Bio Sci 37 Midterm 2
1/202
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
203 Terms
Is dementia part of normal aging?
No —> dementia is characterized by multiple cognitive deficits with memory impairment as a frequent early symptom.
Most significant risk factor for Alzheimer’s Disease
Aging (also the leading cause of dementia)
What is normal aging?
trouble recalling people or places
forgetting appts or events occasionally
taking longer to process info
sometimes losing track of a convo
forgetting where item is occasionally
What are symptoms of dementia?
not remembering the names of close family or friends
frequently forgetting appts and events
trouble verbalizing thoughts, frequent pauses in convos, sub common words
regularly repeating statement or questions
consistently misplacing items
frequency confusion
unable to focus
becoming lost in familiar places
mood changes
The trajectories of age-related cognitive change
better than avg —> super aging
normal aging
mild cognitive impairment
***independent function in daily living***
abnormal aging —> dementia
***cannot function w/o assistance due to cognitive loss***
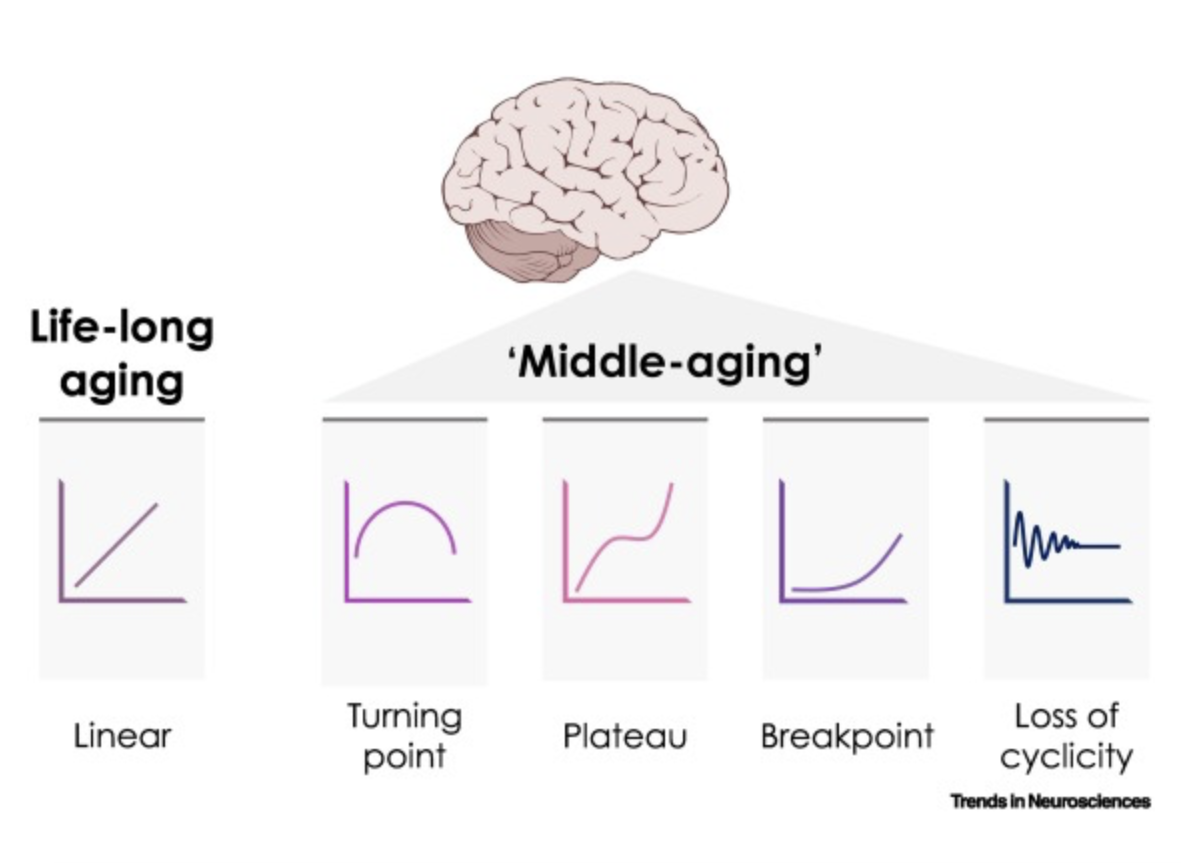
Middle Age
Represents period that shapes future cognitive trajectories and brain health —> brain aging comprises many process that change in different ways.
Does brain volume decrease with age?
Yes
gray matter decreases —> associated with reductions in neuronal number and/or volume
white matter decreases —> associated with reductions in the diameter of the myelin sheath
Synaptic Plasticity
Ability of synapses to strengthen or weaken in response to activity —> often associated with structural changes.
***greater when we are young
What does demyelination in normal aging do?
Contributes to age-related memory changes.
What are subtle cognitive decline in aging brains?
slower reaction times
lower attention levels
slower processing speeds
decreases sensory and perception function
changing in sleep pattern (less time in dream and deep sleep)
What is the number one factor that can improve the performance of ages individuals?
Exercise
What are factors that influence brain aging?
Genetics (eg. family history)
Environment (eg. levels of education)
8 hours of sleep per night (sleep activates healthy clearance mechanism —> removes toxins in brain)
Immune system, gut, vasculature —> communicate with brain and influences cognition
Neurogenesis
Process by which neurons are generated from neural stem cell (cells in the brain that divide) and progenitor cells —> responsible for populating the growing brain w/ neurons.
Adult Neurogenesis
Neurons are generated from adult stem cells.
Is neurogenesis restricted?
Yes
Where does neurogenesis occur?
hippocampus (subgranular zone) —> lead cells to repopulate the olfactory bulb (OB)
subventricular zone (SVZ) —> lead cells to repopulate the granular cell layer in dentate gyrus
Does neurogenesis slow aging?
Yes —> a bit unclear though regarding how it contributes to cognitive processes and aging.
Factors that affect neurogenesis?
environmental enrichment
exercise
neurodegenerative diseases
depression
aging
How to delay cognitive decline?
minimize stress —> decrease cortisol levels (stress hormone) which negatively impacts learning and memory
exercise —> aerobic
networking —> active social life
diet: omega 3 fatty acids, antioxidants, less sugar
higher education —> mental activity
Parabiosis
“Leaving beside” —> anatomical joining of two individuals artificially in physiological research
eg. joining young and old mouse together —> does this influence learning and memory for the old mouse?
What does parabiosis research show?
young blood reverses age-related impairments in cognitive function and synaptic plasticity in mice (young blood improves old subject performance)
aging systemic milieu negatively regulates neurogenesis and cognitive function (old blood impairs young subject performance)
human umbilical cord plasma proteins revitalize hippocampus function in aged mice (young human blood improves cognitive performance)
clinical trial finds blood-plasma infusions from young healthy donors is safe to AD patients
in a small trial, participants receiving blood plasma infusions from young donors showed some evidence of cognitive improvement
What is dementia?
Umbrella term —> abnormal part of aging —> many biological causes
Characterized by problems with:
thinking
language
memory
judgment
reasoning
These problems get in the way of daily living
What are activities of daily living?
Basic:
feeding
dressing
bathing
toileting
Instrumental:
transportation
taking medication
prepping meals
managing finances
What are diseases under dementia?
Alzheimer’s Disease
Frontotemporal Lobar Degeneration
Parkinson’s Disease-related Dementias
Progressive Supranuclear Palsy
Creutzfield Jacob Disease (Prion)
Huntington’s Disease
Dementia with Lewy bodies
Types of Brain Disorder
specific disorders (focal damage) —> depends on the area of the brain affected (where a bullet hits, strokes)
generalized disorders (widespread damage) —> affects multiple cognitive abilities (closed head injury, dementing disorders, demyelinating diseases, toxic substances)
Dementing Diseases
loss of cognitive function, sometimes accompanies by personality changes, which interfere significantly with the individual’s daily activities work and social activities
mild: retain judgment, sustain daily activities, but work and social activities are impaired
moderate: independent living = hazardous (eg. forgetting to turn off stove) and requires some supervision
severe: cognitive abilities are so compromised that constant supervision needed
Aphasia
Loss of ability to understand or express speech.
Apraxia
Inability to link skilled motor movements to ideas or representations (eg. I want to tie my shoes, but I physically cannot).
Agnosia
Deficit in recognizing objects that occurs in the absence of deficits in sensory processing (eg. see a cup and shoe —> cannot distinguish objects).
Acalculia
The inability to perform simple mathematic calculations the patient previously knew.
Types of Dementias —> clinical classification
cortical, subcortical, and mixed
Cortical
Co-occurence of many cognitive deficits (aphasia, apraxia, agnosia, acalculia, visuospatial deficits, and memory problems) —> eg. Alzheimer’s, frontotemporal dementias, Creutzfeldt-Jakob (prion diseases)
Subcortical
More likely to manifest first as personality changes, attention deficits, slowness in cognitive processing, difficulties w/ tasks requiring strategy —> eg. Parkinson’s, Huntington’s
Mixed
Both cortical and subcortical involvement, patterns of cognitive performance midway between cortical and subcortical types —> eg. Vascular dementia, Lewy body dementia
What is the molecular classification of dementia?
Accumulation of abnormal protein aggregates in neurons and glia and also in extracellular compartments, in vulnerable regions of the brain.
What neurodegenerative proteinopathies does non-vascular dementia fall into?
Amyloid-B (AB)
Microtubule-associated protein tau
TAR DNA-binding protein 43 (TDP-43)
Fused in sarcoma (FUS)
Alpha synclein
Prion protein
Alzheimer’s Disease
impaired memory
impairment in at least one other cognitive domain
impaires social or occupational functioning
gradual onset and continual decline
What is found in many neurodegenerative diseases?
Abnormal protein deposits/aggregates —> protein misfolding disorders.
What types of protein aggregates are associated with certain neurodegenerative diseases?
Alzheimer’s —> plagues and tangles
Huntington’s —> intranuclear inclusions
Parkinson’s —> lewy bodies
Prion —> amyloid plaques
Amyotrophic Lateral Sclerosis Aggregates
Are there genetic associations in Alzheimer’s Disease?
Yes —> if we know mutation is in “X” gene, then this will lead to this disease.
Mutations can be direct causes or increase risk of Alzheimer’s
***there are a lot of unknown mutations however (we do not know what caused the Alzheimer’s)
Is Alzheimer’s a public health issue?
Yes —> more women have Alzheimer’s, number of people age 65 and older with the disease is increasing through the years, very prevalent in California
Frontotemporal Dementia
No amnesia in early stages
Associated with shrinkage of frontal and temporal lobes
Impulsive, bored, listless
Inappropriate social behaviors (eg. hypersexual)
Neglect of personal hygiene
Repetitive or compulsive behavior
Speech problems, semantic deficits
What are the three types of frontotemporal dementia?
Behavioral-variant
Semantic dementia
Progressive nonfluent aphasia
Behavioral-variant frontotemporal dementia
changes in social conduct and behavior
loss of empathy
apathy
disinhibition
lack of insight
Semantic dementia
loss of semantic knowledge, impaired word comprehension, and object naming
fluent speech and spared repetition
Progressive nonfluent aphasia
apraxia and effortful speech
spared object knowledge and word comprehension
Dementia with Lewy Bodies
Lewy bodies (alpha synuclein neuronal inclusion bodies —> protein in Parkinson’s disease too)
similar to Alzheimer’s in terms of cognitive features
defining symptoms: bradykinesia, rigidity (like Parkinson’s), recurrent and well-formed hallucinations
memory deficits less severe than AD but visuospatial deficits are more sever than AD
Stages of Lewy Body Dementia
early: delusions, restlessness, REM sleep disorder, movement difficulties, urinary issues
middle: motor impairment, speech difficulty, decreased attention, paranoia, confusion
later: extreme muscle rigidity and speech difficulties, sensitivity to touch, susceptible to infections
Vascular Dementia (VAD)/Multi-Infarct Dementia (MID)
caused by blockages in brain’s blood supply (not by protein aggregates)
second most common form of dementia (1st = Alzheimer’s)
may cause or worsen Alzheimer’s (complicates diagnosis as vascular factors contribute to AD)
cognitive abilities more impaired than AD patients on executive function (planning, organizing, control impulses, achieve goals)
less impaired on episodic memory
What are the risk factors of Vascular Dementia?
high blood pressure (50% caused by hypertension)
diabetes
high cholesterol
family history of heart problems
obesity
smoking
Parkinson’s Disease
progressive neurologic disease
fourth most common neurodegenerative disease in elderly
neuropathology —> degeneration of dopamine (DA) producing neurons in the brain (substantially nigra)
motor symptoms
neuropsychiatric symptoms
What are the motor symptoms of Parkinson’s Disease?
tremor
bradykinesia (slow movement)
rigidity
What are the neuropsychiatric symptoms of Parkinson’s Disease?
executive dysfunction
memory deficits
attention deficits
visuospatial deficits
mood disturbances
impulse control behaviors (eg. food, drugs, gambling)
Are there trials for dementia?
Yes! —> drugs approved but have minimal effects.
What is preclinical cognitive decline?
silent phase —> brain changes without measurable symptoms
individual may notice changes but not detectable on tests
a stage where the patient knows but the doctor does not
What is mild cognitive impairment?
cognitive changes are of concern to individual and/or family
one or more cognitive domains impaired significantly
preserved activities of daily living
What is dementia (severe cognitive impairment)?
cognitive impairment severe enough to interfere with everyday activities
#1 Risk Factor of AD
age
What is Alzheimer’s Disease?
An irreversible and progressive neurodegenerative disorder characterized by a gradual loss of memory and other cognitive function, deficits in activities of daily living, behavior, personality and judgment. Accounts for the majority of dementia cases at 65 years of age or older.
destroys cognition, personality, and ability to function
What are symptoms of Alzheimer’s Disease?
memory loss
language deterioration
impaired ability to mentally manipulate visual info.
poor judgment
confusion
restlessness
mood swings
What are the early signs of AD?
forgetfulness
loss of concentration
***missed because they resemble natural signs of aging
Behavioral symptoms in AD?
very common
more distressing for caregivers than cognitive symptoms
overlapping clusters: depression, apathy, sleep, agitation, psychosis
others: anxiety, emotional lability, delusions, hallucinations, euphoria, irritability, aberrant motor behavior, appetite/EDs
Is AD fatal?
yes —> a person with AD will depend on others for complete care
progressive cerebral deterioration
bed ridden
dysphagia —> difficulty swallowing foods and liquids
failure to thrive
***the 6th leading cause of death in the US
Is AD insidious?
yes —> changes happen to the brain years prior, BEFORE symptoms show
What is mild cognitive impairment?
Memory and/or other cognitive problems that
are a source of complaint
demonstrable on cognitive tests
do NOT impair activities of daily living
do NOT meet criteria for dementia'
***general forgetfulness
Does mild cognitive impairment lead to dementia?
~12-16%/year progress to dementia
more frequently AD —> especially for those with memory problem or memory/other cognitive problems
risk is increased for those with supportive evidence of AD
still, up to 50% do not progress to dementia after 1- years
20% revert to normal cognition —> this group remains at an elevated risk for dementia however
What are the stages of AD?
Mild
recent memory loss
language impairment
faulty judgment
personality changes
Moderate
aggression (verbal and physical)
agitation
wandering
sleep disturbances
delusions
Severe
loss of all reasoning
bedridden
incontinent
What does AD do to neurons?
Disrupts the three essential functions of neurons
neurons must communicate with each other
carry out metabolism
repair themselves
Amyloid Plaques
insoluble extracellular deposits which accumulate in the cortex and hippocampus
composed of amyloid-beta (AB) protein fragments: AB40 and AB42
Neurofibrillary Tangles
bundles of insoluble helical fibers within neurons
composed of hyperphosphorylated tau proteins that are normally associated with microtubules
What does AD do to brain mass?
Since it causes an intensive loss of synaptic contacts and neurons, cortical atrophy occurs —> loss of 1/3 of brain mass
Cause of amyloid plaques?
incorrect cleavage
AB 42 cleave product of APP (amyloid precursor protein) —> produces toxic AB 42 cleavage product
in the cell membrane. B-secretase or y-secretase cleaves AB —> causes plaque aggregation
point mutations in the y-secretase gene can lead to early onset AD inherited in families in an autosomal dominant pattern
point mutations in the APP gene located on chromosome 21 can lead to early onset AD inherited in families in an autosomal dominant pattern
multiple fragments link —> now a plaque
How to fight against amyloid plaques?
find drugs that inhibit the secretase
antibodies against AB
sleep clears AB
What are the risk factors of AD?
age (80-90) = #1
genetics —> known genetic bases (APP, PS-1, PS-2) —> but mostly for early onset, familial AD
ApoE4 = reliably identified genetic risk factor for AD (does not mean if you have it you will get AD)
other genes —> MAPT (tau), SORL1, TREM2)
non-genetic factors have associated risks —> head trauma, high blood pressure, heart diesease, stroke, diabetes, high cholesterol
How is AD and Down Syndrome connected?
Individuals with Down syndrome are 3-5x more likely than the general population to develop AD —> onset of AD may be as early as 30 in the Down syndrome population (age 50 in general population).
duplications of a small part of chromosome 21 which includes the APP gene can cause early onset AD
Is there a protective APP mutation?
Yes —> whole genome sequencing on Icelandic population identified a FUNCTIONAL variant protecting against Alzheimer’s disease! —> will be a therapeutic target for AD
A673T —> prevents cleavage of APP and cognitive decline in the elderly
Amyloid cascade hypothesis
Missense mutations in APP —> accumulation of plaques —> cascade of damage and dysfunction in pathways —> dementia
What molecular pathways are involved in AD?
amyloid-beta (AB) pathway
tau protein pathology
calcium signaling
excitotoxicity
genetic factors, inflammation, oxidative stress play a role
What happens to the ventricles in the brain when a person has AD?
Enlarges as surrounding brain tissue shrinks due to neuronal loss and atrophy.
What do Tau proteins do?
Tau stabilizes MT in neurons (in axonal processes)
MT main functions —> structure, organize the cytoplasm, serve as tracks for the transport of cellular elements form the cell body to the axonal terminals (synapses)
What leads to neuroinflammation in AD?
microglia genes are activated by amyloid-beta deposition, leading to the release of pro-inflammatory cytokines and the recruitment of other immune cells.
microglia SHOULD clear out AB —> but when not regulated, causes problems
astrocytes are also activated by AB and contribute to inflammation
What are the modifiable risk factors of AD?
Social determinants, which primarily affects underserved and socioeconomically disadvantaged individuals.
How is mild cognitive impairment measured?
memory complaint corroborated by informant
measurable, greater-than-normal memory impairment detected with standard memory assessment tests
still has normal general thinking and reasoning skills
should have the ability to perform normal daily activities
several subtypes (the AMNESTIC subtype is more likely to process to AD)
Components of the AD evaluation
check clinical history —> largely dependent on informant
physical and neurological exams
lab tests
neuroimaging
structural (CT/MRI)
functional (PET)
neuropsychological assessment
Which of the following is characteristic of MCI?
memory loss
What does an ABC score depend on?
presence of AB plaques
What does BRAAK staging depend on?
neurofibillary tangles
How does imaging the AD brain work?
magnetic resonance imaging used
assesses brain atrophy
stage 1-2 —> entorhinal cortex is affected
stage 3-4 —> hippocampus, amygdala, parahippocampus
stage 5-6 —> neocortex
this loss corresponds with NFTs (tangles)
What type of metabolism is reduced in AD brains?
glucose metabolism
What does PET (position emission tomography) imaging show in AD?
Shows hypo metabolism compared to normal patients, in relevant brain areas.
***shows what is missing (such as the loss of glucose metabolism)
What does structural MRI show in AD?
Show amyloid plaque accumulation in the brain and structural changes associated with Alzheimer’s disease.
***shows what is added
How does amyloid PET imaging work to show plaques?
plaques directly imaged via amyloid tracers
other ligands FDA- approved —> amyvid, neuroceq, vizamyl
How does amyloid PET imaging work to show NFTs?
ligands bind to hyperphosphorylated tau aggregates found in NFTs
several ligands are in development that can highlight tau pathology
Why is AD a public health concern?
prevalence will increase as population ages
death from AD has increased
Why is AD an economic concern?
There are billions of dollars needed to care for people with AD.
Why is AD a social concern?
Caregivers face significant emotional and physical strain, impacting families, communities, and their jobs.
Why are biomarkers for AD important?
helpful for early diagnosis (which is IMPORTANT)
is this person progressing?
establishes a baseline
lets doctor know if a drug is working
Does cerebral spinal fluid help predict progression from MCI to AD?
Yes —> higher risk of progression to Alzheimer's disease because AB is released in CSF
Can AB be prevented?
no evidence for prevention yet
cognitive and psychological activities may reduce risk for AD
phase III prevention trial —> A4 Trial (concluded) (Anti-Amyloid Treatment in Asymptomatic AD)
targeting older adults with biomarkers for AD (eg. amyloid) but no symptoms of AD using an anti-amyloid agent to see if clearing amyloid prevents AD onset
Can exercise reduce the risk of AD?
yes —> physical activity linked to reduced risk for AD
small benefits in clinical trials (especially in executive function)
aerobic and strength training
sessions longer than 30 minutes show larger effects than shorter sessions
more studies needed!