hormones and homeostasis
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
hormone → definition
a chemical substance produced in minute amounts by glands, carried by the blood, which alters the activity or one or more specific target organs and is eventually broken down by the liver
hormones
together with the nervous system help to coordinate various activities within the body
made of either protein or steroids (lipid)
some are also involved in homeostasis
exocrine glands
glands with ducts
produce a secretion that is carried by the duct
e.g.: the salivary gland has a duct that carries the saliva to the buccal cavity
endocrine glands
ductless glands produce hormones and secrete them directly into the bloodstream
the blood then carries the hormone to the target organ or tissues
endocrine system
some glands produce only hormones and are hence purely endocrine glands
e.g.: testes: secrete testosterone into the bloodstream which then distributes it to the rest of the body
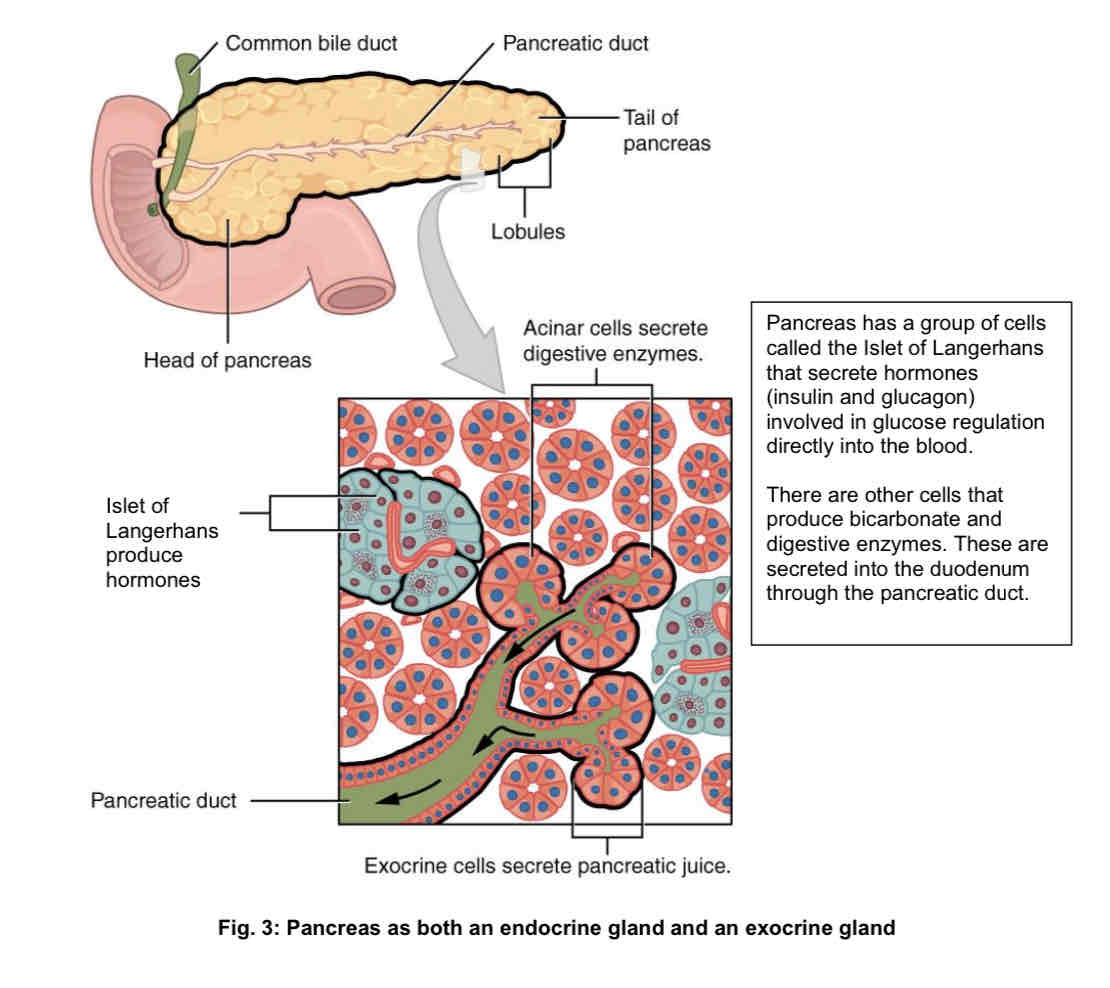
pancreas produce hormones (insulin and glucagon) as well as pancreatic juice → both an endocrine and an exocrine gland
pancreas as both a endocrine and exocrine gland
a group of cells called the islet of langerhans: secrete hormones (insulin and glucagon) involved in glucose regulation directly into the blood.
there are other cells that produce bicarbonate and digestive enzymes. These are secreted into the duodenum through the pancreatic duct
endocrine glands → example
hypothalamus produces ADH, pituitary gland stores and releases ADH
pancreas (islets of Langerhans)
hypothalamus produces ADH, pituitary gland stores and releases ADH
hormone: anti-diuretic hormone (ADH)
function: osmoregulation
target organ(s): walls of collecting duct of kidney nephron
pancreas (islets of Langerhans)
hormone: insulin and glucagon
function: blood glucose regulation
target organ(s):
insulin: liver and muscle cells
glucagon: liver cells only
homeostasis → definition
the maintenance of a constant internal environment
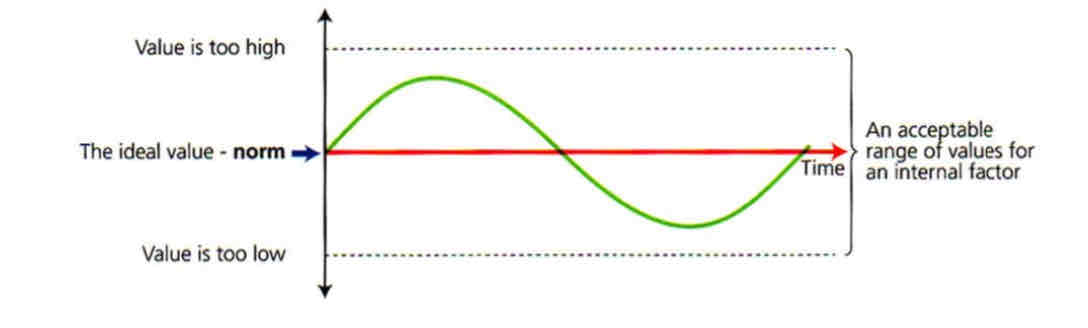
importance of homeostasis
ensures a stable internal environment in the organism, with minimal unavoidable disturbances
allow the organism to function:
more efficiently as cells are maintained in an internal environment with optimal conditions
with a degree of independence from the external environment as the organism is not adversely affected by changes in the external environment
examples in the body
regulation of blood glucose concentration
temperature regulation
regulation of blood plasma water potential
internal environment
cellular level
tissue level
cellular level
composed of cytoplasm, whose constituents are controlled by:
the cell membrane
this partially permeable membrane permits only certain molecules and ions to enter and leave.
the rates at which molecules are exchanged are controlled by diffusion gradients, osmotic gradients and active transport mechanisms
enzyme activity, which is controlled by the rate of protein synthesis
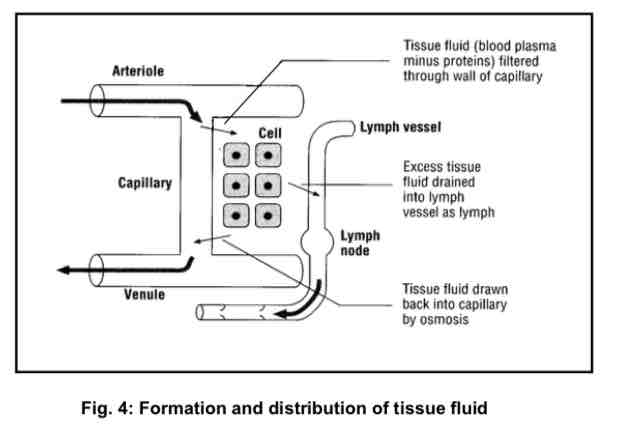
tissue level
the immediate environment surrounding cells of multicellular organisms is the extracellular fluid. In mammals → tissue fluid
tissue fluid fills the space between cells (intercellular spaces) → formed when the higher blood pressure at the arterial ends of the capillaries forces blood plasma out of the capillaries
tissue fluid = blood plasma minus proteins
it provides cells with the medium in which they live
features of the internal environment to be kept constant
temperature
pH
concentration of respiratory gases (oxygen and carbon dioxide)
concentration of essential molecules e.g. glucose
concentration of ions (which affect the water potential)
concentration of toxic substances e.g. nitrogenous waste products that arise from protein metabolism
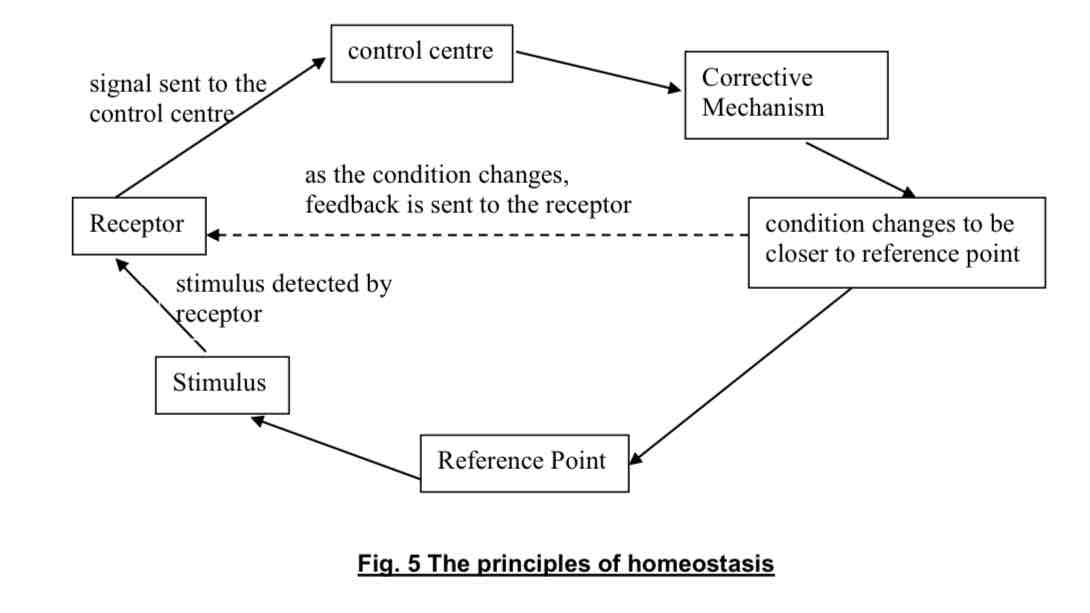
components of homeostatic control system
reference point/set point represents the optimal level in a homeostatic control system
consists of:
receptor
control centre
effector
receptor
detects the stimulus (any change or deviation) from the reference point
this information is then relayed to the control centre
control centre
information is compared with the reference point
if there is a deviation, the control centre sends an appropriate signal to the effector
effector
serves to carry out the appropriate response based on the signal received from the control centre
the response from the effector counteracts the initial change/ deviation which results in an effect (new stimulus) that is picked up by the receptor
this information is relayed to the control centre and returns the system to normal, optimal conditions after comparison against the reference point → negative feedback
principles of homeostasis
can be achieved through negative feedback → mechanism that counteract changes in the internal environment and restores it to the reference point
for negative feedback to take place:
reference point to be maintained
stimulus → change in the internal environment
receptor to detect the stimulus
self-regulatory corrective mechanism to bring about the reverse effect of the stimulus
importance of regulating blood glucose level
glucose is the ideal substrate for cellular respiration → the preferred fuel molecule for both cardiac and skeletal muscle’s
is the only metabolic fuel molecule used by the brain → a drastic decrease in blood glucose level could lead to fainting, convulsions, coma and finally death
regulation of blood glucose level
regulated by 2 hormones secreted from the islets of Langerhans of the pancreas:
glucagon is secreted from the alpha (α) cells and helps increase blood glucose concentration
insulin is secreted from the beta (β) cells and helps decrease blood glucose concentration
normal level of blood glucose is about 90 mg/ 100 ml of blood (fluctuating between 70 mg and 150 mg)
glucagon and insulin operate antagonistically → oppose the actions of the other
e.g. glucagon stimulates the breakdown of glycogen to glucose while insulin promotes the conversion of excess glucose to glycogen.
response to a rise in blood glucose levels
Blood glucose levels increase above the reference point of around 90 mg/ 100 ml (stimulus).
The rise in blood glucose level is detected by islets of Langerhans (receptor) in pancreas.
This triggers the secretion of insulin (signal) by the β-cells of the islets of Langerhans of the pancreas. (control centre)
Insulin will be transported by the blood to the liver and muscles (effectors).
Insulin secreted in the blood stream causes the following responses:
Increases permeability of cell membranes to glucose, thus increasing rate of uptake of glucose from the blood by cells
Increases rate of cellular respiration – increases the rate of oxidation of glucose in cells
Stimulates liver and muscle cells to convert excess glucose to glycogen for storage (process is known as glycogenesis).
Decreased break down of glycogen to glucose.
These actions decrease blood glucose concentration until it returns to the reference point (negative feedback).
This return to reference point is detected by the β-cells of the islets of Langerhans, which in turn, decreases secretion of insulin.
The circulating insulin is broken down in the liver and excreted by the kidneys.
response to a fall in blood glucose levels
Blood glucose levels decrease below the reference of around 90mg/100ml (stimulus).
The fall in blood glucose level is detected by islets of Langerhans (receptor) in pancreas.
This triggers the secretion of glucagon (a hormone,) by the α-cells in the islets of Langerhans of the pancreas. (control centre)
Glucagon will be transported by the blood to the liver. (signal)
Glucagon triggers the following response in the liver: (effector)
Stimulates conversion of stored glycogen back to glucose in the liver
Conversion of non-carbohydrate sources such as pyruvate, amino acids and glycerol to glucose in the liver (this is known as gluconeogenesis)
Glucose is released into the blood stream, hence increasing blood glucose concentration until it returns to reference point. (negative feedback)
This return to reference point is detected by the α-cells of the islets of Langerhans, which in turn, decreases secretion of glucagon.
The circulating glucagon is broken in the liver and excreted by the kidneys.
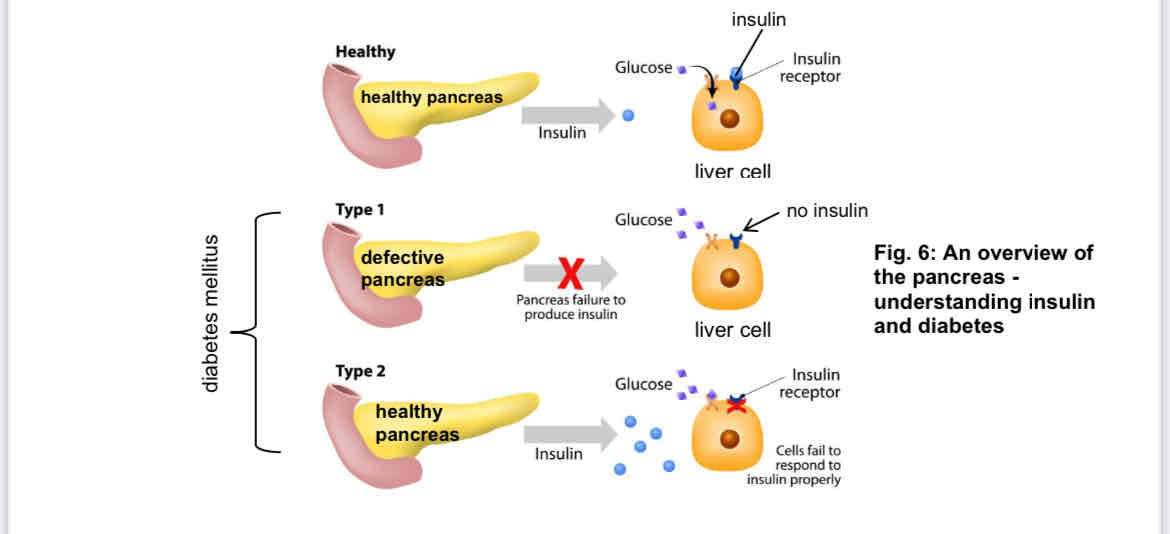
what if there’s not enough insulin
diabetes mellitus
type 1 diabetes → pancreas fails to produce enough insulin
type 2 diabetes → person’s body cells no longer respond to insulin produced by the pancreas
signs and symptoms: increase in blood glucose, glucose found in urine, excessive thirst and urination, tiredness, loss of weight
treatment
injection of insulin (for Type 1 only)
controlled diet and exercise
taking medicine (e.g Metformin lowers glucose production in the liver and increases body’s sensitivity to insulin)
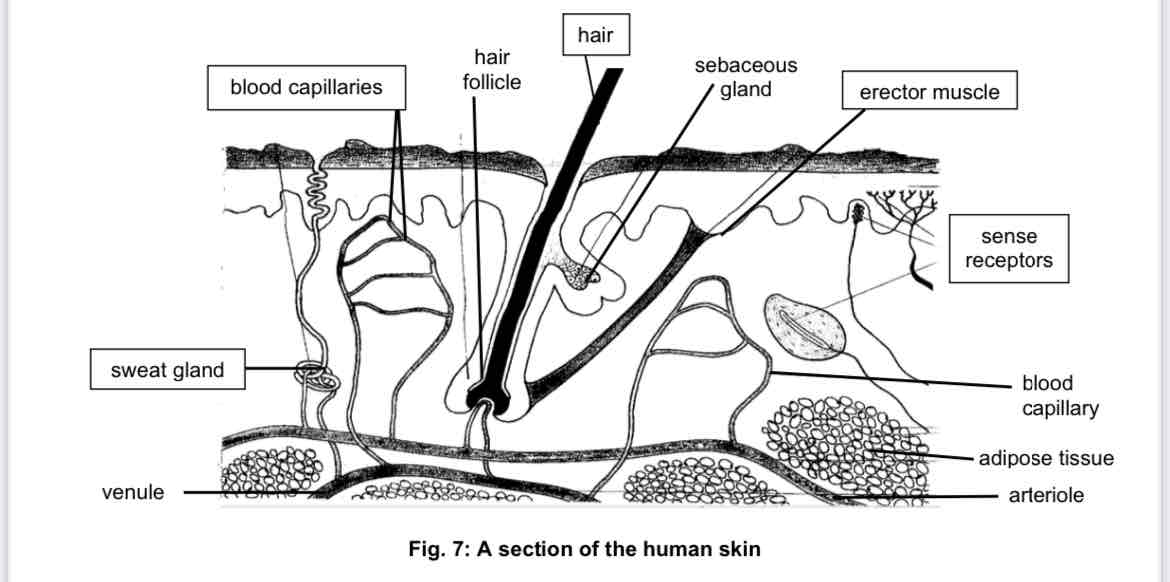
mammalian skin
forms a protective covering over the body surface
acts as an excretory organ as well as a regulator of body temperature
consists of:
hairs, sweat glands, temperature receptors, blood vessels and fatty tissue
importance of temperature regulation
enzymes in the body can only work within a certain range of temperature
changes in the body temperature may result in enzyme inactivation or even denaturation
the body maintains a constant internal temperature by regulating heat gain and heat loss
heat is gained through the external environment and metabolic activities
heat is lost through radiation, convection and conduction of heat from the skin; evaporation of sweat from the skin and exhalation; and through defecation and urination.
rise in temperature
A rise in bodily temperature can be due to:
Increase in temperature in the external environment: on a warm day, the rate of heat loss from the body is reduced OR heat is absorbed from a warmer external environment.
In both cases, thermoreceptors in the skin detect a rise in external temperature and nerve impulses are sent to the hypothalamus.
Increase in temperature in the internal environment: when you perform vigorous muscular activities, a great deal of heat is produced OR when you consume hot beverages or food.
A rise in blood temperature is directly detected by the thermoreceptors in the hypothalamus when warmer blood flows through it.
The hypothalamus will send out nerve impulses to the relevant body parts where corrective processes occur to restore the temperature back to normal.
Homeostasis of temperature is controlled by nerve impulses, and not by hormone
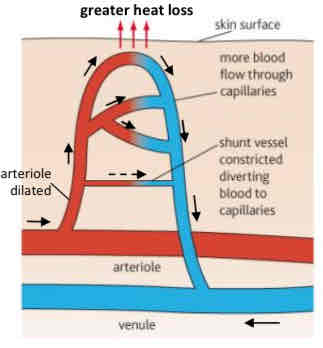
response to rise in temperature
arterioles in the skin dilate (vasodilation) while shunt vessels constrict to allow more blood to flow through blood capillaries under the skin surface
more heat is lost through the skin by radiation, convection and conduction
sweat glands become more active; increased production of sweat
as more sweat evaporates from the surface of the skin, more latent heat of vaporisation is removed from the body
the metabolic rate of the body slows down, thus less heat is produced within the body
these processes decrease blood temperature until it returns to the reference point.
This return to reference point is detected by the thermoreceptors.
The removal of the stimulus will stop the homeostatic action.
fall in temperature
On a cold day, the rate of heat loss is increased, especially at the skin surface.
A drop in external temperature is detected by the temperature receptors in the skin which then send nerve impulses to the brain.
In the brain, the hypothalamus sends out nerve impulses to the relevant body parts.
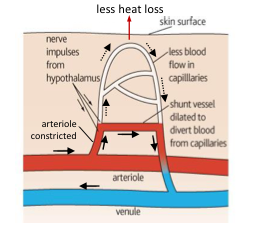
response to fall in temperature
arterioles in the skin constrict (vasoconstriction) and shunt vessels dilate to allow less blood to flow through blood capillaries under the skin surface
less heat is lost through the skin by radiation, convection and conduction
sweat glands become less active, and the production of sweat decreases ⇒ less latent heat of vaporisation is lost from the body
the metabolic rate of the body increases, thus more heat is produced within the body
sometimes the above reactions are not sufficient to prevent a drop body temperature ⇒ shivering (a reflex) occurs
the spasmodic contraction of the muscles increases heat production
these actions increase blood temperature until it returns to reference point
this return to normal is detected by the thermoreceptors; the removal of the stimulus will stop the homeostatic action
regulation of blood plasma water potential
The water potential of blood depends on the amount of water and salts in the plasma.
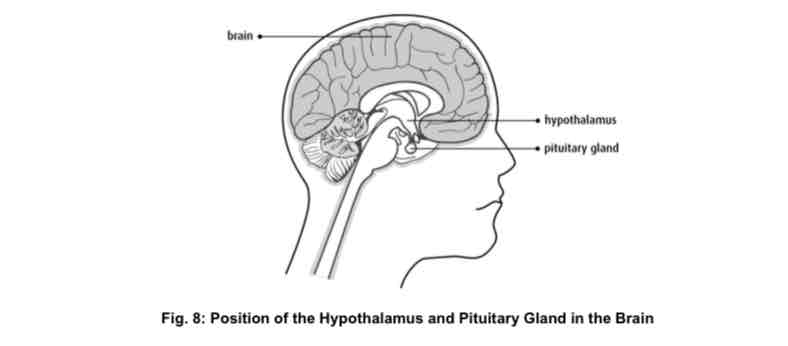
There are special receptor cells in the hypothalamus of the brain called osmoreceptors.
Osmoreceptors are sensitive to changes in water potential of the blood.
The amount of water in the blood plasma is controlled by anti-diuretic hormone (ADH).
ADH is produced by the hypothalamus in the brain and is released by the pituitary gland. It causes an increase in water reabsorption at the kidney tubules.
importance of blood plasma water potential regulation
Any drastic change in water potential will affect the cells in the body.
If the blood plasma is too dilute, water molecules will enter the cells by osmosis. The cells will swell and burst.
If blood plasma is too concentrated, water molecules will move out of the cells by osmosis. The cells will become dehydrated, shrink and are thus unable to carry out their metabolic functions.
The composition of tissue fluid must be kept within very narrow limits. This ensures that tissue fluid is kept at a constant water potential
response to rise in the blood plasma water potential
When water potential in the blood plasma increases above the reference point (e.g. large intake of water/ drinking), osmoreceptors in the hypothalamus detect the change and stimulates the pituitary gland.
Pituitary gland releases less ADH into the bloodstream, causing the walls of the distal convoluted tubule and collecting duct to be less permeable to water.
Kidney tubules reabsorb less water back into the blood capillaries.
More urine is produced. Urine is also more dilute.
These actions decrease the water potential of blood plasma until it returns to the reference point.
This return of water potential to reference point is detected by the osmoreceptors. Secretion of ADH returns to norm.
response to fall in blood plasma water potential
When water potential in the blood plasma decreases to below the reference point (e.g. loss of water through sweating), osmoreceptors in the hypothalamus detect the change and stimulates the pituitary gland.
Pituitary gland releases more ADH into the bloodstream. ADH makes the walls of the distal convoluted tubule and collecting duct more permeable to water.
Kidney tubules reabsorb more water back into the blood capillaries.
Less urine is produced. Urine is also more concentrated.
These actions increase the water potential of blood plasma until it returns to normal levels.
This return of water potential of blood plasma to reference point is detected by the osmoreceptors. The increased secretion of ADH stops.