5. Diagnostics, therapy, and prevention of forestomach/abomasum diseases
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
Simple indigestion
Acute and chronic ruminal acidosis
Ruminal alkalosis
Bloat
Hoflund syndrome
Traumatic reticuloperitonitis
Ruminal drinking
Ruminal parakeratosis
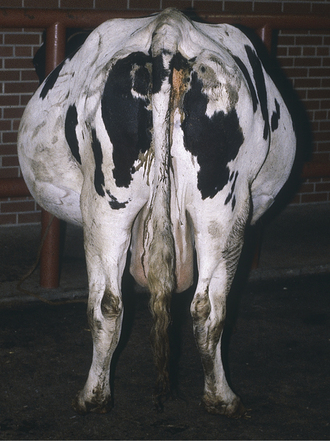
Abomasal displacement (left and right)
Volvulus
Impaction
Ulcers
Excessive intake of highly fermentable carbohydrates (decrease acetic acid, increase propionic acid) causing pH decrease
Decreased pH → Lactobacillus overgrowth → lactic acid build-up (+increased VFA and decreased salivation) → ruminal stasis → water influx → hypovolaemia, circulatory shock, metabolic acidosis → shock → death
How is acute ruminal acidosis diagnosed?
Milky grey ruminal fluid, acidic odour, pH <5, elevated blood lactate and phosphate, hypocalcaemia
How is acute ruminal acidosis treated?
Ruminal lavage, sodium bicarbonate, electrolytes, antacids, correct acidosis and dehydration
What is chronic ruminal acidosis?
Periods of low ruminal pH (5.2-5.6) due to high fermentable carbohydrate intake and low fibre
What is the cause of chronic ruminal acidosis?
Ingestion of diets high in rapidly fermentable carbohydrates and/or deficient in physically active fibre.
Parakeratosis: increased thickness and cornification of ruminal epithelium that reduces absorption.
Rumenitis and liver abscesses: ulceration is caused by endotoxins of bacteria. Ulcers allow bacteria to access to portal circulation and reach the liver, forming abscesses.
Low-fat milk syndrome: the shift in VFA initiates insulin secretion that inhibits lipolysis.
Cerebrocortical necrosis: acidosis leads to thiamine deficiency Without thiamine there will be oedema and haemorrhages in the brain, as well as lysis of cortex.
Laminitis: LPS produce histamine, cause vasodilation and increase blood pressure so more blood is accumulated in the hooves.
Bone demineralization: ions are released from bone, causing osteoporosis + milk fever
Clinical signs: Reduced feed intake, decreased milk production, reduced fat, poor body condition, and unexplained diarrhoea. High rates of culling or unexplained deaths may be noted in the herd.
How is chronic ruminal acidosis diagnosed and prevented?
Diagnosis: ruminal pH measurement;
Prevention: proper diet, slow adaptation to high-grain diets, dietary buffers
Urea converts to ammonia, raising pH, with rapid ammonia absorption leading to toxicity (brain, liver)
How is acute ruminal alkalosis diagnosed?
Rumen fluid (pH >7, content dark grey and putrid)
How is acute ruminal alkalosis treated?
Rumen lavage, IV saline, acetic acid orally, oral VFAs
How is acute ruminal alkalosis prevented?
Adequate dietary mixing of urea or slow introduction.
What are the types of bloat?
Primary (foam bloat), secondary (free-gas bloat)
What is the pathogenesis of primary acute ruminal tympany?
Legumes contain pectic substances → pectin → polygalacturonic acid and pectic acid, which cause jellification of the rumen content → increase the rumen fluid viscosity → inhibition of eructation.
Oesophageal obstruction, failure of oesophageal groove function, nerve damage, or muscular motility disorders
What are clinical signs of acute ruminal tympany?
Left abdominal distension, dyspnoea, hypersalivation, distress, rapid death within 3–4 hours

How is acute ruminal tympany diagnosed?
Clinical signs, clinical examination- free gas produces a higher pitched ping on percussion than frothy bloat. The distention of the rumen can be detected on rectal examination. Examination of oesophageal patency, urinalysis, CRT, blood analysis (pH, urea, calcium)
What are differential diagnoses for acute ruminal tympany?
Abomasal displacement, hoflund syndrome, caecum dilation, uterine hydrops, subcutaneous emphysema
What are examples of antifoaming agents to treat float?
Vegetable oils (e.g., peanut, corn, soybean) and mineral oils (paraffins)
What are causes of chronic tympany?
Hoflund, listeria, tetanus, botulism, foreign body, reticular or liver abscess, abomasal volvulus, diaphragmatic hernia, omasum impaction, lymphosarcoma
How is chronic tympany diagnosed?
History, clinical exam, sonography, explorative laparotomy, laparoscopy
What is the treatment for chronic tympany?
Depends on aetiology DO NOT RISK ruminitis - rather slow and perfect treatment
What is ruminal drinking?
Failure of the reticular groove reflex causing milk to enter the rumen, leading to ruminal acidosis
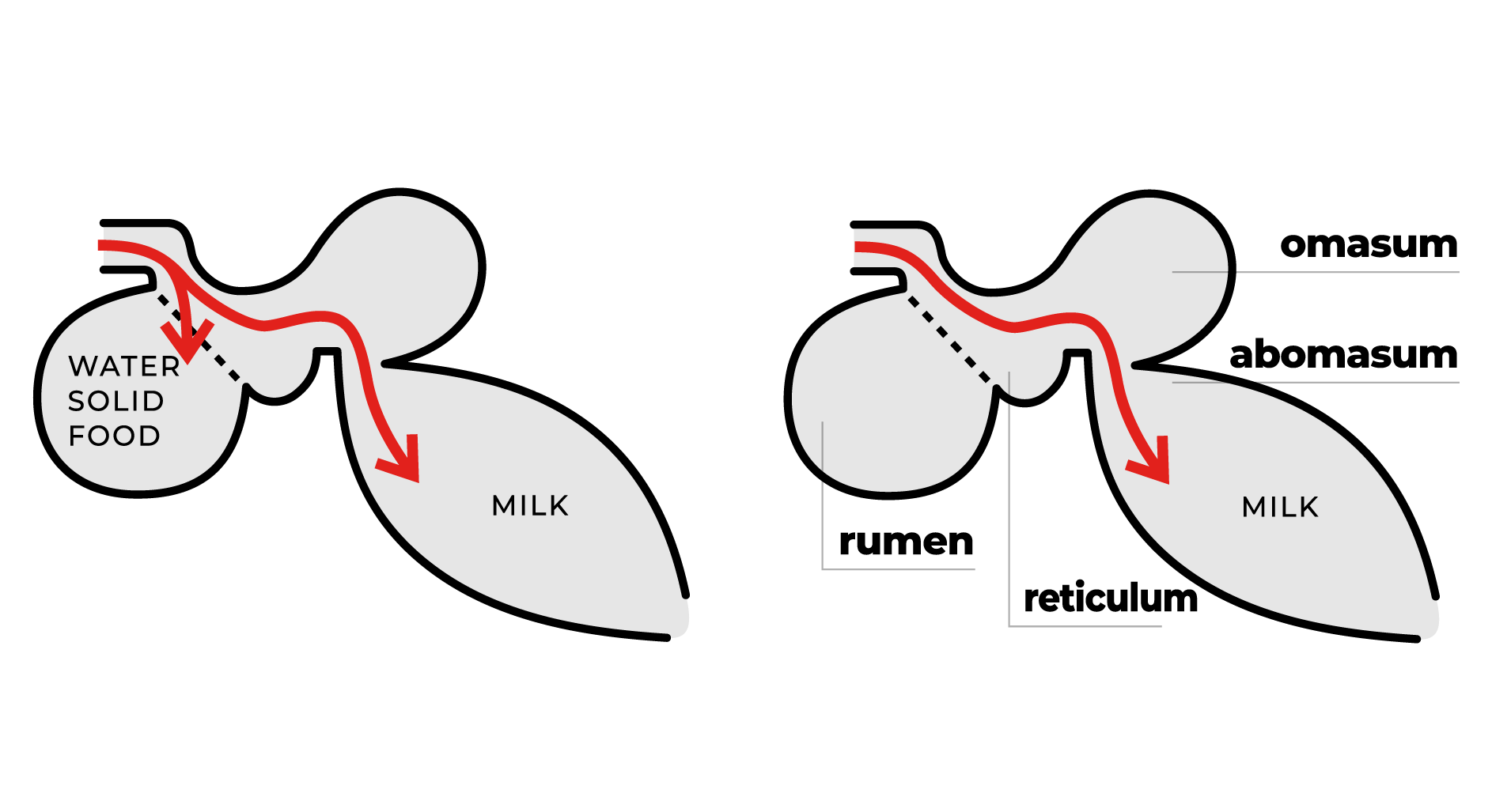
What is the pathogenesis of ruminal drinking?
Calves on milk feeding have sensitive reflex for glowing oesophageal tube to prevent milk entering rumen
When weak reflex, or force feeding, can enter rumen → anaerobic bacteria, putrid bacteria, suboptimal gases formed
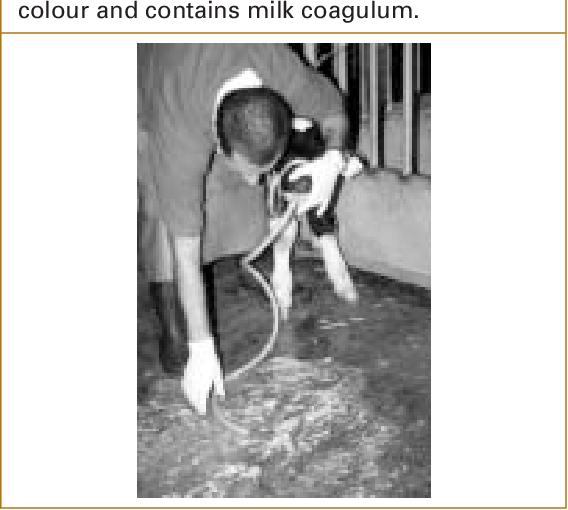
How is ruminal drinking diagnosed?
Characterised by metallic percussion/splashing sound. Stomach tube= stinky grey fluid
What are causes of Hoflund syndrome?
Reticuloperitonitis
Foreign bodies
Abscesses
Bronchopneumonia
Pyloric stenosis
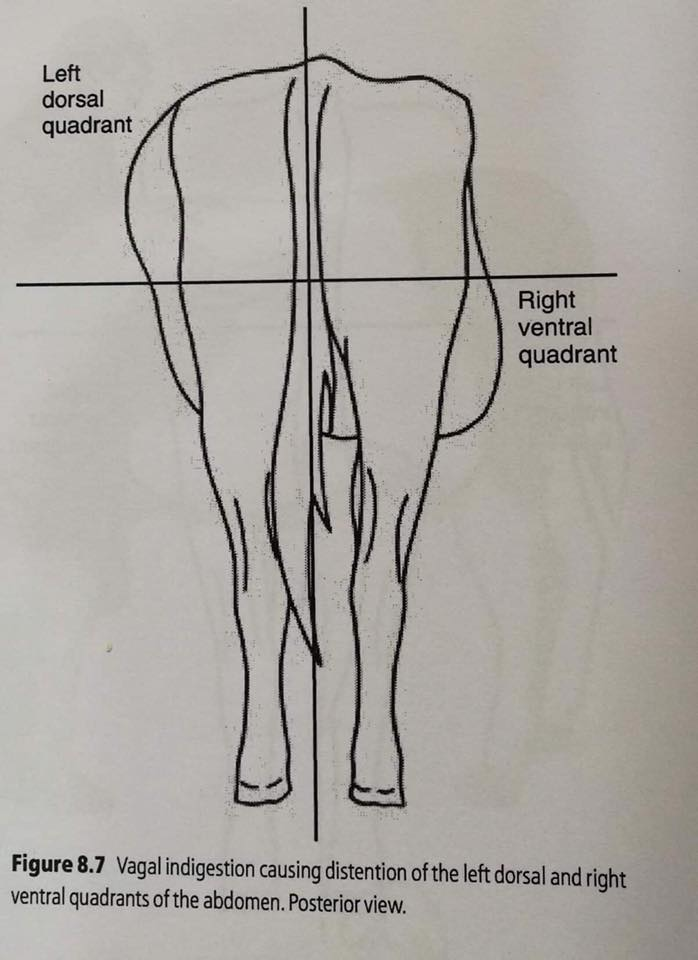
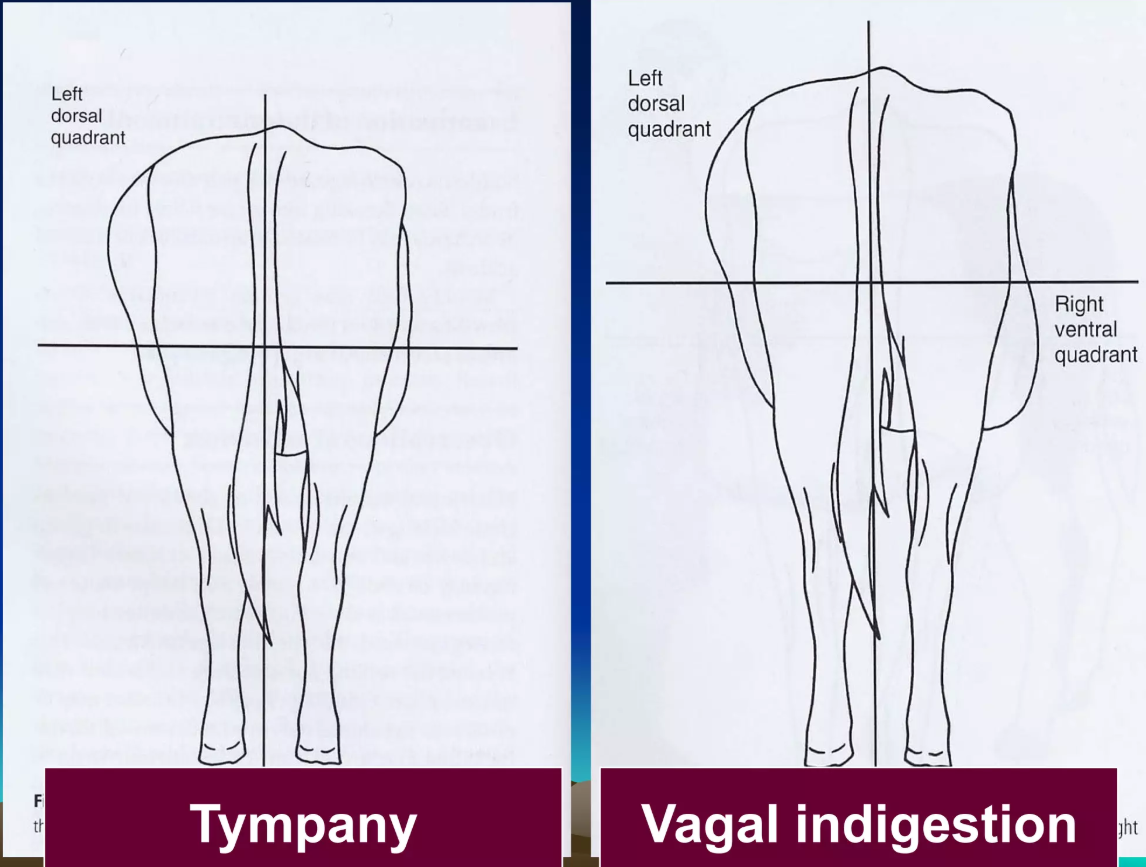
What are signs of Hoflund syndrome?
L-shaped abdomen, decreased appetite, progressive apathy, bradycardia, ruminal contractions
How is Hoflund syndrome diagnosed?
Clinical examination: clinical signs, rectal exam (dilation of ventral ruminal sac), sonography,
Blood analysis: protein, leucocytes, BHB, AST, GGT, pH, BE, urea
Urinalysis: paradoxical aciduria
What are differential diagnoses of Hoflund syndrome?
Abomasal displacement
Primary tympany: no rumen movement and TACHYCARDIA (Hoflund - rumen contraction, BRADYCARDIA)
How is Hoflund syndrome treated?
Based on cause: paraffin oil, rumenotomy (reticuloperitonitis), abomasal correction (DA), rehydration, antibiotics, and supportive care
What are contributing factors to traumatic peritonitis?
Late pregnancy: gravid uterus press on rumen and reticulum
Calving: sudden increase in abdominal pressure
Tenesmus: proctitis, vaginitis, cystitis, obstipation
What are clinical signs of acute localised reticuloperitonitis?
Anorexia, sudden milk drop, arched back, elbow abduction, pain on ventral abdomen, tachycardia

What are signs of diffuse reticuloperitonitis?
(most dangerous): fever, severe tachycardia/pnoe, no milk, complete GIT stasis, strong pain signs (grunts), hard tension of abdominal wall, reluctance to move, scant manure, lift abdomen (sensitive to pressure), short CRT
How is traumatic reticuloperitonitis diagnosed?
Clinical exam: clinical signs, test for foreign bodies (back grip, box sounds, pain percussion)
Laboratory examination
Blood analysis: increased WBC, increased protein, increased BHB, high pH (alkalosis due to restricted feed intake)
Abdominal puncate (10cm right of navel): increased exudate (normal: nothing)
Urine: pH (alkalic, paradoxic aciduria), high protein (nb always high during alkaline urine)
GAT (glutaraldehyde test): tell length of inflammatory process. 5000 leu
What allows the abomasum to be displaced in cows?
Its loose suspension by the greater omentum and lesser omentum
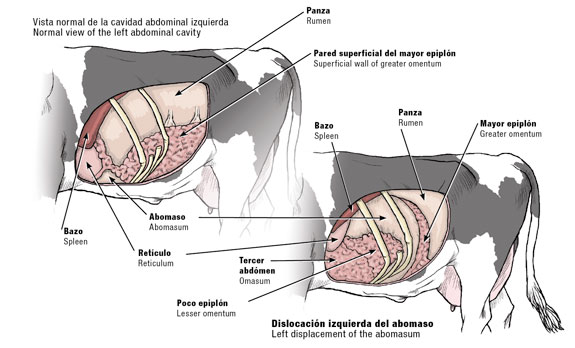
Abomasal hypomotility
High concentrates and low fibre in TMR
Hypocalcaemia
Hypokalemia
Lipo-mobilisation/ketosis
Concurrent diseases like mastitis and metritis
Heredity
What is the metabolic pathway leading to abomasal displacement from high concentrates in TMR?
High NEFA → high VFA → metabolic acidosis → decreased circulating calcium, fermentation in the abomasum, and gas production
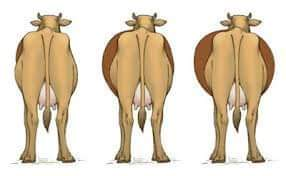
What happens during left abomasal displacement (LDA)?
The abomasum moves below and to the left of the rumen due to gas and digesta accumulation, resulting in gaseous distension and inhibition of motility
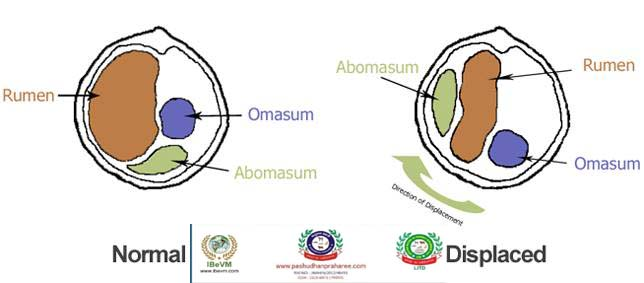
Acute and life-threatening volvulus with ischemia and haemorrhagic strangulating obstruction → melena
What are clinical signs of abomasal displacement?
Anorexia, decreased milk production, reduced watery faeces, lifted tail, arched back, dehydration, and enophthalmos

What are the common methods for treating displaced abomasum?
Rolling (LDA only)
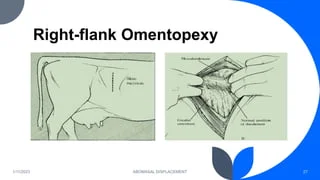
Laparotomic omentopexy right (LDA + RDA)
Percutaneus abomasopexy (LDA) - toggle or blind stitch
Laparoscopy (Christiansen method) (LDA)
What is the treatment for left abomasal displacement using rolling?
Casting the cow on her right side and rolling through a 180° arc

What is laparotomic omentopexy?
A surgical procedure where the abomasum is decompressed, repositioned, and secured using omentopexy through the right paralumbar fossa
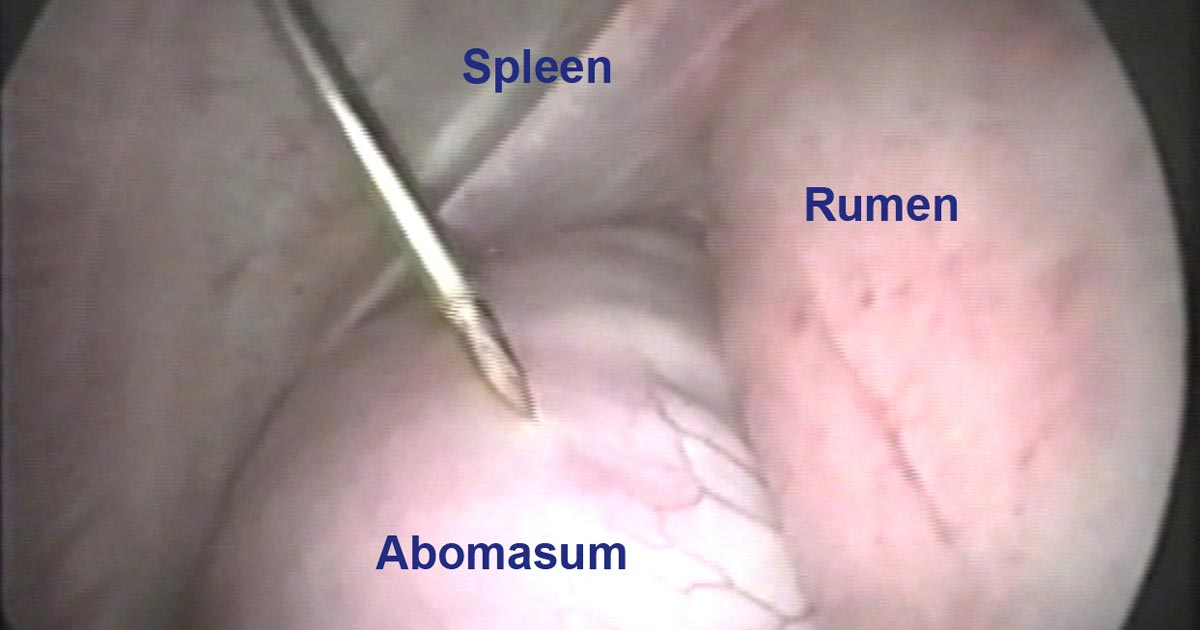
What is the Christiansen method of abomasopexy?
A laparoscopic procedure using a spieker to place toggle pins and tie them externally to stabilize the abomasum

Complication of RDA. Rotation of the abomasum on its mesenteric axis, leading to circulatory impairment, ischemia, and necrosis
How is abomasal volvulus treated?
Volvulus is corrected surgically using right paralumbar fossa omentopexy when economically feasible.
What are the causes of abomasal ulcers?
Unknown, can be due to viral diseases, prolonged inappetence, lymphosarcoma, abomasal disorders, other disorders.
What are the classifications of abomasal ulcers?
Type I: erosion without haemorrhage;
Type II: haemorrhagic;
Type III: perforated with acute localised peritonitis;
Type IV: perforated with acute diffuse peritonitis;
Type V: perforated within the omental bursa

How are abomasal ulcers diagnosed?
Physical examination and excluding other causes of peritonitis.
What is the surgical correction of left and right abomasal displacement?
Right laparotomic omentopexy
What is the most recent type of abomasopexy invented?
Christiansen laparoscopic abomasopexy.
What is the difference in changes of shape in Hoflund vs. tympany?
Tympany is distended left side of abdomen, right if very acute
Hoflund is L-shaped
How is hardwire disease diagnosed and treated?
Dx: Grip back, increased TP and WBC, abdominal punctuation
Treatment: rumenotomy and magnet
What is a secondary cause of ruminal tympany?
Obstruction and therefore not able to regurgitate, e.g. apple
How is Hoflund syndrome treated?
Soften reticular content w/ paraffin oil, rumenotomy, correction of abomasal displacement, supportive
How is an LDA diagnosed?
Percussion and auscultation, splashing sound.
What is worse: ruminal tympany or Hoflund syndrome, and what's the difference?
Ruminal tympany (acute and life-threatening). RT: no rumen contraction, tachycardia. HS: rumen contraction, bradycardia.
What is a common preventive measure for hardware disease?
Administering a magnet to cows over 1 year old (usually 14-16 months at first AI)
Which abomasal displacement causes melena in faeces (dark/black faeces)?
Right abomasal displacement due to volvulus.
How is the Christiansen method carried out?
Percutaneous/laparoscopic abomasopexy standing procedure. This procedure requires a special instrument named a spieker to push the toggle ends through the ventral abdomen from a standing left flank approach.
Two 10 cm x 10-cm squares are shaved and prepared for the introduction of the laparoscope and instruments.
The laparoscope is introduced just behind the last rib and ventrally to the transverse process of the lumbar vertebras.
Room air is allowed to enter the abdomen.
The instrument portal is located at the 11th or 12th intercostal space at the same level or slightly ventral compared with the laparoscope portal.
A long trocar and its cannula are introduced through the instrument portal into the abomasum.
The trocar is removed, and the toggle pin is introduced within the abomasum.
The abomasum is deflated, and the toggle ends are kept outside the abdomen.
They are passed through the push rod within the spieker. This unit is then introduced in the abdomen through the instrument portal and directed in the cranial right paramedian part of the abdomen.
The tip of the spieker is felt or seen before pushing the rods through the abdominal wall.
Finally, the toggle ends are tied over a roll of gauze until the markers are visualized (5 cm from the pin)
What is the most dangerous type of rumen acidosis?
Acute.