PSYC 304 - Midterm 2
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
129 Terms
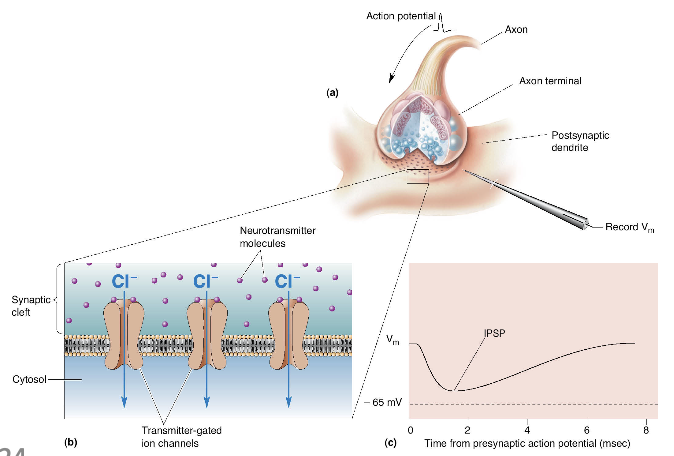
what happens when a neurotransmitter molecule binds to a poststynaptic receptor?
Depolarization of the membrane (excitatory postsynaptic potential) - decrease membrane potential from -70 to -67 mV
Hyperpolarize the membrane (inhibitory postsynaptic potential) -increase membrane potential from -70 to -72 mV
excitatory postsynaptic potential
increase likelihood that postsynaptic neuron will fire an action potential (change of voltage on dendrites) when binding to a receptor
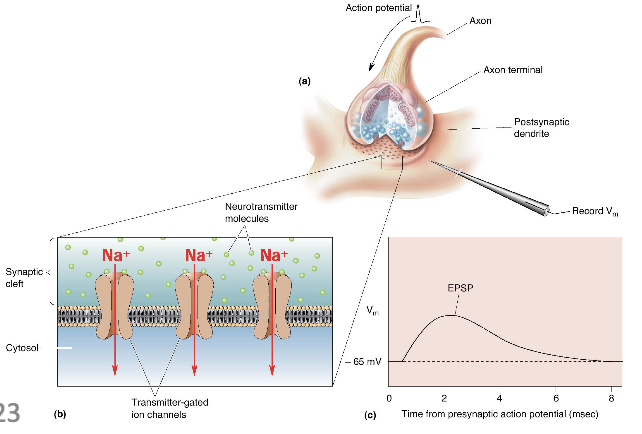
inhibitory postsynaptic potential
decrease likelihood that the postsynaptic neuron will fire an AP
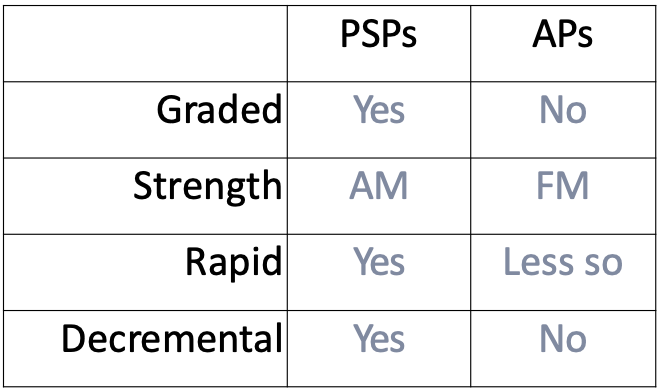
how is the transmission of postsynaptic potentials (PSPs)?
graded: different sizes
rapid: travels fast
decremental: further you get, weaker it becomes
larger the potential, the more neurotransmitters binding to more receptors
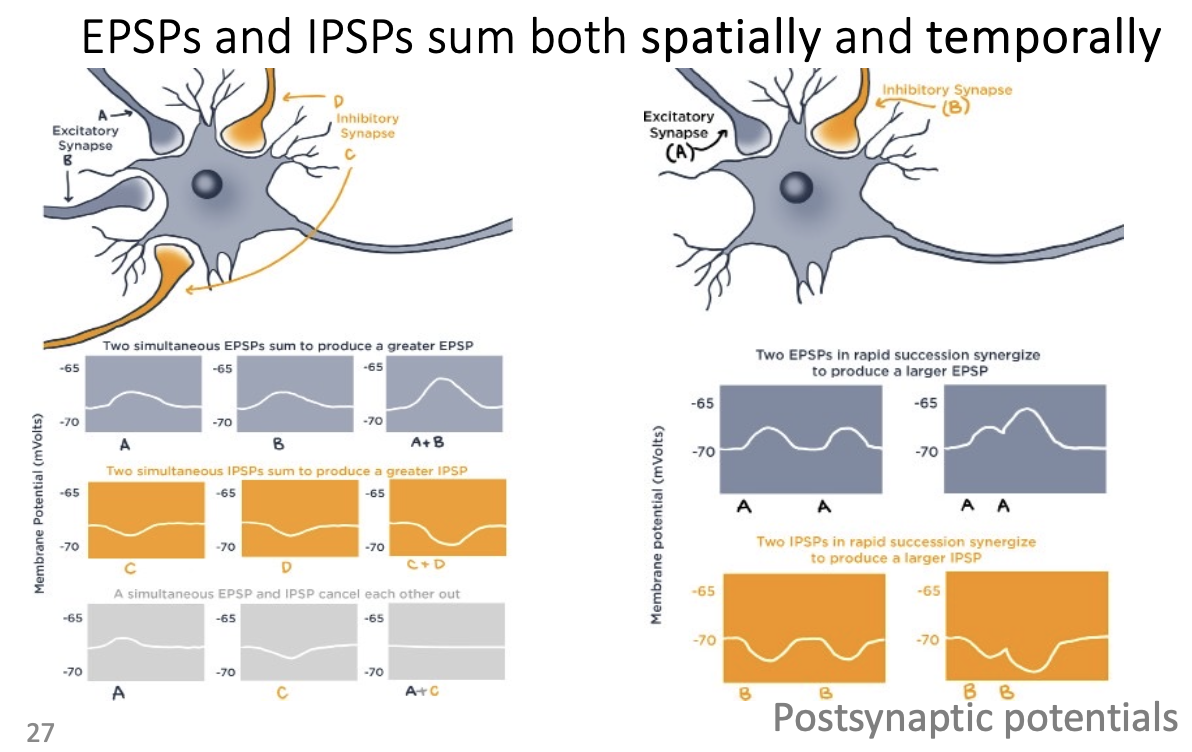
spatial summation
EPSPs arriving at different synapses summed all together
strongest ones are the ones closes to the axon - need a lot to reach action potential
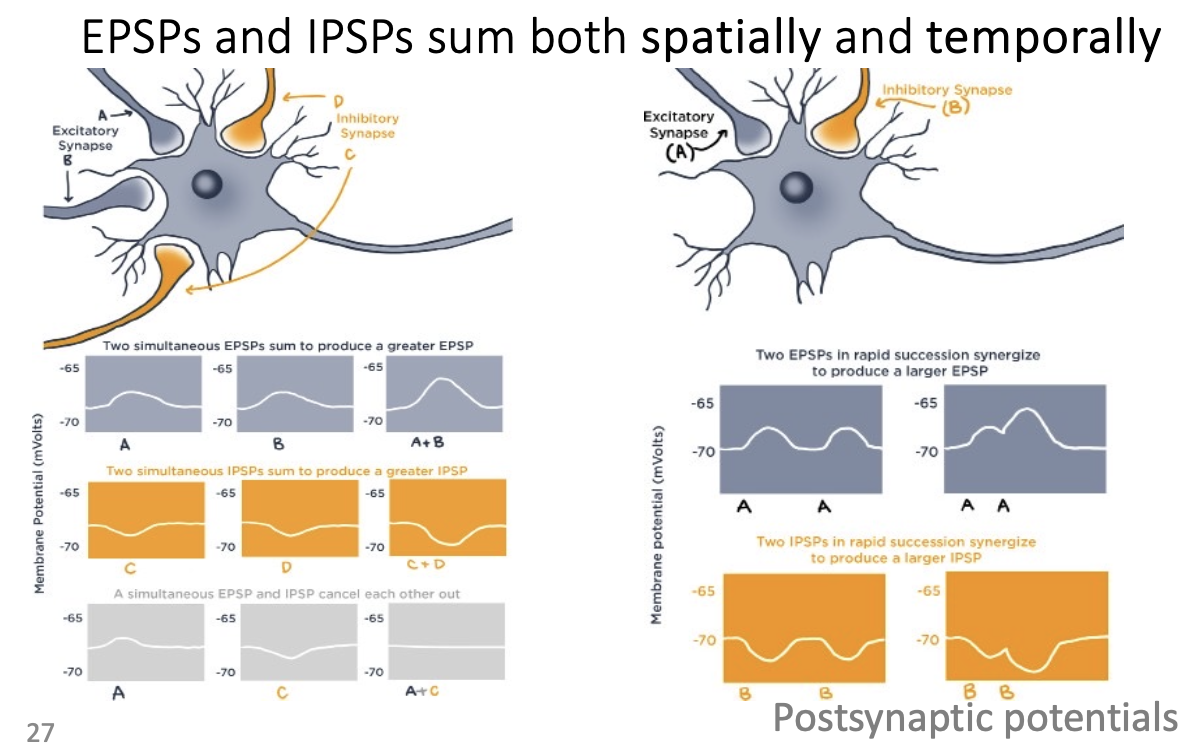
temporal summation
multiple EPSPS arriving in rapid succession to a neuron - produce a larger EPSP
where do the different potentials generate?
post-synaptic on dendrites
action on axons
what needs to happen for action potentials to generate?
EPSPS reach dotted line of threshold potential (-60 to -55 mV)
sum of EPSPs and IPSPs that reaches axon initial segment is sufficient enough to depolarize membrane above threshold of excitation (-55 mV)
only lasts for 1-2 milliseconds
action potential
rapid, brief reversal of polarity at the membrane, from negative to positive
main method of brain communication
once you reach the voltage threshold
all or none
what is the size of an action potential?
Always the same size/shape/ no matter the cells
How do neurons convey magnitude if action potential always looks the same?
through changing frequency/pattern of action potentials
rate coding: strong signal = more firing
temporal coding: specific patterns of firing depending on signal
population coding: strong signal = more neurons used
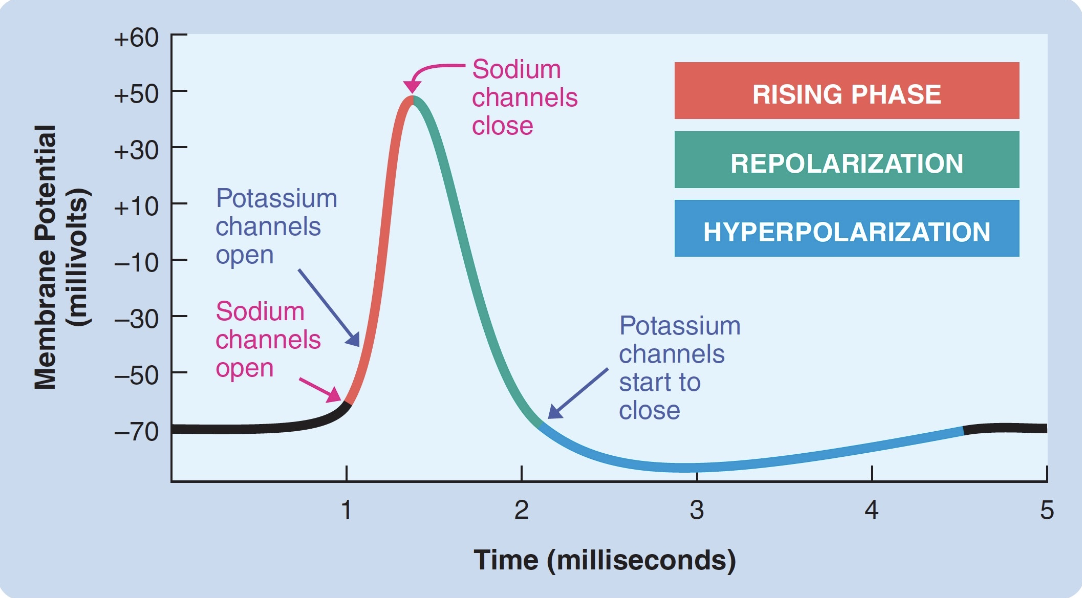
how does reversing polarity happen?
channels (voltage-gated Na channels) open at voltage threshold. (~55mV)
when enough EPSPs arrive at the same time, membrane depolarizes enough to reach Na+ channels’ threshold → channels open
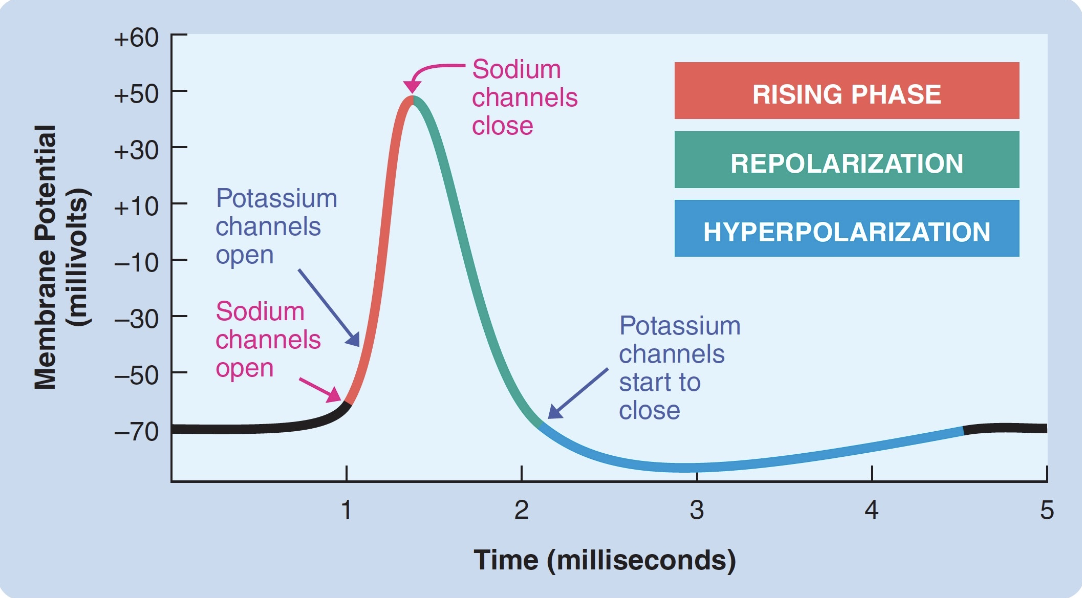
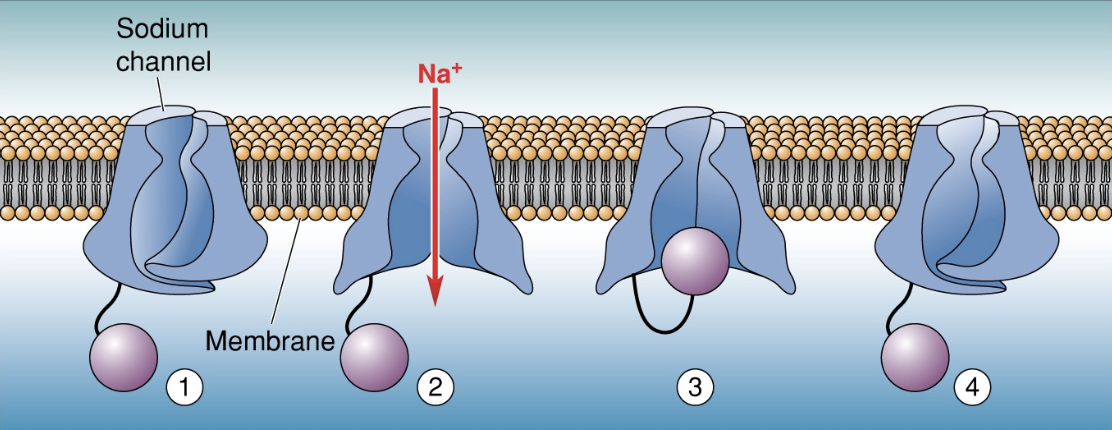
voltage-activated ion channels (Na)
Depolarization: Na+ coming into cell from gradient force (make cell positive)
Cross 0 mv to positive
Inactivated state: ball and chain - ball flips up to inside and plugs the channel
absolute refractory period: inactivated state to resting potentional = no neurons firing
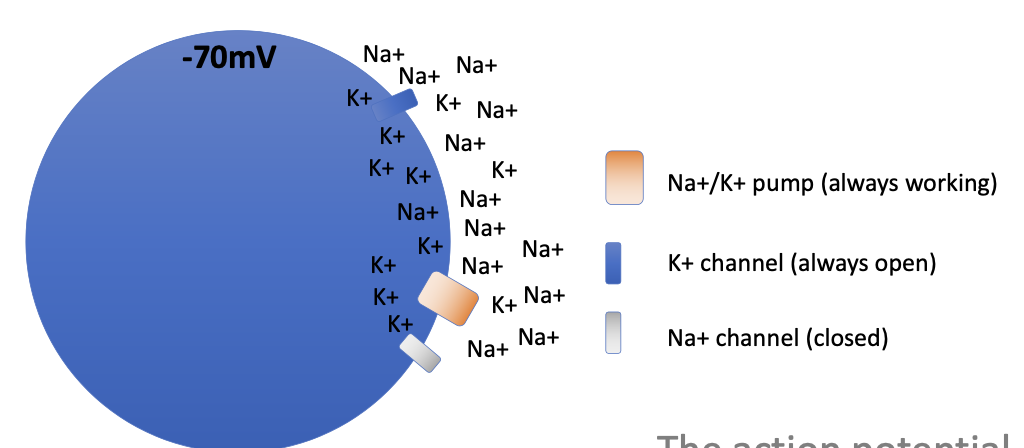
Which direction does Na+ want to flow in the cell?
wants to go inside the cell → makes cell more positive
what happens in a rapid, huge depolarization?
Na channels open and cell quickly flips from negative to positive - Na+ channels have built-in inactivation gate and shut off automatically after ~1 ms
Na channels stay inactivated until membrane goes back to resting potential (absolute refractory period)
K+ channels during repolarization
leak channels are always open, but are overwhelmed by forces against Na+ - even more open during AP
at peak of AP, membrane is positive because cell is very porous for K
which direction does K want to flow during repolarization?
wants to move outside of cell to return it to resting potential
hyperpolarization
slow closing of voltage-gated K+ channels - also contains a refractory period (can have action potential, it just takes more work)
returns to resting potential
Na/K pump restores ion balance over time - has no effect on AP
subthreshold stimulation of an axon
excitatory potential is produced, but not sufficient to elicit an AP
suprathreshold stimulation of an axon
excitatory potential is produced that exceeds threshold of excitation and produces an AP that continues undiminished down axon (conduction)
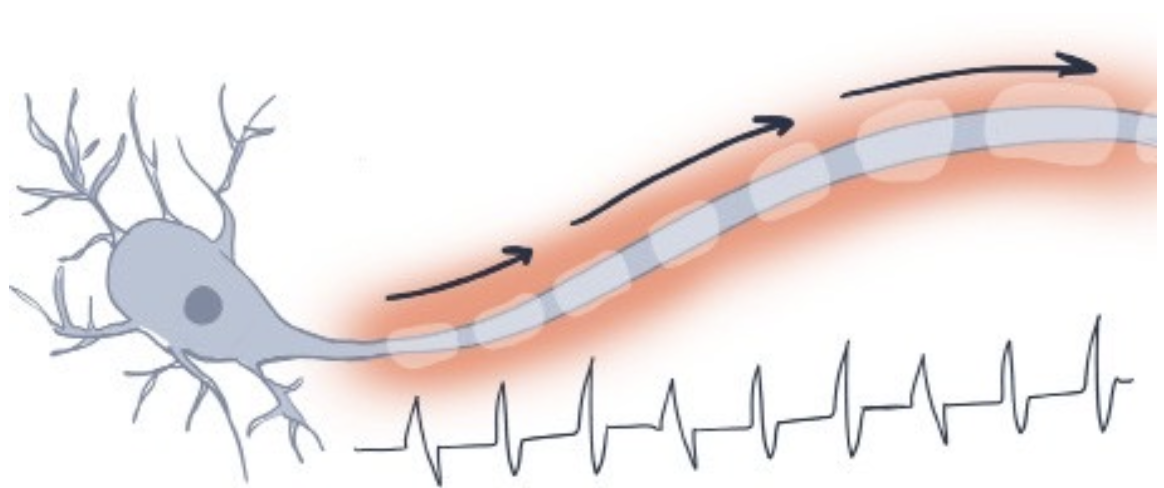
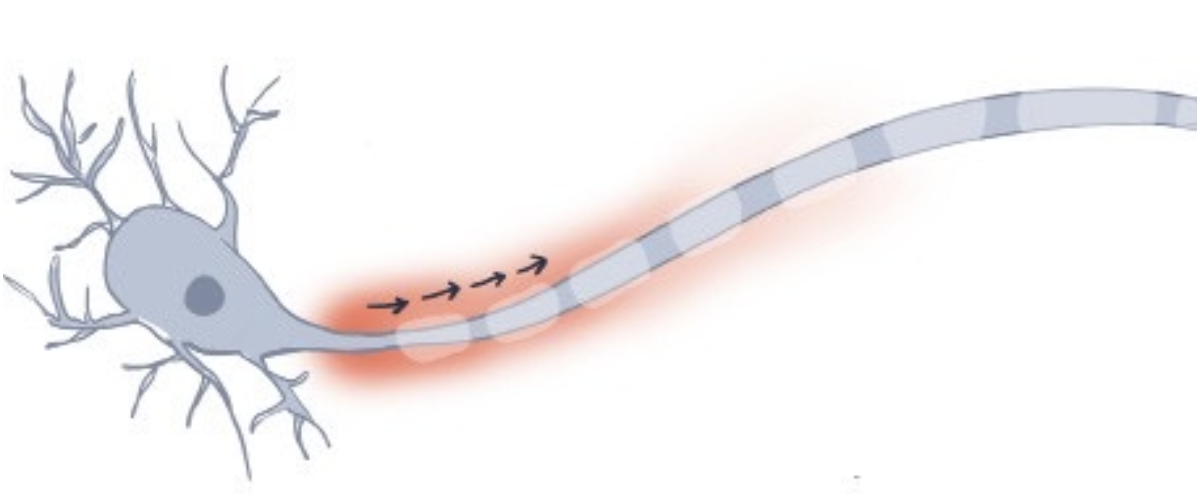
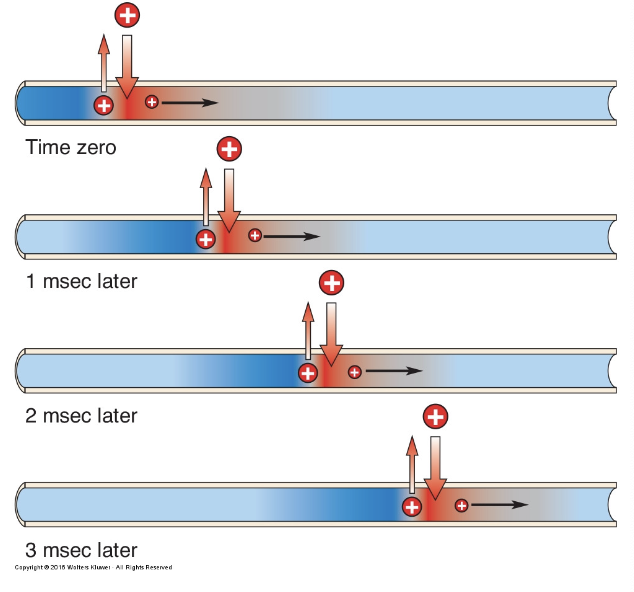
conduction in an unmyelinated axon
Na channels present all along axon - decaying slightly as signal goes, but constantly regenerated by voltage spreading to neighbouring Na channels
slows the process down slightly
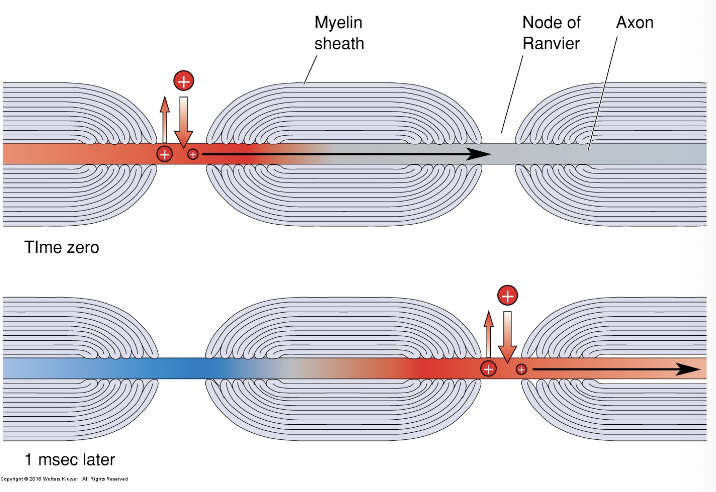
conduction in a myelinated axon
speeds up action potential conduction - insulating substance, lose less energy due to resistance
only find Na channels at Nodes of Ranvier (gaps between myelin) since AP can move passively by electricity
neurotransmission
end of signal transmission
terminal boutons with vesicles of neurotransmissions
AP depolarizes boutons → cause voltage-gated Ca+ channels to open → SNARE complex activates → fuses vesicles with membrane → nts released into synapse
synapse
dendrite membrane has special receptors that fit like lock and key with certain nts
receptors are often just closed channels that open when they bind with nts
types of potentials
look at image
Berthold, 1849: first experiment on hormones
loss of function experiment - testes removed or reimplanted into abdominal cavity in roosters
developed normally in both the control and reimplant condition
restoration of unction with native or donor testes
make a secretory blood-borne chemical" - brain isn’t only thing involved
hormones
released primarily by glands (sometimes other tissues), primarily into bloodstream (sometimes locally), primarily by animals (sometimes by plants)
exocrine vs. endocrine glands
endocrine glands release hormones
exocrine glands release fluid outside of body
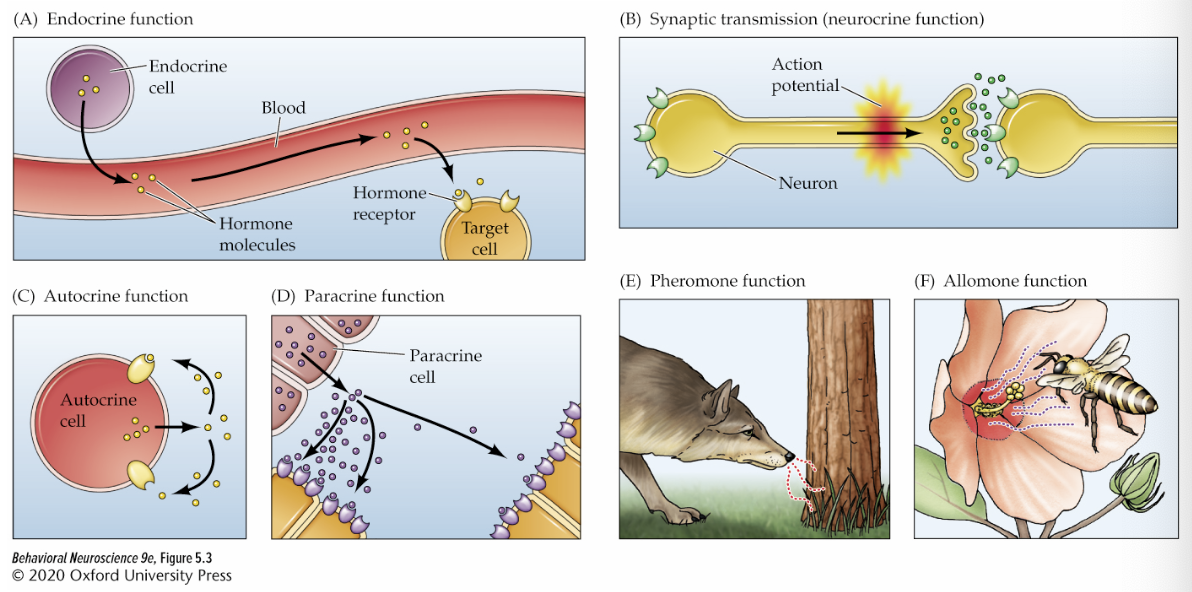
neurocrine function
neural communication - sends electrical signals
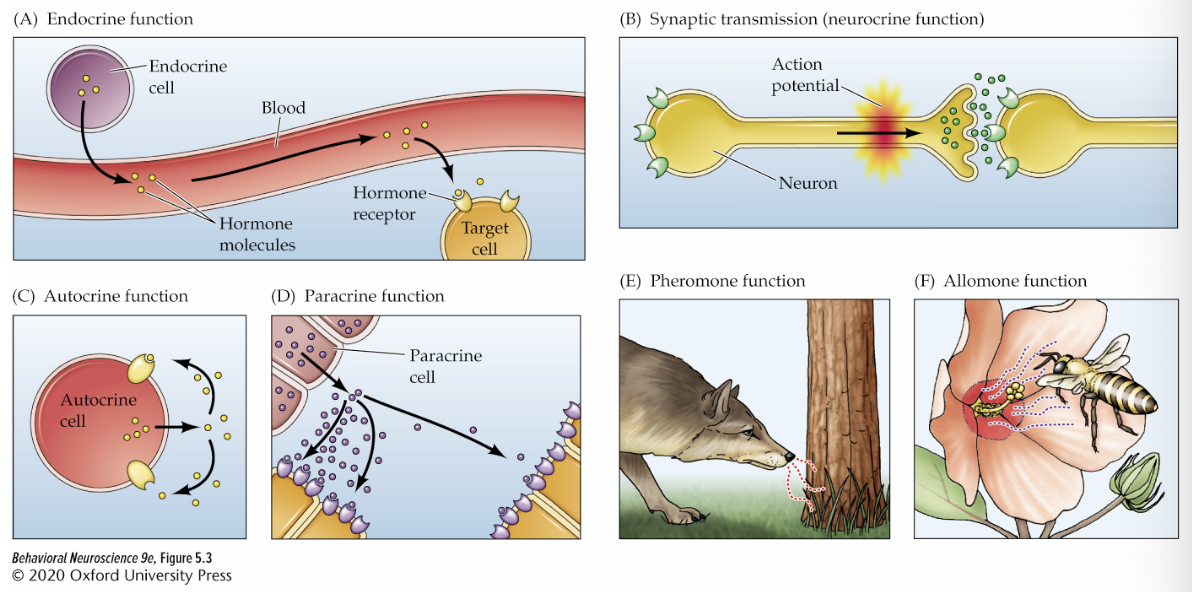
endocrine function
releases hormones into blood stream
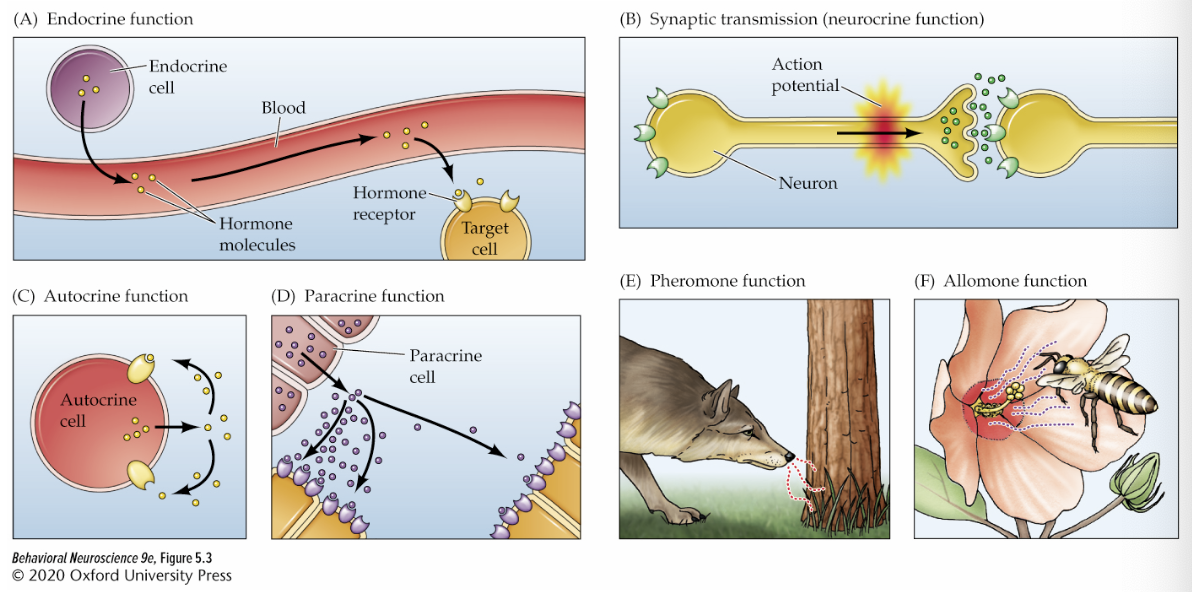
autocrine function
cells release signals to itself - hormone bind to receptors on the same cell (autoreceptors)
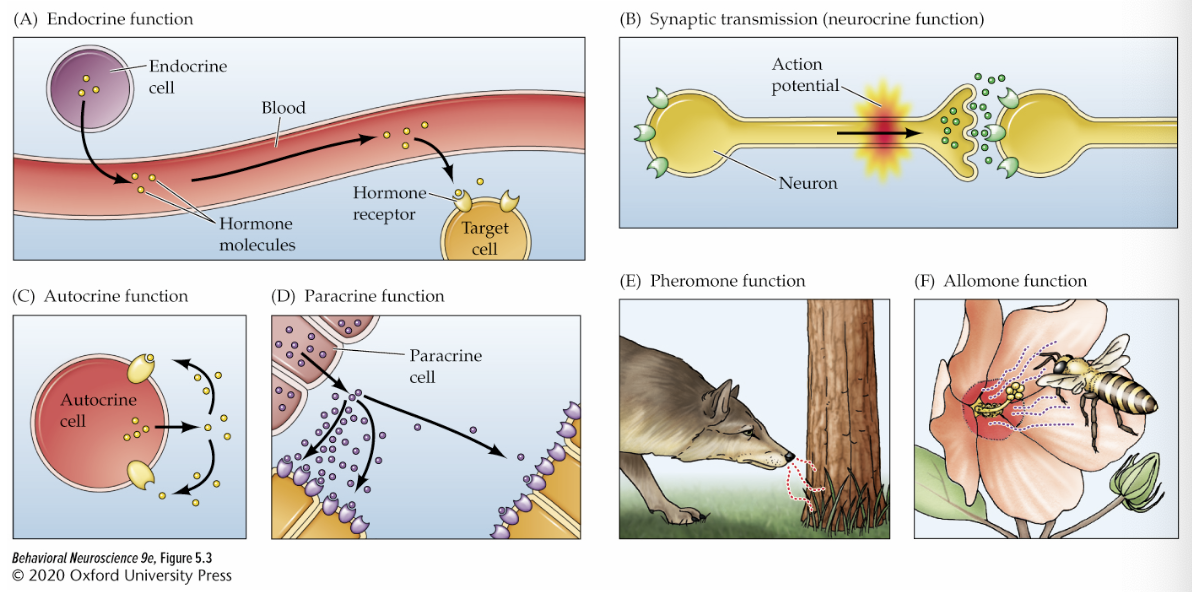
paracrine function
cells release to neigbouring cells (strongest effects on closest cells)
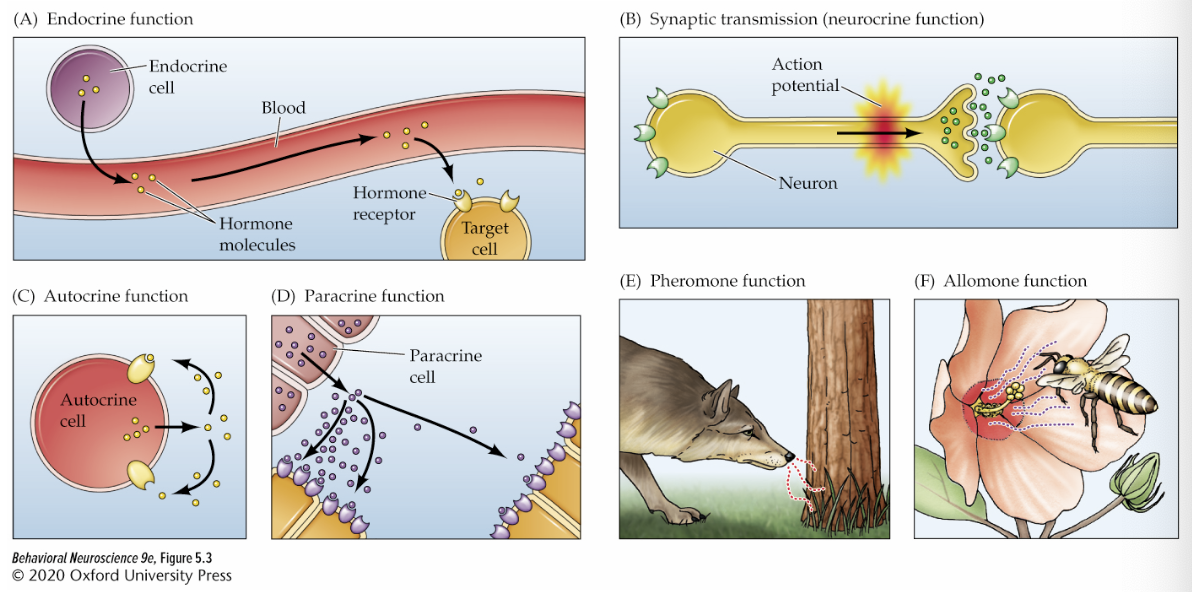
pheromone function
release hormones to other within species to smell
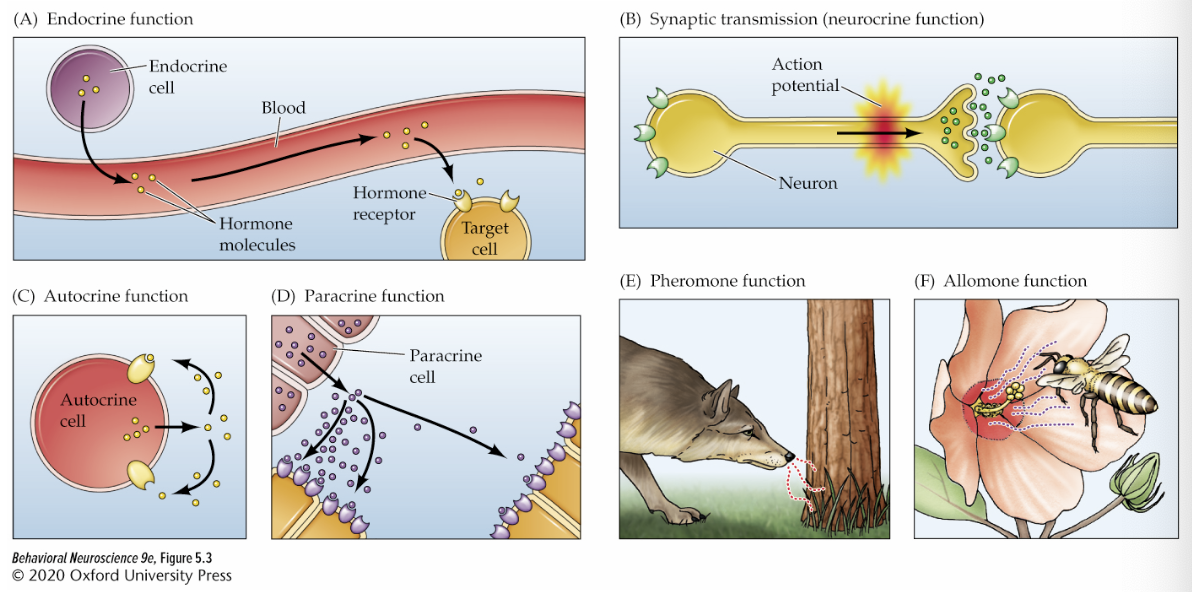
allomone function
one organism releases hormones that other species smell
principles of hormone function
slow-acting, gradual (effects in hours to weeks)
changes in intensity/probability
behaviour and hormone release are reciprocal (cause each other)
multiplicity of action - differ based on targets and effects
secretion is pulsatile/rhythmic (occurs at some points in day/month)
can interact
need receptors
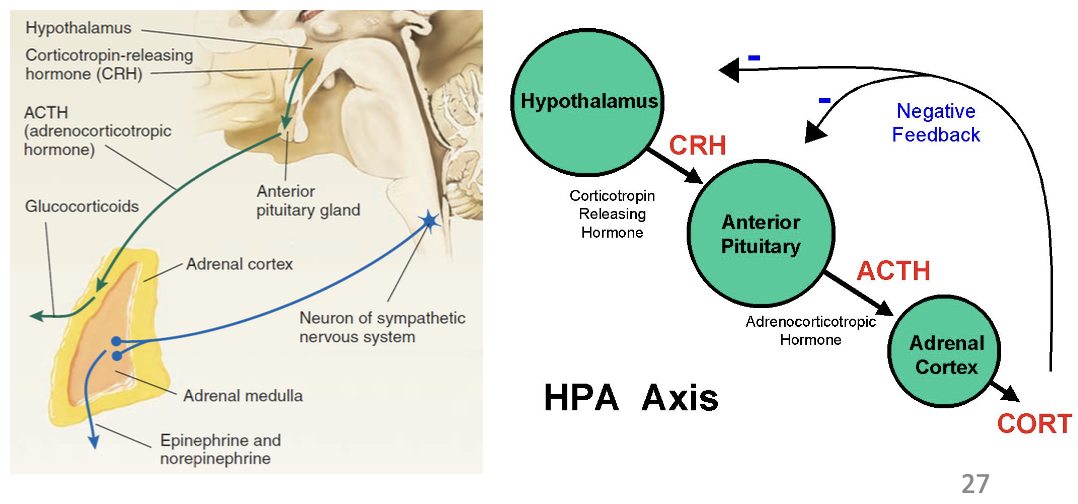
hypothalamus and hormones
junction between NS and endocrine system
contains neuroendocrine cells (neurosecretory cells)
some hormones also nts and some nts can be released by glands and neurons
peptide hormones
mostly outside cell - long strings of amino acids
amine hormones
mostly outside cell - single amino acid
steroid hormone
cross plasma membrane - similar structurally to cholesterol
hormone receptors
GCPRs - typically at the membrane, faster than neurotransmission
can also be in the cell (intracellular): usually near nucleus, transcription, slower
steroid hormones are intracellular
radioimmunoassay
measures hormone levels in the blood
autoradiography
measures brain areas affected by hormone
immunohistochemistry
measures horomones by creating antibody for hormone receptor to bind onto
immunocytochemistry
measures hormones by taking a section of tissue to look at receptors
in situ hybridization
measures hormones by taking a complementary strand of RNA and adding a fluorescent tag to see where a hormone receptor is
hormone negative feedback mechanisms
similar to synapse feedback - autocrine feedback, target cell feedback, brain regulation, brain and pituitary regulation, certain hormones for certain things
autocrine feedback
same as autocrine hormone - release hormones that bind on same cell
target cell feedback
target cell's response to a hormone regulates the further release of that hormone by the original cell
brain regulation of hormone
hypothalamus interacts with pituitary glands and generates activity in endocrine cells
pituitary gland
other side of NS/endocrine intersection - has anterior and posterior divisions
posterior pituitary gland
axons coming thalamus, down infundibulum to capillaried
releases hormones in capillaries
no dedicated endocrine cells
axons relese oxytocin and vasopressin/anti-diuretic hormone (ADH) into blood
oxytocin
stimulates uterine contraceptions; milk letdown reflex
ADH
releases when dehydrated - conserves water through blood vessel constriction
alcohol inhibits ADH release - why it makes you urinate/more dehydrated
anterior pituitary gland
neuroendocrine cells terminate at median eminence, release tropic hormones
hormones carried via hypophyseal portal veins
tropic hormones cause further hormone releases
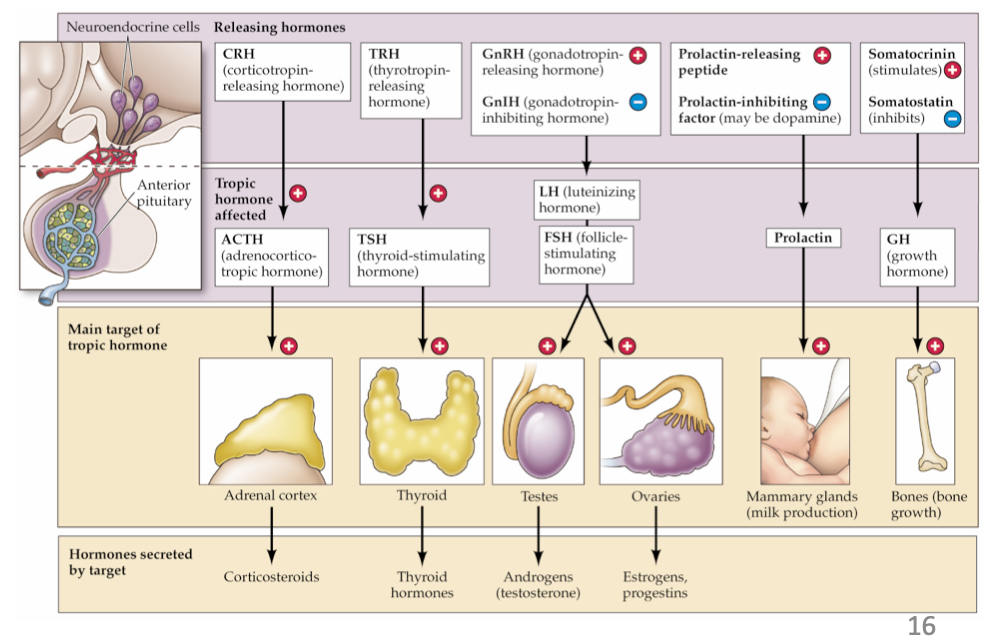
adrenal glands
adrenal cortex (gets hormones) and medulla (gets inputs from CNS)
cortex releases steroid hormones: glucocorticoids (cortisol), mineralocorticoids (aldosterone), sex steroids (androstenedione) - synthesized on demand via ACTH
medulla releases amine hormones: epinephrine and norepinephrine
thyroid glands
releases thyroid hormones: thyroxine, triiodothyronine
amines that act like steroids
regulate growth and metabolism
activating effect on NS - needs iodine
pineal glands
releases melatonin
has photoreceptors (third eye?)
from sympathetic NS - as melatonin goes up, gonad hormones go down
not a target of anterior pituitary
gonads
two compartments - one for sex hormone production, one for gamete production
GnRH and org GNIH (peptide nts)
testes
sertoli cells - sperm
leydig cells - androgens (testosterone)
ovaries
ova - mature gametes
steroid hormones (progestins)
do hormone influence behaviour?
yes, but more notable limitations in humans than in animals
our cortex often supersedes many older controls for behaviour
does behaviour influence hormones?
psychosocial dwarfism: stress can cause reduced release of growth hormones
more exogenous oxytocin in rats makes them touch each other more → less cause social amnesia (don’t remember each other)
prarie vole types: prarie voles are monogamous (and have high density oxy), meadow voles are not (have low density oxy)
is oxytocin the love molecule?
Not directly - blocking oxytocin increases sociability, but also increases in-group bias and propensity for revenge
do pheromones meidate behaviour?
not in humans
animals = yes (vomeronasal organ [VNO])
we do not really have a VNO
human pheromone effects (sweat studies) often do not replicate
do stress hormones mediate behaviour?
yes - part of stress response is central (in brain)
dual pathway, HPA axis, sympathetic NS causes immediate changes in behaviour
hippocampus maintains stress (suffers under chronic stress)
Schacter and Singer, 1962: placebo stress vitamin caused less stress response
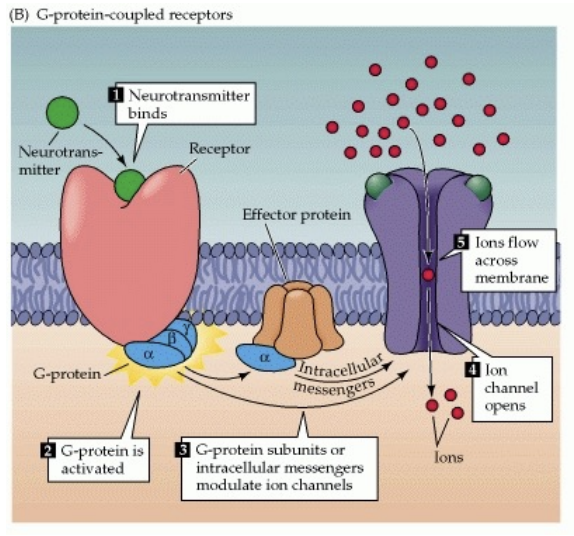
metabotropic receptors (G-protein-coupled receptors [GPCR])
signalling proteins - don’t allow ions to cross membrane directly
also utilized the ionotropic receptors
no holes/channels/pores
metabolism-like effect
releases G-proteins when nts bind to receptor
indirectly cause IPSPs and influence rates of transcription/translation
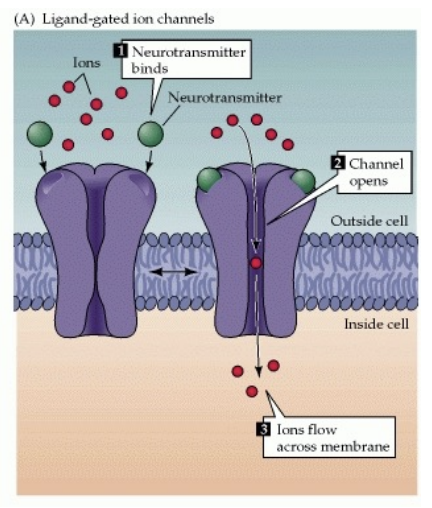
ionotropic receptors (ligand-gated ion channels)
ligand binds to them and then they open
Excitatory (EPSPs - lets Na or K into cell) and inhibitory (IPSPs - lets chloride into cell)
common for glutamate
where are nt receptors most commonly located?
postsynaptic side
presynaptic receptors
autoreceptors
heteroreceptors
both influence how many nts are released
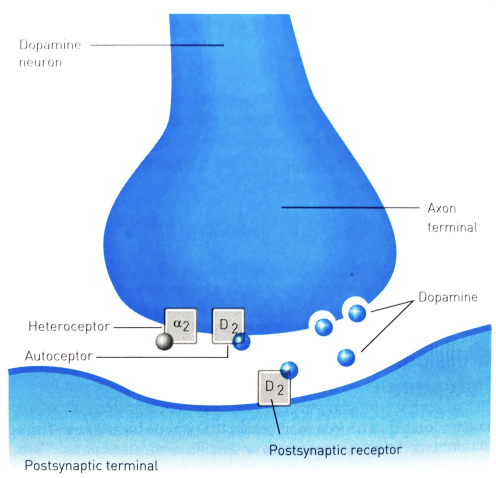
autoreceptors
regulates synthesis and release of own nts
negative feedback system - don’t want neurons to lose too many nts
inhibit the axon when they identify too many nts being released (not the same as reuptake)
heteroreceptors
receptors that regulate release of different nts - ex. dopamine binds to norepinephrine
don’t cause nts to be released but influence how much are released
the “volume” of the “music”
importance of neurotransmitter clean-up?
without it, nt signals would never ed
types: diffusion, enzymatic degradation, re-uptake
diffusion
nts floating away from synapse - not common unless we want the nts to bind to neighbouring synapses
enzymatic degradation
specialized enzymes that break down nts into metabolites (can’t activate receptors)
red to green in image
MAO, COMT
not the preferred way - energetically wasteful
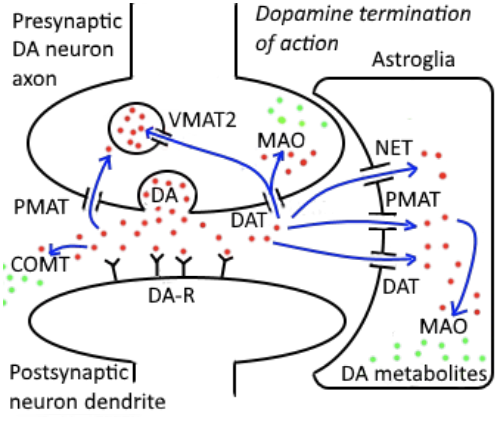
re-uptake
repackage nts back into vesicles (into axon and then into vesicle) - most common clean up method
pre-synaptic = PMAT, DAT (dopamine) - back into axon; VMAT = to vesicles
astrocytes = PMAT, DAT, NET (can make clean-up faster
drug types
agonists
antagonists
also transporter blockers, reuptake inhibitors, enzyme inhibitors
amino acids
glutamate
GABA
monoamines
catecholamines: dopamine, epinephrine, norepinephrine
indolamines: serotonin
acetylcholine
is its own neurotransmitter system
small-molecule neurotransmitters
amino acids
monoamines
acetylcholine
unconventional neurotransmitters
large molecule neurotransmitters
neuropeptides → opioid peptides
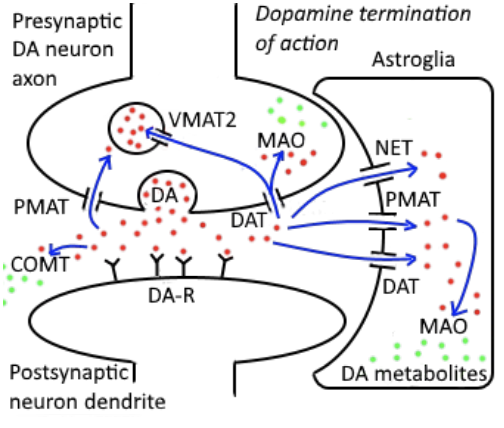
glutamate
primary excitatory nt
used throughout brain
ionotropic and metabotropic receptors
some glutamate-targeted drugs inhibit nt receptors because they affect negative feedback mechanisms
often not a great target for drugs because its all over the brain
typically antagonist drugs
glutamate receptors
ionotropic: AMPAS, NMDAR, Kainate receptor
metabotropic: mGluR 1-8
glutamate drugs
antagonists
barbiturates
nitrous oxide
ketamine
ethanol
agonists? - can cause seizures when excitation is really high since it excites other nts
GABA (gamma-aminobutyric acid)
primary inhibitor nt, used throughout brain
GABA-A = ionotropic, GABA-B = metabotropic receptors
also not a great target for drugs because it is everywhere
agonist and antagonist drugs
GABA drugs
agonists
benzodiazepines: therapeutic and recreational, reduces anxiety (Xanax, Ativan)
ethanol: decreases excitation and increases inhibition (also glutamate agonist)
chloroform
ether
antagonists looks similar to glutamate agonist, vice versa
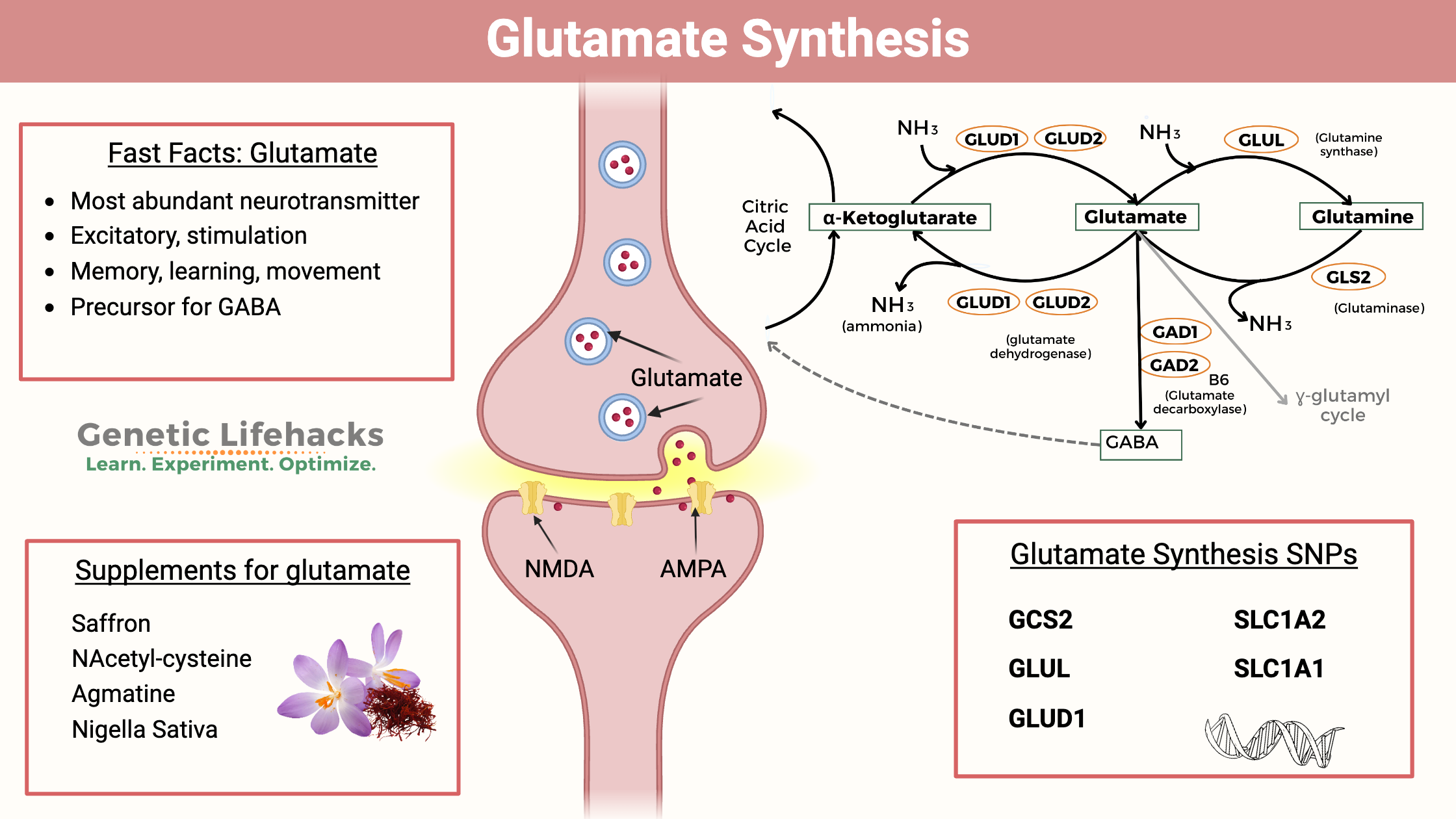
where is dopamine in the brain?
originates from 2 nuclei in tegmentum
substantia nigra pars compacta
ventral tegmental area
projects to some, but not all brain areas; also made in hypothalamus
tyrosine = dietary precursor → converted to DA by enzymes (first converted to DOPA)
DA receptors
D1R-D54/D1-5
all metabotropic
some positive modulatory, some negative
what does DA do?
it is NOT the pleasure/reward molecule
does dopamine facilitate motivation for brain stimulation? (Olds and Milner, 1954)
electrodes accidentally hit the ventral tegmental area going to nucleus accumbens → dopamine axons project from VTA to NAcc
caused rats to self-stimulate dopamine release by pressing a button constantly until exhaustion
dopamine must be part of pleasure circuit (valid but incorrect conclusion)
Actually, humans who did this study reported that the sensation was unpleasant but felt compelled to do it
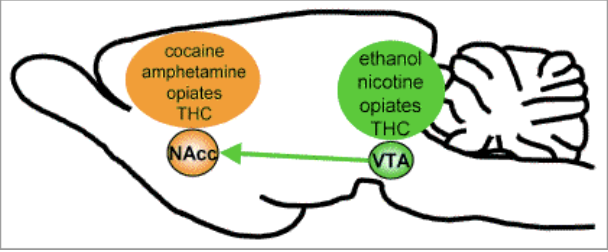
addiction and dopamine
all addictive drugs directly or indirectly increase dopamine transmission
amphertamine and cocaine directly do
heroin, nicotine, oxycodone, ethanol, cannabinoids indirectly do
Nicotine only has mildly euphoric effects for heavy smokers - why is it addicting?
stimulates the VTA to NAcc pathway causing a feeling of obligation towards smoking once you start
dopamine and parkinson’s disease
caused by a loss of neurons in substantia nigra pars compacta (SNc) → dopamine producing region in tegmentum
causes difficulty initiating voluntary, spontaneous behaviour (feel frozen), trembling of extremeties, shuffling gait, stooped posture
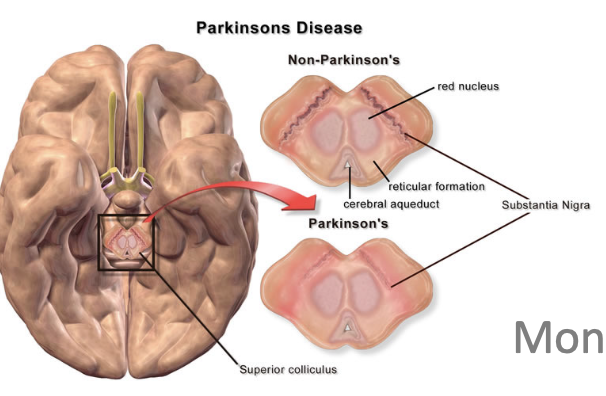
how to treat parkinson’s?
gold standard: administering L-DOPA
dopamine can’t cross blood-brain barrier but L-DOPA can (subsequently convert L-DOPA to dopamine)
improvement of motor skills
don’t see great increase in pleasure levels
high levels of L-DOPA can cause impulsivity, gambling, high sexuality
other drugs: D1 agonist
dopamine and schizophrenia
people with it have too much dopamine - not more likely to experience pleasure (have loss of touch with reality)
individuals with schizophrenia do not have higher baseline pleasure levels
agonist drug
bind to receptors and activates them
antagonists
drugs that block or reverse receptors by binding to them
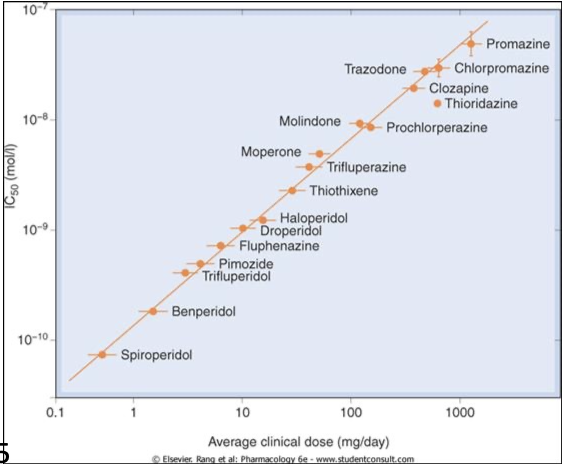
treatment of schizophrenia
all initial medications are DA D2R antagonists (gradually build up)
more effective drugs are as agonists = more effecting at treating schizophrenia
all illicit drugs can increase risk of schizophrenia/schizophrenic symptoms due to increase in DA
psychostimulants and dopamine
cocaine, crack cocaine, methamphetamines, cathinones
act on different monoamine systems - esp. DA, NE, 5-HT
crack has highest increase in dopamine - hard to quit
cause a wide range of effects (including euphoria)
high doses can cause temporary psychosis
not easily distinguishable from positive symptoms of schizophrenia
separating pleasure from motivation (Salamone, 1990s)
t-maze task with rats - can choose two options: low effort, low reward vs. high effort, high reward
training by blocking one of 2 arms
free choice baseline trial: more likely to choose high effort
choice + DA antagonist trial
choice + DA antagonist + no barrier trial
give them dopamine antagonists = decrease motivation, but no pleasure or preferences (switch preference to low effort)
when barrier is removed, they switch back to original preference (still with DA antagonist