Pathology Case Study Quiz 2
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
What is Emphysema?
- A type of chronic, obstructive pulmonary disease characterised by destruction of the alveolar sacks which leads to destruction of the elastic fibres and the pulmonary capillary bed.
- Larger, less elastic sacks remain, preventing gas diffusion and causing air to become trapped inside alveoli.
What are the two key types of emphysema?
- Centre-acinar Emphysema: typical in smokers where the proximal acini (bronchioles) are affected.
- Pan-acinar Emphysema: typical in hereditary cases where the distal acini (alveoli) are affected.
What are the three key risk factors of emphysema?
- Smoking: Oxidants and free radicals damage alveolar walls and stimulate inflammatory cells which release elastase, destroying elastic fibres in the alveoli. It inactivates Alpha-1 antitrypsin which neutralises elastase.
- Air Pollution: Chronic inhalation of irritants causes persistent airway inflammation, destroying elastic fibres.
- Hereditary Factors: Alpha-1 antitrypsin inhibits elastase. A deficiency increases elastase, increasing the destruction of elastic fibres.
Describe the pathogenesis or pathophysiology of emphysema.
1. Smoking or air pollution attracts inflammatory cells, which release elastase, destroying elastic fibres.
- Alpha-1 antitrypsin inhibits the action of elastase to inhibit it.
2. Continued exposure causes deficiencies in Alpha-1 antitrypsin, and destruction of elastic fibres.
What 8 key symptoms may be observed in emphysema and why?
- Dyspnoea: shortness of breath due to air trapping and reduced elasticity stopping full inhalation and exhalation.
- Barrel chest: air becomes trapped in the alveoli, causing the lungs to become chronically overinflated.
- Coughing Mucus: irritants to the airways, like smoking, increases mucus production in to attempt to clear debris.
- Muscle Wasting and weight loss: hypoxia and increased energy required for breathing increase energy demands while lowering supply to the body’s cells.
- Increased muscle use of accessory respiratory muscles: all used to breath in attempt to increase depth of breathing in response to low lung elasticity, which can cause a red appearance.
- Difficulty breathing while lying down: thoracic volume decreases, which restricts diaphragmatic movement, preventing inhalation and exhalation.
- Hunched forward breathing: being hunched assists the accessory muscles in breathing, and assists diaphragm.
- Pursed lip breathing: helps to keep airways open, and allows more complete exhalation.
What may be observed in 5 vital signs in a person with emphysema.
- Blood pressure: Usually normal, except for right sided heart failure due to increased work.
- Heart Rate: increased as a compensatory mechanism for low oxygen intake.
- Respiratory Rate: increased as a compensatory mechanism for low oxygen intake.
- Temperature: Usually normal, except for if an infection is present, temperature may become raised.
- SpO2 (Oxygen Saturation): low due to damage to and reduced functioning of gas exchange surfaces.
What might be seen in a chest x-ray of a person with emphysema?
- Lung size enlarged with a lowered diaphragm.
- Large holes in the lung as alveoli join together.
What might be seen in a chest CT of a person with emphysema?
- Better than a chest X-ray as it provides information about the extent of emphysema and other COPD changes.
- Enlarged arteries can be seen and the over-inflation of alveoli is seen as daker spots.
What 4 things might be measured in spirometry for a person with emphysema, and what may be found?
- Pulmonary/Lung Function Test: measures flow of air through the lungs, and the amount of air which can be exhaled.
-Lung Capacity: increased due to hyperinflation of trapped air.
-Residual Volume: greatly increased due to trapped air in the alveoli which is unable to be exhaled.
- Forced Expiratory Volume in 1 second (FEV1): should be able to expire 80% of inhaled air in one second. Decreased in emphysema as lack of elastic fibres lowers ability to quickly exhale.
- Forced Vital Capacity (FVC): The maximum volume which can be exhaled after a deep inhalation. May be normal or slightly decreased due to air trapping.
- FEV1 / FVC ratio: normal over 80%, but will be lower in emphysema due to reduced FEV1.
What 6 things may be used as treatment for emphysema?
- There is no cure, but solutions can be used to slow progression and lessen symptoms.
- Change in Lifestyle: stopping smoking can prevent further damage to the lungs and reduce mucus production.
- Albuterol inhaler (Ventolin): attaches to beta receptors and relax bronchiole smooth muscle to increase lumen.
- Budesonide (steroid) inhaler: reduces inflammation and mucus production in the airways to increase lumen.
- Enalapril: an ACE inhibitor, prevents conversion of angiotensin 1 to 2, lowering blood pressure.
- Amoxicillin: antibiotics based on the sputum culture to combat inflammation.
- Oxygen therapy: increases the oxygen present in the lungs, and hence that able to enter the bloodstream.
What might be investigated in a blood test for emphysema?
- Arterial blood gases (ABGs): measure carbon dioxide, higher due to air trapping poor ventilation, large alveoli.
- Blood pH: will be lower with greater carbon dioxide in the bloodstream.
- Complete blood count: RBC count increased due to release of EPO in response to low oxygen levels in blood. White blood cells may be increased due to infection indicated by yellow-green sputum.
Why might out of bed assistance be needed for emphysema?
As shortness of breath, light-headedness or dizziness make standing are unsafe.
Why might continuous ECG monitoring be needed for a person with emphysema?
They may suffer from heart attack due to low oxygen delivery to cardiac tissue.
Why might a sputum culture be used for a person with emphysema?
- check presence of bacteria before using antibiotics.
What is the difference between obstructive and restrictive lung disease, and give an example of each?
Obstructive: the entry of air into the alveoli is obstructed in some way.
Eg. destruction of capillaries and elastic fibres in emphysema.
Restrictive: the expansion capacity of lung tissue is restricted in some way, reducing lung capacity and volume.
Eg. lung fibrosis causing stiff lungs as elastic lung tissue is replaced by fibrous tissue
Explain why a person who smokes / with emphysema might have increased mucus production and how this can influence gas exchange.
Smoking acts as an irritant to the airways, and mucus production is increased by goblet and mucus cells to attempt to clear debris. Chronically, this can cause damage to the cilia, preventing its function of helping to remove mucus from the body. This means smokers need to cough harder to remove mucus. Less oxygen enters the gas exchange surfaces due to a smaller lumen, inhibiting gas exchange.
What is a V/Q ratio, and how might it appear in emphysema vs chronic bronchitis?
V = ventilation: movement of air from lungs and atmosphere.
Q = perfusion: how much blood is going through pulmonary vein.
V/Q ratio: the relationship between air reaching alveoli, and blood reaching alveoli. normal = 4/5.
- Lower - problems in ventilation – chronic bronchitis
- Higher – problems in perfusion – emphysema
Explain why COPD can lead to cor-pulmonale.
COPD causes increased pulmonary blood pressure as a compensatory mechanism to low blood oxygen. This can cause pulmonary hypertension, causing the right ventricle to work harder, which can lead to cor-pulmonale (right sided heart failure).
What is Chronic Bronchitis?
Chronic bronchitis is a form of COPD in which a persistent cough producing mucus is present for 3 months or more. This includes excess mucus prouction and bronchial inflammation.
Describe the differences in symptoms between a blue bloater and pink puffer.
Blue Bloater - Chronic Bronchitis
Right sided heart failure occurs, causing peripheral oedema and cyanosis.
Pink Puffer - Emphysema
Alveoli are destroyed, making breathing harder, hunching and a red appearance occurs due to using accessory breathing muscles.
What are Peptic ulcers and where and how can they occur.
- Peptic ulcers are breaks or ulcerations in the mucosal lining of the oesophagus, stomach, or duodenum.
- Helicobacter pylori accumulates in the antrum and increases urease, which splits urea into ammonia and CO2.
-It also produces catalase, and enzyme which protects microbes from phagocytosis.
- Mucosal linings can be damaged by increased ammonia or other factors which increase stomach acids.
- This leads to inflammation of the mucosa (gastritis), which can lead to formation of an ulcer.
What are 5 risk factors of developing peptic ulcers?
- Medications: NSAIDS’s like aspirin thin the mucus membrane.
-Inhibit COX-1 and COX-2, decreasing prostaglandin synthesis, preventing protection of mucus layer (systemic).
-NSAID’s are weak acids, hence having a weak damage on the epithelial layers (topical).
- Lifestyle Factors: stress, high alcohol intake, and eating spicy foods all increase stomach acids.
- Smoking: Increases risk of helicobacter pylori infections, and damages stomach lining. Delays ulcer healing.
- Diabetes and Hypertension: increase thickness of blood vessels to stomach, narrowing lumen and preventing blood flow to the stomach, causing thinning of the gastric mucosa.
- Age: as you age, the mucosal lining of the stomach gets thinner, making it more prone to damage.
What are 7 symptoms of peptic ulcers.
- Epigastric Discomfort or Pain: burning or aching pain caused when stomach acids irritates exposed tissue.
-Pain can radiate towards the back when located on the posterior wall of the organ.
-Heartburn can occur due to upwards movement of stomach acid.
-In gastric ulcers, pain occurs rapidly (30-60 minutes) while in duodenal ulcers it occurs later (2-5 hours).
- Bloating and fullness: abdominal distension occurs as the stomach size increases.
- Nausea and Vomiting: Caused by fluid in the stomach and irritation triggering visceral nerves.
-Can be undigested in peptic ulcer.
- Haematemesis: vomiting blood occurs when vomiting sensations are triggered, and an ulcer is bleeding.
- Tarry Stool: dark coloured stool caused by bleeding from an ulcer which is oxidised as the stool passes.
- Weight Loss: occurs due to bloating, early fullness, and stomach aches causing food avoidance.
- Fatigue, Pallor: occurs due to chronic blood loss via blood in the stool leading to iron-deficiency anaemia.
What 3 vital signs might be observed with peptic ulcers?
- Heart Rate: increased to compensate for lack of oxygen to tissues from anaemia.
- Respiratory Rate: increased to compensate for lack of oxygen to tissues from anaemia.
- Pulse Oxygenation: reduced due to anaemia.
How is a urea breath test undertaken, and how does it indicate peptic ulcers.
- A capsule containing urea (made from carbon isotope) is swallowed. If H. Pylori is present in the stomach, urea is broken into carbon dioxide, which is absorbed across the stomach lining into the blood.
- Samples of exhaled breath are collected, and if isotopic carbon in exhaled carbon dioxide is measured, H. pylori is present.
- This is the preferred method of testing as it is specific, non-invasive, and sensitive test.
What is antigen and antibody testing for peptic ulcers / H. pylori?
- Antigen: The presence of H. pylori in the stool. This is reliable for initial diagnosis, and post-treatment follow up.
- Antibodies: The presence of specific Ig-G antibodies to H. pylori in the bloodstream.
What is an endoscopy and what are 3 reasons it is used for peptic ulcers?
- Used to visualise the oesophagus, stomach, and duodenum.
- Detection: can be used to detect ulcers. Can check location, severity, and for further complications.
- Further Investigation: Other disorders can also be investigated, gastritis, ulcer, obstruction or cancer cells.
- Biopsy: can be used to take a biopsy of an ulcer, to ensure it is not carcinogenic.
How might an x-ray be used for investigation of peptic ulcers?
- Detection: Barium meals are used for x-rays to visualise the digestive system. This cannot be used when an ulcer has perforated all 4 mucosal layers.
How might a CT scan be used for investigation of peptic ulcers?
- Can indicate obstruction or perforation occurring due to a peptic ulcer.
Why might a blood test be done for peptic ulcers?
- Full Blood Count / Iron Studies: check for iron-deficiency anaemia caused by chronic blood loss.
What are 4 possible complications of peptic ulcers.
- Perforation: Food contents enter the abdominal cavity and peritoneum. This can lead to peritonitis, which can cause shock. Sharp abdominal pain can be present.
- GI Bleeding: blood vessels become damaged, causing blood to be released into the GI tract. This leads to blood in the stool, or tarry stools. This ultimately leads to anaemia.
- Obstruction of Gastric Outlet: chyme cannot exit the stomach into the duodenum.
- Malignancy: gastric ulcers can become malignant cancers.
What are 4 possible treatments of peptic ulcers?
- Antacids: works instantly as bicarb neutralising the stomach acids.
- H2 Receptor Blocker: Ranitidine (Xantax) is H2 (histamine) receptor blocker, which hence inhibits more acid production.
- Antibiotics: Prevent growth of H. pylori
- Bismuth: coats the ulcer to protect it from stomach acid.
Why do peptic ulcers occur in each location?
Ulcers form due to exposure to acids and pepsin which digest the mucosal layer.
Oesophagus: lack of protection from stomach acids due to upwards reflux of stomach acids.
Stomach: lack of protection due to thinning or damage to mucosal layer.
Duodenum: lack of protection from stomach acids as food passes through GI tract.
What are the differences between gastric and Duodenal ulcers?
Gastric
- Age 50+
- Weight gain less common.
- Pain straight after eating. Pain relieved after vomiting.
- Nausea and vomiting common.
- Blood in the stool. Bleeding more likely.
- Vomiting of blood more common.
- Perforation less likely.
- More likely to become cancerous.
NSAID use more likely to increase risk.
Duodenal
- Age 30 to 60.
- Make up 80% of peptic ulcers.
- Weight gain common.
- Pain 2-3 hours after meal. Pain relived with eating.
- Nausea and vomiting uncommon.
- Blood in the stool. Bleeding less likely.
- Blood in the stool more common.
- Perforation more likely.
- Less likely to become cancerous.
NSAID use does not increase risk.
What is Barrett oesophagus and its link to gastroesophageal reflux.
Barrett oesophagus: changes to the lining of the oesophagus caused by exposure to stomach acids. Can include inflammation, ulceration or cancer.
gastroesophageal reflux increases exposure to stomach acids, causing Barrett’s oesophagus.
What are the 4 breast quadrants, and in which is breast cancer most common?
Upper inner quadrant
Upper outer quadrant
Lower outer quadrant
Lower inner quadrant
Breast cancer is most common in the upper outer quadrant.
What is breast cancer?
The uncontrolled growth of abnormal cells within the breast tissue, which can metastasise to further parts of the body.
What is in situ vs invasive breast cancer.
- In Situ: cancer cells are confined to the duct and lobule, and the basement membrane is still intact. Hence there is no lymphatic and distal spread. No symptoms generally occur, and it is found in a mammogram. Better prognosis.
- Invasive: cancer cells have invaded surrounding tissue by invading the basement membrane. Metastasis via lymphatic vessels to distal organs is possible. A physical lump can often be felt, pain near the tumor, and skin changes occur.
What is ductal vs lobular breast cancer?
- Lobular: cancer originating from lobule cells (simple cuboidal) where milk production occurs. A single cell, diffuse mass grows, which is more difficult to detect. More subtle and harder to find.
- Ductal: cancer originating in the ductal cells (simple cuboidal). Much more common. A discrete mass grows which is easier to detect on imaging. A lump or abnormal mammogram is also found.
What is Triple positive vs triple negative breast cancer?
- Triple Negative Breast Cancer: cancer cells contain no estrogen, progesterone or HER2 receptors.
-Does not respond to hormonal therapy, and hence the main therapy is chemotherapy.
-often high-grade, fast growing, with a worse prognosis. Recurrence is more common.
- Triple Positive Breast Cancer: cancer cells contain estrogen, progesterone and HER 2 receptors.
-Responds well to hormone therapy, which can be used in conjunction with chemotherapy.
-Often less aggressive, slower growing, with a better prognosis and lower risk of recurrence.
-HER2 positive cells have lots of receptors to promote rapid growth
what are some risk factors of breast cancer?
- Female: breast cells more influenced by estrogen and progesterone, increasing risk.
- Age (over 50): genetic mutations accumulate over time.
- Family History: inherited mutations, BRACA-1 and 2, impair DNA repair and increase cancer risk.
- Early menarche and late menopause: longer time exposed to sex hormones, increasing risk.
- Having had no full-term pregnancy: cells mature and differentiate in pregnancy, reducing cancer risk.
- First child after age 30: longer exposure to estrogen before protective cell changes occur.
- Environmental factors: alcohol, obesity (fat tissue produces oestrogen) inactivity or diet.
- Hormonal influence: hormonal therapy increases stimulation of breast cells and hence breast cancer risk.
- Fibrocystic changes: make denser masses harder to recognise in the breast.
- Dense breast tissue: there is more tissue which breast cancer can occur in.
- Triple-Negative Breast Cancer: younger women (<40), BRACA-1, black people.
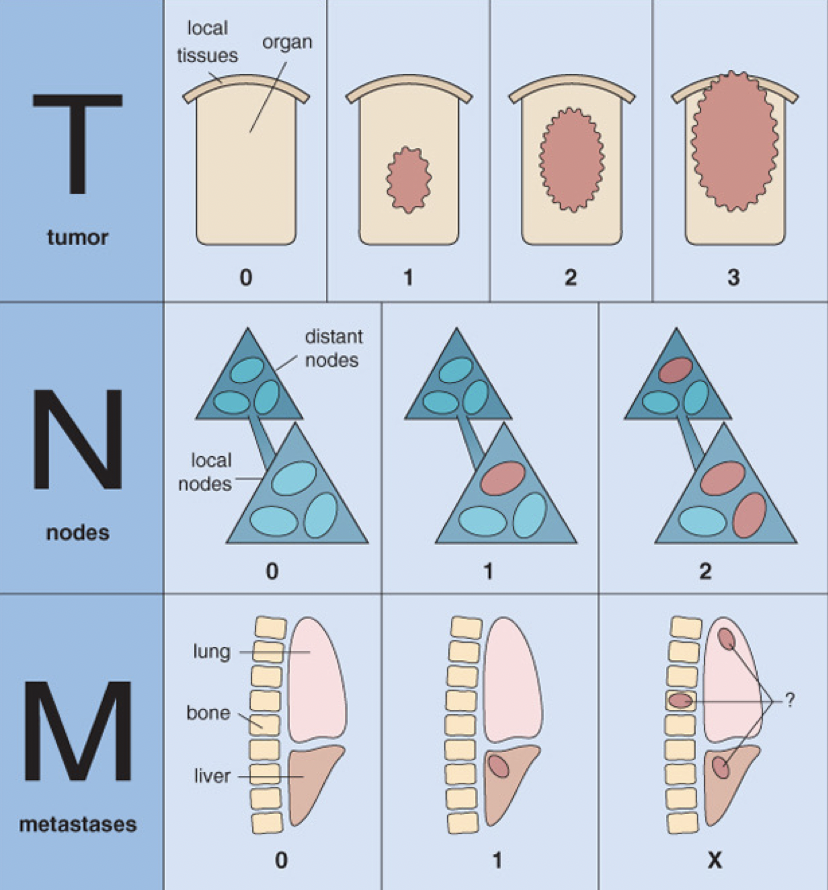
Describe the staging of breast cancer
Staging: Refers to extent of cancer spread in the body. Guides prognosis and treatment.
T (Tumor): based on the size of the tumour.
N (Node): based on nodal involvement
M (Metastasis) based on metastasis of tumour
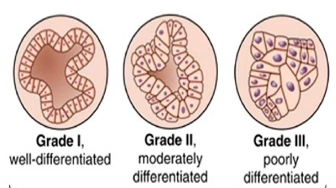
Describe the grading of breast cancer and Nottingham grading
Grading: Refers to the abnormality of cancer cells under the microscope. Refers to differentiation indicating how aggressive and likely to spread the cancer is.
- Nottingham Grading: based on differentiation, nucleus and speed of cell growth indicating the aggressiveness of the cancer.
-NG 3-5. Grade = I
-NG 6-7. Grade = II
-NG 8-9. Grade = III
What are some general symptoms of breast cancer
- Painless Lump: mitotic cell division is uncontrolled, forming a palpable mass.
- Changes in Breast Size and Shape: necrosis can occur around the mass, causing fibrous tissue, changing shape.
- Edema: obstruction of axillary lymphatic drainage causes build-up of interstitial fluid.
- Pain: tumour places pressure on nerve endings
- Skin Dimpling: tumour infiltrates cooper’s ligaments, causing retraction and hence skin dimpling.
- Reddened skin: inflammation and increased blood supply to tumour region.
- Nipple inversion: tumour invasion of the ducts can pull the tissue inwards.
- Enlargement of Lymph nodes: once tumour spreads to lymph nodes, lymph nodes will become enlarged.
- Nipple Discharge: bloody or serous fluid can leak as tumour erodes ducts.
- Weight loss, fatigue and bone pain can present as the tumour progresses.
- Chest Pain: metastasis of the tumour to the lung.
What is triple testing and why is it done for breast cancer?
- Triple testing is used to suggest benign or malignant disease. Together the results from the three tests provide a more accurate diagnosis of breast cancer in a patient.
1. Clinical Testing
- Clinical Examination: doctor examines the breast, lump, skin changes, nipple changes and lymph nodes.
- Patient History
2. Imaging Tests
- Mammogram, Ultrasound and/or MRI to look for/visualise the mass and view the size, and microcalcifications.
3. Biopsy
- Fine needle biopsy or core needle biopsy.
- Removal of cells for further examination under a microscope.
- This allows histological diagnosis, and testing for hormone receptors.
Apart from triple testing, what other factors may be checked for breast cancer
ER, PR, and HER2 presence. Indicates triple-negative or triple-positive. This gives information about the risk of the cancer and treatment options.
Lymph node evaluation. Lymph nodes are tested to see if the cancer has began to spread.
What is a complication of breast cancer.
- Metastasis: A breast tumour generally drains into the sentinel lymph nodes.
How is surgery used as a treatment option for breast cancer?
- Lumpectomy: physical removal of cancer cells and a margin of tissue, preserving most of the breast.
- Mastectomy: removes the entire breast and all its tissues.
- Axillary lymph node dissection: following positive sentinel lymph node testing to prevent spread.
How is chemotherapy used as a treatment option for breast cancer? What 4 drugs may be used and their impacts.
- Two or three chemotherapy drugs are used together as different medications work by different mechanisms, increasing effectiveness and reducing likelihood of cancer cells developing resistance.
-It increases effectiveness as drugs target cancer cells different ways and at different stages of the life cycle.
-Lower dosage can be given of each drug, reducing toxicity.
- TAC chemotherapy:
-Taxotere: inhibits cell division by disrupting microtubules.
-Adriamycin: slows growth of cancer cells by blocking an enzyme (isomerase) needed for growth/division.
-Cyclophosphamide: prevents division of cancer cells by cross-linking strands to prevent DNA synthesis.
- Pegfilgrastim: stimulates growth of healthy WBC in bone marrow to reduce risk of infection during chemotherapy.
How is Radiotherapy used as a treatment option for breast cancer?
- Using high energy radiation to kill cancer cells in the breast tissue.
- Can be given after a lumpectomy to reduce recurrence, or in conjunction with other treatments.
How is hormone therapy and HER2 targeted therapy used as a treatment option for breast cancer?
- Can only be used for triple positive cancers.
- Tamoxifen – given for 5 years to pre- and post-menopausal women to block estrogen receptors. Should not be given to women who are pregnant or breastfeeding.
- Aromatase Inhibitor - given for post-menopausal women to block estrogen production or conversion of androgens to estrogen in adrenal cortex.
- Herceptin – blocks the activation of HER2 receptors to prevent growth signalling.
What are the hormonal influences on the breast in non-pregnant, pregnant and lactating women?
Non-Pregnant (menstrual)
- Estrogen and Progesterone have cyclic effects on the breast tissue.
- Low estrogen and progesterone trigger a menstrual cycle.
- Higher progesterone before a menstrual cycle causes tender and enlarged breasts.
Pregnant
- Key hormones include estrogen, progesterone, prolactin, cortisol, and insulin.
- Ductal proliferation and milk production in preparation for childbirth.
Lactation
- Key hormones include prolactin and oxytocin.
- Prolactin: breast milk synthesis.
- Oxytocin: breast milk ejection.
What is a Sentinel lymph node and where are they usually in breast cancer?
- Sentinel lymph nodes: first group of lymph node receiving lymphatic drainage from primary tumour site.
- In breast cancer, sentinel nodes are usually in the axilla.
- A biopsy or dye scan can be used to determine if cancer has spread to the sentinel lymph nodes.
What is lymph and what are lymph nodes (+ 5 key clusters)?
- Lymph is clear fluid originated from excess interstitial fluid between cells.
- It is mainly water, electrolytes, and proteins.
- It also contains immune cells to provide protection from pathogens.
- Two key functions: fluid balance regulation to prevent oedema, immune system protection.
- Lymph nodes are located along lymph vessels and found all throughout the body.
- They are concentrated into clusters in some areas, including the neck/cervicale (head and neck), axillary (breast, upper limb and thoracic walls), thoracic (lungs and heart), abdominal (GI tract and abdominal organs) groin (lower limb, lower abdominal wall and groin).
What factors can affect breast cancer prognosis?
- Size: larger tumours have worse prognosis.
- Lymph Node Involvement: more lymph nodes involved generally indicates worse prognosis.
- Histological Grading: poorly differentiated cancers generally have worse prognosis.
- Histological Type: invasive or in situ. Ductal or lobular.
- Hormone status: triple positive has greater prognosis than triple negative.
- Proliferation index: greater proliferation generally has a worse prognosis.
- Metastasis: the presence, extent and location of metastasis can impact prognosis.
1. What are the most common sites of metastasis in breast cancer, and the symptoms at each site?
Bone (bone pain, fractures, hypercalcaemia)
Lung (cough, difficulty breathing, pleural effusion)
Liver (RUQ pain, jaundice, liver enzymes)
Brain (headache, neurological changes, behavioural changes)