Ch 84-88 + F Ch 19
1/406
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
407 Terms
Makeup of Extracellular Matrix of Tendons
Water - 65% wet weight
Collagen - 30% wet weight
Noncollagenous glycoproteins - 5% wet weight
Collagens and proteoglycans accounts for 70-80% of dry weight
What percentage of the total collagen in a tendon is made up of fibril-forming type I collagen?
About 95%
What percentage of the total collagen in a tendon is made up of type III collagen and other minor collagens?
About 5%
What is endotenon or the interfascicular matrix?
Looser connective tissue that groups collagen fibers in subunits
What are fascicles?
Collagen subunits
Structural hierarchy of the tendon from largest unit to smallest
Tendon unit surrounded by paratenon in extrasynovial locations and epitenon in synovial locations
Third-degree fascicle (1-3 mm diameter)
Second-degree fascicle (400- to 1000-um diameter)
First-degree fascicle (15- to 400-um diameter)
Collagen fiber (1- to 20-um diameter)
Collagen fibril (20- to 150-nm diameter)
Collagen triple helix (1-nm diameter)
Synthesis of Collagen Type I
Two identical a-1 chains and one a-2 chain are the molecular substructure for collagen formation Each chain contains around 1050 amino acids wound around one another in a left-handed triple helix Chains then self-assemble to form procollagen with a right-handed triple helical structure Extracellularly, amino- and carboxy-terminal extensions of procollagen are cleaved by procollagenases Resulting tropocollagen polymerizes to form a type I collagen fibril In fibrils, adjacent tropocollagen molecules are displaced from one another about 1/4 of their length (quarter stagger) Growth of the tendon occurs via a "seed-and-feed" mechanism, whereby collagen fibrils form extracellularly and accrete onto the sides of the template fibrils
What are the two classes of regulatory molecules involved in the regulation of linear and lateral fibril growth?
Small leucine-rich proteoglycans (SLRPs)
Fibril-associated collagens with interrupted triple helices (FACITs)
Small Leucine-Rich Proteoglycans (SLRPs)
Two subclasses
In the tendon, decorin (class 1) and fibromodulin (class 2) are dominant in regulation but can be modulated by biglycan (class 1) and lumican (class 2)
Fibril-Associated Collagens with Interrupted Triple Helices (FACITs)
Closely interact with the fibril-forming collagens and affect surface properties as well as fibril packing
FACITs XII and XIV may play a role during tendon development
Cartilage Oligomeric Matrix Protein (COMP)
Second most abundant protein in young tendon to collagen type I
Believed to be involved in the organization of the collagen fibril framework during formation and growth
Bring together five separate collagen molecules in the "quarter stagger" Once these collagen molecules have formed a fibril, COMP no longer functions in binding and is displaced from the collagen fibril
Levels of COMP in tensional regions of equine digital flexor tendons increase dramatically during growth an peak around 2 years of age
Extracellular Composition in the Mid-Substance (Tensional) Tendon
Collagen type I and the small proteoglycans (decorin, fibromodulin, lumican, and mimecan) predominate
Extracellular Composition in the Fibrocartilagenous Zone of the Tendon (e.g. DDFT at the level of the MCPJ/MTPJ)
Rich in collagen type II and the large proteoglycans (aggrecan and versican)
Reflects ability to cope with compressive load
Tenocytes
Constitute 90-95% of the cellular elements of the tendon
Essential for the formation and maintenance of the extracellular matrix
Exhibit long cytoplasmic processes which link together other tenocytes via gap junctions and thereby allow for communication between cells and appropriate responsiveness to mechanical stimuli
Type I Tenocytes
Thin, spindle-shaped nuclei
Type I cells predominate with aging
Type II Tenocytes
More rounded, thick, cigar-shaped nuclei
Less mature tendon has large numbers of type II cells
Type III Tenocytes
Cartilage-like appearance with round nuclei and visible nucleoli
Type III cells are identified in areas subjected to compressive forces (fibrocartilaginous zone)
What makes up the 5-10% of cellular elements of tendons that are not tenocytes?
Remaining 5-10% of cellular elements of tendons consists of chondrocytes at the bone attachment and insertion sites, synovial cells of the tendon sheaths, and vascular cells, including capillary endothelial cells and smooth muscle cells of arterioles
Endotenon (Interfascicular matrix)
Carries blood vessels and nerves
Contains more rounded cells which are believed to represent a source of multipotent stromal cells within the tendon
Contains higher levels of certain growth factors, such as TGF-B, than the content of the fascicles
Continuous with epitenon
Epitenon
Layer of connective tissue surrounding the outside of the tendon
Paratenon
Outside the epitenon around tendons that are not contained within a tendon sheath
Able to stretch considerably and therefore rarely ruptures when a tendon suffers a strain injury
Believed to play important roles in reducing frictional forces between the tendon and the surrounding soft tissues and as a supplier of new blood vessels and cellular elements for repair
Tendon Sheath
Consists of an outer fibrous wall and an inner synovial membrane
Mesotenons
Composed of two layers of synovium
Frequently carry the blood supply to the tendon
What are the two primary processes for nutrient supply of tendons?
Perfusion
Diffusion
Diffusion for Nutrient Supply of Tendons
Diffusion from compartments other than blood occurs primarily through the synovial fluid where the tendon is enclosed by a sheath
What are the three sources from which blood supply in tendons arises?
Proximal from the musculotendinous junction
Distal from the osseous insertion
In between through intra- and extratendinous vessels
Functional Characteristics of Positional Tendons
Flex, extend, or rotate joints
CDET (low-load positional tendon) and DDFT Lower levels of COMP Predominantly large collagen fibrils
Functional Characteristics of Weight- Bearing Tendons
E.g. flexor tendons, suspensory ligament
Located on the palmar/plantar aspect of the equine distal limb
Receive large weight bearing loads
More elastic
Function as elastic energy stores for energy efficient locomotion System optimized by hyperextended MCP and energy being stored in the SDFT and SL
Two weight bearing structures of the distal limb (SDFT and SL) have very similar matrix compositions and configurations High COMP levels Combination of small and large collagen fibrils
What is crimp?
Fascicle waveform in relaxed tendons
- Best seen under polarized light
- Partly responsible for tendon elasticity
Where does the majority of tendon elongation come from?
Majority of tendon elongation comes from the sliding of fascicles over one another rather than stretching of the fascicles themselves Endotenon believed to be critically important Rotational sliding in SDFT fascicles CDET fascicles slide linearly
Viscoelastic Properties of Tendons
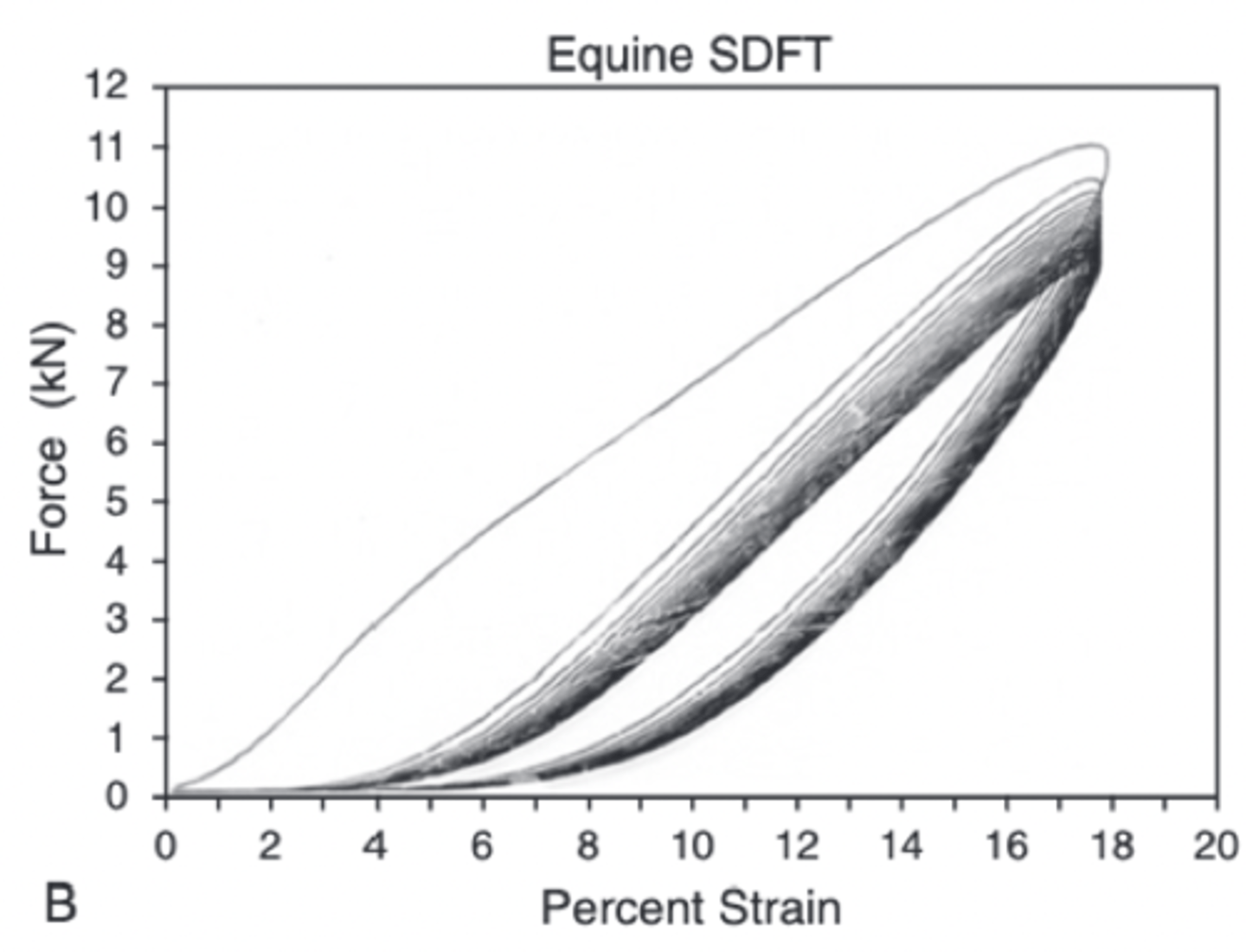
Initially tendon stretches under relatively little load which is associated with the elimination of crimp in the fascicles (toe region)
Then curve is almost linear (operating in elastic fashion) The structural property of stiffness (load divided by deformation) is divided from this area of the curve
As the load increases further, there is a change in the gradient such that the tendon becomes less stiff - yield point (end of the linear region) Thought to arise from covalent crosslink rupture and irreversible slippage of collagen fibrils
If the tendon is stretched past the yield point, irreversible damage occurs and the tendon ruptures For SDFT is ~ 12 KN or 1.2 tons (ultimate tensile strength)
If the cross-sectional area and length of the tendon is known, the stress (force/unit area) can be plotted against the strain (change in length over original length) from which the material properties of ultimate tensile strength (N/mm2) and Young's modulus of elasticity (E[Mpa]) can be calculated
In vitro, equine flexor tendons can extend 10-12% of their length before they rupture (ultimate tensile strength) and values of up to 20% have been reported
Ultimate tensile strain reflects only the final strain before rupture and includes the yield portion of the stress-strain curve, which represents irreversible damage to the tendon tissue
![<p>Initially tendon stretches under relatively little load which is associated with the elimination of crimp in the fascicles (toe region)</p><p>Then curve is almost linear (operating in elastic fashion) The structural property of stiffness (load divided by deformation) is divided from this area of the curve</p><p>As the load increases further, there is a change in the gradient such that the tendon becomes less stiff - yield point (end of the linear region) Thought to arise from covalent crosslink rupture and irreversible slippage of collagen fibrils</p><p>If the tendon is stretched past the yield point, irreversible damage occurs and the tendon ruptures For SDFT is ~ 12 KN or 1.2 tons (ultimate tensile strength)</p><p>If the cross-sectional area and length of the tendon is known, the stress (force/unit area) can be plotted against the strain (change in length over original length) from which the material properties of ultimate tensile strength (N/mm2) and Young's modulus of elasticity (E[Mpa]) can be calculated</p><p>In vitro, equine flexor tendons can extend 10-12% of their length before they rupture (ultimate tensile strength) and values of up to 20% have been reported</p><p>Ultimate tensile strain reflects only the final strain before rupture and includes the yield portion of the stress-strain curve, which represents irreversible damage to the tendon tissue</p>](https://knowt-user-attachments.s3.amazonaws.com/bb878276-0e66-41c5-806c-2a29d0583c06.image/png)
Normal Strains in Digital Flexor Tendons at the Walk
3-8%
Normal Strains in Digital Flexor Tendons at the Trot
7-10%
Normal Strains in Digital Flexor Tendons at the Gallop
12-16%
Hysteresis
Difference between the stress-strain relationship when the tendon is loaded and unloaded
Area between the two curves represents the energy lost during the loading cycle (usually about 5%) Much of this energy is lost as heat Core temperatures can rise to as high as 44 C which is potentially damaging to tendon matrix and tenocytes
Loading Rate of Tendons
Rapid loading rate = stiffer tendon
Repeated loading = less stiff tendon
- Conditioning
What are the two mechanisms by which overstrain injuries of tendons occurs?
Sudden overloading of the structure which overwhelms its resistive strength
Injury preceded by a phase of degeneration which induces neither a clinically evident inflammatory reaction nor any reparative response, but instead progressively weakens the tendon
Response of Tendons to Aging and Exercise
Strength of a tendon is correlated to the number and size of the collagen fibrils and intermolecular covalent crosslinks between fibrils Collagen fibrils increase in size during development and in response to increased physical demands or training The conversion of chemically reducible divalent crosslinks to a network of nonreducible trivalent crosslinks is thought to be responsible for a large proportion of this increase in the mechanical strength of tendons as they mature
SDFT and DDFT are mature by 2 years of age Replacement of immature collagen crosslinks with no further increase in collagen fibril size and the cessation of rapid changes in the collagen fibril crimp morphology
Collagen content varies little with age and exercise
A higher proportion of small fibrils were present in the central region of horses exercised long term Suggested to be due to disassembly of the larger diameter fibrils In longer term exercised and older horses, the noncollagenous component of tendon showed an accelerated loss of glycosaminoglycans (GAGs) and COMP
Additional exercise-accelerated degenerative changes that occur inevitably with aging Regional reduction of the collagen crimp angle and length in the central core of the tendon
Under loading conditions, central fibers are straightened first and are more likely to rupture first
What does cycling loading in tendons lead to?
Cyclical loading leads to cumulative fatigue and microdamage of the tendon matrix, with a failure of the resident cell population to repair this damage
What may be involved in the mechanism for the failure of tenocytes to repair or adapt to exercise-induced microdamage in adult horses?
Reduced cell numbers and gap junctions that would enable a coordinated anabolic response
Reduced growth factor stimulus
Cellular senescence
Mechanisms for Tendon Degeneration
Number of loading cycles important
Amount of time spent at the fastest gaits is likely to contribute the most to degeneration
Primary via physical damage
Secondary because of influences on cell metabolism
Physical energy imparted to the tendon under weight-bearing load can directly damage the matrix by disrupting fibers, crosslinks, or actual matrix proteins and can induce proteolytic enzymes
Cleaved matrix proteins, generated either from direct physical forces or from enzymatic cleavage, were associated with tendon damage and can provoke further matrix degradation
Physically induced microdamage of the extracellular matrix can also result in unloading of the damaged fibrils, which results in reduction in loading of the tenocytes
Increase in temperature in SDFT during galloping could be damaging to matrix proteins or cell metabolism
Strain-Induced Tendon Injury
Degeneration is usually the first phase of a tendinopathy
Clinical injury occurs when the highest stresses encountered by the tendon overwhelm its structural integrity, resulting in irreversible damage
Once the peak load on the tendon overcomes its structural strength there is physical disruption to the tendon matrix
Clinical injury varies from fibrillar slippage, with breakage of crosslinking elements, to fibrillar rupture, and in some cases, complete separation of tendon tissue
Damage induces a repair process characterized by inflammation followed by fibroplasia
Risk Factors for Inducing Tendinopathy
Things that act to increase the peak loads on the SDFT
Speed of the horse
Increased peak impact loading
Weight the horse is carrying
Shoeing
Fatigue
Tendon Tears
Most common sites are DDFT (mainly forelimb) and manica flexoria (mainly in the hindlimb) Higher pressures within the compressed portion of the DDFT as it passes over the palmar aspect of the MCP joint may cause bursting of the lateral (less commonly medial) borders of the tendon Manica tears may develop because it impacts against the proximal scutum within the fetlock canal when the fetlock overextends Highest compressive force on the DDFT in the foot occurs over the proximal border of the navicular bone so this is another common site for intrabursal tendon tears on the tendon's dorsal border in the forelimb
Percutaneous Tendon INjury
A tendon laceration usually requires the tendon to be taut during the impact
Phases of Tendon Repair
Acute Inflammatory Phase
Subacute Reparative or Fibroblastic Phase
Remodeling Phase
Acute Inflammatory Phase of Tendon Repair
Begins with the onset of clinical injury
Characterized by intertendinous hemorrhage, increased blood supply and edema, infiltration of leukocytes, initially neutrophils, followed by microphages and monocytes, and the release of proteolytic enzymes
Designed to remove damaged tendon tissue but thought to be excessive, further damaging the tendon
Lasts 1-2 weeks, but persists at a subclinical level
Subacute Reparative or Fibroblastic Phase of Tendon Repair
Begins a few days after onset of injury, overlaps with the inflammatory phase
Characterized by a strong angiogenic response and the accumulation of fibroblasts within the damaged tissue, which are responsible for synthesizing the scar tissue
Invading fibroblasts are larger and more basophilic and have large vesicular nuclei when compared to normal tenocytes More similar to myofibroblasts than tenocytes
Scar tissue has a higher collagen III content (20-30% compared to
Remodeling Phase of Tendon Repair
Reparative phase merges with the remodeling phase
Gradual but incomplete transformation to a higher proportion of type I collage as the scar tissue matures
New collagen fibrils become thicker, crosslinks increase in number and mature, and fiber alignment improves
Large amounts of fibrous tissue are laid down within and around the tendon, giving rise to a tendon that is persistently enlarged and strong but has greater structural stiffness Increase in stiffness reduces the efficiency of the tendon as a spring Increased stiffness results in increased strain rates in adjacent and relatively undamaged regions of the tendon which are then more prone to injury
Origin of Cells Involved in the Tendon Repair Process
Initially fibroblasts and inflammatory cells from the tendon periphery, blood vessels, and circulation are recruited to the injury site, thereby contributing to cellular infiltrate
Then intrinsic cells from the endotenon are activated as they migrate and proliferate at the injury site, recognizing the extracellular matrix and giving support to the internal vascular network
Growth Factors and Cytokines Involved in Tendon Healing
TGF-B
Basic fibroblast growth factor (bFGF/FGF2)
Insulin-like growth factor (IGF)-1
Vascular endothelial growth factor (VEGF)
Bone morphologic protein (BMP)
Growth and differentiation factor (GDF)
Epidermal growth factor (EGF)
Platelet-derived growth factor (PDGF)
TGF-B in Tendon Healing
Recruits fibroblasts and macrophages to the site of injury and induces increased proliferation, angiogenesis, and upregulation of MMP inhibitors and collagen expression as well as downregulation of proteinase activity
Connective tissue growth factor (CTGF) is a downstream mediator of TGF-B1 signaling and acts as a cofactor in fibrosis
Basic Fibroblast Growth Factor in Tendon Healing
Found in early wound healing
Has a role in fibroblast chemotaxis, proliferation, and angiogenesis
Epidermal Growth Factor in Tendon Healing
Role in regulating cell growth, proliferation, and differentiation
When is the optima baseline ultrasound for the severity of tendon injuries performed?
Approximately 1 week after the onset of injury
Ultrasonographic Characterization of Acute Tendon Pathology
Acute tendon pathology is characterized ultrasonographically by enlargement, hypoechogenicity (focal or generalized), reduced striated pattern in the longitudinal images, and changes in shape, margin, or position
Ultrasonographic Characterization of Chronic Tendinopathy
Chronic tendinopathy is associated with variable enlargement and echogenicity (often heterogenous and with retained echogenicity on off-incidence views when the transducer is tilted 5-10 degree), and an irregular striated pattern, which indicated fibrosis
Computerized Ultrasonographic Tissue Characterization (UTC)
A high-frequency ultrasonographic probe, fixed in a transverse position, is moved along the long axis of a tendon by a precision instrument at a constant speed
Contiguous transverse images are stored at real time and compounded in a 3D ultrasonographic data bloc
Additional Information Provided by Molecular Markers for Tendon Injury
May offer additional information over traditional clinical examination and imaging by providing
A diagnosis when other tests are negative
Screening as part of a preventative strategy; early detection may enable introduction of measures (e.g. altered training) to minimize the risk of a career-ending injury
An objective assessment of the severity of the pathology and therefore helping to determine prognosis
Staging of the disease process, optimizing rehabilitation protocols
Choices of treatment and an objective assessment of their efficacy
Molecular Markers for Tendon Injury
Initial investigations assessed markers of both collagen I synthesis (carboxy-terminal propeptide of type I collagen [PICP] and degradation (crosslinked carboxy-terminal telopeptide of type I collage [ICTP]) after tendon injury (Jackson, Smith, and Price, 2003)
Tendinopathy resulted in a significant rise in PICP concentrations, whereas ICTP concentrations were not different from those in the control group
Serum concentrations of PICP are able to reflect changes in type I collagen formation in healing connective tissue in one area of the body
Confirm that PICP is not an entirely bone-specific marker
COMP is another candidate marker because it is abundant in young flexor tendon
Synovial fluid levels were more than tenfold higher than serum levels and have been shown to be significantly elevated in the synovial fluid from the digital flexor tendon sheath in cases of intrathecal tendon and ligament tears
In older horses, increased levels of COMP within the DFTS synovial fluid appeared to be strongly suggestive of the presence of a tear even when there is no evidence of this ultrasonographically
Serum COMP levels were not significantly elevated with tendon disease because of the relatively high natural levels of COMP in blood
Clinical Characteristics of SDFT Strain-Induced Injuries
May be focal or generalized
One of the more common manifestations is a central region of injury ("core lesion")
Usually most severe level is centered just below the mid-metacarpal region, but frequently extends throughout most of the length of the metacarpal extrasynovial tendon and gives rise to swelling on the palmar aspect of the metacarpal region ("bowed" limb)
Regions of the SDFT enclosed with in a tendon sheath (carpal sheath proximally, tendon sheath distally) are much less often affected
Injury to branches of the SDFT in the pastern region results in abaxial swelling with pain on palpation and ultrasonography may be necessary to distinguish injuries of the oblique distal sesamoidean ligaments and palmar ligaments of the proximal interphalangeal region
Clinical Characteristics of Strain-Induced Injuries of the Accessory Ligament of the DDFT
May occur as an isolated injury or in conjunction with SDF tendinopathy
Lameness is often mild or absent
Swelling restricted to the proximal half of the palmar metacarpal region, immediately dorsal to the SDFT and is usually more evident laterally
Clinical Characteristics of DDFT Strain-Induced Injuries
Most frequently injured within the DFTS or navicular podotrochlear bursa
Clinical Characteristics of SDFT Lacerations
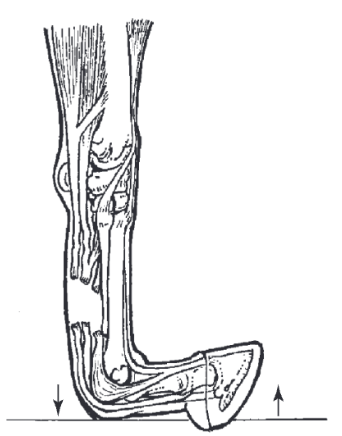
MCP/MTP joint is hyperextended (dropped) when limb is loaded

Clinical Characteristics of SDFT+DDFT Lacerations
MCP/MTP joint is hyperextended (dropped) when limb is loaded
Toe is raised from the ground
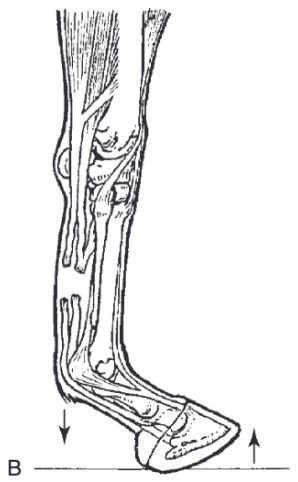
Clinical Characteristics of SDFT+DDFT+SL Lacerations
Complete loss of support of the MCP/MTP joint which is hyperextended to the extent that the MCP/MTP joint contacts the ground during the stance phase
Cold Therapy for Tendon and Ligament Injuries
Important in acute inflammatory phase
Antiinflammatory and analgesia, largely through ability to increase vasoconstriction, decrease enzymatic activity, reduce the formation of inflammatory mediators, and slow down nerve conduction
Recommended not to apply cold therapy for longer than 30 minutes as prolonged exposure to cold temperatures can cause a reflex vasodilation, which can accentuate tissue swelling and edema
Compression and Coaptation for Tendon and Ligament Injuries
In the acute phase of injury, pressure applied to the affected limb reduces inflammation and edema by increasing interstitial hydrostatic pressure
With severe injuries when there is hyperextension of the MCP joint, a palmar/plantar splint of cast can be applied or a specially designed support boot can be used
Shoeing for DDFT Injuries
Raising the heels reduces the tension in the DDFT (and ALDDFT)
Short-term management strategy for DDFT tendinopathy and desmitis of the ALDDFT because there is equilibration of forces in the supporting tendons and ligament in time and the heels need to be lowered at a later point to prevent heel collapse
Should be avoided for primary supporters of the MCP/MTP joint (SDFT and SL injuries) as the lowering of tension in the DDFT may increase loads in those structures
Shoeing for SL Injuries
Increasing the palmar/plantar support of the hoof with a shoe with an extended length or increased width at the heels or egg bar shoe is often advocated for SL desmopathy, but raising the toe or fitting the shoe with a wider width in the toe region so it sinks less than the heels in soft ground can also be considered
Controlled Exercise for Tendon and Ligament Injuries
Most SDFT, DDFT, and collateral ligament of the DIPJ injuries require up to 12 months of rehabilitation before resumption of full athletic function but some require up to 18 months
SL desmitis can usually be rehabilitated within 6-9 months
ALDDFT injuries can usually be rehabilitated within 3 months
Increase in tendon CSA of greater than 10% between examinations suggests a degree of reinjury and the exercise level should be reduced
In 28 Thoroughbred racehorses with SDFT tendinopathy 71% with a controlled exercise program returned to racing compared with only 25% managed with uncontrolled turnout (Gillis, 1997)
Extracorporeal Shock Wave Therapy for Tendon and Ligament Injuries
Mechanism of action is unclear but is most likely related to induction of analgesia through an effect on sensory nerves
Investigation of ECSWT as a treatment for chronic SL desmopathy resulted in 41% of hind limb patients returning to full work within 6 months of diagnosis (Crowe et al, 2004) compared with the previously reported 13% for conservatively managed cases (Dyson, 1994)
Therapeutic Ultrasound for Tendon and Ligament Injuries
Thought that the main effect of ultrasound is conversion of sound energy into thermal energy
In experimentally split equine tendons, therapeutic ultrasound resulted in increased vascularization and fibroblastic proliferation compared with controls (Morcos and Aswad, 1978)
Therapeutic Laser for Tendon and Ligament Injury
Low-level laser therapy has been shown to stimulate cellular metabolism and to enhance fibroblast proliferation and collagen synthesis in vitro (Henninger, 1994)
Counter-Irritation for Tendon and Ligament Injury
Studies have shown that there are no histologic differences between the collagen arrangement in the scar in cases of tendinopathy treated with firing and that of the controls (Silver et al, 1983)
Firing is not an effective treatment for tendon and ligament injuries
When can intralesional treatment be considered for tendon and ligament injuries?
Intralesional treatment should not be administered until 3 days after the injury because there is potential to increase hemorrhage
Intralesional Medication for Tendon and Ligament Injury - PSGAGs
Inhibit collagenases and metalloproteinases and inhibit macrophage activation
Have no effect on fibroblast synthesis
Viewed as a soft tissue antiinflammatory agent
In one study, treatment with PSGAGs either intramuscularly or intralesionally resulted in 76% of horses returning to work versus 46% of control animals, although these results were not stastically significant (Marr et al, 1993)
Another study demonstrated improved echogenicity of collagenase-induced superficial digital flexor tendinopathy treated with intralesional PSGAGs with faster resolution of core lesion (Redding, Booth, and Pool, 1992)
Another study demonstrated no significant difference in reinjury rates between horses treated with PSGAGs and those treated with controlled exercise alone (Dyson, 2004)
Intralesional Medication for Tendon and Ligament Injury - HA
Consists of repeating units of D-glucuronic acid and repeating units of N-acetyl-D-glucosamine and is a component of tendon matrix
Study showed no significant difference between the reinjury rates of horses with a superficial digital flexor tendinopathy treated with intralesional HA and those treated conservatively (Dyson, 2004)
In a study of collagenase-induced digital flexor tendinopathy, HA was found to minimize tendon enlargement compared with controls, although histopathologic examination of the tendons failed to demonstrate a significant difference in the degree of inflammation (Gift, Gaughan, and DeBowes, 1992)
Peritendinous HA has been shown to have no effect on ultrasonographic or histologic appearance, biomechanical properties, or molecular composition of tendons in collagenase-induced tendinopathy compared with controls, although it did appear to reduce lameness
HA has been shown to decrease the extent of adhesions when administered intrathecally to treat collagenase-induced DDF tendinopathy within the digital sheath
Horses treated with intrathecal HA showed decreased inflammatory cell infiltrate and less intratendinous hemorrhage than controls
Intralesional Medication for Tendon and Ligament Injury - Methylprednisolone
Methylprednisolone injected into and around normal equine tendons has been shown to cause dystrophic tissue mineralization and tissue necrosis
IGF-1 for Tendon and Ligament Injury
Stimulates extracellular tendon matrix synthesis and is a potent mitogen
In collagenase-induced models of tendinopathy, initial swelling was decreased after intralesional injections of IGF-1 compared with controls, although no differences were found at later time points and there was no difference between the quantities of type I and type III collagen synthesized
In a study assessing the efficacy of IGF-1 in natural disease, there appeared to be no significant benefits over other treatments
rEGH for Tendon and Ligament Injury
rEGH administered intramuscularly has demonstrated a negative effect on some of the biomechanical properties (decreased yield point and ultimate tensile strength) of the SDFT during the early phases of healing in collagenase-induced tendinopathy, although elasticity was maintained
TGF-B for Tendon and Ligament Injury
Horses treated with TGF-B1 showed significant enlargement of the tendon and although reinjury rates were similar to those in conservatively managed horses, these reinjuries were all on contralateral, untreated limbs
PRP for Tendon and Ligament Injury
Has been demonstrated to enhance the expression of collagen genes 1A and 3A and COMP in equine SDFT explants with no associated increase in MMP3 or MMP13
In a randomized, prospective clinical trial on a limited number of naturally occurring superficial digital flexor tendinopathies, a single intralesional PRP treatment contributed to an earlier reduction of lameness and to an advanced organization of the repair tissue compared with intralesional saline injection as a control (Geburek et al, 2016)
ACS (IRAP) for Tendon and Ligament Injury
A study found no significant difference in GAG, COMP, or type I collagen between normal equine serum and ACS treated tendon explants (Dahlgren and Harvey, 2008)
A clinical trial in horses with acute tendinopathies of the SDFT revealed a significantly faster reduction of lameness and a temporary improvement of ultrasonographic parameters in the ACS-treated group compared with controls (Geburek et al, 2015)
A cases series of 272 horses treated with ACS for proximal suspensory desmopathy reported a high success rate combined with a shortened convalescence period, but only included cases with no or only minor fiber disruption, and provided no control group (Easter and Watts, 2014)
MSCs for Tendon and LIgament Injury
Standard cell dosages for the treatment of a SDFT core lesion are ~50 million for minimally manipulated preparations and !20 million for culture preparations and these are delivered intralesionally
Using scintigraphy, the distribution of hexamethyl propylene amine oxime (HMPAO) and Tc99m labeled allogenic bone marrow-derived MSCs after intraarterial (median artery) and intravenous (cephalic vein) regional limb perfusion was evaluated in healthy horses (Sole et al, 2012)
In contrast to intravenous RLP, distribution of labeled MSCs through the entire distal limb was achieved with intraarterial RLPS but severe arterial thrombosis occurred in 1/6 horses
Median persistence of MSCs was 39% and 28% at 6 hours and 29% and 16% at 24 hours following intraarterial and intravenous injection, respectively
Utilizing the same technique in experimentally induced lesions (Sole et al, 2013) and in naturally occurring injuries (Becerra et al, 2013), similar levels of cell retention of only 24% after 24 hours following intralesional treatment were observed in both studies
In naturally occurring injuries, focal uptake was evident at the site of injury in all horses after intralesional injection of labeled cells, with 4/13 horses displaying diffuse or focal uptake of radiopharmaceutical within the lung field immediately after implantation
Immediately after IVRLP, focal uptake at the site of injury was evident in 75% of horses
Cell retention was only 32% and 9% at 12 hours after intralesional injection and RLP, respectively
Stem cell-treated racehorses showed a 50% reduction in reinjury rate compared with historical controls selected and followed up in identical fashion
Indications and Contraindications for Tendon Splitting
Not recommended for chronic cases due to extensive granulation tissue formation, increased trauma to the tendon tissue, and persistent lameness after treatment
Some advocate use for management of acute cases when there is an anechoic core lesion in order to decompress the core lesion by evacuating the serum or hemorrhage and to facilitate vascular ingrowth. Removal of the fluid in the core lesion may also reduce proximodistal propagation of the lesion
In a collagenase-induced model of tendinopathy in six horses, tendon splitting using the knife technique resulted in faster resolution of the core lesion and quicker revascularization of the lesion, and increased collagen deposition compared with untreated controls (Henninger, Bramlage, and Bailey, 1992)
Tendon Splitting Technique
Can be performed under standing sedation or general anesthesia
Can be done blindly or using ultrasonographic guidance which reduces damage to nromal tendon tissue
#11 scalpel blade or double-edged blade is inserted into the tendon and "fanned" proximad and distad
The procedure can also be achieved with multiple insertions of a 23-gauge needle, possibly with less damage to the remaining, relatively intact tendon tissue
After tendon splitting has been performed, a modified Robert Jones bandage should be applied and the horse rested in a stall for 10-14 days, after which a slow progressing exercise program should be initiated
Goal of Desmotomy of the Accessory Ligament of the SDFT
First described as treatment for SDFT tendinopathy
Aim is to produce a functionally longer musculotendinous unit to reduce strain on the SDFT
Transected accessory ligament heals within 60 days but measures approximately 2 cm longer than preoperatively
Has been shown in equine cadaver models that DALSDFT actually increases the strain on the SDFT during loading because of increased extension of the MCP joint
Increased risk of injury of the SL after DALSDFT has also been demonstrated in vivo
A recent retrospective published positive results with 69% of Thoroughbred racehorses with SDFT tendinopathy treated by DALSDFT returning to racing (Hu and Bramlage, 2014)
70% raced more than five times after surgery
Horses older than 4 years were significantly less likely to return to racing than younger horses
Desmotomy of the Accessory Ligament of the SDFT Technique
Can be performed via an open medial approach or tenoscopically through the carpal sheath
Horse in dorsal or lateral recumbency
Affected limb partially flexed, carpal sheath distended
Tenoscopic portal into the carpal sheath created 2-3 cm proximal to the distal radial physis on the lateral side of the limb between the ulnaris lateralis and lateral digital extensor muscles
Instrument portal is made immediately proximal to the distal radial physis
Probe used to palpate the distal and proximal limit of the subsynovially located accessory ligament which is transected directly over the flexor carpi radialis tendon using a #10 scalpel blade on a long handle, menisectomy knife, or a tenotomy knife
The very proximal portion of the ligament cannot be visualized directly because it extends proximad to the synovial reflection of the carpal sheath
For the proximal portion, careful dissection using punch biopsy forceps is needed, taking care to avoid the perforating blood vessel at the proximal limit of the accessory ligament
Transection can also be performed using electrosurgical instruments such as loop-headed or hook-headed monopolar electrodes or bipolar radiofrequency probes
Main benefit is reduction of intrathecal hemorrhage
Desmotomy or Desmectomy of the Accessory Ligament of the DDFT
Conservative management of accessory ligament of the DDFT (ALDDFT) desmopathy is usually successful
In some cases desmopathy recurs or causes adhesions between the ALDDFT and the SDFT which can result in a flexural deformity
In these cases desmotomy or desmectomy may be considered
Open approach or less invasive techniques which utilize either ultrasonographic guided transection of the ALDDFT or a tenoscopic technique, utilizing a distomedial approach into the carpal sheath at the level of the junction between the middle and proximal third of MCIII and a contralateral instrument portal and the same level
Palmar/Plantar Annular Ligament Desmotomy Indications
PAL desmotomy is indicated when there is a relative constriction of the PAL in the DFTS, impeding the normal gliding function of the flexor tendons causing lameness that does not respond to conservative management
Logical to only transect the PAL if it is causing a clinical problem as second-look arthroscopies have identified adhesions to the site of the PAL transection, but a recent study revealed a trend for improved outcome if PAL desmotomy was performed in addition to tenoscopic debridement
Best performed tenoscopically to assess the digital sheath for primary pathology but can also be achieved via an open approach or a limited open incision
Open Approach for Palmar/Plantar Annular Ligament Desmotomy
Performed under general anesthesia in lateral recumbency
Paramedian skin incision extends over the entire length of the PAL slightly abaxially to the palmar/plantar midline
Dissection through the subcutaneous tissue is directed towards the palmar/plantar midline to allow transection of the PAL at the level of the mesotenon and division of adhesions if required
Routine closure of subcutis and skin
Disadvantages: need for general anesthesia and risk of wound dehiscence, with potential further complications such as septic tenosynovitis
Limited Open Approach for for Palmar/Plantar Annular Ligament Desmotomy
Where only the PAL is affected, the limited open approach can be used
1-2 cm long skin incision at the proximal border of the PAL and transection of the ligament with a curved bistoury or a scalpel blade guided by a curved instrument or a groove director
Can be performed in the standing animal but does not allow resection of adhesions or comprehensive assessment of the DFTS
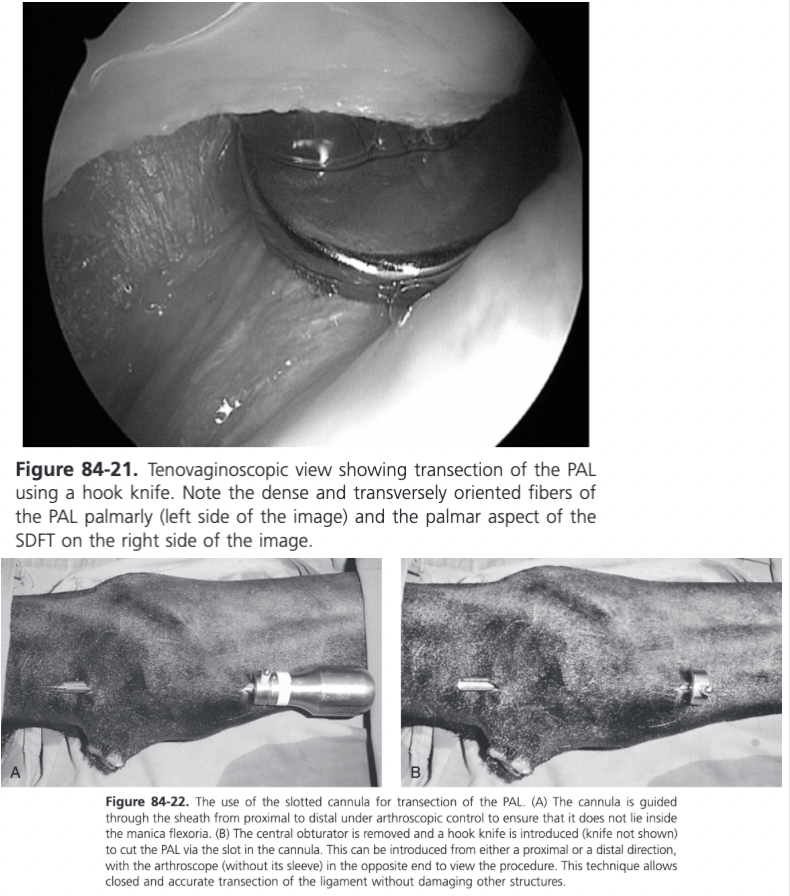
Tenoscopic Transection of the Palmar/Plantar Annular Ligament
Preferred because it is less traumatic, ensure accurate transection of only the PAL, and allows evaluation of the tendons to identify any primary causes
Performed via standard tenoscopic approach and is most easily performed using a hooked knife introduced via a proximal portal and guided to the distal end of the PAL under tenoscopic control to ensure it does not pass through the manica flexoria
Can also be performed using a slotted cannula by introducing the cannula through a proximal instrument portal and passing it out of the scope portal
A radiofrequency probe can also be used which allows precise transection and reduces hemorrhage
Indications for Digital Flexor Tendon Sheath Tenoscopy
The DDFT is more commonly affected than the SDFT in the forelimb, whereas tears to the manica flexoria of the SDFT are more frequently found in the hind limbs
Intrathecal tears of the DDFT are most commonly directed longitudinally and located at the periphery of the tendon, usually laterally
A survey further specified that most DDFT tears are long (>7 cm), extending from the proximal aspect of the DFTS distally to the PAL, and superficial (<5 mm deep)
On study showed 63% sensitivity and 75% specificity of ultrasonography to identify longitudinal tears of the flexor tendons in the DFTS (Arensburg et al, 2011)
Contrast radiography has a sensitivity of 96% to detect tears of the manica flexoria and sensitivity of 57% to find marginal tears of the DDFT. The specificity for both types of lesions is approximately 80%
Tears of the manica flexoria are most commonly located at the medial attachment of the manica flexoria to the SDFT
Standard tenoscopic portal is located slightly palmar/plantar of the center of the outpouching between the PAL and the proximal digital annular ligament, adjacent and palmar/plantar to the neurovascular bundle, and just distal to the PAL
All tears of the manica flexoria should be treated by complete tenoscopic resection, since debridement has been associated with poor outcome
Tenoscopic Resection of the Manica Flexoria
PAL desmotomy can be performed first if necessary for ease of movement of surgical instruments
In the lateral recumbency approach where portals need to be created ipsilaterally, the lateral border of the MF is transected first using a #12 scalpel blade or 14 gauge needled inserted through a second instrument portal located laterally at the level of the distal end of the manica flexoria, between the DDFT and SDFT
A third instrument portal is created in the proximal part of the DFTS to introduce a rongeur to grasp the distal and lateral edge of the manica flexoria and apply tension which rolls the SDFT medially and allows resection of the medial border of the manica flexoria dorsad to the DDFT using arthroscopic scissors, a hook knife, 14 gauge needle, or biopsy punch instruments
When in dorsal recumbency, the manica flexoria can be severed from its attachment to the SDFT on each side of the limb using a hook knife introduced via biaxial proximal instrument portals, ensuring the blade is introduced under the manica flexoria (so the hook knife points abaxially to avoid iatrogenic damage to the DDFT) and is aligned in the same plane as the border of the SDFT
The manica flexoria is withdrawn from one of the proximal instrument portals having transected the remaining synovial attachments to its proximal border
Digital Flexor Tendon Sheath Tenoscopy Aftercare
Horse should be rested for at least 2 weeks after which handwalking can be started at 5 minutes/day, increasing by 5 minutes/week for at least 6 weeks
Digital Flexor Tendon Sheath Tenoscopy Prognosis
Prognosis for a successful outcome defined as soundness and return to previous level of activity is better for patients treated with tenoscopic removal of the manica flexoria (~80% success rate) than for tears of the flexor tendons (~40% success rate)
Digital Flexor Tendon Sheath Synoviocoeles
Not all synoviocoeles are significant, the ones that do not decompress when the limb is lifted are more likely to be significant
If significant, can be resected via an open approach and the defect in the DFTS carefully sutured to avoid recurrence or have also been successfully treated by enlarging the opening to the synoviocoele using a synovial resector
Approach to the Carpal Sheath
Horse in dorsal or lateral recumbency
Affected limb partially flexed, carpal sheath distended
Tenoscopic portal into the carpal sheath created 2-3 cm proximal to the distal radial physis on the lateral side of the limb between the ulnaris lateralis and lateral digital extensor muscles