Immunity Infection Medications
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
What are the two main classifications of antibiotics?
Broad-spectrum and narrow-spectrum
What do broad-spectrum antibiotics do?
Kill a wide variety of bacteria, including normal flora in the gut, mouth, and vagina
What risks are associated with broad-spectrum antibiotics?
Opportunistic infections and superinfections like C. diff
What do narrow-spectrum antibiotics do?
Target specific bacteria; preferred when the organism is known
Why is a culture & sensitivity (C&S) done before starting antibiotics?
To identify the organism and determine which antibiotic it is sensitive to. Antibiotics started before C&S can skew the results
What is the purpose of starting broad-spectrum antibiotics before C&S results are back?
To begin treatment while waiting for results (takes 48–72 hours)
What happens once C&S results are available?
Broad-spectrum antibiotics are stopped, and narrow-spectrum antibiotics are started
What does bactericidal mean?
Kills bacteria; preferred for serious infections and immunocompromised patients
What does bacteriostatic mean?
Inhibits bacterial growth; relies on the immune system to eliminate bacteria
Can a drug be both bacteriostatic and bactericidal?
Yes, depending on the organism
What is MIC?
Minimum inhibitory concentration. The lowest concentration of an antibiotic that prevents visible bacterial growth
Is a high or low MIC better?
Low MIC is better—it means the antibiotic is effective at low doses
What increases MIC/resistance risk?
Not completing the full prescribed course of antibiotics
Key teaching point for patients taking antibiotics?
Take the full prescribed dose for the full amount of time
Common GI side effects of antibiotics?
Nausea, vomiting, diarrhea, gastritis (inflammation of the stomach)
What is a superinfection?
A new infection (like C. diff) that occurs while treating another infection
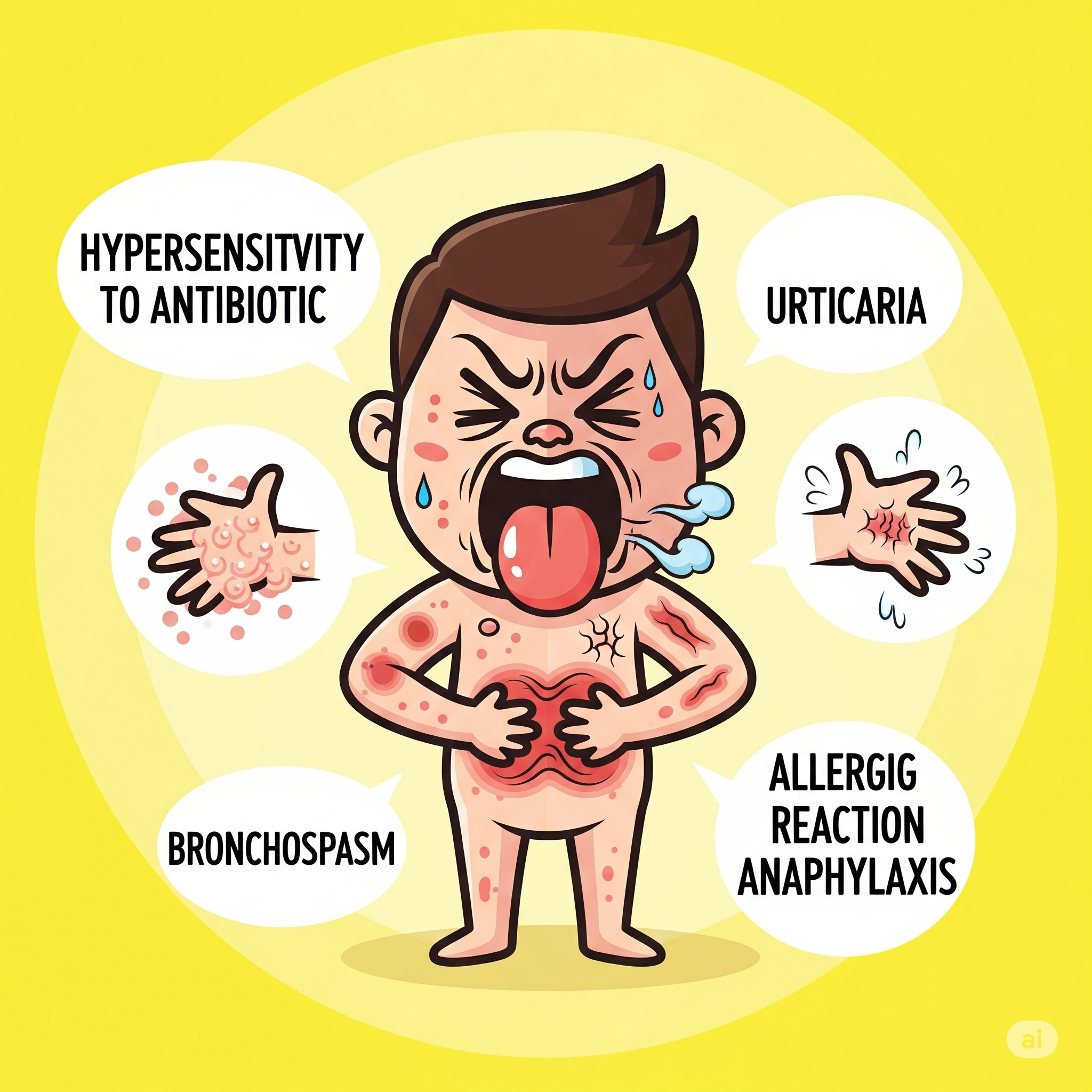
What are signs of hypersensitivity to antibiotics?
Redness, hives (urticaria), bronchospasm, anaphylaxis
How is C. diff diarrhea different from typical antibiotic-related diarrhea?
It's very watery, has a distinct smell, happens 10–15 times/day, and is highly contagious
What can help prevent superinfections like C. diff?
Taking probiotics to restore normal gut flora
What is the mechanism of beta-lactam antibiotics?
Bind to bacterial cell wall proteins → inhibit wall synthesis → cell death
What are the four classes of beta-lactam antibiotics?
Penicillins, cephalosporins, carbapenems, monobactams
What’s important about beta-lactam cross-sensitivity?
Allergy to one (e.g., penicillin) means risk of allergy to others in the group
Are penicillins (Ampicillin (Principen) broad or narrow spectrum?
Broad spectrum (e.g., ampicillin)
Are penicillins (Ampicillin (Principen) bacteriostatic or bactericidal?
Bactericidal
What are penicillins (Ampicillin (Principen) commonly used for?
GU, GI, skin, soft tissue, and respiratory infections
How are penicillins (Ampicillin (Principen) excreted?
Largely by the kidneys.
Why should we use caution with penicillins (Ampicillin (Principen) in renal impairment?
Accumulation can increase toxicity; monitor BUN and creatinine.
Normal BUN and Creatinine values?
BUN: 7–21 mg/dL
Creatinine: 0.6–1.2 mg/dL
Penicillin routes of administration?
PO, IM, IV.
What are common adverse effects of penicillins (Ampicillin (Principen)?
Hypersensitivity (hives/anaphylaxis)
Nephropathy (proteinuria, oliguria)
GI: nausea, vomiting, diarrhea, gastritis
Describe the kidney-related reaction to penicillin.
Allergic reaction → inflammation in kidney tubules → damage → less pee (oliguria) and protein in urine (proteinuria)
What to assess before giving penicillin?
Allergy history (e.g., hives, throat tightness, shortness of breath)
When should PO penicillin be given?
On an empty stomach (1 hour before or 2 hours after meals).
What should you encourage patients taking penicillin to do?
Drink plenty of water to help flush the kidneys.
IM Penicillin (Ampicillin (Principen) administration tip?
Use a large muscle for injection.
When should you notify the provider while on penicillin (Ampicillin (Principen)?
If the patient develops diarrhea—could indicate C. diff.
Is penicillin (Ampicillin (Principen) safe in breastfeeding women?
Yes
What class are cephalosporins (Cefazolin (Ancef) part of and what is their mechanism of action?
Cephalosporins (Cefazolin (Ancef) are beta-lactam antibiotics with a mechanism of action similar to penicillins; they inhibit bacterial cell wall synthesis
Are cephalosporins bacteriostatic or bactericidal?
Bactericidal
How are cephalosporins classified and which generation is more active against gram-negative bacteria?
Classified into 5 generations; later generations (3rd, 4th, 5th) are more effective against gram-negative organisms
What is the prototype of first-generation cephalosporins and what is it commonly used for?
Cefazolin (Ancef); used for surgical prophylaxis due to good tissue penetration, long half-life, low cost, and low side effects
When must cefazolin be administered for surgery scheduled at 10:00 am?
By 9:00 am (1 hour before first incision)
What route is cefazolin commonly given through?
IV (most common), sometimes IM
What are key contraindications or adverse effects of cephalosporins?
Milk allergy (cross-reactivity due to protein structure), C. diff, nephrotoxicity (kidney damage), bleeding risk (interferes with vitamin K), and should not be taken with calcium
Which drugs increase the risk of nephrotoxicity when combined with cephalosporins?
Aminoglycosides, vancomycin, and furosemide
What is the prototype carbapenem and what’s the role of cilastatin in it?
Imipenem-cilastatin (Primaxin); cilastatin protects imipenem from being rapidly degraded by kidneys
What are carbapenems (Imipenem-cilastatin (Primaxin) used to treat?
Lower respiratory, urinary, intra-abdominal infections, endocarditis, septicemia
How is imipenem-cilastatin administered and what are adverse effects?
IV only. Adverse effects: hypersensitivity, nephropathy (oliguria, proteinuria), GI upset
What is a major contraindication for carbapenems (Imipenem-cilastatin (Primaxin)?
Allergy to carbapenems or penicillins (cross-sensitivity)
What is the prototype monobactam and it’s spectrum?
Aztreonam (Azactam); used for gram-negative bacteria only
What infections is aztreonam used to treat?
UTIs, lower respiratory tract, skin infections
What are adverse effects of monobactam (Aztreonam)?
Rash, diarrhea (C. diff risk), N/V, thrombophlebitis (inflammation of a vein so rotate IV sites)
What is a key contraindication of monobactam (Aztreonam)?
Hypersensitivity to monobactam (Aztreonam)
What is the prototype aminoglycoside and its target bacteria?
Gentamicin (Garamycin); targets gram-negative aerobes like Pseudomonas, E. coli
What’s important about trough levels when administering aminoglycosides (Gentamicin (Garamycin)?
Trough must be drawn before the 3rd dose and results known before giving the dose to avoid toxicity
What is the MOA of aminoglycosides (Gentamicin (Garamycin)?
Inhibits bacterial protein synthesis by binding to ribosomes
What are the main uses of gentamicin?
Serious gram-negative infections: septicemia, UTIs, RTIs, osteomyelitis (inflammation in bones), intra-abdominal
What are the black box warnings for aminoglycosides (Gentamicin)?
Nephrotoxicity (BUN, Cr), ototoxicity (vertigo, tinnitus, hearing loss), especially in older adults
What are nursing considerations for aminoglycosides (Gentamicin)?
Monitor peak/trough, renal function, avoid combining with penicillins in IV line (inactivates), do not mix with skeletal muscle relaxants (risk for respiratory arrest)
What is the prototype fluoroquinolone and what bacteria does it cover?
Ciprofloxacin (Cipro); covers gram-negative and some gram-positive bacteria
What is ciprofloxacin’s MOA?
Inhibits bacterial DNA synthesis enzymes
What are its major uses?
Sinusitis, respiratory, GI, GU, bone, joint, skin infections. First line for anthrax exposure.
What are the major black box warnings for Fluoroquinolone (Ciprofloxacin)?
Tendonitis, Achilles tendon rupture, seizures, cardiac effects, peripheral neuropathy (nerve damage), dermatologic reactions
What are nursing considerations for Fluoroquinolone (Ciprofloxacin)?
Avoid in seizure patients.
Avoid sun (photosensitivity).
Do not take with dairy or antacids (wait 2 hrs).
Ensure hydration.
Monitor for tendonitis and tendon rupture symptoms.
Which mechanism of action applies to penicillin?
A. Prevents reproduction of the pathogen
B. Inhibits cell wall synthesis of the pathogen
C. Inhibits nucleic acid synthesis of the pathogen
D. Injuries the cytoplasmic membrane of the pathogen
Inhibits cell wall synthesis of the pathogen
A client has been admitted to the hospital for osteromyelitis
The client’s labs”
Blood, urea, nitrogen (BUN): 38 mg/dL
Creatinine (Cr): 2.1 mg/dL
Which medication should the nurse question adminstering?
A. Ciprofloxacin (cipro) 500 mg by mouth every 12 hours
B. Gentamicin (Garamycin) 1 gram IV every 12 hours
C. Cefepine maxipime 1 gram IV every 12 hours
D. Ceftraoline teflaro 200 mg IV every 12 hours
Gentamicin (Garamycin) 1 gram IV every 12 hours
The client’s BUN/Cr is already high so the nurse would question administering an aminoglycoside like gentamicin (Garamycin) that has a black box warning of nephrotoxicity. Fluroquinolones like cipro and cephalosporins like cefepime and cefpime are non nephrotoxic