Lecture 19: MHC Structure and Function (+ Natural Killer Cells)
1/8
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
9 Terms
Major Histocompatibility Complex (MHC)
also known as HLA (human leukocyte antigen) in humans
exists in many alternative (allelic) forms
most polymorphic genes found within our genome
MHC-I - expressed by all nucleated cells
humans express 3 ‘isotypes’: HLA-A, B, and C
MHC-II - expressed by antigen presenting cells (DC, B, monocytes, and macrophages
humans express 3 ‘isotypes’: HLA-DR, DP, and DQ
most important alleles to match in a transplant: HLA-A, HLA-B, and HLA DR genes
remember that humans are diploid so we have 12 genes (6 alleles total but 12 overall)
Polymorphism - presence of multiple variants of MHC genes
Polygeny - multiple genes contribute to MHC (allowing for diverse antigen presentation and immune response)
Polymorphism + Polygeny = all 12 alleles expressed all at once
ethnic based alleles give Europeans genetic advantage to transplant compared to ethnic minorities (like maori)
MHC structure
MHC-1 (~8-9 amino acids) (shorter, constricted on one end)
Heterodimer
alpha chain and beta2-microglobulin
one transmembrane region
polymorphisms on alpha 1 and alpha 2 subunits
MHC-2 (15-25 amino acids) (not constricted, longer)
heterodimer
alpha chain and beta chain
two transmembrane regions
Polymorphism on beta 1 subunit
Anchor Residues
anchors peptides into MHC structure
MHC-1
anchors short peptides
lock in certain amino acids
MHC-2
anchors (but not as much)
non-covalent binding
TCR recognition
the TCR recognizes MHC and peptide as a combined complex (the peptide on its own will not activate a T-cell, neither will an empty MHC
polymorphism determines how TCR binds to MHC-peptide complex
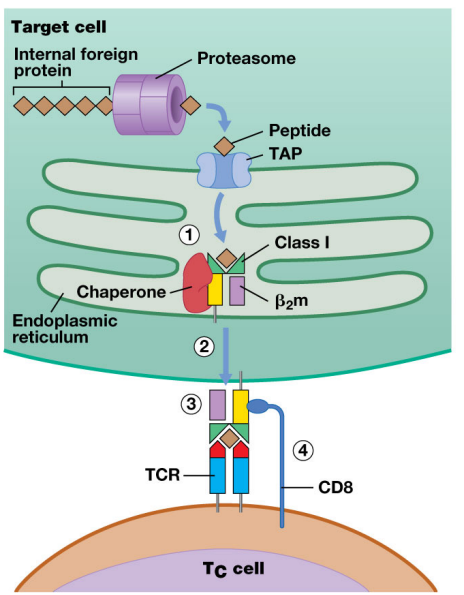
MHC class 1
displays endogenous antigen
recognized by TCR on CD8 T cells
allows CD8 to visualize what is happening in the cell of the MHC-1 receptor (intracellular infection)
almost exclusively self-peptide displayed
Presentation pathway:
foreign protein forced through proteasome, becomes peptide
peptide goes to ER
MHC-1 parts hanging out in ER (unstable)
Peptide binds to MHC-1 w/ help of chaperone protein making MHC-1 stable
MHC/peptide complex goes through secretory pathways and onto cell surface
the MHC complex has transmembrane domain which makes MHC stop at membrane and anchor at surface
CD8 T-cell activated by MHC complex and kills infected cells
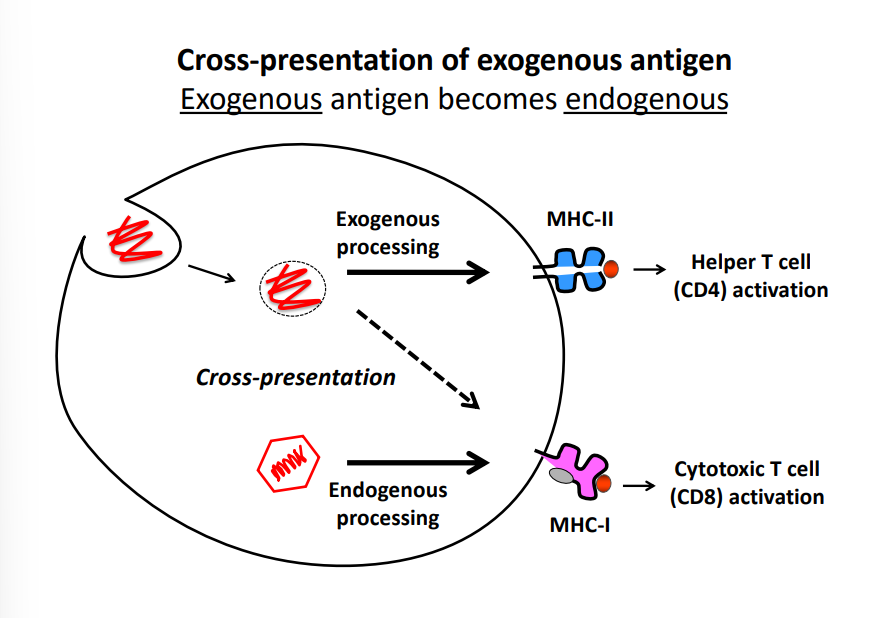
Cross presentation of exogenous antigen
occurs when exogeneous antigen becomes endogenous and is displayed on MHC1 instead of MHC2
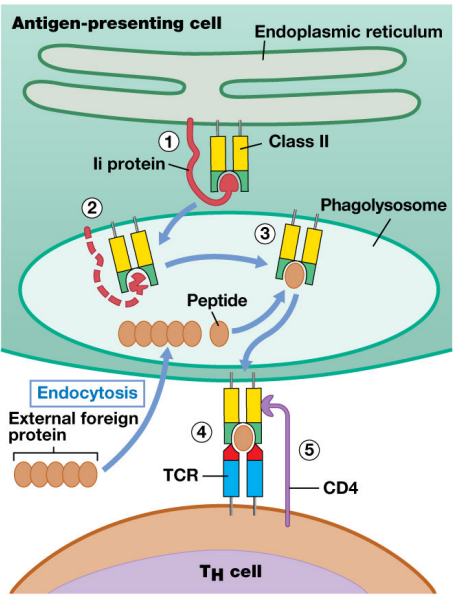
MHC class 2
antigen presentation pathway:
synthesized in ER
attached to MHC2 BUT also loaded with phagolysosome (very acidic and causes peptide degradation)
once stable brought to surface + binds w/ CD4 T cell
Superantigens
proteins produced by Gram + bacteria that interact with MHC2 and the TCR to induce massive T-cell activation
results in expansion of whole T cell receptor families of both CD4 and CD8 T cells (stimulate ~30% of CD4 and CD8 T cells)
T-cells quickly get worn out → organ failure
bacteria exploits the T-cell uncoordinated activity and invades isolated parts of body (results in vascular leakage which allows the microbe to disseminate)
can result in toxic shock
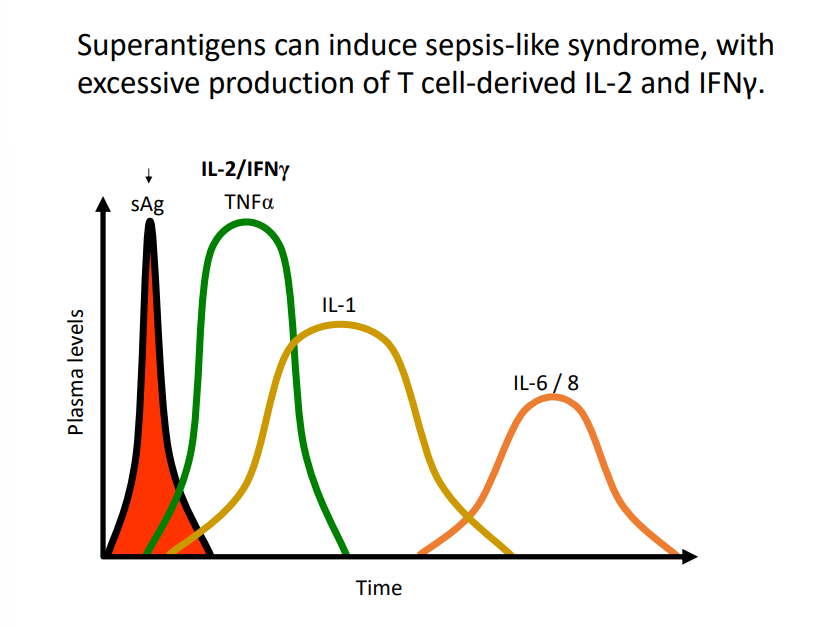
Pathway of Toxic shock
Local Inflammation - monocyte activation, endothelial cell activation, and complement activation (occurs in low quantities)
systemic effects - induces fever and acute-phase reactants in liver (occurs in moderate quantities)
Toxic Shock - low cardiac output, low peripheral resistance (high quantities)