposed intestines and could push them back inside of the baby, which we do not want.
C is correct. This is a therapeutic statement. It educates the parent about the need to swaddle the baby only very loosely, and avoid any pressure on the exposed intestines so that they do not get putheyd back inside of the baby. It also promotes bonding with the infant, as it encourages the parent to touch and care for their baby.
D is incorrect. This is not appropriate. Swaddling is not ideal for an infant with an omphalocele due to the exposed intestines, but if it is done loosely and avoids placing pressure on the defect it can certainly be done. Telling the parent to stop will not promote bonding and decrease their interaction with the baby. The nurse should educate the parent on the necessary precautions when traveling and help them develop a positive relationship with their new baby.
A is incorrect. This is inappropriate to say to a parent as it would cause panic and upset them. The nurse wants to promote the parent bonding with their infant, and phrases like this will scare the parent and make them afraid to touch the baby, which is not therapeutic.
B is incorrect. It is not appropriate to tightly swaddle an infant with an omphalocele. This would place pressure on their exposed intestines and could push them back inside of the baby, which we do not want.
C is correct. This is a therapeutic statement. It educates the parent about the need to swaddle the baby only very loosely, and avoid any pressure on the exposed intestines so that they do not get putheyd back inside of the baby. It also promotes bonding with the infant, as it encourages the parent to touch and care for their baby.
D is incorrect. This is not appropriate. Swaddling is not ideal for an infant with an omphalocele due to the exposed intestines, but if it is done loosely and avoids placing pressure on the defect it can certainly be done. Telling the parent to stop will not promote bonding and decrease their interaction with the baby. The nurse should educate the parent on the necessary precautions when traveling and help them develop a positive relationship with their new baby.
99
New cards
Intussusception
● Occurs when one part of the intestine slips inside the other intestine
● “Telescoping”
● Often occurs where the small intestine and large intestine meet.
● “Telescoping”
● Often occurs where the small intestine and large intestine meet.
100
New cards
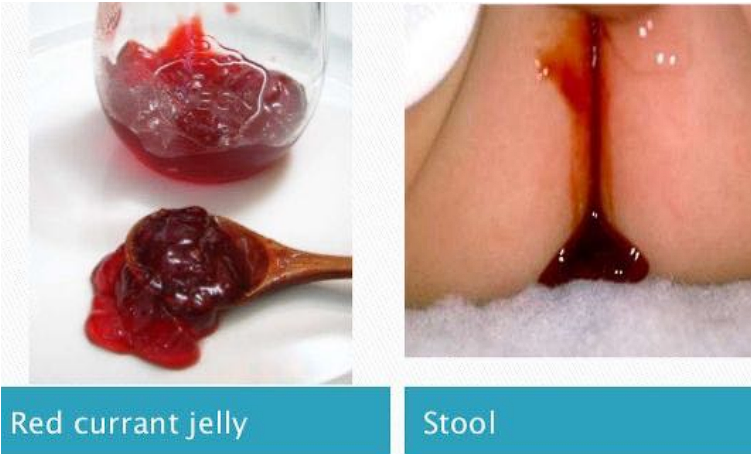
Intussusception Assessment
● Red currant jelly stools
● Cyclical abdominal pain
● Nausea
● Vomiting
● Green, bilious emesis
● Sausage-shaped mass in abdomen
● Cyclical abdominal pain
● Nausea
● Vomiting
● Green, bilious emesis
● Sausage-shaped mass in abdomen