GU 4 - Abnormalities of Menstruation
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
Normal menstruation parameters (cycles) are between > 24 and ______ days, with a duration of < 8 days.
< 38
What are some structural causes of AUB?
PALM
- polyps
- adenomyosis
- leiomyoma (fibroids--- gen. from muscle (myo) tissue)
- malignancy/hyperplasia
What are some non-structural causes of AUB?
COIEN
- coagulopathy (vwd)
- ovulatory dysfunction
- endometrial
- iatrogenic
- not yet classified
What is a first line diagnostic evaluation test for abnormal uterine bleeding?
trans-vaginal US
note: pap test if due; you can also do a cervical swab and endometrial sampling
What hormone(s) peak right before ovulation?
LH, FSH, estradiol
When does body temperature peak in the menstrual cycle?
Following ovulation, in the luteal phase
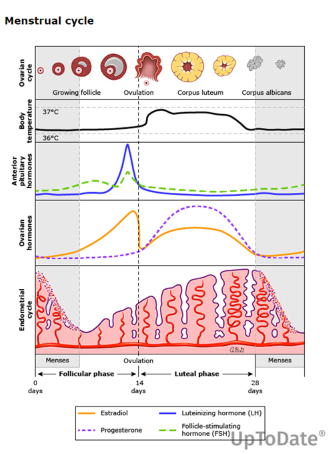
When are the follicular and luteal phases?
follicular phase - 1-14
luteal phase - 14-28
ROUGHLY, for a 28 day cycle
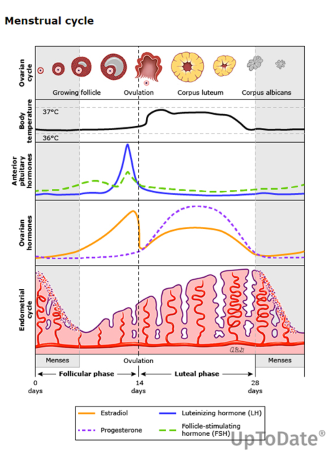
When does progesterone peak?
mid luteal phase
Ovulatory bleeding is often caused by ________ or ______ issues, and anovulatory bleeding is often caused by _______ issues.
ovulatory - usually structural or hemostasis
anovulatory - PCOS, Endocrine disorders, stress, anorexia, iatrogenic
What is the purpose of doing a saline infused sonogram?
clearer visualization of uterine cavity to help look for fibroids, polyps, etc.
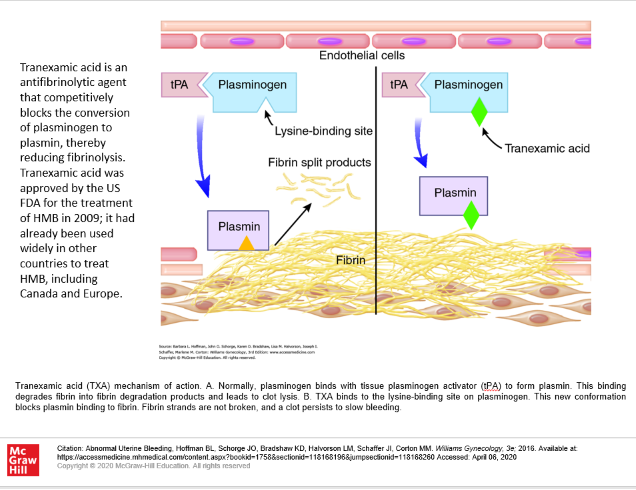
How should a patient on TXA (Lysteda) for heavy menstrual bleeding be counseled to take their medication if they desire pregnancy?
Take TXA only during active menstrual cycle, as it is contraindicated in pregnancy
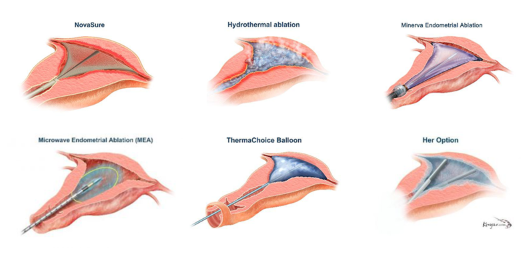
What are some contraindications to endometrial ablation? What is this used to treat?
desire for future pregnancy
hyperplasia/malignancy
post-menopausal
significant cavity distortion
Endometrial ablation is a treatment for HMB which can be used in pre-menopausal patients who have no desire for future pregnancy and who don’t have hyperplasia, malignancy, or significant cavity distortion.
Which of the following options may be used as management for heavy menstrual bleeding?
a. combined hormonal contraceptives
b. oral progestin
c. depo-provera
d. NSAIDs
e. TXA (Lysteda)
f. all of the above
f. all of the above
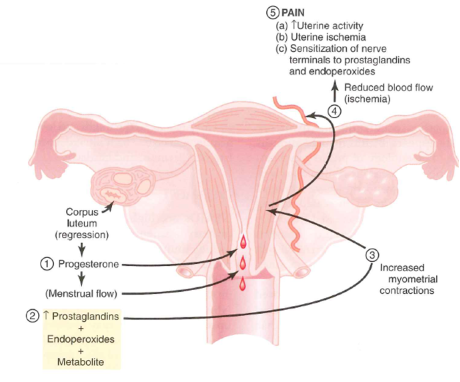
NSAIDs work because of prostaglandins
NOTE: NSAIDs and TXA should only be taken during menstruation to avoid potential harm to embryo/fetus
also, NSAIDs may worsen bleeding in some patients, i.e. those on anticoag tx for bleeding disorder
True or False: Oral progestin can be used for AUB-O in patients who desire pregnancy.
True; medroxyprogesterone acetate (provera) oral, not the depot. can be used cyclically 5-26 in patients who want to be pregnant
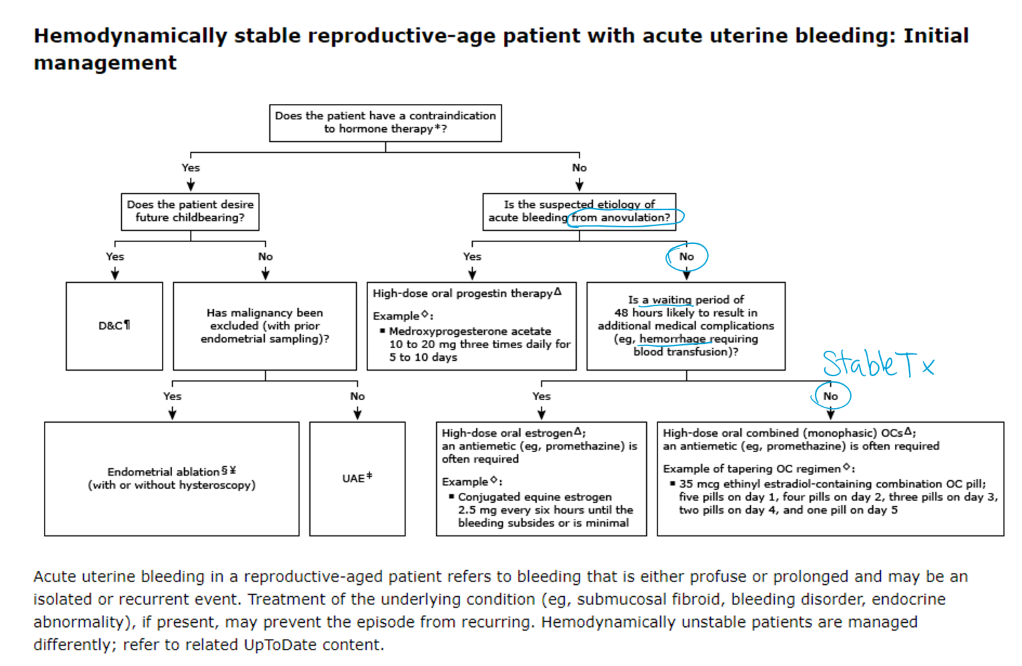
How does IV estrogen treat acute uterine hemorrhage? In who is it contraindicated?
IV estrogen signals body to regrow endometrium and stop bleed; there is a risk of DTE, so they have to be a candidate to receive it.
Other options include fluid resus and blood replacement, uterine curettage, and uterine tamponade (U. Tamponade is where they put a balloon in uterus and blow it up to help compress vessels and stop bleeding, esp. in cases of a relaxed uterus (i.e. post partum))
hysterectomy may be needed if above tx unsuccessful
A patient who is on COC presents with intermenstrual bleeding, and you decide to change her to a pill with a higher dose of estrogen. Why might an increased dose of Estrogen help with her bleeding?
A pill with more estrogen can help reduce intermenstrual bleeding because it helps stabilize the uterine lining (endometrium), making it less prone to shedding and bleeding between periods.
In some cases, low-dose estrogen pills may not provide enough estrogen to adequately support the endometrium, leading to a thinner, more fragile lining that is prone to bleeding between periods (breakthrough bleeding).
Higher Estrogen Doses and Endometrial Stability:
Increasing the estrogen dose in a birth control pill can help thicken and stabilize the endometrium, making it less likely to bleed unexpectedly.
When should a patient with primary dysmenorrhea begin taking NSAIDs?
1-2 days prior to expected menses
Secondary Dysmenorrhea usually develops in patients aged ____ and is usually associated with other symptoms such as…
30-40 yo; usually associated w ssx such as dyspareunia, infertility, AUB
Name some potential underlying causes of secondary dysmenorrhea.
pelvic inflammatory disease; uterine fibroids; ovarian cysts; pelvic congestion; endometriosis
Define primary amenorrhea
failure to reach menarche (no menses age 15-16 with normal growth and secondary sexual characteristics; or , no menses by age 13-14 w complete absence of secondary sexual characteristics
What is the #1 cause of secondary amenorrhea?
pregnancy
A 16 year old patient presents to the clinic because they have not yet menstruated. They have a short stature and shield shaped thorax. Their FSH and LH is elevated. What should your next step be?
evaluate for turner syndrome or presence of Y chromatin (karyotype)
A patient with a uterus and primary amenorrhea has normal FSH and LH levels. What should you consider as a cause?
consider outflow tract obstruction (imperforate hymen)
What are some labs you should look at in the evaluation of secondary amenorrhea?
Name 5.
Pregnancy test, LH, FSH, TSH (thyroid), prolactin (pituitary causes)
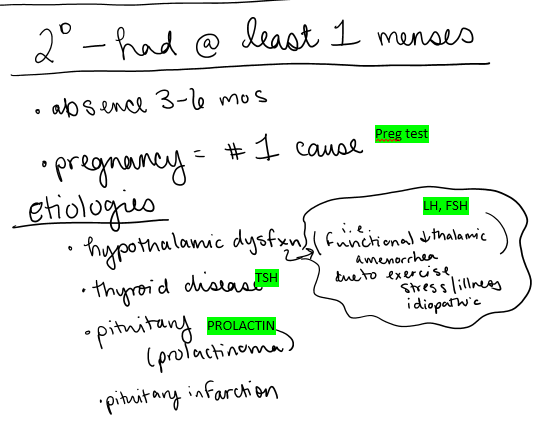
How can prolactin affect gonadotrophs (and cause menorrhea)?
elevated prolactin may induce amenorrhea by inhibiting gonadotrophs (this is why we check for prolactin when evaluating for amenorrhea)
https://www.aafp.org/pubs/afp/issues/2019/0701/p39.html
How does Sheehan syndrome affect menstruation?
this is a syndrome caused by postpartum hemorrhage, which leads to pituitary infarct. Can lead to amenorrhea (because it’s not able to produce LH and FSH)
this syndrome is more common in areas with limited obstetric care
What is Asherman’s syndrome?
(Hint- it affects uterus and can lead to amenorrhea)
scarring of endometrial lining due to previous infection or surgery
How does the hormonal progestin challenge work?
10mg of oral progestin (medroxyprogesterone) for 10 days- then they see if withdrawal bleeding occurs.
+ withdrawal bleeding - estrogen exposure/PCOS
- withdrawal bleeding - low estrogen condition
A patient with secondary amenorrhea does the hormonal progestin challenge and does NOT experience withdrawal bleeding after finishing the ten day course of Provera. What does this indicate?
a low estrogen condition
A patient with secondary amenorrhea does the hormonal progestin challenge and DOES experience withdrawal bleeding after finishing the ten day course of Provera. What does this indicate?
Estrogen exposure… may have PCOS
True or False - a patient without a uterus cannot get PMS
false; if they still have ovaries they may still experience PMS
True or False - a patient must have a symptom free interval during follicular phase in order to meet diagnosis of PMS
True
true or false - SSRIs may be taken cyclically for PMS or PMDD (more severe form of PMS with 5+ ssx) and side effects/AEs should decrease over time