Human Nutrition Exam #2
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
86 Terms
Identify the main roles, deficiency symptoms, and food sources for vitamin A
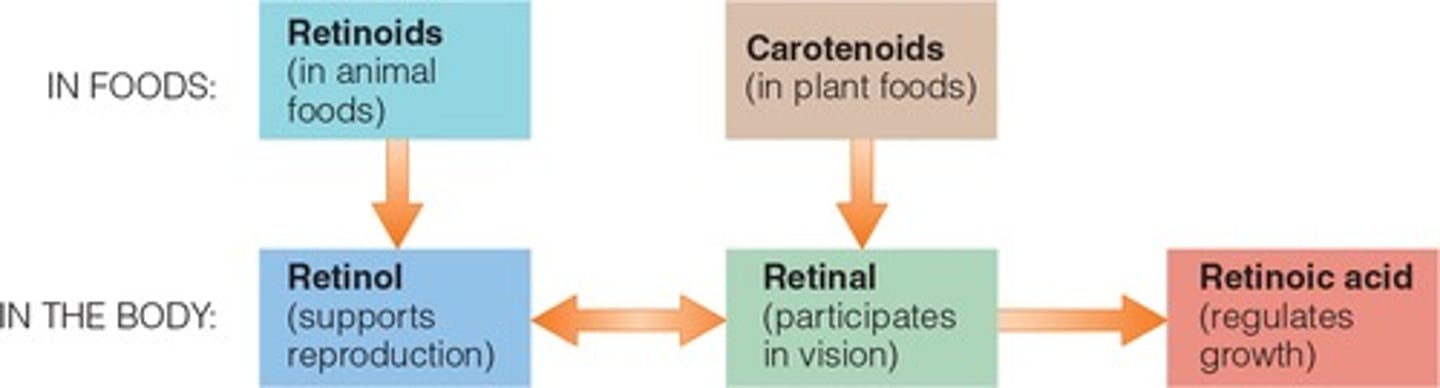
Vitamin A is found in the body in three forms: retinol, retinal, and retinoic acid.
-Together, they are essential to vision, healthy epithelial tissues, and growth.
-Vitamin A deficiency is a major health problem world wide, leading to infections, blindness, and keratinization. Toxicity can also cause problems and is most often associated with supplement abuse.
-Animal derived foods such as liver and whole or fortified milk provide retinoids, whereas brightly colored plant-derived foods such as spinach, carrots, and pumpkins provide beta-carotene and other carotenoids. In addition to serving as a precursor for vitamin A, beta-carotene acts as a anti-oxidant in the body. The accompanying table provides a summary of vitamin A.
Identify the main roles, deficiency symptoms and food sources for vitamin D
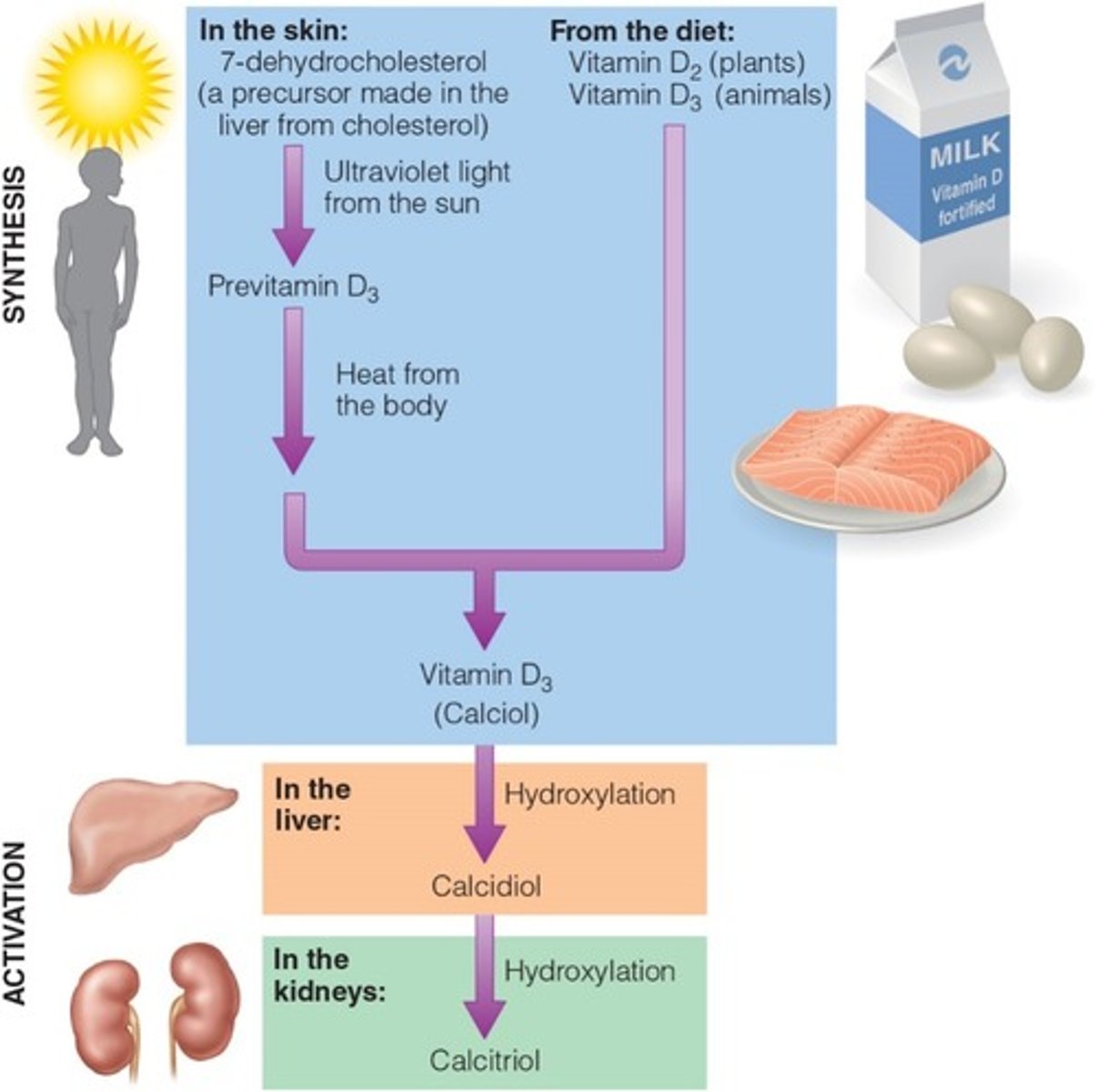
Vitamin D can be synthesized in the body with the help of sunlight or obtained from some foods, most notably fortified milk.
-Vitamin D sends signals to three primary target sites: the GI tract to absorb more calcium and phosphorous, the bones to release more, and the kidneys to retain more. These actions maintain blood calcium concentrations and support bone formation.
-A deficiency causes rickets in childhood and osteomalacia in later life.
Identify the main roles, deficiency symptoms and food sources for vitamin E
Vitamin E acts as an antioxidant, defending lipids and other components of the cells against oxidative damage.
-Deficiencies are rare, but they do occur in premature infants, the primary symptom being erythrocyte hemolysis.
-Vitamin E is found predominantly in vegetable oils and appears to be one of the least toxic of the fat-soluble vitamins.
Identify the main roles, deficiency symptoms and food sources for vitamin K
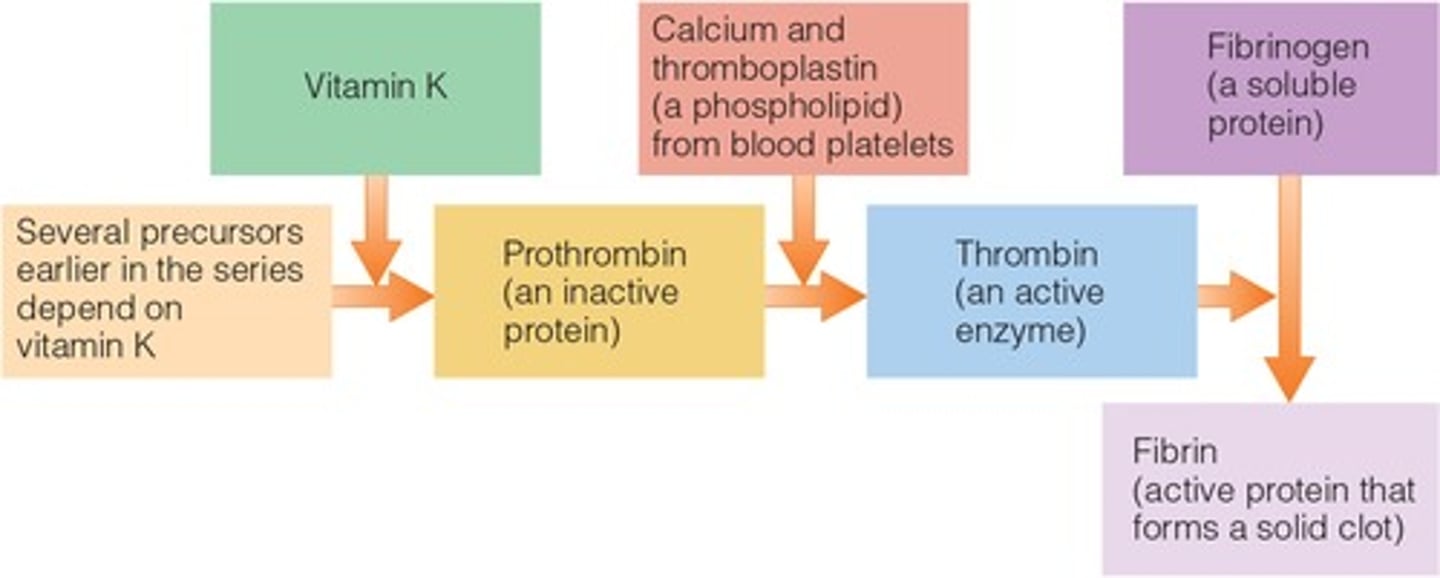
Vitamin K helps with blood clotting, and its deficiency causes hemorrhagic disease (uncontrolled bleeding).
-Bacteria in the GI tract can make the vitamin; people typically receive about half of their requirements from bacterial synthesis and half from foods such as green vegetables and vegetable oils.
-Because people depend on bacterial synthesis for vitamin K, deficiency is most likely in newborn infants and in people taking antibiotics.
Overview of Fat-soluble vitamins:
•Absorption: first enter into the lymph system and then into the blood
•Transport and storage: travels with protein carriers; stored in liver or fatty tissues
•Excretion: not readily excreted; builds up in the tissue
•Toxicity: likely caused by supplements but occurs rarely from foods
•Requirements: periodic doses; body can draw on stores
Describe the key differences between water- and fat-soluble vitamins
Describe how fat-soluble vitamins differ from water-soluble vitamins
Fat-soluble vitamins differ from water-soluble vitamins in that:
•They require bile for digestion and absorption
•They travel through the lymphatic system
•Excesses are stored in the liver and adipose tissues
•They are not readily excreted which may lead to toxicity symptoms
Recall if and when supplements are needed, how they are regulated, and misleading claims associated with them
After dietary assessment, a health care provider will make recommendations for you. Best course of action is to improve food choices.
People who need supplements:
-People with specific nutrient deficiencies
-People whose energy intakes are low
•Vegetarians who eat all-plant diets and older adults with atrophic gastritis may need vitamin B12
•People who have lactose intolerance or milk allergies may need calcium or vitamin D supplements
•Physiological states requiring specific nutrient supplements (i.e., pregnancy)
•Surgical procedures that have interfered with intake, absorption, metabolism or excretion of nutrients
•People taking medications that interfere with the body’s use of nutrients
Vitamins A and E:
oxidation, absorption, and storage
Vitamins A, D, and K:
bone growth and remodeling
Vitamins E and K:
blood clotting
How do vitamins differ from the energy nutrients?
They differ in structure, function, and food contents.
Characteristics of vitamins:
•Structure: individual units; not linked together like molecules of glucose or amino acids
•Essential and organic molecule—readily destroyed
•Function: do not yield energy but do assist enzymes with releasing energy from energy-dense nutrients
•Food contents: when ingested from foods, measured in micrograms or milligrams rather than grams
•Determining the amount or quantity of a vitamin in a food is easily analyzed and reported on by researchers
•Bioavailability: the amount of a vitamin that is absorbed and used by the body
Describe how water-soluble vitamins differ from the fat-soluble vitamins
•Dissolve in water
•Not stored in the body- should be consumed regularly in the diet
•Excreted in urine
•Help to form coenzymes that activate vitamins
•Most water-soluble vitamins have sufficient data to determine an RDA; however, if there is insufficient data- an AI is determined
Identify the main roles deficiency/toxicity symptoms, and food sources for each of the B-vitamins (i.e., Thiamin, riboflavin, niacin, biotin, pantothenic acid, vitamin B6, folate, vitamin B12, and choline)
Thiamin:
assists in energy production, carbohydrate metabolism, the production of ribose and the health of the nervous system.
•Thiamin deficiency disease (reported in malnourished individuals, homeless people, or individuals consuming ‘empty’ calories [e.g., alcoholics]) is called Beriberi
•Dry beriberi effects the nervous system; wet beriberi effects the cardiovascular system
•Alcohol impairs thiamin absorption and enhances thiamin excretion in urine
•Toxicity: no adverse effects and no UL established
Riboflavin:
a B vitamin active in the body's energy-releasing mechanisms; accepts and donates 2 H molecules during the TCA cycle (FMN and FAD)
•Deficiency: inflammation of membranes (mouth, skin, eyes, and GI tract)
•Heat stable but destroyed by ultraviolet light and irradiation
•Toxicity: no UL established
Niacin:
Two chemical structures: Nicotinic acid and Nicotinamide (major form of niacin in the blood)
Two coenzyme forms--metabolic rxns
•Nicotinamide adenine dinucleotide (NAD)
•Carries hydrogens and their electrons
•Protects against neurological degeneration
•NADP (the phosphate form)
Deficiency: Pellagra: diarrhea, dermatitis, dementia, and death
•Toxicity: “niacin flush”
•Not seen in excess niacin from food; only in supplemental forms (nicotinic acid 3-4x that of the RDA) causing capillary dilation and tingling sensation
•Not seen in the nicotinamide form
•Potential health benefits of large doses of nicotinic acid -may lower LDL and triglycerides; protect against heart disease if patient is not being treated with statins
Biotin:
Coenzyme that carries activated carbon dioxide
•Critical in TCA cycle
•Delivers carbon to pyruvate to form oxaloacetate
•Also participates in gluconeogenesis and fatty acid synthesis
•Breakdown of fatty acids and amino acids
Deficiency: very rare
•Symptoms include skin rash, hair loss, neurological impairment
•More than two dozen raw egg whites must be consumed daily for several months to produce these effects—protein in egg binds biotin-preventing absorption
Toxicity: No UL
Pantothenic acid:
Part of chemical structure of coenzyme A (acetyl CoA)
•Involved in more than 100 different steps in the synthesis of lipids, neurotransmitters, steroid hormones, and hemoglobin
Readily destroyed by freezing, canning, and refining processes
•Diets supply adequate amounts
•Widespread in foods (beef, poultry, whole grains, potatoes, tomatoes, and broccoli)
Deficiency:
•Rare
•Symptoms include: general fatigue, GI distress, neurological disturbances
Toxicity: None reported and no UL established
Vitamin B6:
Three forms:
•Pyridoxal, pyridoxine, and pyridoxamine
All forms can be converted to coenzyme PLP (pyridoxal phosphate)
•Amino acid metabolism
•Carbohydrate and fatty acid metabolism
•Conversion of tryptophan to niacin or serotonin
•Synthesis of heme, nucleic acids, and lecithin
•Can add and remove amino groups to make non essential AA; valuable in protein and urea metabolism
Exclusively stored in muscle tissue.
Deficiency: inflammation of the skin (dermatitis) and a red, greasy, scaly rash. The hands and feet may feel numb and prickling—like pins and needles. The tongue may become sore and red, and cracks may form in the corners of the mouth
Folate:
Folacin or folic acid
Folate disposal:
•Secretion by liver into bile
•Enterohepatic circulation
•GI tract injuries hinder absorption
Deficiency:
•Neural tube defects
•Supplement use during pregnancy
•One month before conception
•Through first trimester
•Fortified grain products
•Congenital birth defects
•Cleft lip and cleft palate
•autism
•Folate plays a role in protecting against heart disease
•Breakdown of homocysteine
•Folate may protect against the initiation of some cancers but may enhance progression of some cancers if development has already begun
Folate deficiency impairs cell division, protein synthesis, and replacement of red blood cells
Toxicity:
•Naturally occurring from food sources – no harm
•Fortified foods or supplements – UL has been established (400 micrograms per day)
Vitamin B12:
Vitamin B12 and Folate depend on each other for activation:
•When folate gives up its methyl group, the vitamin B12 coenzyme becomes activated
•Regeneration of methionine
•Synthesis of DNA and RNA
Individual roles of vitamin B12:
•Maintains the sheath around nerve fibers that protects them
•Bone cell activity and metabolism
Digestion and absorption:
•Stomach
•HCl and pepsin release vitamin B12 from the proteins to which it is attached in foods
•Small intestine
•Vitamin B12 binds with intrinsic factor, travels to the end of the SI, where receptors recognize the complex (receptors will not recognize B12 without intrinsic factor)
•Enters enterohepatic circulation, continuously secreted into bile and delivered to the intestine to be reabsorbed
Deficiency- marginal: impaired cognition; advanced: neurological symptoms (e.g., creeping paralysis in the extremities working inward and up the spine)
•Reflect inadequate absorption; not poor intake
•A lack of HCl – not released from proteins
•Lack of intrinsic factor- not recognized by receptors
•Common in elderly due to atrophic gastritis (a condition that damages the cells of the stomach)
•Deficiency from atrophic gastritis or lack of intrinsic factor = pernicious anemia
•Can be given as an injection or nasal spray to bypass intestinal absorption
•Rapidly growing blood cells are the first affect by B12 deficiency
•If folate is given when B12 is needed, consequences can be harmful (neurological symptoms)
Toxicity: No adverse effects and no UL
Choline:
Essential nutrient, not defined as a vitamin; commonly grouped w/ B vitamins.
•Used to make lecithin and neurotransmitter acetylcholine
•During fetal development, choline supports the structure and function of the brain and spinal cord (supporting NT closure and enhancing learning performance)
•Manufactured from AA methionine in body (synthesis is insufficient to meet needs)
•Conditionally essential nutrient
•Adequate intake (AI)
•Men = 550 mg/day
•Women = 425 mg/day
•UL = 3500 mg/day
•Life-threatening lowering of blood pressure
•Common sources (milk, eggs, and peanuts)
•Impact of deficiency not fully understood
Nonvitamins:
commonly mistaken as vitamins but are not essential nutrients and can be made by the body
Inositol: part of cell membrane structure
Carnitine: transports long-chain fatty acids for oxidation
PABA (para-aminobenzoic acid): a component of folates chemical structure
Bioflavonoids: (vitamin P or hesperidin)
Vitamin B interections:
Each B vitamin is involved directly/indirectly.
•Deficiencies: a deficiency in one may alter the action of another OR a deficiency in one may create a deficiency of another
•B vitamin deficiencies seldom show up in isolation
•Beriberi and pellagra
•Excesses of the nutrients are eliminated through urine excretion
Vitamin C:
serves as a cofactor helping a specific enzyme perform its job, as antioxidant (participating in more general ways), defends against free radicals, protects tissues from oxidative stress, loses electrons easily, and enhances iron absorption.
Vitamin C as a cofactor:
-Cofactor in collagen formation
--Matrix for bone and tooth formation
--Conversion of proline to hydroxyproline
-Cofactor in other reactions
--Hydroxylation of carnitine
--Conversion of tryptophan to serotonin
--Conversion of tyrosine to norepinephrine
--Making hormones
Roles of Vitamin C:
prevention and treatment of common cold (-200 mg), deactivates histamines
-10 mg/day prevents scurvy
Adrenal glands release
vitamin C and hormones into the blood
Smoking increases the need for
Vitamin C
Vitamin C deficiency and toxicity:
Deficiency:
scurvy- affects teeth & gums (bleeding), pinpoint hemorrhages
toxicity:
diarrhea, GI distress, pro-oxidant qualities at high doses
Sodium:
Electrolyte; principle cation of the extracellular fluid and regulator of volume; readily absorbed by intestinal tract -- travels in blood to kidneys
Tightly regulated by the kidneys
Function: acid-base balance, nerve impulse transmission, and muscle contraction
Sources: table salt (NaCl), processed foods, milk, meat, egg, and vegetables
Chloride:
Electrolyte; major anion of extracellular fluid, negatively charged; neutralizes the positive charge of sodium
Functions:
•Major electrolyte
•Part of hydrochloric acid
•Exchange anion; associates with potassium inside the cell
Potassium:
Electrolyte; principal intracellular cation (95% within cells)
Function:
•Maintains fluid and electrolyte balance and cell integrity
•Effects excitability of nerve tissue
•Influences contractility of smooth, skeletal, and cardiac muscle
Sources: widespread in diet, most abundant in fresh fruits and vegatables
Calcium:
Blood clotting and hormone functions; Most abundant divalent cation in the body; 40% of body's mineral mass, 99% found in bone and teeth, 1% found in intra- and extracellular fluids
Major role:
Bone structure
•Constant turnover of minerals while bones are growing and developing (similar process in teeth)
•Max bone mass achieved by 25-35 yoa in females (later in males)
•When withdrawals of minerals substantially exceed deposits, problems arise (e.g., osteoporosis)
•Calcium bank- readily available source of Ca
•All cells can detect calcium in extracellular fluids and respond accordingly (e.g., maintain normal blood pressure & blood clotting)
•Intracellular calcium: binds to proteins within cells and activates them (e.g., breaking down glycogen by binding with calmodulin; muscle contraction)
Phosphorus:
Second most abundant mineral in the body; 85% in skeleton, 14% in soft tissue, 1% in circulation
Function:
•Bone mineralization
•Cell membrane structure
•Nucleic acid formation - important for growth
•Energy transfer and storage (ATP uses 3 phosphate groups to do work)
•Activates enzymes and B vitamins
•Acid-base buffer system
•Component of phospholipids that provide stability to lipid transport vessels
Magnesium:
4th most abundant cation in the body; 50-60% in bone, 20-25% in soft tissue; 1% extracellular tissue
Function:
•Bone component
•Nerve impulse transmission
•Important for 300+ different enzyme reactions, 2 roles
•Structural cofactor
•Allosteric activator of enzyme activity
Sulfur:
found in connect tissue and functions also in metabolism
Iron:
•65% of the body's Fe is found in hemoglobin; The rest is in myoglobin, cofactor to enzymes involved in oxidation-reduction reactions (enzymes involved in making AA, collagen, hormones, and neurotransmitters all require iron), circulating or stored
•Ferric (Fe3+) and ferrous (Fe2+)
•Only forms stable in aqueous environment of body and food
Sources:
•Heme: animal products (turkey, beef, liver, etc.)
•Non-heme: plant foods (chick peas, pumpkin seeds, mushrooms, beans)
•RDA: 8 mg for men; 18 mg for females
•Deficiency: inadequate intake
•Iron-deficiency anemia
•Fatigue
Impaired work performance
Zinc:
•All cells contain zinc but in highest concentrations in muscle and bone
•Function: cofactor for 100+ enzyme (cofactor for collagenase - wound healing-, spermatogenesis and growth in children
•Sources: red meat and seafood, whole grains, leafy and root vegetables
•RDA: 11 mg male; 8 mg female
•Deficiency - delay in wound healing, decrease in adult hair (facial, pubic, axillary); hypogonadism, loss of taste and smell; suppressed immune system
Copper:
•Function - enzyme cofactor for:
•ferroxidase, attaches iron to transferrin
•lysyl oxidase, cross-links in collagen and elastic tissue
•tyrosinase, converts tyrosine to melanin
•Sources: varies widely in whole foods
•RDA: 990 ug
•Deficiency - microcytic anemia, aortic dissection, poor healing, skeletal and blood vessel abnormalities
Selenium:
•Sources: variable; dependent on soil content
•RDA: 55 ug
•Function: cofactor for glutathione, peroxidase (antioxidant role), converts peroxide to water
•Deficiency: weakness and muscle pain, dilated cardiomyopathy, loss of pigmentation in hair and skin, whitening of nail bed
•Toxicity: selenosis (vomiting, hair and nail brittleness, paresthesia)
Iodine:
•Found in thyroid gland and functions in its ionic form (iodide)
•Sources: based on soil content (iodized salt), crops grown for consumption
•RDA: 150 ug
•Function: structural role in hormones, regulating basal metabolic rate
•Deficiency:
•Cretinism: poor development in children
•Goiter: overdevelopment of thyroid gland in adults
How does the body regulate fluid balance?
Water makes up about 60 percent of the body's weight. It assists with the transport of nutrients and waste products throughout the body, participates in chemical reactions, acts as a solvent, serves as a shock absorber, and regulates body temperature.
To maintain water balance, intake from liquids, foods and metabolism must equal losses from the kidneys, skin, lungs, and GI tract. Whenever the body experiences low blood volume, low blood pressure, or highly concentrated body fluids, the actions of ADH, renin, angiotensin, and aldosterone restore homeostasis.
Electrolytes (charged minerals) in the fluids help distributes the fluids inside and outside the cells, thus ensuring the appropriate water balance and acid-base balance to support all life processes. Excessive losses of fluids and electrolytes upset these balances, and the kidneys play a key role in restoring homeostasis.
Sodium deficiencies and toxicities:
Deficiencies: •Does not develop from inadequate diet
•Results from vomiting, diarrhea, and heavy sweating
•Anorexia, nausea, muscle atrophy, poor growth, and weight loss
•Hyponatremia: loss of sodium + too much water = headache, confusion, seizures, stupor
Toxicities:
•Immediate: Edema and high blood pressure
•Prolonged: Hypertension
•High sodium intake associated with increased calcium excretion
Phosphorus deficiencies and toxicities:
•Deficiencies: rare--found in almost all foods (meat, poultry, fish, eggs = highest; nuts, legumes, cereals, grains, vegetables)
•Renal disease, neuromuscular, skeletal, and cardiac conditions
•Toxicity: UL = 4,000 mg (if diet contains an excessive amount of processed foods)
•Kidney failure, heart disease, bone loss
•Disruptions in normal hormonal functions
Calcium deficiencies and toxicities:
Deficiency:
•Related to inadequate intake
•Rickets (children) and osteoporosis (adults)
•Tetany (intermittent muscle contractions, fail to relax)
•Long-term deficiency
•Osteoporosis, hypertension, colon cancer, type 2 diabetes and obesity
•Toxicity:
•UL = 2,500 mg/day (19-50 yoa); 2,000 mg/day (>51 yoa)
•Mild toxicity = constipation, bloating, gas
•Hypercalcemia = lethargy, anorexia, vomiting, heart arrhythmias
•Calcium-containing kidney stones
Potassium deficiency and toxcitiy:
Deficiency:
•Increase in blood pressure, kidney stones, bone turnover
•Progressive symptoms: irregular heartbeats, muscle weakness, and glucose intolerance
Toxicity:
No UL is set; results from overconsumption of potassium salts or supplements
Chloride deficiency and toxicity:
Deficiencies:
•Can result from excessive vomiting (bulimia nervosa)
•Infants: loss of appetite, weakness, lethargy, sever hypochloremia, metabolic acidosis
Toxicities:
•Vomiting
Magnesium deficiency and toxicity:
Deficiency: muscles spasms/cramps, restless leg syndrome, insomnia, chronic fatigue, nausea and vomiting
Toxicity: from food = no health risk; from supplements = diarrhea, nausea, abdominal cramping; risk increases with impaired renal function
Conditions associated w/ Copper:
•Menke's syndrome: sex-linked recessive defect; deficiency
•-Cu malabsorption leading to an increase in Cu loss and abnormal intercellular Cu transport
•-Decreased activity of lysyl oxidase
•-Brittle hair
•-Growth retardation
•-Hypotonia
•Wilson's Disease: autosomal recessive; toxicity (vegetarian diet is recommended)
•-Excessive accumulation of copper (poor elimination Cu into bile)
•-Chronic liver disease
•-Basal ganglia degeneration
•-Kayser-Fleischer ring around cornea
Describe the physiological processes that influence food intake
Hunger and appetite are likely to increase food intake. Satiation determines how much food is consumed during a meal. Satiety inhibits eating until the next meal; it determines how much time passes between meals. A high level of satiety is likely to decrease food intake between meals.
Identify the components of energy expenditure and factors that influence each
1. Basal Metabolic Rate- Energy needed to maintain core body functions.
2. Physical Activity - Energy needed to move muscles.
3. Thermic effect on food - energy needed to process food.
Identify methods to assess both body weight and body composition
Body Mass Index, skinfold measurements, waist and hip circumferences, sagittal abdominal diameter
The body mass index (BMI) is based on weight relative to height and serves as a reliable indicator of chronic disease risks, but it says little about body composition. The ideal amount of body fat varies from person to person, but researchers have found that body fat in excess of 22 percent for young men and 27 percent for young women (the levels rise slightly with age) poses health risks. Central obesity is measured by waist circumference and indicates excess abdominal fat undisturbed around the trunk of the body. Central obesity contributes to chronic obesity.
Identify relationships between body weight and chronic diseases (underweight, overweight)
The weight appropriate for and individual depends largely on factors specific to that individual, including body fat distribution, family health history, and current health status. At the extremes, both overweight and underweight carry clear risks to health.
Identify the nutrients involved in energy metabolism and the various high energy compounds that captures the energy released during their breakdown
During digestion the energy-yielding nutrients—carbohydrates, fats, and proteins—are broken down to glucose (and other monosaccharides), glycerol, fatty acids, and amino acids. With the help of enzymes and coenzymes, the cells use these molecules to build more complex compounds (anabolism) or break them down further to release energy (catabolism).
High-energy compounds such as ATP may capture the energy released during catabolism and provide the energy needed for anabolism.
pyruvate
Describe the difference between anabolic and catabolic reactions and provide examples of each
Anabolic reactions use energy to build complex molecules from simpler organic compounds (e.g., proteins from amino acids, carbohydrates from sugars, fats from fatty acids and glycerol); catabolic reactions break complex molecules down into simpler ones, releasing chemical energy.
Summarize the main steps in the energy metabolism of glucose, glycerol, fatty acids, and amino acids
Carbohydrate, fat, and protein take different paths to acetyl CoA, but once there, the final pathways—the TCA cycle and electron transport chain—are shared.
The digestion of carbohydrates yields glucose (and other momosaccharides): some is stored as glycogen, and some is broken down to pyruvate and acetal CoA to provide energy. The acetyl CoA can then enter the TCA cycle and electron transport chain to provide more energy. The digestion of fat yields glycerol and fatty acids; some are reassembled nd stored as fat, and others are broken down to acetyl CoA, which can enter the TCA cycle and electron transport chain to provide energy. The digestion of protein yields amino acids, most of which are used to build body protein or other nitrogen-containing compounds, but some amino acids may be broken down through the same pathways as glucose to provide energy. Other amino acids enter directly into the TCA cycle, and these, too, can be broken down to yield energy. In summary, although carbohydrate, fats and protein enter the TCA cycle by different routes, the final pathways are common to all energy-yielding nutrients.
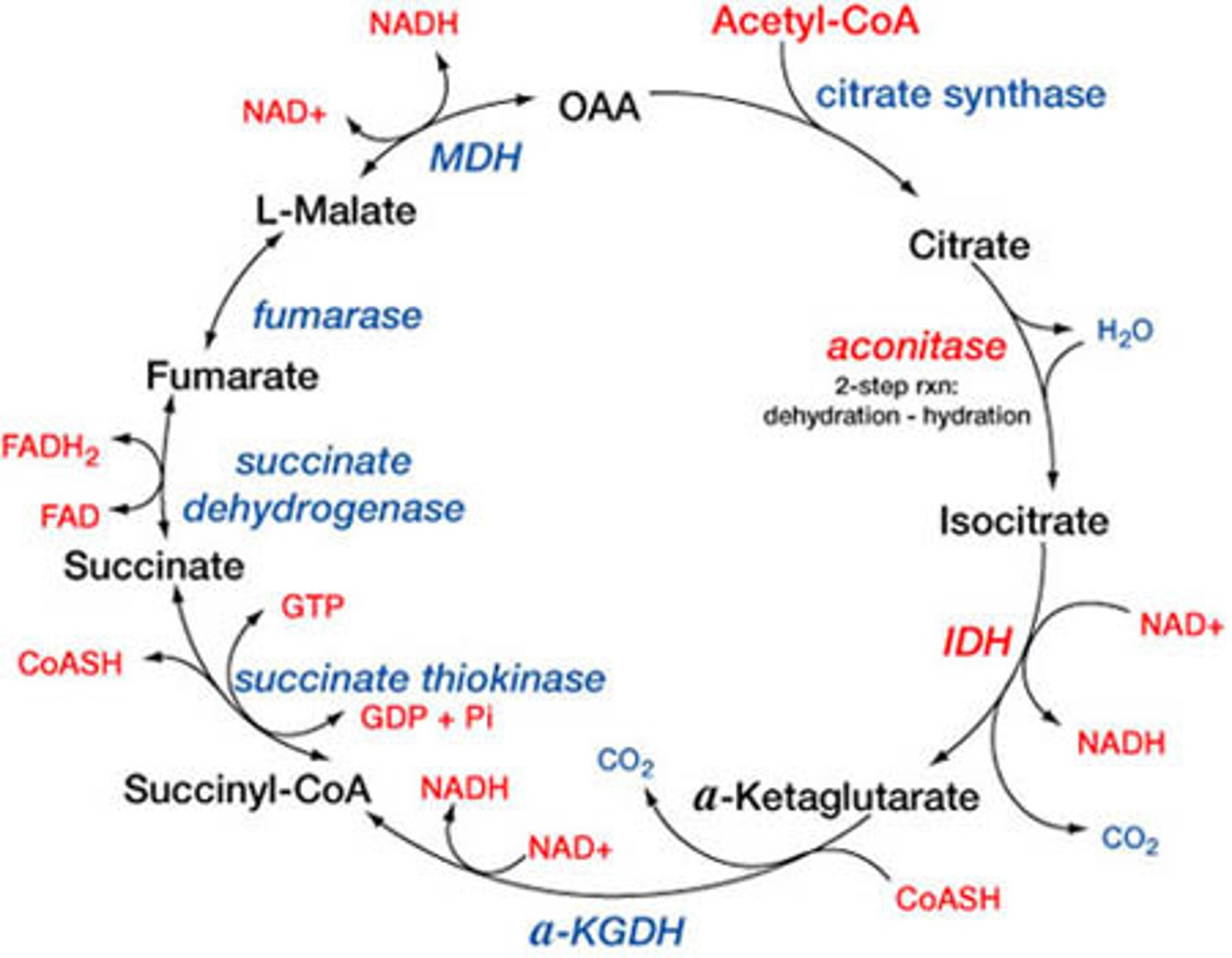
TCA cycle:
this is for complete oxidation of acetyl CoA
if there is sufficient oxygen in the cell, the pyruvate continues down the pathway to acetyl CoA and enters the TCA cycle
deaminated amino acids can be oxidized in the TCA cycle
occurs in the mitochondria, begins with acetyl CoA. its products are hydrogen atoms and electrons --- transported to electron transport chain for ATP synthase
Explain how an excess of any of the three macronutrients contributes to body fat
When energy intake exceeds energy needs, the body makes fat- regardless of whether the excess intake is from protein, carbohydrate, or fat.
The only difference is that the body is much more efficient at storing energy when the excess derives from dietary fat.
When fasting, the body makes a number of adaptations: increasing the breakdown of fat to provide energy for most of the cells, using glycerol and amino acids to make glucose for the red blood cells and central nervous system, producing ketones to fuel the brain, suppressing the appetite, and slowing metabolism. All of these measures conserve energy and minimize losses.
Low carbohydrate diets incur similar changes in metabolism.
Electron transport chain:
formation of ATP is generated from the energy released in glycolysis and TCA cycle
electrons are passed along by protein complexes. hydrogen ions are used to form ATP during oxidative phosphorylation, and join with oxygen to make water
The electron transport chain captures energy the high-energy bonds of ATP. The electron transport chain consists of a series of proteins that serve as electron "carriers."
1- Coenzymes deliver hydrogens and high energy electrons to the electron transport chain from the TCA cycle, glycolysis, and fatty acid oxidation
2-Passing electrons from carrier to carrier along the chain releases enough energy to pump hydrogen ions across the membrane
3- Oxygen accepts the electrons and combines with hydrogens to form water
4- Hydrogenions flow "downhill"--from an area of high concentration to an area of low concentration--through a special protein complex that powers the synthesis of ATP
Describe the function and requirements for the ingredient lists on food products
Ingredient List:
•All ingredients (including additives)
•Listed in descending order of predominance by weight
Serving Size:
•Established by FDA; uniform across all labels for a given product
•E.g., ice cream = 1 cup
Nutrient Quantities:
•In grams
•In percentages as the Daily Values: ballpark estimates based on 2000 kcal/day (needs vary based on age, physical activity, and other factors)
•% Daily Values and grams required for: Food energy, total fat, saturated fat, trans fat, cholesterol, sodium, carbohydrates, fiber, sugars, added sugars, protein, vitamin D, and minerals (calcium, iron, potassium) (*grams not required for vitamin D and minerals)
Recall the diet planning principles; explain how each can be used to plan a healthy diet
adequacy: sufficient energy and enough nutrients, meeting EAR and hopefully RDA
balance: enough but not too much
kcal control: key is to select high nutrient density foods
moderation: occasionally low nutrient density foods, keep calorie intake in check
variety: "eat the rainbow"nutrient
density: maximum nutrients on a limited energy budget, avoid empty kcal foods
Differentiate between claims on labels (e.g., nutrient, health, structure-function)
•Nutrient claims: characterize the level of a nutrient in the food—for example, "fat free" or "less sodium."
•Health Claims: characterize the relationship of a food or food component to a disease or health-related condition—for example, "soluble fiber from oatmeal daily in a diet low in saturated fat and cholesterol may reduce the risk of heart disease" or "a diet low in total fat may reduce the risk of some cancers."
•Structure-function claims: describe the effect that a substance has on the structure or function of the body and do not make reference to a disease—for example, "supports immunity and digestive health" or "calcium builds strong bones."
Integrate behavior change models into an assessment of individuals willingness, compliance, and success with nutrition intervention strategies
•Modification - positive outcomes on health
•Awareness - keep record
•Change - small, specific goals; practice; rewards
Cognitive skills
•Problem solving
•Integrate meal plan and physical activity into lifestyle so as to maintain weight loss
•Restructuring (replacing negative thoughts)
•Personal attitude - emotional health, understanding relationships with food
•Identify and interrupt cues to inappropriate eating behaviors
•Support groups - build a network
Identify various effective approaches to nutrition care (e.g., long-term dietary care, education, etc.) and ineffective approaches
Food and/or nutrient delivery:
Providing appropriate meals, snacks, and dietary supplements
Providing specialized nutrition support (tube feedings or parenteral nutrition)
Determining the need for feeding assistance or adjustment in feeding environment
Managing nutrition-related medication problems
Nutrition education:
Providing basic nutrition-related instruction
Providing in-depth training to increase dietary knowledge or skills
Providing information about a modified diet or change in formula
Nutrition counseling:
Helping the individual set priorities and establish diet-related goals
Motivating the individual to change behaviors to achieve goals
Solving problems that interfere with the nutrition care plan
Coordination of nutrition care:
Providing referrals or consulting other health professionals or agencies that can assist with treatment
Organizing treatments that involve other health professionals or health care facilities
Arranging transfer of nutrition care to another professional or location
Ineffective approaches:
•Diet books and weight loss programs/products
•Maintenance of behavior change
•Fad diets
•Herbal supplements
Recall the current nutritional recommendations for adolescents and adult women during preconception and pregnancy.
Maternal Nutritional Needs
•Buildup of structures to support fetal growth
•Uterus, placenta, mammary glands
•Increased blood volume, metabolism
•Nutrients going to baby
•Difficult to catch up and/or keep up once pregnant
•Adequate nutrition status to begin with
•Competition for space in abdominal cavity à feel full faster; smaller, more frequent meals
Fetal Nutritional Needs (1 cell à trillions of cells)
•Primary: development/growth of body structures
•Muscles, nerves, organs, bones, CNS
•Small amount for maintenance metabolism
Energy Requirements:
•First trimester- energy needs remain the same for non pregnant women
•Second trimester- energy needs increase 340 kcals/day
•Third trimester- energy needs increase 452 kcal/day
•Multiparous- 40-45 kcal/kg pre-pregnancy weight/day
Carbohydrates: fuels fetal brain; protein sparing
•~175 g/day (or more)
Protein: supports tissue growth and development in mom and fetus
•0.8 g/kg/day in first trimester through first half of second trimester
•1.1 g/kg/day during 2nd half of 2nd trimester through the third trimester - ~additional 25 g/day more than non pregnant women
Essential Fatty Acids: fetal nerve and vision development- brain growth, structure, and function
Fiber: adequate laxation (progesterone decreases intestinal motility) and provision of phytochemicals (protect against metabolic stress)
•25-30 g/day (avg. for females = 7-12 g/d)
Identify various types of foods or supplements that should be included or avoided in the diet during this period.
Explain how maternal malnutrition can affect critical periods of fetal and maternal growth
During pregnancy, poor diets lacking in key nutrients – like iodine, iron, folate, calcium and zinc – can cause anaemia, pre-eclampsia, haemorrhage and death in mothers. They can also lead to stillbirth, low birthweight, wasting and developmental delays for children.
Identify the target goals for BMI and weight gain in normal, under- or overweight for healthy pregnancies and fetal development; based on pre-pregnancy heights and weights.
Explain how both underweight and overweight can interfere with a healthy pregnancy and how weight gain and PA can support maternal health and infant growth
Weight gain
- Highly variable
- One third is only due to growing foetus
- Breast tissue gets ready for lactation
- Fat reserves deposit in the abdomen, thighs and back, to support foetal growth and later lactation
Maternal weight stator is an important predictor of pregnancy outcome
- Preconception obesity ↑s risk of gestational diabetes, preeclampsia, higher birth weight, complications at birth and birth defects- Underweight prior to pregnancy ↑s risk malnutrition and small weight for gestational age ("fetal programming").
- Optimal weight gain depends upon pre- pregnancy body mass index (BMI)
- Underweight women need to aim for more weight gain
- Overweight women may need to control weight gain
Summarize nutrient and physical activity needs of women during pregnancy
2nd trimester: 340kcals
3rd trimester: 450kcals increased
B12
Iron
Zinc
Protein +25g
Essential fatty acids (brain growth)
CHO (fuel infants brain)
Describe how maternal health may impact the ability for mothers to breastfeed
Describe the typical growth rate of infants in their first years of life and their energy requirements
Of all stages of the life cycle, growth rate is highest during infancy.
At birth, the average infant is 7.5 pounds (about 3.5 kg) and 20 inches (about 50 cm) long.
Infant weight usually doubles from birth to 6 months of age and triples from birth to 12 months of age.
Infant height usually increases by 50% from birth to 12 months of age.
Growth is not linear (growth spurts are followed by plateaus).
Per kilogram of body weight, needs for most nutrients are highest during infancy.
Describe the appropriate foods for infants during the first year of life and strategies for their introduction
· An infant must be physically and physiologically ready before being introduced to solid foods.· Solid foods should be introduced gradually and cautiously.· Choking hazards and honey should be avoided, and infants should always be supervised while eating.· Avoid excessive amounts of seasonings such as salt, sugar, and butter in the infant's diet, as well as too much fiber.
Identify which nutrients are most commonly given as supplements within the first year of life
breastfed babies are generally recommended to receive a vitamin D supplement daily. breastfed babies of vegan mothers may need a vitamin B12 supplement. all breastfed babies should receive an iron supplement daily from birth.
Identify the nutritive and non-nutritive characteristics and functions of breast milk.
Describe why iron deficiency and obesity are often concerns during childhood
Iron deficiency a concern?-because associated w/ impaired cognitive development
Children grow out then up
32% overweight (>95%ile)
17% obese (>85%ile)
Normal= 10-85th
List the macro- and micro- nutrient recommendations for children and how they compare to adults
Identify inappropriate and appropriate behaviors for children and feeding strategies for parents during mealtimes
Describe the challenges of meeting the nutrient needs of adolescents
Calcium- 1300mg
Iron
males- 11mg
females- 15-18 mg
KCals
-vary depending on physical activity and growth spurts
Lots of soda, fast food, less milk, less fruit and veggies(Family mealtimes improve diet quality)
List federally and state funded school lunch programs and the guidelines they must follow
Explain the nutritional and metabolism shifts from adolescents to adulthood
Summarize how nutrition interacts with physical and psychological changes involved in aging
-moderately overweight can help/ protective in times of illness (2/3rds older adults are overweight/ obese)
-sarcopenia: loss in skeletal muscle mass, strength, and quality
-loss of eye sight-tooth loss-taste changes
-dysphagia (difficulty swallowing)
-less ghrelin (smaller appetite)
-more cholecystokinin (CCK) (satiety)
-slower motility
Psychological changes
-depression
Economic changes
-9% live in poverty
Explain why the needs for some nutrients increase or decrease during aging (e.g., water, vitamins, minerals, etc.)
Energy needs decline 5% / decade
-less physical activity
-thyroid function declines
Iron needs decrease women after menopause
Nutrients increased
-calcium (decreased absorption)
-vit D (decreased synthesis)
-folate (low hcl impairs absorption)
-vit b 12
-zinc (deficiency decreases appetite and blunts sense of taste)
-water (blunted thirst sensation-
-dehydration, confusion, pressure ulcers
Explain why energy needs increase or decrease during aging