cardiology
1/293
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
294 Terms
defibrillation vs cardioversion
- elective or emergency
- synchronised or non
- high or low energy
- for which types of patients
defib - emergency, non sync, high energy, for cardiac arrests
cardioversion - elective/emergency. sync to R wave, lower energy, for patients WITH PULSE
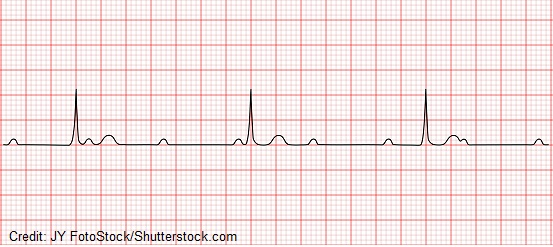
ventricular tachycardia is
a broad complex tachycardia ordiginating from a ventricular ectopic focus, regular or fast rhythm, P wave migh be present or absent
symptoms : lightheadedness, palpitations, chest pain
ECG shows broad complex tachycardia,
conscious/semiconscious
atrial activity present
haemodynamically stable
diagnose and treat
ventricular tachycardia, give amiodorone
ECG shows ventricular tachycardia and haemodynamically unstable, (sbp<90), treatment is
cardioversion (shock). he is unstable but has a pulse
patient is unconscious, collapsed or not breathing, no pulse.
it could be _________, management will be ___________
vFib…defibrillation = asynchronised shock
if patient is still conscious and with a felt pulse, it is likely
ventricular tachycardia, not vFib
ventricular tachycardia is managed by ________ if the patient is stable, and by _________ if unstable. if no pulse, ___________
amiodorone…cardioversion…immediate defibrillation
main cause of ventricular tachycardia
hypokalemia (<K)
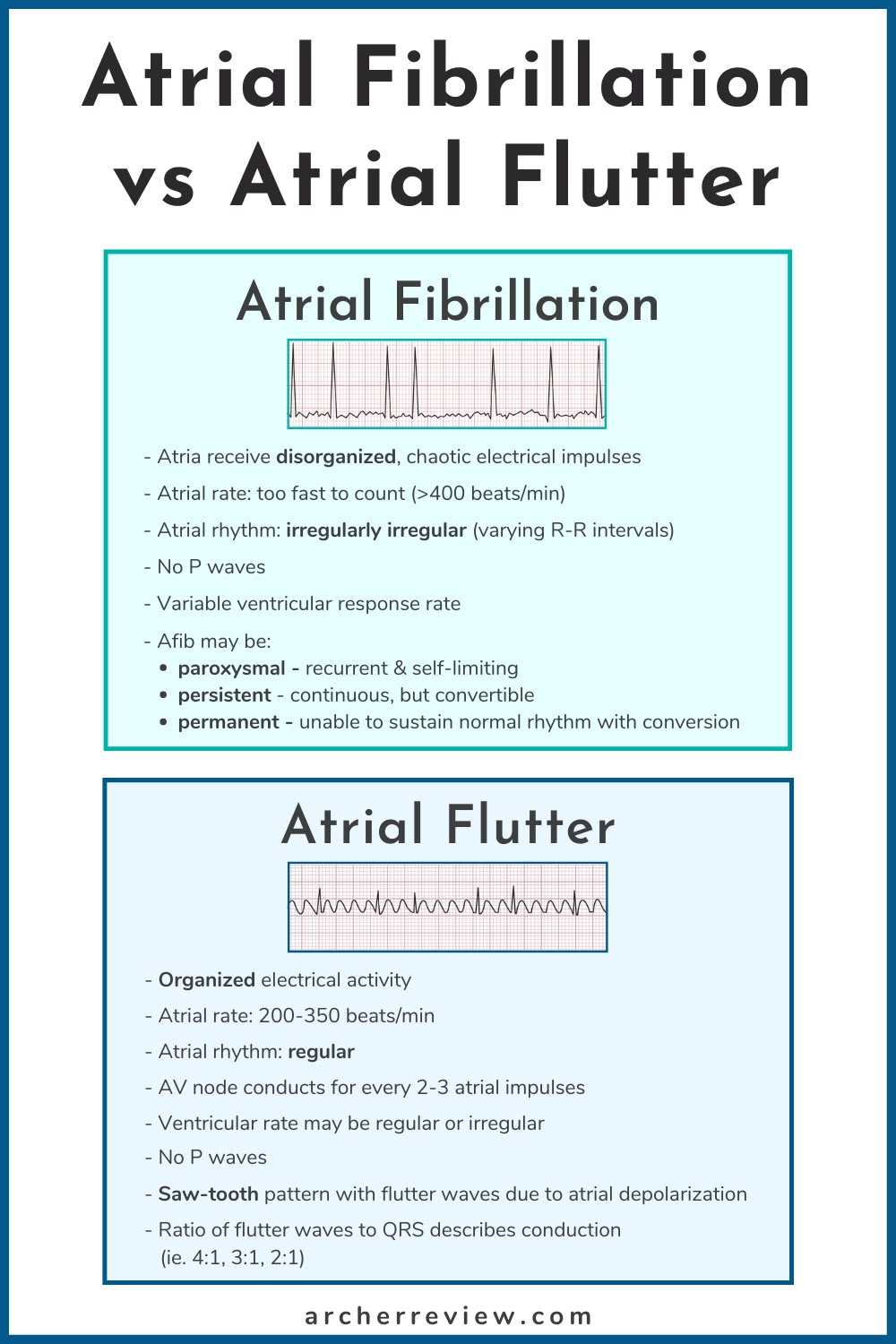
symptoms and features of aFib
basic management
palpitation, tachycardia, dyspnoea
fibrillatory wave on ecg, irregularly irregular rythm
give BB
if asthmatic give Ca blocker
if haemodynamically unstable give cardioversion
if cardioversion not available give IV amiadarone
symptoms and features of atrial flutter
basic management
fluttering feeling in chest, sawtooth waves on ecg
synchronised cardioversion
sinus bradycardia. definition, symptoms and treatment
Sinus bradycardia is a heart rhythm where your heart beats slower than expected.
normal in young athletes
lightheadedness, hypotension, vertigo, syncope, dizziness
dizziness, unwell → atropine
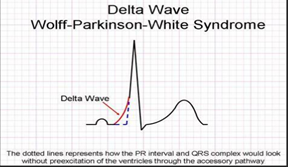
wpws. definition and ecg peculiarity
Wolff-Parkinson-White (WPW) syndrome is a condition that causes the heart to beat abnormally fast for periods of time.
delta wave on ecg
narrow complex supraventricular tachycardia (SVT)
symptoms, treatment
palpitations, lightheadedness, recurrent, usually in younger patients
initial line : valsava manoeuvre, carotid massage
not improved : iv adenosine
polymorphic (broad complex) ventricular tachycardia = Torsades De Pointes (TDP)
symptoms, treatment
no uniform pattern of ventricular contractions
broad QRS, prolonged QT, fainting episodes
young athletes
IV MgSo
atrial fibrillation is
an irregular and often very rapid heart rhythm.

atrial flutter is
a saw tooth patterned arrhythmia

atrial fibrillation vs atrial flutter
(electrical activity, atrial rate, atrial rhythm, P waves, types)
treatment of aFib on stable patient
BB (atenolol,bisoprolol,metoprolol) - contra for asthma
Ca channel blocker (verapamil,diltiazem) - used for asthma
Digoxin (preferred for patients with coexistent heart failure)
treatment of aFib on haemodynamically unstable patient (SBP <90)
cardioversion (shock)
treatment of aFib on unstable patient (hypotension), aFib has just started and no cardioversion in the option, pick
IV amiodarone
management of atrial flutter
cardioversion (shock)
degrees of heart blocks
first, second (mobitz I,II and 2:1) and third
characteristics of first degree heart block
PR interval > 0.2 seconds (larger than 5 small squares)
characteristics of second degree heart block (type 1)
progressive prolongation of PR interval until a dropped beat occurs

characteristics of second degree heart block (type 2)
PR interval is constant + dropped beat
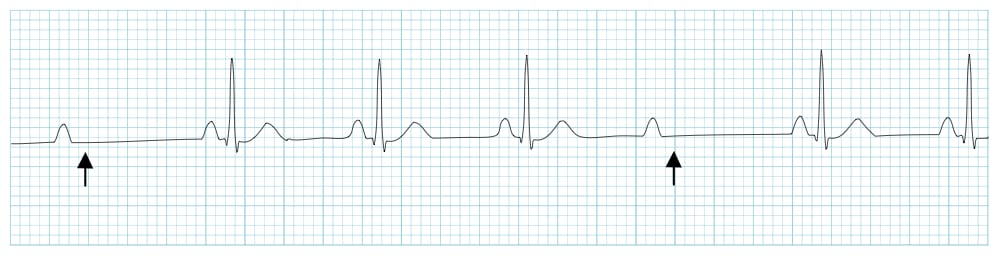
characteristics of second degree heart block (2:1)
occurs when every other P wave is not conducted through the AV node

characteristics of third degree heart block
no relation between P wave and QRS complex, P>QRS
management of first degree AV heart block and Mobitz type 1
does not require treatment as long as the patient is asymptomatic
management of Mobitz type 2 and complete heart block (3rd degree)
atropine (for symptomatic bradycardia)
transcutaneous pacing
transvenous pacing
permanent pacing (pacemaker)
acute coronary syndrome is
reduced blood flow to the heart
ischemic chest pain could be
unstable angina, STEMI or NSTEMI
STEMI is characterised by
-completely occlusive thrombus
-high troponin level
-elevated ST segments on ECG
-severe symptoms
ACS treatment
MONA (morphine, oxygen therapy, nitrates, aspirin)
clinical picture of MI
-chest pain (left-sided, epigastric, central, anteroseptal)
-irradiate to jaw, shoulder and habd
-’elephant on chest’
-dyspnoea
-paleness
-nausea and vomit
risk factors of MI (modifiable and non)
modifiable (age, male, fam history)
non-modifiable (SMOKING, diabetes, hypertension, hypercholestrolemia, obesity)
diabetic patient with MI may not experience chest pain, it is known as
silent MI
Types of MI
lateral, anterior, inferior and anterolateral MI
lateral MI (ST elevated leads on ECG leads and which artery is most likely occluded)
lead : I, avL, V5,V6
left circumflex artery
inferior MI (ST elevated leads on ECG leads and which artery is most likely occluded)
lead : II, III, avF
right coronary artery
anterior MI (ST elevated leads on ECG leads and which artery is most likely occluded)
lead : V1-V4
LAD artery
anterolateral MI (ST elevated leads on ECG leads and which artery is most likely occluded)
lead : I, avR, V4-V6
LMCA occlusion ECG findings and diagnostics
widespread of ST depression
ST elevated on avR
emergency coronary angiography
gold standard treatment of STEMI
PCI - angioplasty through radial or femoral artery
if PCI is not available for the treatment of STEMI, we prescribe
alteplase > streptokinase
chronic long term management of STEMI
aspirin, ACEi, BB, Clopidogrel, Statin
management of NSTEMI and unstable angina
aspirin + LMWH
LMWH examples
deltaparin, enoxaparin and fondaparinux
LMWH should not be administered for patients with
high risk of bleeding and are having angiography within 24h
unfractioned heparin is administered in patients with
creatinine level >265
angiography in 24h
how are unfractioned heparin and LMWH administered
LMWH & fondaparinux - subcutaneous
unfractioned - IV
atrial myxoma is
primary heart BENIGN tumour (tumor started within the heart)
inherited atrial myxoma is known as
familial myxoma (10%)
75% of atrial myxoma occur in
left atrium ( grown on the inter atrial septum wall)
feature of obstruction of mitral valve
mid-diastolic murmur, dyspnea, syncope, congestive HF
small pieces of atrial myxoma may break off and travel to arteries causing _______ of different parts of body such as
- _____ can cause ________
- _____ can cause ________
- _____ can cause ______ and _______
ischemia
-lung…pulmonary embolism
-brain…stroke
-peripheries…clubbing and blue fingers
diagnostics of atrial myxoma
echo (mass attached to fossa ovalis - inter atrial septum)
treatment of acute limb ischemia which develops ‘sudden painful swollen limb + loss of pulse‘
embolectomy - urgent catheter
how many axis deviation types are there
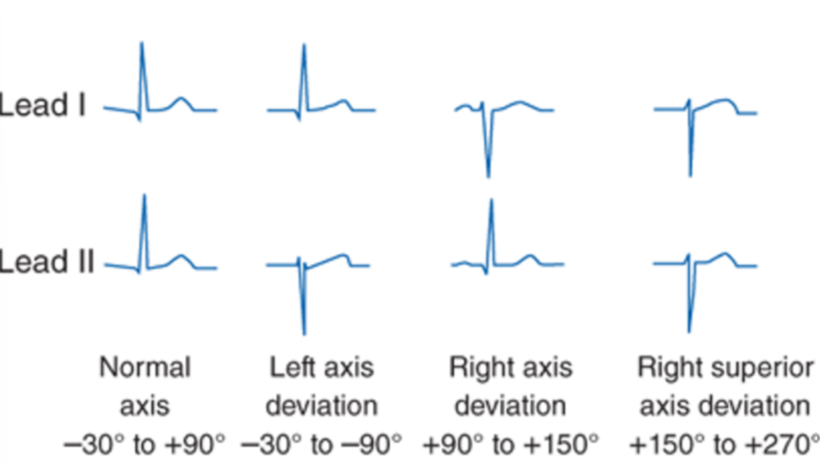
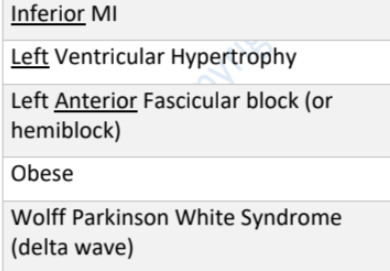
causes of left axis deviation
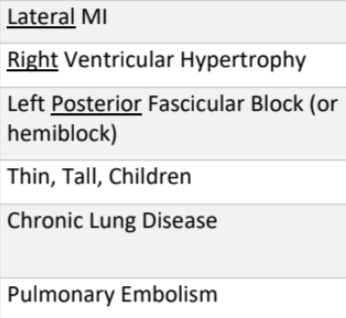
causes of right axis deviation
causes of extremer right axis deviation (no man’s land)
congenital heart disease and left ventricular aneurysm
definition of cardiac tamponade
accumulation of pericardial fluid under pressure
berks triad involves
hypotension, heart murmur and jvp
plexus paradoxus
pressure decreases during inspiration
cause of cardiac tamponade
trauma
chest x-ray shows enlarged globular heart, it could be
cardiac tamponade or pericardial effusion.
diagnostic of cardiac tamponade
echocardiogram
pericardial effusion : sign
water bottle sign (cardiothoracic ratio > 0.5)
treatment of cardiac tamponade
oxygenation and ventilation, 1-2L of IV normal saline, pericardiocentesis
symptoms of infective endocarditis are
fever, new onset murmur
+ rigor, malaise
main diagnostic of infective endocarditis is
blood culture → echo
risk factors of infective endocarditis
-history of infective endocarditis
-congenital heart defect
-prosthetic valve
-IV drug use
-rheumatic valve disease
causatives of infective endocarditis
-staph aureus
-staph epidermis
-strept viridans (most comon)
duke criteria for diagnosis of infective endocarditis (how may of majors and minors)
-2 majors
-1 major 3 minor
-5 minor
major duke criteria of infective endocarditis
-positive blood culture
(2 positive for IE specific bacteria : HACEK/Viridans) or
(2 positive taken >12 hours apart or 3-4 positive for less specific bacteria : aureus/epidermis)
-endocardial involvement
positive echo (structure oscillation, dehiscence of prosthetic valve, abscess formation, new valvular regurgitation)
minor duke criteria of infective endocarditis
-predisposing heart condition/IV drug use
-fever > 38
-microbio evidence that dont meet major criteria
-immuno phenomena (glomerulonephritis, osler node and roth spot)
-vascular phenomena (major emboli, splenomegaly, clubbing, splinter haemorrhage, janeways lesion, petechiae/purpura
what is included in the immuno and vascular phenomena of dukes minor criteria for infective endocarditis
-immuno phenomena (glomerulonephritis, osler node and roth spot)
-vascular phenomena (major emboli, splenomegaly, clubbing, splinter haemorrhage, janeways lesion, petechiae/purpura
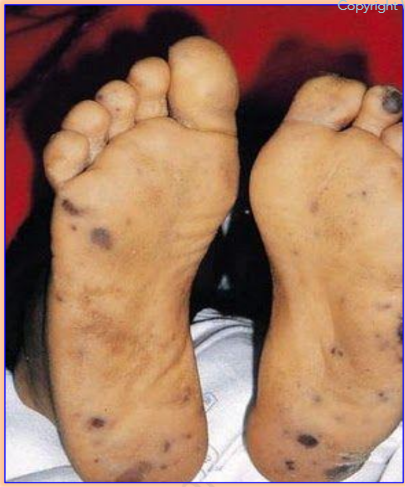
man presents with fever, confusion and petechiae. what is shown in the picture and most likely the diagnosis? how to diagnose?
janeway’s lesion (painless on soles and palms)
infective endocarditis
blood culture → echo
empirical blind therapy of infective endocarditis
natural valve
-amoxicillin + gentamycin (low dose)
-vancomycin + gentamycin (low dose)
(for sepsis, penicillin allergic and staph aureus resistence)
prosthetic valve
-vancomycin + low dose gentamycin + rifampicin
CHA2DS2VASc is used to _____________ in patient who has __________
determine the need to anticoagulants….. aFib
ABCD2 is used to identify ______________ in patients who have had ___________________
risk of future stroke… a suspected TIA in following 7 days
HAS-BLED score estimates ______________ for patients on ____________ for ____________
the risk of major bleeding… anticoagulation… aFib
DRAGON score predicts _____________ in __________ patients receiving tissue plasminogen activator (tPA) e.g. __________
3 month outcome… ischaemic stroke…. alteplase
QRISK2 score is used to determine the risk of a ______________________
cardiovascular event in the next 10 years
Patent foramen ovale (PFO) is
a hole between the left and right atria (upper chambers) of the heart. This hole exists in everyone before birth, but most often closes shortly after being born. PFO is what the hole is called when it fails to close naturally after a baby is born.
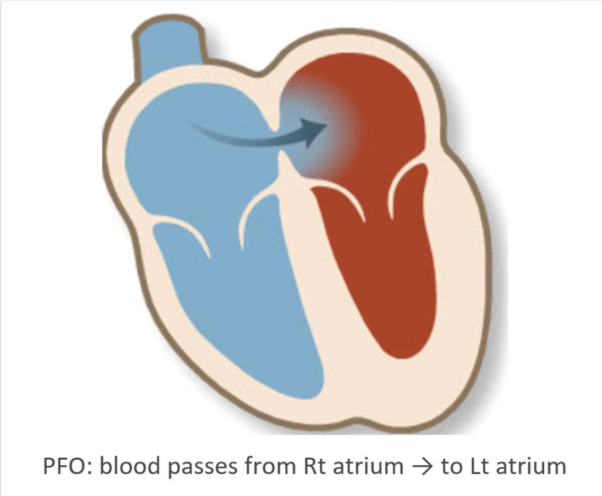
PFO could lead to
paradoxical embolism → stoke or ischemic attach
paradoxical embolism is
an embolism that travels from the venous (right) side to the arterial (left) circulation. It may lead to stroke or ischemic attack
gold standard diagnostic method of PFO
trans-esophageal echocardiography (TEO) with buble contrast
what are the important complications of MI
cardiac arrest, dressler’s syndrome, chronic heart failure, tachyarrythmia, pericarditis, left ventricular aneurysm, ventricular septal defect, acute mitral regurgitation (MR), acute tricuspid regurgitation
cardiac arrest most commonly occur due to patients developing __________ and is the most common cause of _______ following MI
patients are managed with _________
ventricular fibrillation… death
defib
management of chronic heart failure
-loop diuretics (furosemide)
-BB or ACEi
-persists, the other drug
persiste, spironolactone (AA)
if patient is on ACEi and ARB, what would be an additional med for his chronic heart failure?
BB
if patient is on it, go for spironolactone
tachyarrythmias include _________ and _________
management is __________
ventricular fibrillation and ventricular tachycardia
check the patients pulse, if no pulse → arrest protocol + defib
administer oxygen
pericarditis occurs within ________ after MI.
features are _______________________________
_____________ may develop leading to enlarged globular heart on xray
ecg shows _____________ and _____________
management : __________ and ____________
48h
pleuritic chest pain (lying + inspiration intensifies), fever, pleural pericardial rub
pericardial effusion
saddled concave upwards ST elevation and PR depression
NSAIDS 7-14 days (aspirin/ibuprofen/indomethacin) + Colchicine
dressler’s syndrome is similar to _________ in features but it tend to occur _____________ post MI.
it is an ___________ against __________ formed as myocardium recovers
features are _____________, ___ and ___
ecg shows ___________ and ____________
treated with ____________
pericarditis.. 2-6 weeks
autoimmune reaction…antigenic protein
(same as pericarditis),pericardial effusion, raised ESR
(same as pericarditis - saddled concave upward ST elevation + PR depression)
NSAIDs
left ventricular aneurysm.
the ischaemic damage sustained during a MI episode may weaken the _________ resulting in a ___________, thus _____ forms
a ____________ may form within the _______ increasing the risk of _______, so patients are prescribed with ___________
it usually occurs __________ post MI
ecg shows _________ and __________
x ray shows ______________
echo shows ______________
myocardium…thin muscular wall…aneurysm
thrombus…aneurysm…stroke…anticoagulatives
4-6 weeks
ST elevation + left ventricular failure
enlarged heart with a bulge on the left heart border
paradoxical movement of the ventricular wall
ventricular septal defect (VSD).
rupture of the ___________ occurs during ______ post MI
features are __________________
diagnostic will be __________ to exclude ________
management is ____________
interventricular septum…first week
heart failure with pan systolic murmur (best heard at the lower left sternal border), bibasilar crackles, shock (hypotension and tachycardia)
echocardiogram…acute mitral regurgitation
urgent surgical correction
acute mitral regurgitation
occur ___________ post MI (mostly _______ MI)
cause : ischemia or _______________ of mitral valve
features ___________ (typically at _______)
may present with __________, ________, __________
if with ___________ → _______, _________, ______
diagnostic is _________
treatment is ______, often require _______
2-15 days… inferior
rupture of papillary muscle
pansystolic murmur…apex
hypotension, tachycardia, pulmonary edema
pulmonary edema… SOB (dyspnea)..bi basal crackle, tachycardia
echo
vasodilators…surgical repair
acute tricuspid regurgitation.
similar to mitral but _________ is heard over ______________
pan systolic murmur… lower left sternal border
medications that reduce mortality in patients with left ventricular failure
ACEi
BB
ARBs (angiotensin receptor blockers)
AA (aldosterone antagonists - spironolacton/eplerenone)
hydralazine with nitrates