Renal Exam Objectives
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
what does the proximal convoluted tubule do?
reabsorbs majority of K+ (potassium), Na+, & glucose
- while Cr, H+, NH4+ (ammonium) & toxins are filtered into tubular fluid from the blood stream
what happens at the Loop of Henle?
H2O is resorbed
what happens at the distal convoluted tubule?
- resorption of Na, Cl, & Mg
- PTH increases Ca2+ & phos secretion as well as Vit D production (which results in ↑ Ca2+/Vit D & ↓ phos)
what happens at the collecting duct?
if low intravascular volume is detected, hormones work to increase H2O resorption
what patient population should be screened annually for CKD?
HTN & DM
what labs should be used for CKD screening?
CMP (GFR) & UA (urine protein)
when, how & why wold you determine the fraction of excreted Na+ (FENa) level in a patient?
- when?
eval of AKI in pts w/o pre-existing CKD, who are NOT taking diuretics & have low urine output (<400 ml/24h)
- how?
(urine Na+ x plasma Cr)/(plasma Na+ x urine Cr)
- why?
to differentiate prerenal disease from acute tubular necrosis (ATN) which are the 2 most common causes of AKI
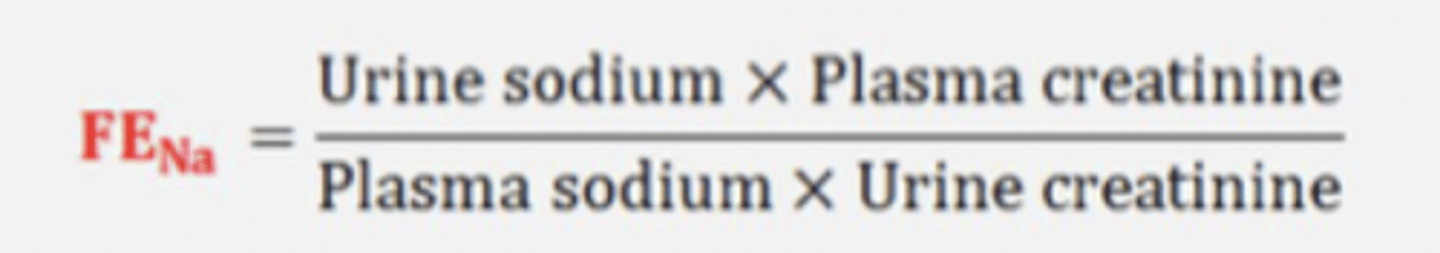
when would you determine the FENa level in a patient?
for eval of AKI in pts w/o pre-existing CKD
- who are NOT taking diuretics & have low urine output (<400 ml/24h)
low urine output = _______ ml/24h
<400 ml/24h
how is FENa calculated?
why would you determine the FENa level in a patient?
to differentiate pre-renal disease from acute tubular necrosis (ATN)
- which are the 2 most common causes of AKI
FENa <1% = _________ cause
prerenal
2 multiple choice options
FENa >2% = _________ cause
intrinsic
2 multiple choice options
when is the FENa level invalid?
- diuretics being taken
- normal urine output
what are the most common causes of AKI?
- pre renal diseases
- acute tubular necrosis (ATN)
common causes of pre-renal AKI
1. low blood flow to the kidney
- hypovolemia
- bilateral renal artery stenosis
- decreased circulating blood volume d/t low CO (CHF, sepsis) or liver failure
2. decreased perfusion pressure in glomeruli
- ↑ afferent arteriole vasoconstriction (NSAIDs, cyclosporine use)
- ↑ efferent arteriole vasodilation (ACE-I/ARB use)
how do the below listed things cause pre-renal AKI?
- hypovolemia
- bilateral renal artery stenosis
- low CO (CHF, sepsis) or liver failure
a. low blood flow to the kidney
b. decreased perfusion pressure in glomeruli
a. low blood flow to the kidney
NSAIDs & cyclosporine use may cause decreased perfusion pressure in the glomeruli, thereby causing pre-renal AKI by:
a. ↑ afferent arteriole vasoconstriction
b. ↑ efferent arteriole vasodilation
a. ↑ afferent arteriole vasoconstriction
ACE-I/ARB use may cause decreased perfusion pressure in the glomeruli, thereby causing pre-renal AKI by:
a. ↑ afferent arteriole vasoconstriction
b. ↑ efferent arteriole vasodilation
b. ↑ efferent arteriole vasodilation
what is the most common intrinsic cause of AKI?
ATN
what insults to the kidneys could result in acute tubular necrosis (ATN)?
- nephrotoxic meds (aminoglycosides, vancomycin, amphotericin B)
- contrast media (iodine-based IV contrast dye for imaging)
- myoglobin from rhabdomyolysis
- massive intravascular hemolysis
- hyperuricemia from chemotherapy (tumor lysis syndrome)
what are the diagnostic findings that support the diagnosis of ATN?
- hyperkalemia
- hyperphosphatemia
- BUN/Cr ratio < 20:1
- FEna >2%
- granular/muddy brown casts (renal tubular epithelial cells) on UA
common drugs that can cause acute interstitial nephritis (AIN):
CNP2RS
- cephalosporins
- NSAIDs
- PCN
- PPIs
- rifampin
- sulfa
what are the diagnostic findings that support the diagnosis of AIN?
- triad of: fever (80%), maculopapular rash (25-50%), & arthralgias
- eosinophilia (80%), eosinophiluria
- mild proteinuria, pyuria (95%), RBC & white casts on UA
- may require renal biopsy to diagnose
clinical manifestations of post-streptococcal glomerulonephritis (PSGN)
usually occurs 1-3 wks after a pharyngitis infection & between 3-6 wks after impetigo
- generalized edema due to low serum protein
- hypertension
- gross hematuria, resulting in urine looking smoky, & tea or cola-colored
what are the diagnostic findings that support the diagnosis of PSGN?
- mild proteinuria
- pyuria
- dysmorphic RBCs
- RBC casts on UA
- antistreptolysin-O (ASO) titer (60-80%)
s/s of nephrotic syndrome
- proteinuria > 3.5 g/d
- serum albumin < 3 mg/dL
- edema, often periorbital upon awakening & in ankles (due to profound hypoalbuminemia or sodium retention in renal tubules)
- hyperlipidemia (most commonly cholesterol & TGs) & lipiduria
- "frothy" appearing urine, fatty acid casts due to lipiduria
granular/muddy brown casts =
ATN
RBC or white casts, eosinophilia, fever, maculopapular rash, & arthralgias =
AIN
RBC casts, smoky/tea or cola colored urine =
PSGN
fatty acid casts & frothy appearing urine =
nephrotic syndrome
why should those w/ nephrotic syndrome be referred to nephrology for managment?
due to the many complications of the disease
causes of post-renal AKI
- benign prostatic hypertrophy (BPH)
- renal calculi (stone) obstructing ureter
- tumor or mass (prostate or cervical cancer)
- urethral strictures/phimosis
- blood clots, preventing urine from passing
clinical manifestations of post-renal AKI
- anuria/oliguria
- distended bladder
- pelvic discomfort
- +/- hematuria (in the cases of renal calculi or prostate cancer)
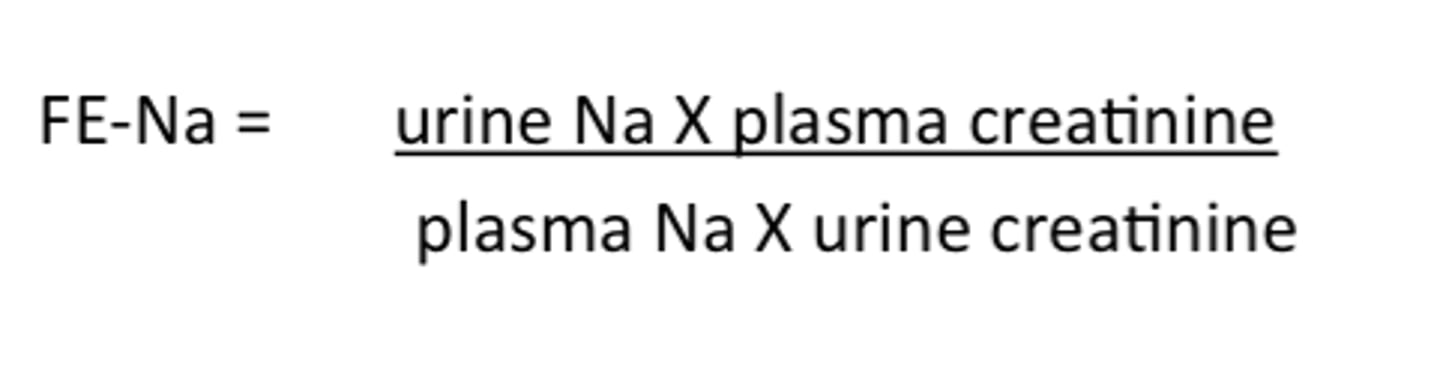
clinical manifestations of chronic kidney disease (CKD)
often asymptomatic in early stages
*uremic sx begin in later stages of 3-5
list some uremic symptoms which occur in later (3-5) stages of CKD:
- N/V, lack of appetite
- fatigue, weakness, malaise
- insomnia, sleep disturbance
- decreased mental sharpness
- edema (esp. pedal & periorbital)
- pruritus
- muscle wasting, muscle cramps, restless leg
- metallic taste
- easy bruising/ecchymosis
- unplanned weight loss or gain (from edema)
- oliguria
what is the eGFR in Stage 3 CKD?
30-59
what labs should a patient have done annually to monitor their CKD?
- CBC/Hgb (for stage 3, q 6mo for 4-5 & q 3 mo if on dialysis)
- CMP/BMP (cholesterol, BUN/Cr, eGFR, glucose)
- urine dipstick or UACR
indications for renal replacement therapy (dialysis)
Acidosis (pH < 7.1, refractory to tx)
Electrolytes (hyperkalemia or any other electrolytes, refractory to tx)
Intoxications/ingestions
Overload (refractory to diuretics)
Uremia (uremic bleeding)
what is the most common form of polycystic kidney disease (PKD)?
autosomal dominant PKD (ADPKD)
- only 1 parent has to have to pass on
characteristics of ADPKD
- cysts on other organs (liver, pancreas, spleen, thyroid, epididymis)
- colonic diverticula
- hernias (abdominal wall, inguinal)
- valvular heart disorders (mitral valve prolapse, aortic regurgitation)
- aneurysms (cerebral, coronary artery, aortic)
characteristics of autosomal recessive PKD (ARPKD)
often detected in utero/infancy by routine US
- sx occur shortly after birth or in childhood
- renal failure
- liver fibrosis
- portal HTN (affects hepatobiliary tract)
valvular heart disorders & cerebral aneurysms =
ADPKD
1 multiple choice option
sx occurring shortly after birth or in childhood, renal failure, liver fibrosis, &/or portal HTN =
ARPKD
1 multiple choice option
clinical manifestations of (either type of) PKD
- flank pain
- HTN
- hematuria
- proteinuria
what is the initial diagnostic imaging tool for PKD?
renal US
(& obtain detailed FH)
what finding on ultrasound is diagnostic for PKD?
3 or more cysts
- 15 to 39 y/o w/ 3 cysts
- 40 to 59 w/ 4 cysts (2 on each kidney)
- >60 y/o w/ 8+ cysts (4+ on each kidney)
what are the BP goals for young, healthy pts w/ lower eGFRs vs older pts w/ lower eGFRs?
- young healthy: < 110/75
- older: < 130/80
what is the BP goal for a young (18-50 y/o), healthy patient w/ a low eGFR?
< 110/75
what is the BP goal for an older patient w/ a low eGFR?
< 130/80
patient education for those w/ PKD
- maintain healthy weight & regular exercise
- avoid caffeine, alcohol & smoking (smoking cessation)
- take meds as prescribed
- minimize OTC meds
- monitor BP
- reduce stress
- signs of extra renal manifestations (heart disease, cerebral aneurysm, etc..)
causes of hyperkalemia
reduced excretion of K+ in urine (d/t variety of possibilities)
- adrenal insufficiency
- dehydration
- HF
- AKI/renal failure (including vasculitis)
- CKD
- meds: ACE/ARBs (& K+ sparing diuretics [spironolactone])
causes of hypocalcemia
- hypoparathyroidism
- vit D deficiency
- CKD
causes of hypernatremia vs hyponatremia
hyper:
- net water loss (burns, DI, excessive sweating)
- insufficient fluid intake (absent thirst response or unable to drink fluids)
- kidney causes are rare
hypo:
- fluid overload (aggressive IV fluid administration, HF, renal failure, cirrhosis)
- fluid & electrolyte depletion (diarrhea, vomiting, excessive diuretic use [thiazides])
- severe nephritis/nephrotic syndrome or SIADH
net water loss (d/t burns, DI, or excessive sweating),
or
insufficient fluid intake (d/t absent thirst response or inability to drink fluids),
may cause:
a. hypernatremia
b. hyponatremia
a. hypernatremia
fluid overload (d/t aggressive IV fluid admin, HF, renal failure, cirrhosis),
fluid/electrolyte depletion (d/t diarrhea, vomiting, excessive thiazide use),
SIADH,
or
severe nephritis/nephrotic syndrome,
may cause:
a. hypernatremia
b. hyponatremia
b. hyponatremia
which type of diuretic causes hyponatremia?
thiazides
which types of diuretics cause hypokalemia?
loops
(or thiazides)
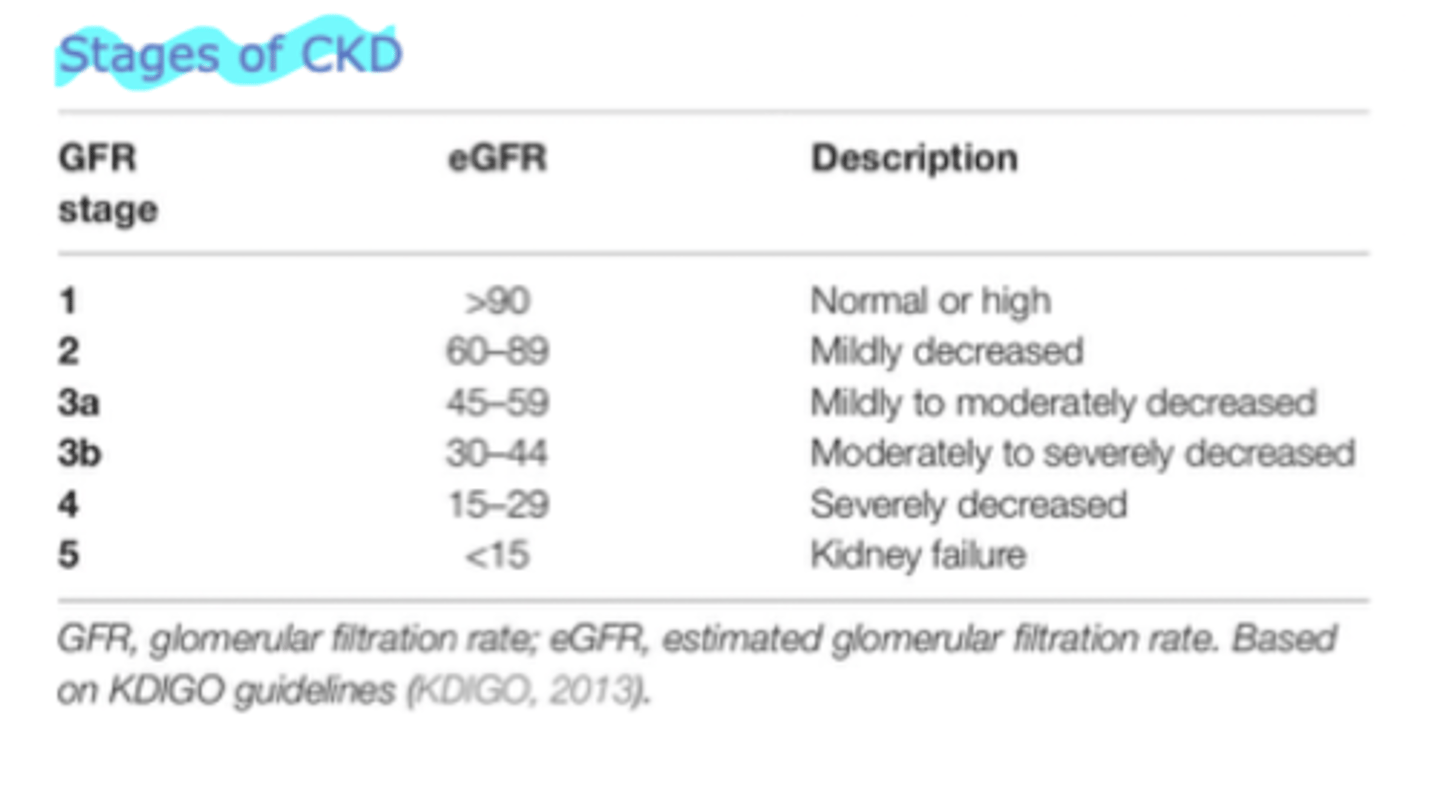
s/s of multiple myeloma (MM)
hyperCalcemia
Renal dysfunction
Anemia
Bone (lytic lesions, osteoporosis, pain)
what is the most common type of renal tubular acidosis (RTA)? where does it occur? what condition does it produce?
type 4 is the most common, but type 1 is also common
*where:
- type 4 is due to impaired aldosterone function in the distal tubule (& causes hyperkalemia)
- type 1 is where kidneys cannot properly acidify the urine (excrete H+) in the distal tubule
*condition:
- type 4 occurs in pts w/ diabetic nephropathy
- type 1 occurs in those w/ autoimmune diseases (SLE, sjogren's, RA)
**all types result in normal anion gap metabolic acidosis (NAGMA)**
what is the most common type of RTA?
type 4
where does type 4 RTA occur?
distal tubule
- d/t impaired aldosterone function
- causes hyperkalemia
- in pts w/ diabetic nephropathy
what condition do all types of RTA cause?
normal anion gap metabolic acidosis (NAGMA)
what are the most common causes of NAGMA?
- infectious diarrhea
- RTA
how is anion gap calculated?
Na - (Cl + HCO3)
if a patient presents w/ low bicarb & elevated chloride on CMP,
what should you do next?
measure the blood pH
- to confirm metabolic acidosis & anion gap
in RTA pts, the anion gap will be _______.
normal
2 multiple choice options
patient presents w/
low bicarb, elevated chloride on CMP, normal anion gap, &
denies diarrhea.
what diagnosis should you consider?
what lab will you order/assess next?
consider RTA
- assess urine pH
which is more likely if urine pH is >5.5?
a. type 1 RTA
b. type 4 RTA
a. type 1 RTA
1 multiple choice option
which is more likely if urine pH is <5.5?
a. type 1 RTA
b. type 4 RTA
b. type 4 RTA
1 multiple choice option
IgA nephropathy (Berger's vasculitis)
- usually in adults
- IgA deposits in kidney
- detected through gross microscopic hematuria, often w/ proteinuria
- commonly an accompanying respiratory infection
- HTN common
- definitive diagnosis through renal biopsy
- tx: ACE/ARBs, fish oil & steroids
IgA vasculitis (Henoch-Schonlein Purpura)
- usually in children
- IgA deposits in skin & kidney
- hematuria & possibly proteinuria
- can do biopsy of skin
- most cases resolve spontaneously, but recurrence is common
- steroids are NOT used (unless severe)
- tx: usually not indicated, but close f/u of kidney function is essential
granulomatosis w/ polyangitis (GPA, AKA Wegener's)
- associated w/ antineutrophil cytoplasmic autoantibodies (ANCA)
- s/s: fever, malaise, anorexia, & weight loss that can be slowly progressing
- multiple systems involved (nasal discharge, oral ulcers, sinusitis, cough, pleuritic pain, glomerulonephritis w/ hematuria & possibly proteinuria, focal necrosis & ulcerations of skin, eye pain, visual disturbance, etc)
usually occurs in adults,
IgA deposits in the kidneys, &
commonly occurs w/ an accompanying respiratory infection
IgA nephropathy
2 multiple choice options
usually occurs in children,
IgA deposits in skin & kidneys, &
tx is usually NOT indicated
IgA vasculitis
2 multiple choice options
associated w/ ANCA,
can have slowly progressing sx, &
multiple systems are involved
granulomatosis w/ polyangitis
2 multiple choice options
s/s of SIADH
euvolemic hyponatremia
- low urine output
- elevated urine Na+ (low serum Na+)
- low BUN
- nausea, malaise, HA, lethargy, disorientation
common risk factors for renal cell carcinoma
- HTN
- smoking
- obesity
- trichlorethylene exposure (which occurs w/ specific manufacturing jobs, mechanics, dry cleaners, & oil processors)
- inherited cancer susceptibility syndromes
- african american men
what is the most common solid renal tumor in children?
nephroblastoma (Wilm's tumor)
which chromosomal disorders have the highest incidence of horseshoe kidney?
- edward syndrome (67%)
- turner syndrome (14-20%)
what is renal colic?
kidney stone related pain
s/s of acute renal colic
- N/V
- malaise
- fever/chills
- diaphoresis
- cramping
- intermittent abdominal & flank pain, or pain in groin
- sudden onset severe pain
- pt unable to find comfortable position
what are the most common type of kidney stone in pregnant vs non-pregnant patients?
- pregnant: calcium phosphate
- non-pregnant: calcium oxalate
most common type of kidney stone in pregnant patients?
calcium phosphate
1 multiple choice option
most common type of kidney stone in non-pregnant patients?
calcium oxalate
1 multiple choice option
what are the 6 most common etiologies of microscopic hematuria?
- BPH
- medical renal disease
- UTI
- urinary calculi
- urethral stricture disease
- urologic malignancy
what is the treatment of choice for expulsive therapy of kidney stones?
alpha blockers
- ex: Tamsulosin or Doxazosin