Micro Exam #4
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
148 Terms
Discuss the origin, structure, and function of the viral envelope
The envelope is acquired from the host cell during viral replication.
Comprised of a phospholipid bilayer.
Some of the proteins on the envelope are from the virus.
The envelope does not act like a cell membrane.
Enveloped viruses are easier to kill than non-enveloped
List the characteristics by which viruses are classified
Type of Nucleic Acid
Presence of an Envelope
Shape
Size
Sketch and describe the five stages of the lytic replication cycle as it typically occurs in bacteriophages
attachment
entry
synthesis
assembly
release
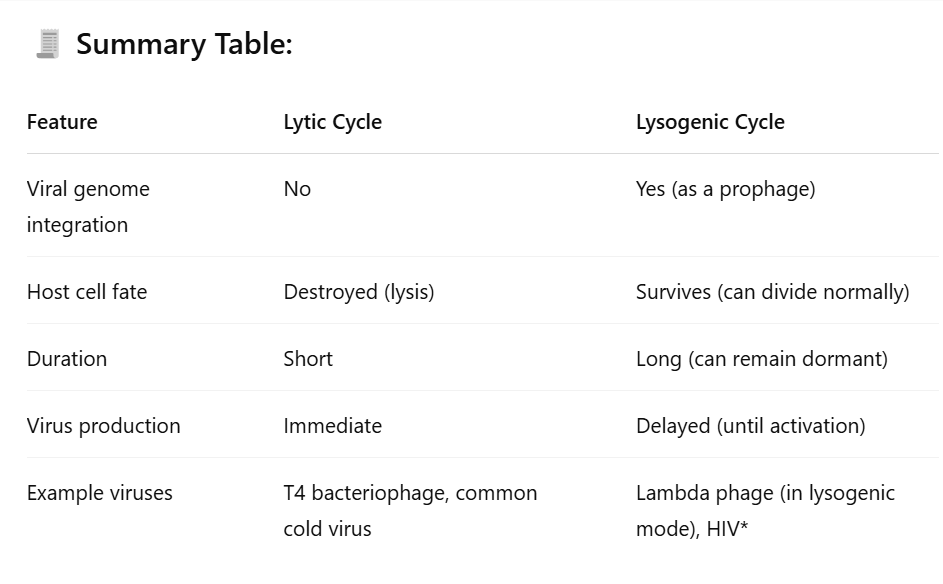
Compare and contrast the lysogenic replication cycle of viruses with the lytic cycle
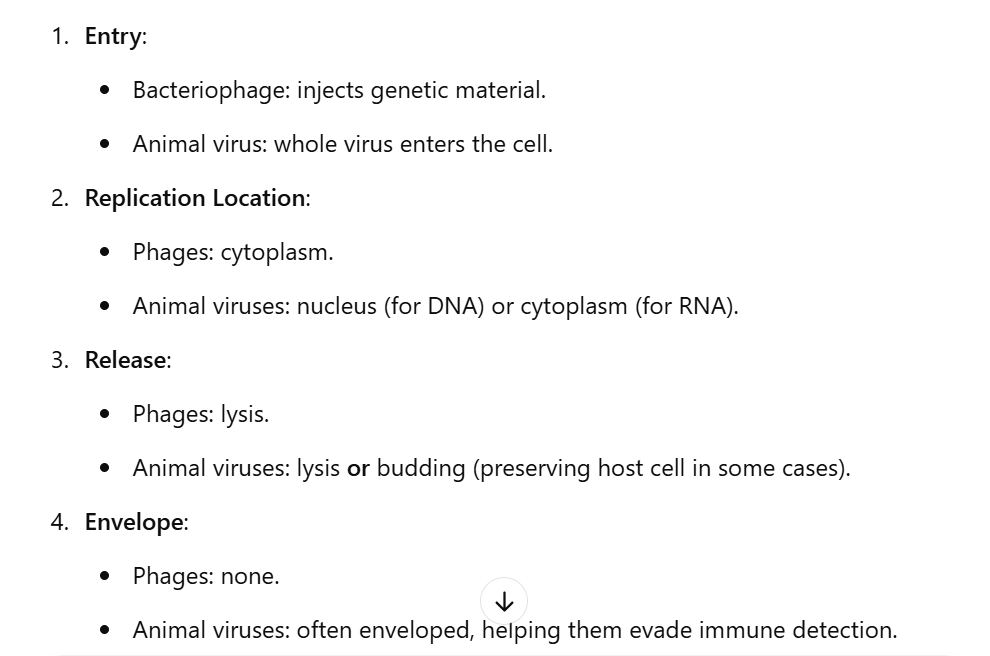
Explain the differences between bacteriophage replication and animal viral replication
take note of the glycoprotein spike on the envelope of the animal virus.
attachment of lytic cycle
Virions are nonmotile so contact with host cell is random.
▪ Dependent upon chemical attraction and precise fit between tail fibers and host receptors.
▪ In the case of the E coli phage, it will only attach to pili, cell walls or flagella of that specific type
entry of lytic cycle
To break through cell wall, the phage will release lysozyme to dissolve through cell wall.
▪ The tail sheath of the virus then contracts and forces a tube into the bacterial cell.
▪ After entry, viral enzymes degrade the bacterial DNA into its constituent nucleotides
synthesis of lytic cycle
After the bacterial chromosomes are degrades it stops making its own molecules and begins
synthesizing new viruses directed by the viral genome.
▪ For dsDNA viruses, the viral genome directs the synthesis of new capsid proteins, tail, viral
polymerase and lysozyme
assembly of lytic cycle
Capsid proteins begin to assemble inside the host cell.
▪ Tails and tail fibers begin to assemble and attach to head.
▪ Capsids form around viral genomes or the genomes are pumped into the newly formed capsid.
release of lytic cycle
As lysozymes weakens the cell wall of the bacterium the new virions can burst free from the cell.
For the T4 bacteriophage the whole process takes about 25 minutes and up to 200 new virions are released.
▪ Burst time – how long it takes to complete the process.
▪ Burst size – how many new virions are released
attachment of lysogenic cycle
Same as in lytic cycle, but the host cell’s DNA is not destroyed
attachment of entry cycle
viral DNA remains silent as a prophage
prophage entry of lysogenic cycle
Prophage incorporates itself in the host cell’s DNA
lysogeny of lysogenic cycle
Every time the bacterial chromosome replicates, the viral DNA is copied along with it.
All daughter cells will now carry the prophage.
Lysogenic phages can cause the phenotype of the bacterium to change from harmless into pathogenic
induction of lysogenic cycle
At some point the prophage may be excised from the host DNA.
At this point it reenters the lytic phase
Inductive agents include: physical and chemical agents that damage bacterial DNA
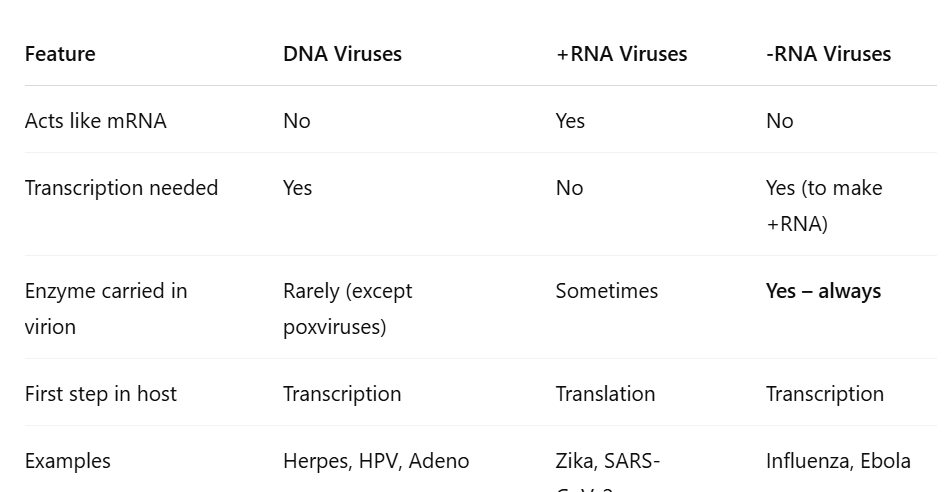
Compare and contrast the replication and synthesis of DNA, -RNA, and +RNA viruses
Compare and contrast the release of viral particles by lysis and budding
Lysis: (Explosive Exit) Viruses build up inside the cell until it ruptures. The host cell is killed. This is typical for bacteriophages and non-enveloped animal viruses.
Budding:(Stealthy Exit) Virus pushes out of the membrane, taking a portion of it as its envelope. The host cell often survives for a time, allowing prolonged viral production. Common in enveloped viruses like HIV, Influenza, and Herpes.
Compare and contrast latency in animal viruses with phage lysogeny
Lysogenic phages can cause the phenotype of the bacterium to change from harmless into pathogenic, integrates into a bacterial chromosome. Phage lysogeny occurs when a bacteriophage (a virus that infects bacteria) enters a dormant state inside a bacterial cell instead of immediately replicating and lysing the host.
Latency in animal viruses occurs when a virus enters a host cell and establishes a long-term, dormant infection without producing new virus particles right away.
There are three methods for viruses to enter animal cells
Direct Penetration – done by some naked viruses.
2. Membrane fusion – phospholipid of the viral envelope fused with host cell.
3. Endocytosis – when the virus trigger receptors on the cell surface to engulf the entire virion
Explain in simple terms how a cell may become cancerous, with special reference to the role of viruses.
Two-hit viruses cause cancer.
The most well-known is cervical cancer caused by HPV (solve by HPV vaccine)
In the Two Hit hypothesis, a virus inserts a promotor that converts a protooncogene into an oncogene. Often this first hit doesn’t cause cancer, but if a second hit damages the downstream repressor gene, then the oncogene disrupts cell division and causes cancer
Protooncogenes
are genes in a host cell involved in normal cell division.
Describe some ethical and practical difficulties to overcome in culturing viruses
ethical difficulties: use of living host (this raises concerns about chicken eggs used to work on vaccines). Informed consent. Risk of biohazard exposure. Genetic modification.
physical difficulties: viruses can’t grow on their own. Host specificity. Slow growth and detection. Contamination risks.
Explain the use of a plaque assay in culturing viruses in bacteria
Quantification: Provides an accurate count of infectious phages.
Purification: Individual plaques can be picked to isolate pure phage clones.
Visual Confirmation: Easy to see and measure viral activity.
Efficiency: Helps assess host range, mutation rates, or lytic ability of a phage.
Discuss aspects of viral replication that are lifelike and non-lifelike.
lifelike: reproduction (with help), genetic material (contain DNA and RNA), adaptation, high specificity
non-lifelike: no metabolism, incapable of independent replication, no cellular structure, do not grow
Define and describe prions
These are infectious protein particles, not viruses.
Prion replication process
In human prion diseases a normal PrP protein’s structure becomes altered and begins to affect other
PrP proteins around it.
As more of the altered PrP proteins aggregate it causes neurons to die and leave holes in the brain.
Diseases caused by prions are called spongiform encephalopathies
Prions are different from viruses because:
no genetic material, just proteins
simpler structure
Prions replicate by converting normal proteins into the misfolded prion form—no need for genes or host-cell machinery.
Describe methods to control and destroy prions
They are not removed through normal autoclaving or decontamination processes.
excess heat
autoclaving with special conditions
chemical decontamination
List four diseases caused by prions.
BSE – Mad Cow disease (most famous)
CWD – in deer and elk (most common the US)
vCJD – in humans (100% fatal)
Kuru - earlier discovered in a tribe
Scrapie - in sheep and goats
Distinguish among four types of symbiosis
Mutualism
Commensalism
Amensalism
Parasitism
Describe the relationships among terms parasite, host, and pathogen
A parasite is an organism that lives on or in another organism (the host) and benefits at the host’s expense
The host is the organism that the parasite lives in or on.
A pathogen is any disease-causing agent. It includes parasites, but also bacteria, viruses, fungi, and prions. So: All parasites that cause disease are pathogens, but not all pathogens are parasites.
Describe the relationships among terms parasite, host, and pathogen simply:
A parasite lives in/on a host.
If the parasite causes disease, it is also considered a pathogen.
A host is negatively affected by the presence of a parasite or pathogen.
Describe the microbiome, including resident and transient members.
The microbiome refers to the community of microorganisms—including bacteria, viruses, fungi, and protozoa—that live in and on the human body
Residents are to be expected. Transients are temporary visitors and eliminated by the immune system.
Resident microbiota
Upper respiratory tract - strep or staph
Upper digestive tract (oral cavity) - strep, Neisseria, staph, treponema
Lower Digestive tract
Female Genitourinary tract - corynebacterium, lactobacillus
Male Genitourinary tract - corynebacterium, streptococcus
Eyes and Skin - candida albacans, gram + organisms
Transient microbiota
Temporary hitchhikers for hours, days, etc.
Found in the same places as resident until they are dislodged by competition, immune cells, or changes to the host body
Rid through the immune system
Examples: Skin bacteria you pick up from a doorknob. Bacteria in food that pass through the gut without colonizing
Describe three conditions that create opportunities for normal microbiota to cause disease.
immune system weakened
antibiotics. changes in normal flora
introduction to a new site in the body
stressful conditions
Describe three types of reservoirs of infection in humans
A reservoir of infection is any place where a pathogen normally lives, grows, and multiplies—basically, where it “hangs out” before infecting someone
animals (zoonoses)
human carriers (sneezing, coughing, physical touch). Typhoid mary.
nonliving reservoirs: soil (anaerobes like clostridium), water, food
Describe the relationship between contamination and infection
Contamination: the presence of microbes on or in the host’s body. Can have no effect. They can become part of our normal flora. Remain as transients for a time. Become pathogens
Infection: When a microbe invades one of our normal systems and overwhelms it. Some infections do not cause disease.
Identify and describe the portals through which pathogens invade the body
skin
mucous membrane (major portal of entry). most common portal is the respiratory membrane
placenta
the parenteral role
List the types of adhesion factors and the roles they play in infection
Viruses and bacteria most commonly use lipoprotein or glycoprotein ligands that allow them to attach to receptors on the host cells
Fimbriae and Pilli will stick to the host cell’s surface
Biofilms: The sticky web created when certain pathogens interact with each other inside the host. Remember that many organisms only cause disease when they are in biofilm form. Some bacteria will change their phenotype drastically when in a biofilm
Explain how a biofilm may facilitate contamination and infection
Microbes land on a surface
Biofilm forms and protects the colony
Surface becomes contaminated
Microbes break off and infect new areas
Infection becomes chronic and hard to treat
define infection
When a pathogen invades a host
define disease
When the injury caused by the pathogen is significant enough to interfere with normal functioning
of the host
define morbidity
Refers to the state of being diseased or the rate of disease in a population. Measures how many people get sick (not necessarily die).
define pathogenicity
The ability of a microorganism to cause disease. It’s a yes/no property—can it cause disease or not?
define virulence
The degree or severity of pathogenicity. In other words, how harmful or aggressive the pathogen is once it causes disease.
Symptoms
Symptoms – Subjective characteristics sensed by the patient.
▪ Pain
▪ Nausea
▪ Headache
▪ Sore throat
▪ Fatigue
▪ Itching, cramps etc.
Signs
Signs – Objective signs of disease that are measurable.
▪ Swelling
▪ Rash or redness
▪ Vomiting
▪ Diarrhea
▪ Fever
▪ Increase or decrease in WBC’s
▪ Increase or decrease in HR
▪ Increase or decrease in BP
Syndrome
Syndrome – A group of signs and symptoms that characterize a disease.
▪ AIDS – hallmarks are malaise, decrease in T4 cells, diarrhea, weight loss, pneumonia, other rare
fungal infections and cancers
Explain how microbial extracellular enzymes affect virulence
Extracellular Enzymes
▪ Hyaluronidase – destroys hyaluronic acid a key substance in ground substance.
▪ Collagenase – destroys collagen allowing bacteria to spread.
▪ Coagulase – causes blood clotting (what lab test did we do for this?)
▪ Kinases (Streptokinase, Staphylokinase) – digest blood clots and release bacteria
Explain how microbial extracellular toxins affect virulence
Exotoxins – produced and released by the bacteria.
▪ Cytotoxins
▪ Neurotoxins
▪ Enterotoxins
▪ Endotoxins – The lipid A component of a gram negative cell wall
▪ Released when the cells die or are destroyed by the host.
▪ Can cause – fever, inflammation, diarrhea, hemorrhage, shock, coagulation
Explain how microbial extracellular adhesion factors affect virulence
These include fimbriae, pili, surface proteins, and viral spikes that help pathogens attach to host cells.
🔹 How they increase virulence:
Allow microbes to stick to host tissues, resist flushing mechanisms (like mucus or urine), and colonize specific areas.
Explain how microbial antiphagocytic factors affect virulence
Capsules – are composed of the same things as body cells. Can evade detection for longer. Some capsules also make the bacteria very slippery and had to grab.
Antiphagocytic Chemicals – chemicals produced by bacteria that prevent lysosomes in the phagocytes from attaching to the bacteria and allows them to survive inside the phagocytes. E.g. – M factor produced by Strep pyogenes
List and describe the five typical stages of infectious diseases
incubation period
prodromal period
illness
decline
convalescence
incubation period
Time between infection and when symptoms first appear.
Depends upon the virulence of the microbe, the infective dose, state of the health of the host, nature of the pathogen, and the site of infection.
Even the same pathogen will have different incubation periods based upon the factors above
prodromal period
A short period of generalized mild signs and symptoms.
Some infectious diseases skip this step. (think about GI bugs)
illness
Most severe stage, signs and symptoms are in full bloom.
Host’s immune system has not responded adequately yet or is being overwhelmed.
This is often, but not always the most infective stage for the patient as well
decline
This is when the patient’s immune system or the effect of medications helps get rid of the
pathogen.
Fever and other signs go away.
Can still be quite sick from the aftereffects.
convalescence
Tissues are repaired and body function returns to normal.
Length depends upon the most of the same factors as in the incubation stage.
Note: You can be infective in every stage listed above. For some diseases you can even continue to be infective after you have recovered.
Contact transmission
contains direct contact, indirect contact, and droplet transmission
Vehicle transmissions
contains airborne, waterborne, foodborne, and bodily fluids
Vector transmission
contains biological vectors and mechanical vectors
direct contact
▪ Involves bodily contact between individuals
▪ Touching, kissing, sexual intercourse between humans
▪ Biting, scratching in zoonoses.
▪ Vertical transmission of disease via the placenta.
▪ Self-transmission – please look at the book
indirect contact
▪ Fomites – inanimate objects that transfer pathogens.
▪ E.g. – toothbrushes, toys, money, diapers, stethoscopes, contaminated needles, etc
droplet
▪ Droplets of mucus propelled out of the body by breathing, coughing, sneezing.
▪ This is for larger droplets that travel 1m or less.
airborne
Spread of droplets further than 1 m away.
▪ Aerosols – tiny droplets that can travel much further.
▪ Common ones – dental and surgical drills, improper flaming of loops in lab
waterborne
Water can act as a reservoir of infection as well as a vehicle.
▪ Fecal-oral route – any fecal contamination of food or utensils
foodborne
Pathogens on foods that are improperly stored, undercooked or improperly handled.
▪ It is usually another route of fecal-oral contamination
bodily fluids
Often considered under waterborne, but also can be direct contact.
▪ Blood, urine, feces, vaginal and seminal secretions.
▪ Should always be treated as if they contain pathogens
biological vectors
Usually caused by the bite of an arthropod vector (ticks, lice, mosquitos)
▪ Biological vectors often serve as important intermediate hosts for the life stages of certain
pathogens as well
mechanical vectors
Passively carry pathogens to new hosts on their feet or other body parts.
▪ Common examples include houseflies and cockroaches
Define epidemiology
The study of Where and When disease occurs and How it spreads through a population.
▪ Where – Place
▪ When – Time
▪ How – Person (who is affected, what are the reservoirs, modes of transmission)
Contrast incidence and prevalence
incidence: The number of new cases in a population in a given time period
prevalence: The total number of cases in a population in a given time period.
endemic
Disease found regularly in the population
sporadic
when only a few cases are found
epidemic
When there are more cases than statistically predicted or historically reported in a period.
▪ Observed versus expected cases
pandemic
An epidemic that spreads across multiple countries or continents, affecting a large portion of the global population.
endemic, sporadic, epidemic, and pandemic summarized
endemic, sporadic, epidemic, and pandemic
Explain three approaches epidemiologists use to study diseases in populations
Descriptive - Case studies, Case Reports
Analytical – Cross-sectional, Case-Control, Cohort
Experimental - Clinical Trials, Koch’s Postulates
Explain how healthcare-associated infections differ from other infections
Exogenous – picked up in a healthcare setting
Endogenous – opportunists because of treatment
Latrogenic – caused by things like catheters, surgery, wrong antibiotics
factors influencing: Presence of microbes in the hospital setting. Immunocompromised patients. Transmission of pathogens between staff, and patients
Describe the factors that influence the development of healthcare-associated infections
factors Influencing HAIs
▪ Presence of microbes in the hospital setting
▪ Immunocompromised patients
▪ Transmission of pathogens between staff, and patients
Describe three types of healthcare-associated infections and how they may be prevented.
Controlling HAIs
▪ All the things you can think of that would prevent spread.
▪ Ignatz Semmelweis was right!
▪ Handwashing protocols can reduce infection by more than 50%
specific immune response
Specific = Adaptive
▪ Every response is unique
▪ The second exposure to a pathogen garners a much faster response by the immune system
because it remembered the pathogen from previous encounters
non-specific immune response
Nonspecific = Innate
▪ Every response is the same
▪ IT HAS NO MEMORY
▪ Cannot differentiate between types of invasions, every pathogen is treated the same
what are the physical barriers of a non-specific immune response?
-Skin and mucous membranes, tears, coughing, sneezing etc.
▪ Acidic secretions from skin destroy pathogens.
▪ Stomach acid and enzymes kill microorganisms.
▪ Saliva and tears have lysozymes that destroy bacteria.
▪ Mucosa of the nose, throat etc. trap and expel pathogens.
▪ Overall function is to prevent entrance of pathogens into the body.
▪ Can be breached when the skin is broken
Chemical – how do these work, what are they effective against in non-specific immune responses?
These help destroy or inhibit microbes
target bacteria and viruses
some chemical barriers:
acidic pH, lysozome, sebum, mucus, defensins
complement system
non-specific immune response
a group of about 20 proteins when exposed to bacterial antigens.
Classical pathway: stimulation by antigen-antibody complex
Alternate pathway: stimulation by microorganism’s cell wall. Stimulated by factors C3 which break down into different components
interferons
non-specific immune response
protects body against viral attack
Virus infected cells produce interferon which stimulates neighboring cells to produce antiviral proteins
toll-like receptors (TLRs)
non-specific immune response
Trigger your body’s responses to a number of various bacterial and viral pathogens.
There are 10 different TLR’s found on human phagocytes.
Binding of Pathogen Associated Molecular Patterns (PAMP) triggers infected cells to do things like apoptosis, initiate the inflammatory mechanism, or stimulate the adaptive response
cells
non-specific immune system (primarily WBCs)
neutrophils, macrophages, basophils, mast cells, eosinophils, lymphocytes
Which type is first to enter the infected site?
Neutrophils are the first to arrive and are the most numerous WBCs in acute inflammation
Neutrophils
phagocytes – about 126 billion/day produced.
▪ Usually the first WBC to make it to an infection.
▪ 1 time use (like a honeybee stinger).
▪ Pus =dead neutrophils, microbes, pathogens
Macrophages
-monocytes in blood, macrophages in tissue.
▪ Leave blood and increase numbers at site of infection.
▪ They are the cleanup crew.
▪ Include many different types – dendritic cells, microglia, alveolar, hepatic
basophils
mobile
▪ Release factors which attract more WBC’s (chemotactic factors)
mast cells
nonmobile
▪ Are found near sites of possible pathogen influx
▪ Release chemotaxic factors
▪ Can also phagocytose bacteria
eosinophils
Act as moderators of inflammatory response and kill parasites by releasing enzymes all over them
Roles of Eosinophils and Basophils in Inflammation
eosinophils: Contribute to allergic reactions
basophils: Release histamine, which promotes vasodilation and increased permeability. Also contribute to allergic inflammation
vascular permeability
allows protein rich fluid to seep into the injured region from the blood vessels (called exudate)
(Blood vessels become leaky, allowing immune cells and proteins to exit into tissue. Helps deliver complement and antibodies.)
vasodilation
caused by the release of histamines, prostaglandins, etc. from the injured tissues. (Blood vessels widen (due to histamine, etc.). Increases blood flow, causing redness and heat.)
chemotaxis
Chemical signals attract immune cells (especially neutrophils and monocytes).
Gradient of cytokines/chemokines guides them to the site of infection.