Mitral Regurgitation (MR)
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
What is MR?
Backflow of blood into the LA during systole.
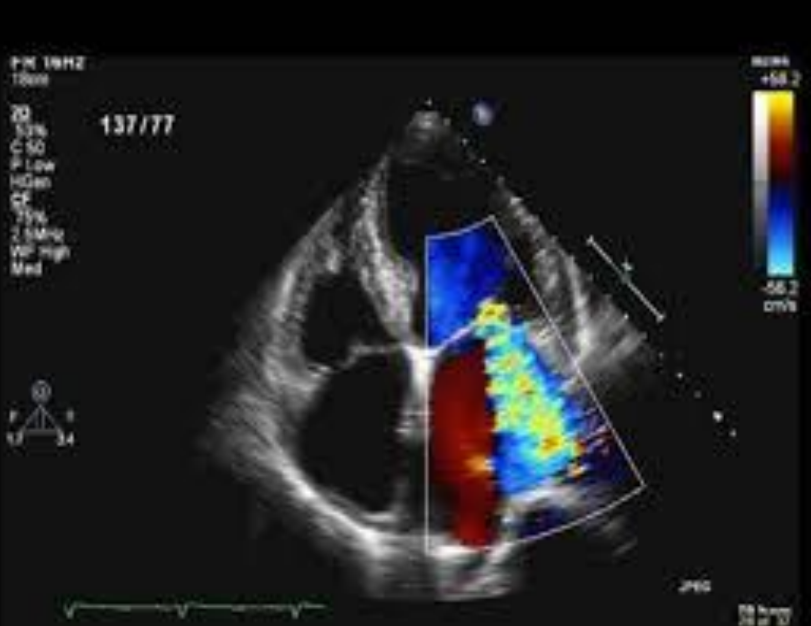
This picture indicates what?
Severe MR - blue in the LV and LA indicates that there is leaking. Blood should be all red in the LA.
What are the possible causes of MR? (3)
Eversion or damaged cusps
Rupture of papillary muscles following an infarct (heart attack)
Rupture of chordae tendineae due to rheumatic heart disease or bacterial endocarditis, thus causing valves to not close properly.
Does majority of the population have a little like in their MV?
Yes.
What are some other possible causes for MR? (8)
LV dysfunction
Mitral annular calcification (MAC)
Flail MV leaflets
Vegetation
Prosthetic valve dysfunction
Congenital anomalies (ie cleft MV)
Idiopathic hypertrophic subaortic stenosis (IHSS)
MVP (Mitral valve prolapse)
What is MVP?
Mitral valve prolapse, when the valves flop back into the left atrium.
What are some symptoms of MR in a patient? (6)
Palpitations
Dysrhythmias
Fatigue
Dyspnea-difficulty breathing SOB (shortness of breath)
Orthopnea (positional SOB - usually cannot lie flat due to breathing issues)
Holosystolic/pansystolic murmur
What are two types of MR that may not produce any symptoms for years?
Chronic MR or moderate MR.
What is a classic symptom of MR?
Holosystolic or pansystolic murmur.
What is holosystolic murmur?
Murmur throughout systole.
What is pansystolic murmur?
Murmur either at the end or beginning of systole (not throughout systole).
If there is an acute issue with the mitral valve, what happens to the heart?
It will not be able to adjust to the new change in blood volume.
What are the four major physiologic changes due to MR?
Dilatation of LA
Increased LA pressure
Dilatation of LV - LVVO
Hyperdynamic LV
Why does the LA dilate when there is MR?
Because blood seeps back into the LA, thus increasing the volume of blood which forces the LA to grow to take on the increased volume.
What is a subeffect of LA dilation due to MR?
Increased LA pressure because there is more blood inside of the LA.
What happens the the LV due to MR?
Dilatation. This occurs because the LA dilates due to blood flow back into the LA. This increases the amount of blood being pushed into the LV during systole and thus causes LV volume overload (LVVO).
When there is LV dilation, this causes what? (Think Starlings Law)
More volume in the LV causes dilation, which causes more stretch, and thus more squeeze.
What is a hyperdynamic LV?
When the EF is less than 55% - ASE (or 60%). If this reaches 30-40%, the patient will need a MV replacement.
What are some other physiologic changes that can be caused by MR? (2)
Pulmonary congestion and edema
Pulmonary hypertension (high pressure in the right heart) This is due to an enlarged right heart.
Why can an enlarged heart occur with MR?
Because blood can leak back into the LA from the LV, and then into the PV, RV, and RA.
What are five complications due to MR?
Arrythmia
Pulmonary edema (fluid accumulation in the lungs)
Pulmonary hypertension (higher pressure in the lungs)
LA thrombus formation and embolization
Heart failure (when EF gets smaller and smaller)
Anything that increases LA size can cause arrythmia. This includes what two things?
Atrial flutter
Atrial fibrillation
When someone has acute MR, how many hours go by until they are most likely entering an emergency room?
2 - 4 hours.
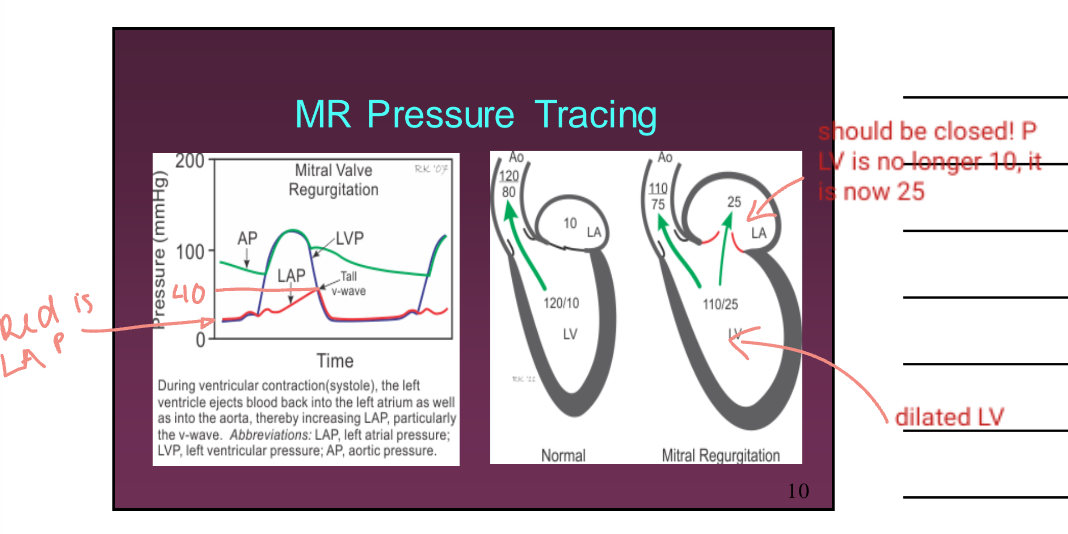
A pressure recording of MR in the cath lab reveals what?
An elevated V wave in the LA/pulmonary capillary wedge pressure tracing.
With acute MR, does the LA have time to compensate for the additional flow?
No. This causes increase LA pressure (and increased LA pressure waveform).
Describe chronic MR.
The LA has time to compensate for the additional flow by dilating. Therefore this prevents LA pressure from increasing. The LA dilated is beneficial for this circumstance as the heart “fixes” itself for the meantime. However, over time this will become problematic.
What are some treatments for MR? (2)
Valve repair or replacement (tissue valve or mechanical man-made valve)
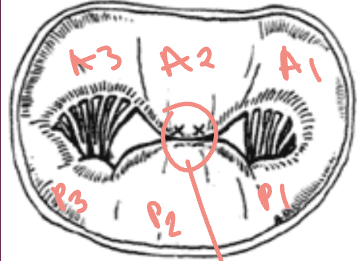
Alfieri stitch-suture placed between A2 and P2 segments. However this can lead to a degree of MS (mitral stenosis).
What are some NON SPECIFIC echocardiography 2-D findings when there is MR? (4)
LA and LV enlargement
LVVO hyperdynamic LV
Incomplete MV leaflet coaptation (when closed there is still an opening for blood to leak back into the LA)
MAC (mitral annulus calcification)
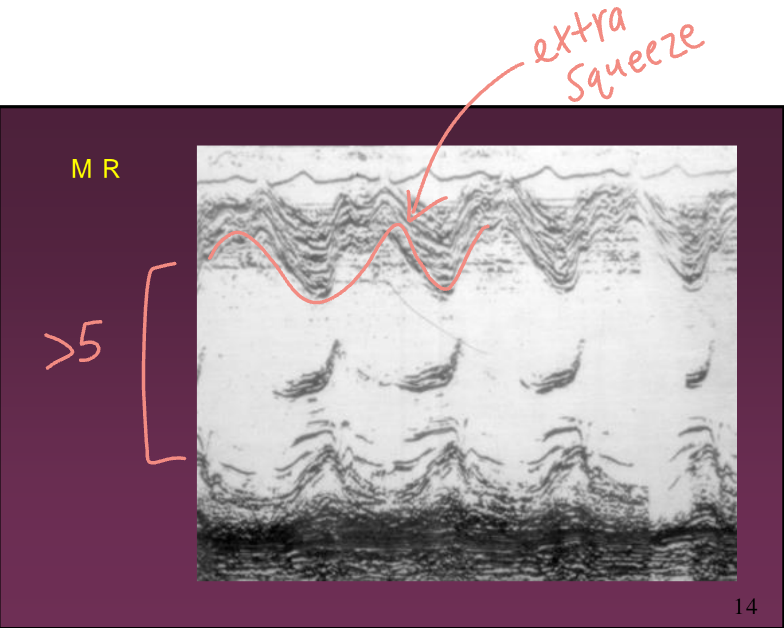
What are some NON SPECIFIC M-Mode findings when there is MR?
Dilated LA and LV (LV bigger than 5 cm)
LVVO hyperdynamic LV
Increased MV amplitude (D-E excursion) - related to increased volume
Early mid systolic closure of the aortic valve
RV enlargement
What is the method of choice for detection and quantification of MR?
Doppler.
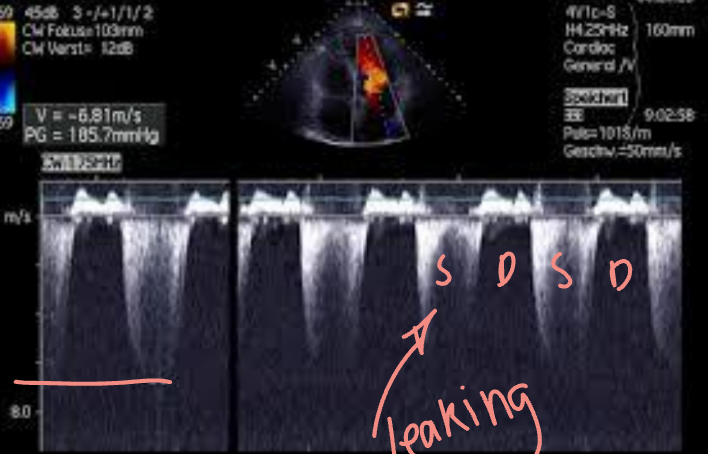
When using continuous wave Doppler, it is important to ensure what it done?
That the transducer is parallel to blood flow.
To assess MR with CW Doppler, where is the cursor placed?
Within the peak of the MR jet.
MR peak velocity reaches around what?
4-6 m/s
A decreased MR peak velocity less than 4 m/s indicates what?
Elevated LA pressure due to severe MR.
What is the calculation for LA pressure due to severe MR?
LA pressure (LAP) = systolic BP - MR gradient
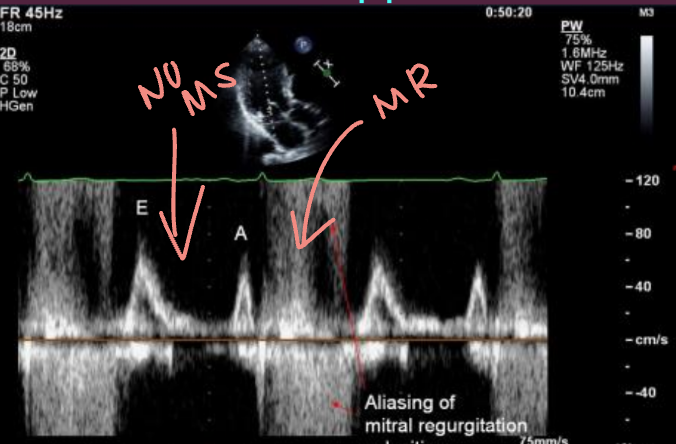
How is pulsed wave Doppler presented when MR is present?
Normal flow in diastole but negative flow occurs in systole (there should be nothing here).
Where is the sample volume situated for PW Doppler in MR?
Behind the MV in the LA.
In MR, aliasing might occur in what versions of Doppler?
PW and Colour Flow Doppler.
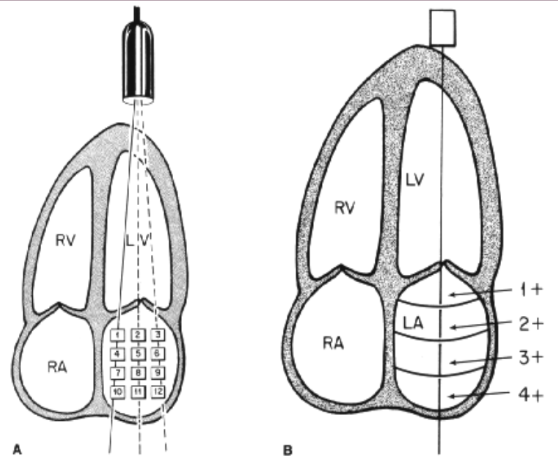
How is PW Doppler performed on MR?
Systematically moving the sample volume through the LA to determine the depth and width of the MR jet. (Out of date but can be useful if colour Doppler signal is suboptimal).
Although PW mapping of MR is out of date, what are the 4 grades to indicate the severity of MR? (This is also the same with Colour Doppler)
Grade 1 - mild (with leaking just beyond the mitral valve leaflets)
Grade 2 - moderate (leaking in the proximal 1/3 way into LA)
Grade 3 - mod/severe (leaking halfway into LA)
Grade 4 - severe (leaking to the backwall of the LA all the way into the pulmonary vein(s))
True or False: Only use PW Doppler when Colour Doppler of MR is inadequate.
True.
With colour Doppler, red indicates what? Blue indicates what? (In terms of MR)
Red in the A4 view indicated normal flow. Blue jet in systole because of leaking.
Colour Doppler of the MV allows what in terms of MR?
Makes it easier to detect/quantify. It is also easier and quicker.
What five views can be used alongside Colour Doppler to indicate MR?
LAX (shows the abnormal systolic MR jet)
SAX (allows visualisation of MR jet origin and width)
Apical 4 (shows the abnormal systolic MR jet travelling away from the transducer)
Apical 2 (shows the abnormal systolic MR jet travelling away from the transducer)
Apical Long/3 chamber (shoes the abnormal systolic MR jet travelling away from the transducer)
What three views are the best for assessing MR using Colour Doppler?
A4
A2
A Long / A3
Pictrue showing parasternal LAX and A4 MR.
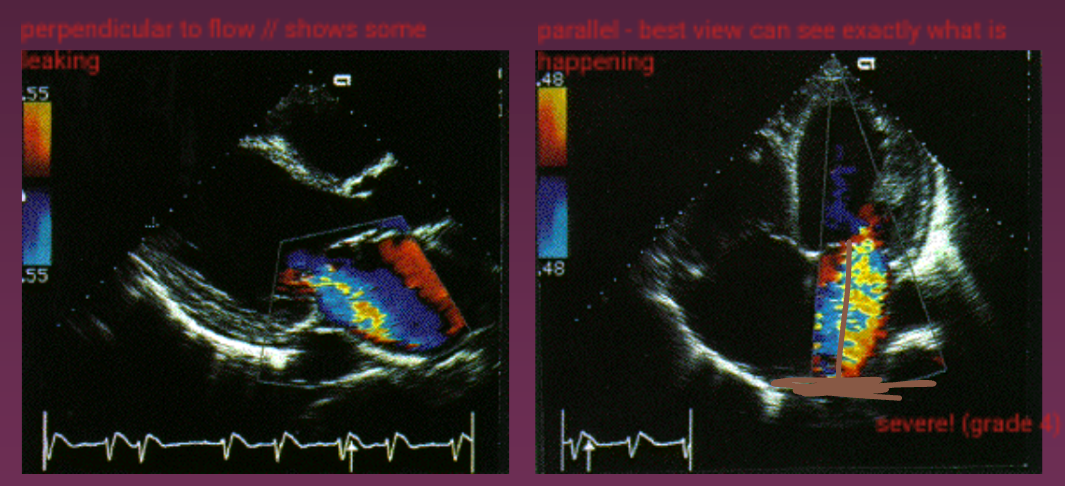
The ASE has set certain standards for quantitating the degree of MR. Describe them. (4)
Grade 1 - Mild (MR jet extends just beyond the leaflets of the MV)
Grade 2 - Moderate (MR just in proximal 1/3 way into the LA)
Grade 3 - Mod/Severe (MR jet halfway into the LA)
Grade 4 - Severe (MR jet to mid to back wall of the LA)
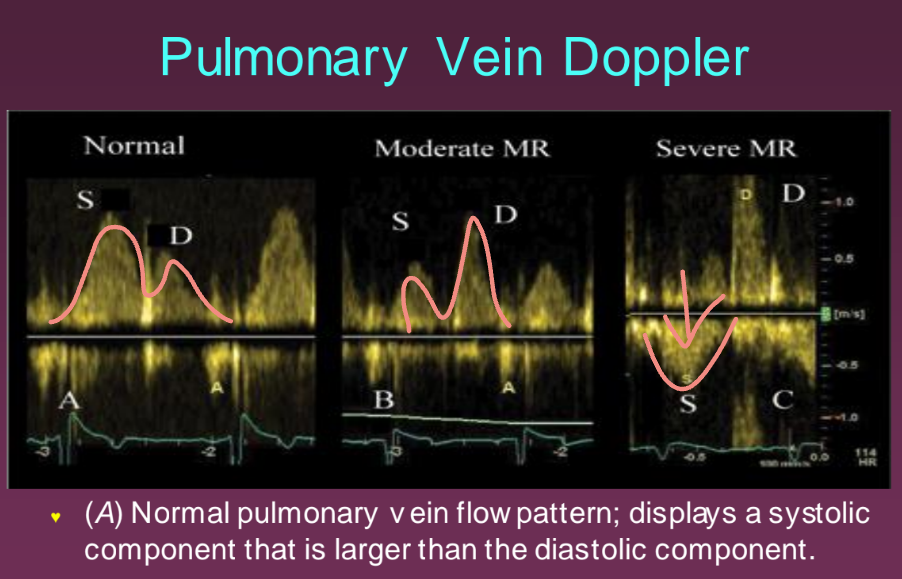
How is pulmonary vein Doppler performed and why?
Using PW Doppler by placing the PW sample volume approx. 1 cm into the RUPV from the A4 or A5 view. This is done when there is grade 4 MR to see how far back the leaking is occurring. This is an additional picture that must be taken per protocol in a case of grade 4 MR.
What is the vena contracta width?
The area of the jet as it leaves the regurgitant orifice and reflects the regurgitant orifice area. (Narrowest area near the mitral annulus).
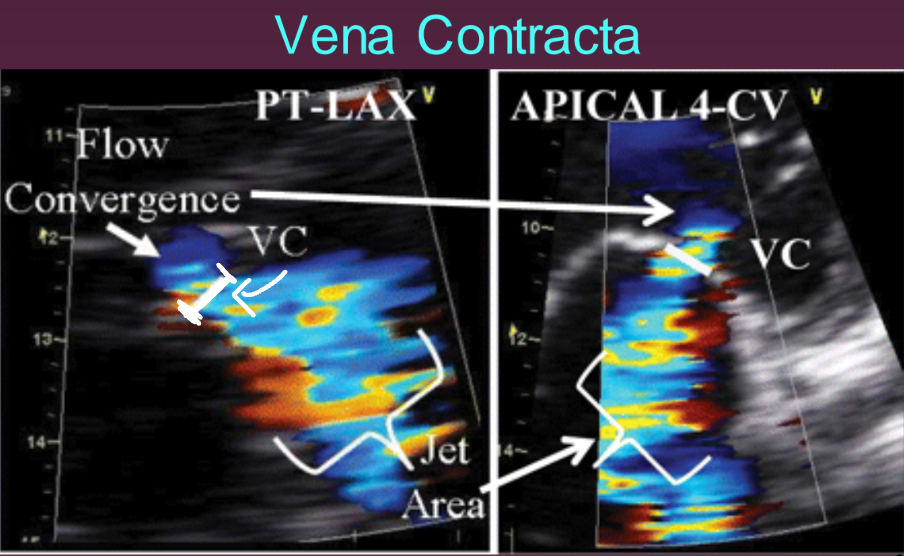
When measuring the vena contracta width, what are three important factors to follow?
Adjusting the Nyquist linit to 40-70 cm/s to identify the neck of the MR jet
Zoom or magnify the area
Average measurements over 2-3 beats
A vena contracta with a width of < 3 mm indicates what?
Mild MR.
A vena contracta of > 7 mm indicates what?
Severe MR.
Are intermediate values of the vena contracta (ie. 4-7 mm) accurate at distinguishing MR?
No, they are not, hence there is only mild or severe.
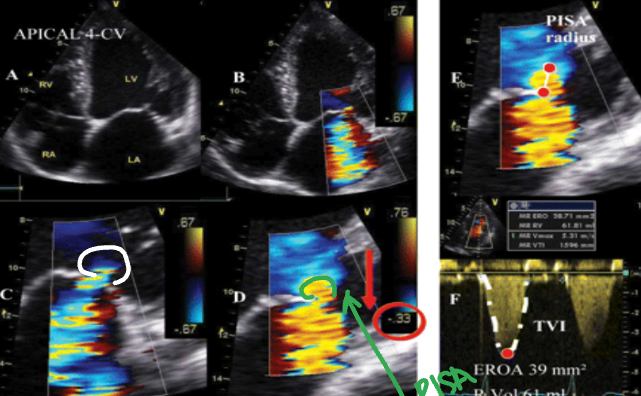
What is PISA?
Proximal Isovelocity Surface Area index.
PISA is also known as what?
The flow convergence method.
What does PISA do?
It estimates the area of an orifice through which blood flows through using Colour Doppler.
With MR, what does PISA do?
It determines the effective regurgitant orifice and regurgitant volume.
In what view is PISA of MV (for MR) is done?
In A4.
PISA helps us do what? Where is it measured?
Determine how severe the leaking is. It is measured on top of the vena contracta.
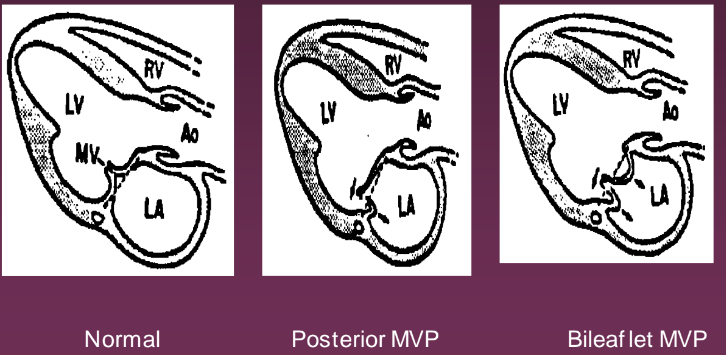
What is mitral valve prolapse (MVP)?
Posterior displacement of the AMVL and/or the PMVL towards the LA in systole.
What are four other names used to describe MVP?
Barlow Syndrome
Floppy Valve Syndrome
Systolic Murmur Click Syndrome
Ballooning Mitral Valve
Is there an exact cause to MVP?
No. (Unknown as of right now).
What are some possible causes of MVP? (3)
Hereditary factor (ie. autosomal dominant)
Seems to be prevelent in women < 40 years of age
May be due to myxomatous degeneration (weakening of the connective tissue)
Can MVP cause MR?
Some MVP are progressive, thus leading to severe MR, however there are others that seems to have a more benign, long term outcome.
Can MVP be an isolated finding (meaning no other pathology is present)?
Yes.
What are some pathologies that MVP can be associated with?
Connective tissue disorders - Marfan Syndrome, Lupus , and Ehler’s Danlos.
What are some heart abnormalities that can be associated with MVP? (5)
Patent ductus arteriosus (PDA)
Atrial septal defect (ASD)
Myocarditis
Ebstein Anomaly
Wolff-Parkinson-White (WPW) Syndrome
What are some skeletal abnormalities associated with MVP? (4)
Pectus excavatum
Pectus carinatum
Straight back
Scoliosis (snake spine)
If a person has MVP, should there be an assessment of the other valves?
Yes, because there might also be prolapse in the other valves, like TVP and AVP.
What are the histology changes when one has MVP?
The leaftlets of the MV are more thicker (myxomatous) and there is weakening of the connective tissue. The valves can also appear redundant or floppy.
What does myxomatous mean?
Tumor like changes (clumping).
What are the symptoms of MVP? (12)
Asymptomatic
Palpitations
Chest pain
Dyspnea
Fatigue
Dizziness/syncope
Arrythmias
Progressive MR
Increased risk of endocarditis
Ruptured chordae or papillary muscles
Embolic event (stroke - blood clot)
Sudden death (rare)
What does the auscultation of MVP sound like?
Mid-late systolic click for light leaks, and pansystolic/holosystolic sounds in heavy leaks. It is important to auscultate in many positions so assess when it is more prevalent. For example, standing will reduce the LV volume and enhance the murmur.
What are the treatments for minor MVP?
None.
What are the treatments for MVP that is moderate or severe?
Prophylaxis antibiotics (used pre dental or GI surgery to prevent possible bacteria infection of the heart)
Follow ups (especially if they have MVP and MR together, this helps to track the progress of the pathology)
Mitral valve repair or replacement in severe cases
What are the 2-D findings of MVP?
Any portion of the AMVL or PMVL leaflets prolapse beyond an imaginary line drawn from the post aortic wall to the AV groove (MV annulus) into LA during systole
Myxomatous (AKA redundant) appearance to the MV leaflets
True or False: MVP must be looked at in all views.
True.
What is the best view for assessing MVP?
Parasternal LAX.
What is the LEAST best view for assessing MVP?
Apical 4.
Tips of the MV should always point in what direction?
South (This is because chordae tendinae helps to keep it in that direction).
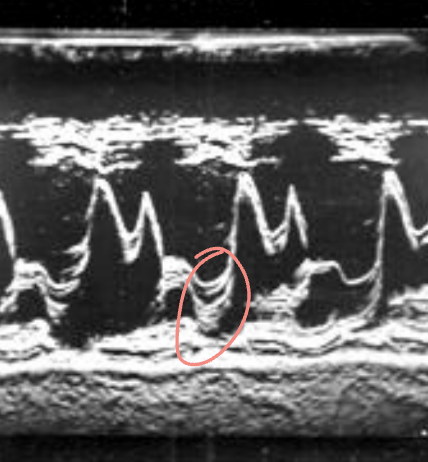
What are some M-Mode findings when there is MVP?
MVL dropping 2 mm or more below the C-D line, at mid to late systole (pansystolic)
MVL dropping 3 mm or more below the C-D line throughout systole (holosystolic)
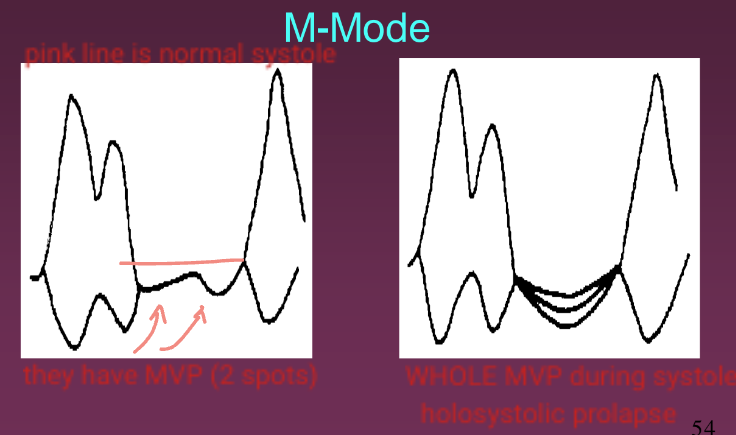
Picture of MVP in late systole.
In Colour Doppler, if the AMVL prolapses, what kind of MR jet will there be?
A posteriorly directed MR jet.
In Colour Doppler, if the PMVL proplases, what kind of MR jet will there be?
Anteriorly directed MR jet.
If both the AMVL and PMVL are prolapsing, using Colour Doppler, what MR jet will be present?
A central MR jet.
What are some enhancing/exaggerating maneuvers that can be done to enhance MVP? (3)
Valsalva (bear down)
Amyl nitrate (a drug that will increase heart rate, therefore decreasing LV filling/volume, allowing MVP to stand out)
Standing
Conversly, what are some maneuvers that can make MVP less obvious? (3)
Squatting
Propranolol (decreasing heart rate)
Bradycardia (decrease in heart rate, typically < 60 bpm)
What is pseudoprolapse?
When improper transducer placement (too high or too low on chest) presents prolapse but there is no prolapse. A large pericardial effusion may also create a false positive MVP (suggested to repeat once effusion is gone).
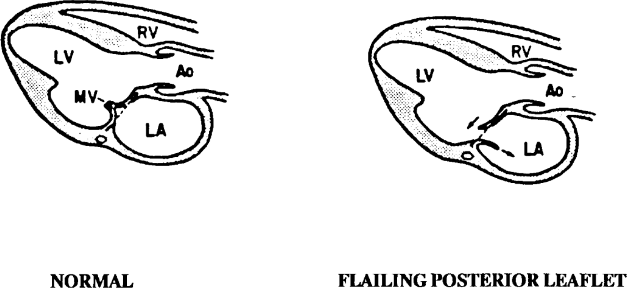
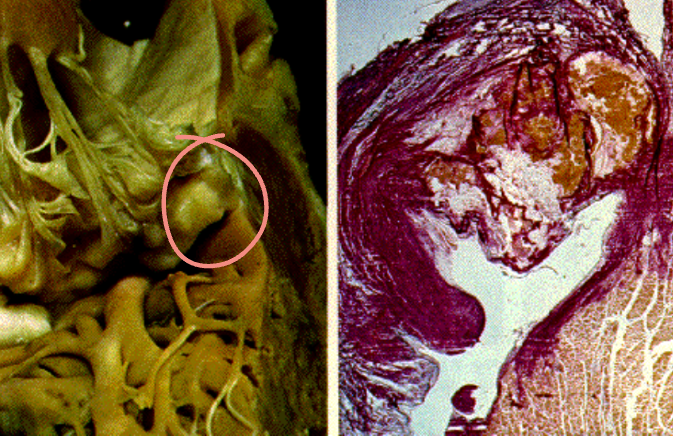
What are the two causes of a flail mitral valve?
Ruptured chordae
Ruptured papillary muscles
(Infection like bacterial endocarditis and heart attack can also cause a flail mitral valve)
What leaflet is most commonly affected in a flail mitral valve?
PMVL
What is the patient presentation when they have a flail mitral valve?
Sudden onset of heart failure (due to heart failure)
Pulmonary edema (fluid/swelling in the lungs)
A flail mitral valve is best detected in what view?
Parasternal LAX.
What does a flail mitral valve look like?
Tip of the MVL points into the LA in systole and in LV in diastole. There is also coarse disorganized flutter of the flail leaflet throughout systole and diastole.
If severe MR is associated with flail MV, what does this look like?
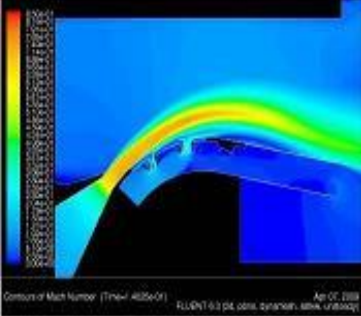
Although we know severe MR goes all the way to the back wall, in a flail MV the jet will only be directed in such a way as the “hug” the valve leaflet and LA wall. In this case, that’s why the MR jet appears smaller with Colour Doppler (known as the coanda effect).
What is the coanda effect?
A phenomena where the jet flows attaches itself to a nearby surface and remains attached even when the surface curves away from the initial jet direction. In free surroundings, a jet of fluid entrains and mixes with its surrounding as it flows away from a nozzle.
What is MAC?
Mitral annulus calcification.
Is MAC a young peoples disease or an old peoples disease?
Old peoples disease.
Where does MAC begin?
Near the MV ring and can extend to the leaflets.
What portion of the MV is most affected by MAC?
The posterior portion most commonly affected.
What percentage of people with MAC have MR?
50%