Major Depressive Disorder
1/254
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
255 Terms
Course of MDD
- single episode
- recurrent episodes
*patients with residual symptoms are more likely to suffer from future depressive episodes
Chance of developing a recurrent episode of MDD
- 60% of patients with a single episode will develop a 2nd episode
- patients with a 2nd episode have 70% chance of developing a 3rd episode
- patients with a 3rd episode have a 90% chance of developing a 4th episode
Etiology of MDD
- exact etiology unknown
- most likely multifactorial (genetic + environmental contribute to functional and structural changes)
What do neuroimaging studies show in the brain with MDD?
- decrease in serotonin transporters
- altered post-synaptic serotonin receptor binding
- small hippocampus
What are the two major hypothesis with depression?
- biogenic amine hypothesis
- hyperactive HPA
Biogenic amine hypothesis
- experimentally induced deficiency of 5HT, NE and DA --> depressive symptoms (not consistently)
Hyperactive HPA (hypothalamic-pituitary-adrenal axis)
- 1/3 to 2/3 of patients display hyperactivity of this axis
- increased serum cortisol levels
- hippocampal atrophy after exposure to stress and elevated glucocorticoids --> decreased BDNF expression
* effectiveness of antidepressants may actually be the result of their ability to promote neuronal growth (increase BDNF) in the hippocampus through remodeling neurons
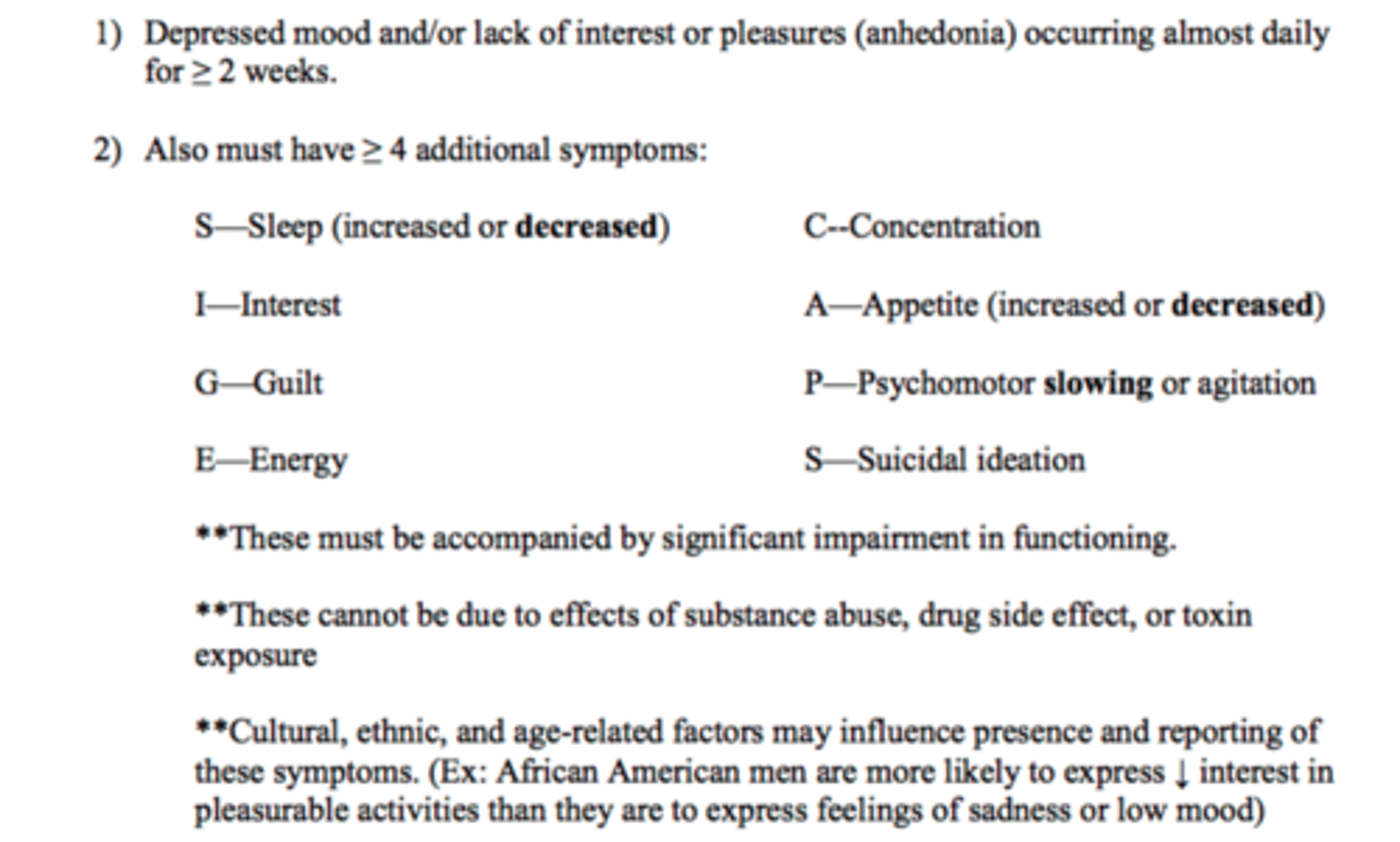
Diagnosis of MDD
down mood for >/= 2 weeks + >/= 4 sigecaps + signifiant impairment of activity
How long must a patient be off substances to be considered diagnosable depression?
drug free for >1 month
What is persistent depressive disorder?
- depressed mood present more days than not for at least 2 years (+2 SIGECAPS symptoms- excluding suicidality)
What are common scales that are used for diagnosis and monitoring of depressive symptoms?
- PHQ-9 (ambulatory setting)
- HAM-D score (research setting)
- MARDS (research setting)
- Columbia Suicidal Scale
What are the score categories of the PHQ-9?
- 0-4= minimal (remission)
- 5-9= depression
- 10-14= moderate
- 15-19= moderately severe
- 20-27= severe
What is the goal of depression treatment in regards to the PHQ-9 scale?
score <5 (remission)
What is the gold standard diagnosis of depression?
structured clinical interview (done by specialists)
In primary care settings, what PHQ-9 score indicates a diagnosis of depression?
>/= 10 (not gold standard)
What is considered to be a clinically significant in regards to PHQ-9 score?
3 points or more
If suicidality lasts longer than 2 years, what does this indicate?
personality disorder
K.L. is a 33-year-old male who presents to the clinic complaining of inability to sleep. He reports that he has not been able to sleep more than 4 hours a night for the past 3 weeks. He denies any change in his energy level, but states that he isn’t interested in doing much of anything. He reports that he has not been attending his book club for the past month because he says it’s just not fun anymore and has been struggling to complete projects at work because he just doesn’t care. He reports an unintentional 10 pound weight gain and it is noted that there is some delay in his response to questions. He denies excessive guilt, difficulty with concentration, and states “yeah, I’ve thought about killing myself, but I don’t think I’d ever really do it.” His PHQ-9 score is 17.
Does K.L. meet criteria for diagnosis of major depressive disorder? Why or why not?
yes
- lack of interest/pleasure for one month (>2 weeks)
- trouble sleeping, difficulty concentrating, suicidal ideation, delay in response
- want to make sure that this is not due to any substance abuse/medication side effect, ask questions about sleep and weight changes
What is the average age of onset of depression?
32 years old, but can manifest at any age
What are triggering factors of depression?
- death of a loved one
- divorce
- chronic medical conditions
- endocrine disorders (Cushing, addisons, hypothyroidism)
What are the 7 classes of antidepressants?
- SSRI
- TCAs
- neuroactive steroids
- SNRI
- second generation
- MAOI
- ketamine
What are examples of SSRIs?
- fluoxetine (Prozac)
- paroxetine (Paxil)
- sertraline (Zoloft)
- citalopram (Celexa)
- escitalopram (Lexapro)
- fluvoxamine (Luvox)
What are examples of TCAs?
- amitriptyline (Elavil)
- nortriptyline (pamelor, Aventyl)
- imipramine (Tofranil)
- desipramine (Norpramin)
- clomipramine (Anafranil)
What are examples of neuroactive steroids?
- bexanolone (Zulresso)
What are examples of SNRIs?
- venlafaxine (Effexor)
- duloxetine (cymbalta)
- desvenlafaxine (pristiq)
- levomilnacipram (Fetzima)
What are examples of second generation antidepressants?
- bupropion (Wellbutrin)
- mirtazapine (remeron)
- nefazodone (Serzone)
- vilazodone (Viibryd)
- trazodone (Desyrel, Oleptro)
- Vortioxetine (trintellix)
What are examples of MAOIs?
- phenelzine (Nardil)
- tranylcypromine (Parnate)
- selegiline (Emsam transdermal)
What are examples of ketamine analogs?
Esketamine (spravato)
What are the 3 phases of of antidepressant treatment?
- acute phase
- continuation phase
- maintenance phase
Acute phase
All AD's require a minimum of a 4 week trial (preferably 8 weeks) at adequate doses
What is the minimum trial that all ADs require?
4 weeks
If a patient has some improvement in symptoms at 4 weeks, what should be done?
Give it another 4 weeks to see if there is more improvement and increase dose if tolerating well
If a patient has zero improvement or worsening symptoms at 4 weeks, what should be done?
Change the drug
Symptoms of depression may improve out to ____________ when starting an antidepressant
12 weeks
Continuation phase
Therapeutic drug dose is continued for at least 6 months after symptoms have resolved (PHQ-9 <5)
What should be done before stopping a patient's antidepressant after the continuation phase is complete?
Put into context the patient's current situation (dog died, loss of a job, etc. is probably not a good time to stop)
Maintenance phase
Antidepressant 2 years or longer after symptom resolved (PHQ-9 <5) for recurrent/chronic depression
Who are candidates for maintenance therapy?
- 3 or more episodes of major depression
- 2 or more episodes + >/= 1 of the following: family history of mood disorders, residual symptoms age <40 at first onset of symptoms, severe episodes, ongoing psychosocial stressors
Dosing of the maintenance regimen
Same dose/drug but dose adjustments may be needed over time
For a first depressive episode, about how long will patients be on AD therapy?
Taking into account the acute and continuation phase, about 1 year
Response
At least 50% reduction in symptoms
_________% of patients will still have residual symptoms that interfere with work, family, and social activities despite AD response.
50%
Remission
Complete resolution of symptoms (PHQ-9 <5)
*this is the goal of treatment!!
What does there achievement of remission confer?
Lower risk of experiencing future depressive episodes
Relapse
Return of symptoms AFTER a period of remission
If a patient has lingering symptoms of depression, what are they at a higher risk of?
Relapse
What are the predictors of response to AD's?
- absence of neurovegetative symptoms
- past response
- familial response
- patient adherence with visits and meds
___________% of patients do NOT receive at least a ________ drug dose for an _________ time period
40%, moderate, adequate
What is information you should tell you patients to improve adherence to ADs?
- this medication works best if taken everyday
- this medication may take 2-4 weeks to show an effect and may take up to 8 weeks to have its full effect
- do not stop taking this medication without first discussing it with your doctor, even if you start to feel better
- it is highly recommended you take this medication for at least 6 months
- if you have any specific questions about this medication, call your doctor or pharmacist
AD's may take up to how long to show an effect?
2-4 weeks (may take up to 8 weeks to see full effect)
How long is it recommended you take AD's for?
At least 6 months
What is the process to see if anything should be changed on an antidepressant regimen?
1. See how long the patient has been on it (at least 4 weeks)
2. See if the patient is tolerating it
3. If only a partial response and tolerating well, increase dose
What are the three general treatment principles with all antidepressants?
1. Discontinuation/withdrawal syndrome
2. Suicidality
3. Serotonin syndrome
What are examples of AD withdrawal symptoms?
- vivid dreams
- nightmares
- tremor
- dizziness
- headache
- electric shock sensations (zing/zap)
- nausea
Will withdrawal symptoms go away on their own?
Yes
How long will it take withdrawal symptoms last?
Depends on how long the 1/2 life is
- short half life: more abrupt withdrawal, shorter
- long 1/2 life: slow onset, longer
How to discontinue antidepressants? What is the exception to this rule?
- abrupt d/c is NOT recommended (taper over >/= 7-10 days)
- fluoxetine is the exception due to its long 1/2 life (1 week)
What dose is the worst to taper off of?
The smallest dose
What can be used if a patient is having severe withdrawal symptoms?
Add fluoxetine to help bridge
What is the boxed warning on all antidepressants?
Increased risk of suicidality in children, adolescents may and adults up to age 25
When is the risk of suicidality with antidepressants?
Occurs within the 1st month of treatment
- after the 1st month, it is more protective to be on an antidepressant
What is the risk:benefit ratio of the suicidality risk of antidepressants?
Overall, untreated depression probably has a greater risk of suicide than dose treatment with an antidepressant
If a patient on an AD experiences suicidal thoughts within the 1st month of treatment, what should be done?
If the patient can be kept in a stable and safe environment, often keep on the same antidepressant to avoid experiencing again
Risk of serotonin syndrome
- present with any agent that increases serotonin levels
- risk increases when combined with another agent that increases serotonin levels
Why does serotonin syndrome occur?
High concentration of 5HT at 5HT-2 receptors
Is serotonin syndrome common if a patient is on 1-2 serotonergic drugs?
No (only a very small number of patients with experience)
What are the symptoms that a patient can experience with serotonin syndrome?
1. Neuromuscular: hyperreflexia, clonus, myoclonus, shivering, tremor, hypertonic/rigidity
2. Autonomic: hyperthermia (>105 F), tachycardia, diaphoresis, flushing, mydriasis
3. Mental state changes: Agitation, hypomania, anxiety, confusion
What are counseling points to tell a patient about serotonin syndrome?
- this is an emergency situation and needs to be treated right away
- if you wonder you have serotonin syndrome, you do not have it
- it will be obvious to the people around you
What is tricyclic antidepressants (TCAs) current use?
- at least 3rd line agent
- unless patient has comorbid migraine prevention, pain, or need to monitor blood serum levels
MOA TCA
- block reuptake of NE and 5HT
- also blocks histamine, acetylcholine, and alpha-adrenergic receptors
Dosing considerations with TCAs
- large inter patient Pk variability
- serum levels play a large role in determining dose
What are the advantages of TCAs vs other antidepressants?
- inexpensive
- long track record
- plasma levels are useful in monitoring
- also useful in treating pain, anxiety, insomnia, and prophylaxis of migraine
What are the disadvantages of TCAs?
- anticholinergic side effects
- CV side effects
- common serotonin side effects like the SSRIs
- lower the seizure threshold
- switch to mania in 10% of patients
- severe or fatal arrhythmias may result from overdose
- significant potential for drug interactions
What are examples of anticholinergic side effects that are seen with TCAs?
- dry mouth
- blurred vision
- urinary retention
- constipation
- central effects (delirium, agitation, delusions, hallucinations, restlessness)
What are the TCAs that are less cholinergic?
Desipramine and nortriptyline
Who should avoid use of TCAs?
- elderly patients
- patients with underlying cardiac disease (esp. frank bundle-branch disease or complete heart block)
What are the CV side effects that are seen with TCAs?
- orthostatic hypotension (esp. a problem with the elderly)
- tachycardia
- prolonged conduction
Why should you use caution with the use of TCAs in suicidal patients?
- fatal arrhythmia if >7-10 day supply ingested at one time
What are examples of safeguards to use in patients with a previous suicidal history on TCAs?
- only give the patient a 7 day supply
- have someone else store the medications
What are the pharmacokinetic interactions with TCAs?
- metabolized by CYP2D6
- TCA plasma concentrations increased by inhibitors like fluoxetine and paroxetine
- TCA plasma concentrations decreased by inducers like phenytoin
What are the pharmacodynamic interactions with TCAs?
- excessive sedation
- additive anticholinergic effects
What is the MOA of SSRIs?
- inhibit reuptake of 5HT in the synapse
- very little affinity for histaminic, cholinergic, or adrenergic receptors
What does the 5-HT1A receptor provide with SSRIs?
Antidepressant action
What does the 5HT-2 receptor provide with SSRIs?
Sexual dysfunction
What does the 5HT-3 receptor provide with SSRIs?
GI side effects
What is the current treatment of choice for MDD?
- SSRI (try 2 SSRIs before moving out of this class)
What are the advantages of SSRIs over TCAs?
- not lethal in overdose
- less sedating
- less weight gain
- not associated with cardiac conduction changes, orthostatic HOTN, or urinary retention (much less anticholinergic)
What are examples of other comorbidities that SSRIs can treat?
- GAD
- social phobia
- OCD
- bulimia
- PMDD
- PTSD
Should you monitor serum levels with SSRIs?
- no
- serum concentrations are NOT related to clinical outcomes
How often are SSRIs dosed?
Once daily (AM or PM depending on the sedating effects in the individual)
What are the three general types of serotonin side effects?
1. Early onset
2. Late onset
3. Time independent
What are the characteristics of the early onset serotonin side effects?
- come on 24-48 hours after starting medication
- last 1-2 weeks
- will go away on their own
What are the early onset serotonin side effects?
1. Nausea
2. Anxiety and agitation
3. Sleep changes
What is the worse SSRI for nausea?
Sertraline (tolerance develops in 1-2 weeks)
What is the worse SSRI for anxiety and agitation?
Fluoxetine and sertraline
What is the SSRI that tends to cause insomnia?
Fluoxetine
What is the SSRI that tends to cause sedation?
Paroxetine
In general, when should most SSRIs be given during the day? What is the exception?
- take in AM
- Paroxetine taken in the PM
- but adjust based on your own response (do not fluctuate on a daily basis, try one week and if having issues then switch to a different time)
Why do we start low and go slow with antidepressants in the outpatient setting?
early onset serotonin side effects
- in inpatient setting, you can increase faster if you know patient is tolerating well
What are characteristics of late onset serotonin symptoms?
- occurs after about 3 months
- symptoms persist