Chapter 93: Third Metacarpal and Metatarsal Bones
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
45 Terms
Anatomy of MCIII and MTIII
MC/MT II and IV are often termed vestigial, but both MCII and MTII have major weight bearing functions and MCIV and MTIV serve as sites for important carpal and tarsal ligamentous insertions
MTIII is slightly longer and typically more round in cross section than MCIII
The cross section of MCIII changes dramatically in response to increased loading as the horse ages and trains
Little soft tissue coverage of MCIII/MTIII except for their palmar/plantar aspects where the superficial and deep digital flexor tendons, accessory (check) ligament of the deep digital flexor, and the suspensory (interosseous) ligament are located
The soft tissues in the proximal palmar/plantar metacarpal and metatarsal regions are invested in a retinacular sheath
Where does the suspensory ligament originate?
In a broad attachment on the proximal palmar/plantar aspect of MCIII/MTIII
Major Neurovascular Structures Surrounding MCIII
In the forelimb, the major neurovascular structures course along the length of the MCIII both medially and laterally just dorsal to the flexor tendons
Major Neurovascular Structures Surrounding MTIII
In the hindlimb, the great metatarsal (dorsal MTIII) artery's location between MTIII and MTIV make it particularly vulnerable to accidental or surgical injury
Lateral Condylar Fractures
Vertical fractures in the sagittal plane occur in the distal condyle of MCIII/MTIII
Predominantly in young racehorses either during fast work or a race
In Thoroughbreds, MCIII fractures are at least twice as common as MTIII fractures but in Standardbreds, the ratio of forelimb to hindlimb fractures is nearly equal
Fractures involving the right MCIII are more likely to be displaced than those in the left
Nearly all propagate from the mid- to midaxial portion of the lateral condyle for a few centimeters in the sagittal plane and then proximolaterally toward the lateral cortex
Typical fracture breaks out 1-3 cm above the physeal scar
Lateral Condylar Fractures Clinical Signs
May have a history of MCP/MTP lameness preceding the onset of a more severe lameness, however the most typical presentation is an acute onset of severe lameness after intense exercise or a race
Horses with bilateral forelimb condylar fractures will present with a short, choppy gait
What percentage of all condylar fractures involve the lateral condyle?
~85%
How many times more common are lateral condylar fractures than medial condylar fractures in the forelimbs? In the hindlimbs?
7 times more common in the forelimbs
3-4 times more common in the hindlimbs
Treatment of Unicortical Lateral Condylar Fractures
Majority of unicortical fractures are managed conservatively with stall confinement for 2-4 weeks followed by stall confinement with increasing amounts of hand walking over the next 4-8 weeks
Screw fixation applying lag technique can also be performed under general anesthesia or standing sedation
Prognosis for return to racing is excellent (>90%) however recurrence was reported in 5/30 horses treated conservatively
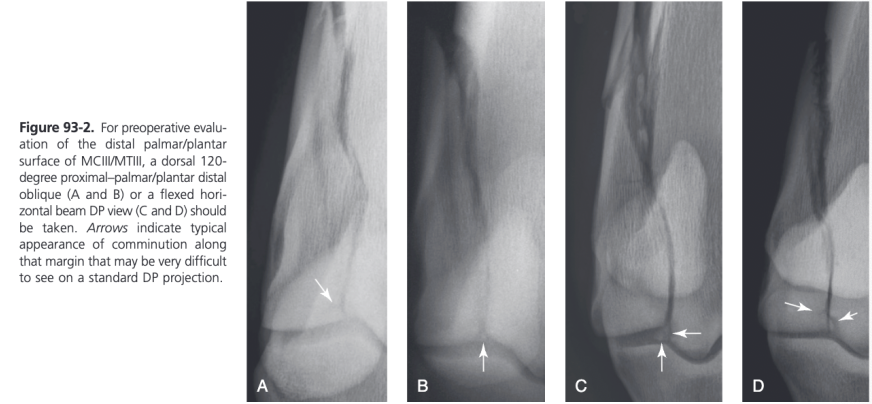
Diagnosis of Lateral Condylar Fractures
Many horses have preexisting degenerative disease involving the distal palmar/plantar condyle adjacent to the base of the ispsilateral proximal sesamoid bone so an additional radiographic projection further defining this region should be taken
Silhouetting of the distal palmar/plantar condyle can be obtained in slight flexion with the beam angled proximally or by putting the joint in more flexion with the limb pulled forward and using a horizontal beam
Should be used in all displaced condylar fractures because comminution along the fracture line is commonly identified in this location
Lateral Condylar Fractures - First Aid
Compression bandaging, NSAIDs, and absolute rest until definitive therapy is undertaking
Cost of casting not warranted because very few lateral condylar fractures propagate if the horse is kept quiet in a heavy bandage
Splints and boots not indicated
Lateral Condylar Fractures - Surgical Management
Involves compression of the fracture with cortex screws applied in lag fashion
Screws prevent proximal propagation of the fracture and enhance articular healing
Condylar fractures can heal successfully without internal fixation and a conservative approach is reasonable in nondisplaced fractures, especially where there are economic limitations or planned retirement from athletic activity
Majority of lateral condylar fractures can be treated with two screws
Little evidence to suggest placing a third or fourth screw in the longer fractures results in a better outcome, particularly in nondisplaced fractures
Unless there is a strong economic reason not to do so, arthroscopic examination of the dorsal and palmar/plantar joint should be done to confirm fracture reduction and characterize preexisting or fracture associated cartilage damage at the time of surgery
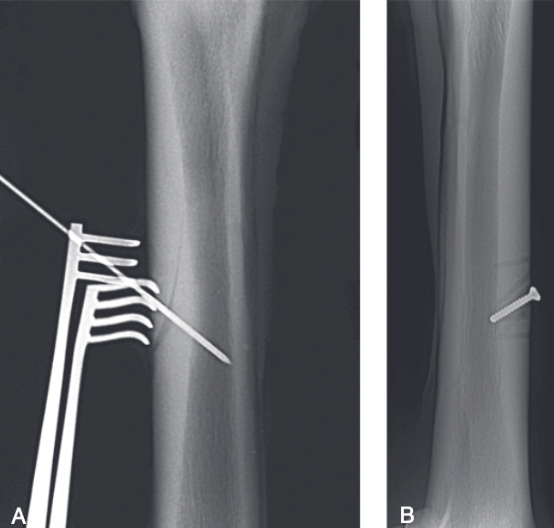
Surgical Management of Nondisplaced Lateral Condylar Fracutres
Repaired with screws applied in lag fashion using minimal soft tissue dissection
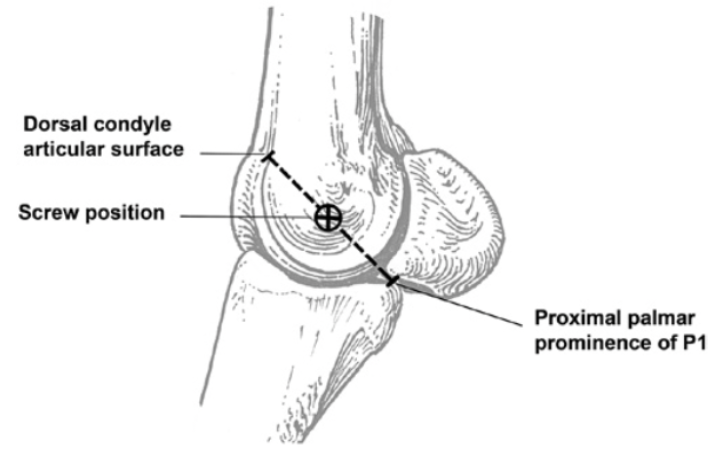
Distal screw is usually placed as centrally as possible in the lateral condylar (epicondylar) fossa
This site can be accurately estimated by taking the midpoint of an imaginary line drawn between the proximal palmar/plantar prominence of the proximal phalanx and the most dorsal aspect of the lateral condyle
A more distally and/or palmarly/plantarly placed screw may be used for short, incomplete, or unicortical fractures to achieve maximal compression across an incomplete fracture plane
Stab incision is made down to the surface of the bone in this location and parallel with the collateral ligament fibers to minimize injury to them
Can feel scalpel slide into the fossa, confirming accurate placement of the incision
As many additional screws as needed are placed at 15-20 mm intervals more proximad
Placing a screw too close to the proximal end of the fracture increases the risk of splitting the tapering end of the fragment or entering a fracture line and does not significantly contribute to the outcome of the case
Either 4.5 or 5.5 mm cortex screws can be used
Screw failure is rarely a problem in nondisplaced non comminuted fractures
4.5 mm screws have the advantage of being replaceable with a larger cortex screw if the bone thread are stripped
Standing Repair of Nondisplaced Lateral Condylar Fractures
Local anesthesia at the level of the proximal MCIII/MTIII should be administered with generous volumes over the major nerves as well as performing a subcutaneous dorsal ring block
Large sterile drape encircling the foot and a sterile area for the surgeon to kneel
Holding the leg in a partial or non-weight bearing position may facilitate the final tightening of the most distal screw, however adequate reduction is easily achieved in the weight-bearing position
Reported complications: fracture propagation with catastrophic refracture, and breaking of drill bits
Most Common Technical Errors During Repair of Nondisplaced Lateral Condylar Fractures
Most common technical errors: inadequate compression and incorrect drill/screw placement
Inadequate compression can be avoided by drilling the thread hole fully through the far cortex and being certain to completely tap the far cortex
Chances of incorrect proximal to distal aiming of the drill can be minimized by predraping positioning of the fractured bone parallel to the ground
Most horses have some degree of external rotation of the limb (especially hindlimbs) when they are in lateral recumbency so must account for this or the drill will be directed toward the palmar/plantar articular surfaces
Palpation of the medial and lateral wings of the proximal phalanx provides a good topographical key for the surgeon to direct the drill in a true lateral to medial direction
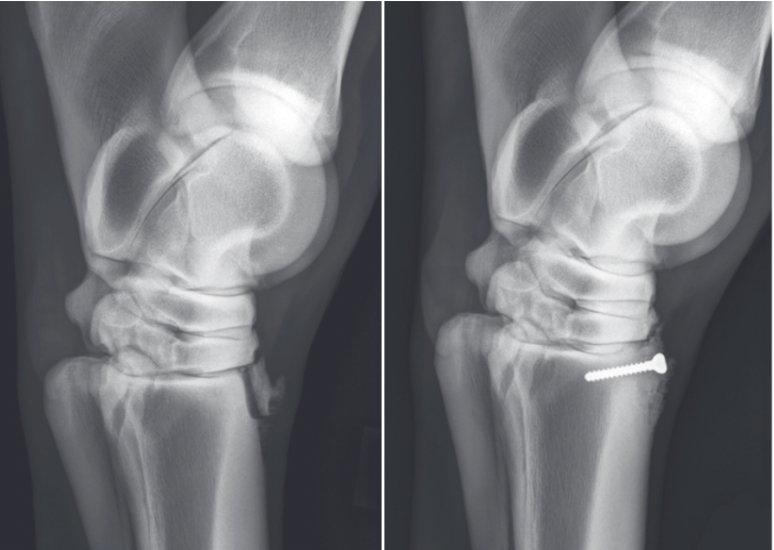
Displaced Lateral Condylar Fractures
Complete radiographic obliteration of the entire fracture line does not always occur, even with accurate reduction and screw placement and correct technique
Due to fibrin lodged within the fracture plane or bone loss along the margins
If the articular surfaces are aligned, the horse has a good chance to heal with minimal articular change
A significant malalignment of the condyle puts very high bending and shear loads on the screws that may lead to failure of the implants
Majority of displaced lateral condylar fractures can be successfully treated with two distal screws, one in the epicondylar fossa and another 18-20 mm proximal to it
More severe and displaced condylar fractures require more stability so 5.5 mm screws should be considered or placing three 4.5 mm screws in a triangular pattern within the condyle can also increase the strength of the repair
Repair of Displaced Lateral Condylar Fractures
Best technique is a by a combination of arthroscopic and fluoroscopic/radiographic guidance
4.5 mm glide hole prepared through the fracture fragment using radiographic/fluoroscopic guidance
Fracture doesn't need to be reduced when this is done, if the fracture is displaced, its easier to feel the 4.5 mm drill enter the fracture plane
Assures proper lag effect and allows freedom to accurately manipulate the fragment into perfect reduction
Insert drill sleeve and a 3 mm pin are placed in the fragment to use as a "handle"
Arthroscope introduced into the proximal dorsolateral joint pouch
MCP/MTP joint flexed, extended, rotated, and valgus/varus stresses can be applied until articular alignment is perfect
When reduction is judged perfect, the large pointed reduction forceps (second pair can be very helpful) are firmly tightened and the remainder of the screw insertion procedure is completed, screw not fully tightened
Arthroscope repositioned and articular compression and alignment are checked as the screw is firmly tightened
Palmar/plantar aspect of the joint is then examined arthroscopically
Many comminuted fragments at the distal margin of the MCIII/MTIII are immobilized by compression of the major fragment
If there are loose fragments they can be removed arthroscopically
Instrument portal must be carefully positioned at the base of the lateral proximal sesamoid bone and instruments with angled ends are invaluable
Treatment if Displaced Lateral Condylar Fracture Fragment Cannot Be Aligned Properly
Occasionally the fragment cannot be aligned properly because of interposed comminuted fragments
Pin and insert sleeve can be used to displace the main fragment laterally, allowing insertion of the arthroscope and cannula into the fracture plane
Dorsal instrument portal positioned exactly over the fracture plane so an instrument can be inserted through the fracture plane to retrieve the palmar/plantar fragment
Rarely necessary
Treatment of Displaced Lateral Condylar Fractures if Arthroscopy Not Possible
If arthroscope reduction is not feasible, displaced fractures should have enough of the fracture line exposed through an open approach to allow verification of accurate reduction
In some cases, a 2-3 cm incision over the proximal tip of the condylar fragment
In rare instances, may mean a longitudinal arthrotomy along the dorsal fracture plane extending nearly to the proximal phalanx
In many horses, accurate reduction seems to get more difficult as the exposure is increased
Injury of the Proximal Sesamoid Bones Associated with Lateral Condylar Fractures
Injury of the proximal sesamoid bones is often associated with lateral condylar fractures
Most involves varying degrees of erosions of articular cartilage
Axial proximal sesamoid bone fractures are complications of displaced condylar fractures and occur in approximately 4% of fractures
Should be identified preoperatively because associated with a very poor prognosis
If present the condylar fracture should be repaired with the understanding the horse has virtually no chance of becoming an athlete or resuming athletic activities
With large displaced fractures, the fragment can be fixed with one or two 3.5 mm cortex screws, but primary fetlock arthrodesis may be a better option
Medial Condylar Fractures
Seen in both forelimb and hindlimb of racehorses
Typically develop severe lameness immediately after exercise or are lame a few hours afterward
Rarely significant soft tissue swelling unless there is displacement of the fracture
Nearly always propagate toward the axial aspect of MCIII/MTIII, either spiraling up the diaphysis with the fracture line in the dorsal cortex traveling medially in most fractures, or remaining nearly sagittal to the mid-diaphysis where oblique fractures can later develop
Particularly prone to catastrophic failure with or without screw fixation, especially when the horse stands after anesthesia
Risk extends for several weeks after repair
First air and coaptation doesn't differ much from lateral fractures except that horses with medial condylar fractures in the hindlimb should be crosstied until surgery is performed
Treatment of Medial Condylar Fractures
Plating techniques are probably the most consistently successful technique
Screws alone are not optimal for any fracture with a known oblique diaphyseal component, especially in a hindlimb
When there is not an option for controlled anesthetic recovery (pool or sling), standing screw fixation of the distal portion of the fracture has been shown to be a reasonably successful option
Open Approach for Repair of Medial Condylar Fractures
Plate and screws can be placed from either medial or lateral side but lateral approach has advantages
Operated limb is uppermost and a lateral plate is easier to remove under local anesthesia in the standing horse after the fracture has healed
Dorsolateral or dorsomedial incision made in one layer down to the level of the bone surface
Periosteum may be elevated to expose the surface of the bone so the fracture line or lines can be clearly identified
Incision is continued distad to the level of the joint capsule but the capsule is not incised
Distal two screws placed through stab incisions using radiographic control, similar to nondisplaced lateral condylar fractures
Broad DCP or LCP is positioned on the lateral aspect of the bone extending from just above the second screw to the most proximal portion of the bone
Typically 10-12 hole plates in MCIII and 12-14 hole plates in MTIII
Can spirally contour the plate if the specific configuration of the fracture is evident but a straight plate can usually be safely applied in nondisplaced fractures
Exposure of the diaphyseal bone surface allows accurate placement of additional screws across the fracture plane and centrally within the fracture fragment
4.5 or 5.5 mm cortex screws used
Inadvertent injury to the suspensory ligament, splint bones, or both can occur
Obliquely directed screws or DP directed screws are drilled with care
If special recovery systems are not available, a full-length hindlimb case should be considered for metatarsal fractures
Forelimb medial condylar fractures are usually recovered in a full-limb Robert Jones bandage

Minimally Invasive Approach for Repair of Medial Condylar Fractures
Particularly straightforward if there is no obvious proximal spiraling of the fracture
2 cm incision made adjacent to the common digital extensor tendon at the level of proximal MCIII/MTIII
A broad DCP with a sharpened end attached to a handle can be used to prepare a subcutaneous tunnel for the plate
A roughly contoured 10 or 12 hole broad 4.5/5.0 mm LCP is slid down along the bone
Plate is recontoured as needed and replaced
Stab incisions made over holes and screws inserted routinely
Push-pull device or cortex screw can be used to pull the plate down to the bone
After two screws are inserted, a plate of the same length is placed on the surface of the skin and incisions are made through that plate's holes
Remaining screws inserted
Distal few screws in the plate may be placed in lag fashion if the fracture plane is radiographically visible at that level
Specific cautions - avoid the contralateral MCII/MTII with the drill bits and screws, difficulty in accurately measuring the depth of holes, ensuring that the drill guides are accurately threaded into the plate, need to check carefully that each screw is fully inserted into the plate
Aftercare Following Medial Condylar Fracture Repair
Stall rest with strictly controlled exercise for at least 2 months
Some turnout in a small paddock allowed in the 3rd moth
Usually return to regular exercise in 4th-5th month
Displaced fractures or those with articular comminution are rested longer
Average time from surgery to first racing start is approximately 11 months
Most horses do not have screws removed after repair of typical fractures
When fractures extend into the middiaphyseal region, screws are more likely to cause pain when horses return to intensive exercise so diaphyseal screws are removed 3-4 months after surgery, usually with the horse under sedation and local anesthesia
After screw removal horse is continued in a walking and jogging program for 60-90 days before returning to galloping exercise
Plates should be removed in horses expected to return to athletic pursuits
Plate Removal Following Medial Condylar Fracture Repair
Performed with the horse standing under sedation and local anesthesia
Medial condylar fracture plates are typically removed 70-80 days after surgery
Short incision made over proximal 2 cm of the plate
Most proximal screw partially removed
Matching bone plate placed on the skin along the plate and stab incisions are made through its hole
Each screw is backed out above the skin edge but not removed
Battery-powered drill with the screwdriver attachment is quieter and easier to use in a standing horse
12 mm osteotome used to pry plate up at proximal end
Plate grasped with sterile vise grips and extracted proximally
Horse handwalked for 60 days, receives paddock turnout for another month, then returns gradually to training
Condylar Fractures - Prognosis
Prognosis for condylar fractures is favorable (80-80% return to full function) if there is minimal preexisting OA and the fracture is not displaced
Displacement requiring open reduction lessens the prognosis considerably
Prognosis for displaced lateral condylar fracture of MCIII is about 50% for return to racing, less if there is serious comminution or sesamoid injury
Lateral condylar fractures of MTIII have a better prognosis than those of MCIII
Prognosis for medial fractures is more variable and depends on development of catastrophic complications
Only 40% of horses with medial condylar fractures repaired with DCP fixation were reported to return to racing
Transverse Fractures of the Distal Diaphysis of the Third Metacarpal Bone
Rare in Thoroughbred racehorses but occur with some frequency in Arabian endurance horses
Only reported in the forelimbs
Likely caused by a stress or fatigue injury
Approximately 40% occur bilaterally
Lameness usually acute and severe with periarticular swelling of the MCPJ and pain on manipulation of the region
Nonsurgical Management of Transverse Fractures of the Distal Diaphysis of the Third Metacarpal Bone
Viable option in less severe cases
Half-limb bandages applied to decrease swelling and pain
Painful or unstable horses can be managed in a cast, bandage cast, or Kimzey splint
Strict stall confinement for 6-12 weeks followed by another 4 weeks of stall confinement and hand walking
Catastrophic failure is a possibility
Surgical Management of Transverse Fractures of the Distal Diaphysis of the Third Metacarpal Bone
Required in moderate to severe cases
In horses with displacement of the distal epiphysis, surgery should be performed within 24 hours of injury to prevent necrosis of the epiphyseal component
Distal transverse fractures are difficult to repair because of the short segment of distal bone available for screw purchase
Arthrodesis of the MCPJ with cortex screws placed in lag fashion from the distal diaphysis to the epiphysis recommended
Variable angle LCP curved condylar plate applied to lateral MCIII may be viable option for fracture stabilization in horses where return to athleticism is a priority
Distal limb cast maintained post-op for 4-6 weeks
Transverse Fractures of the Distal Diaphysis of the Third Metacarpal Bone - Prognosis
Catastrophic fracture is a serious possibility with both conservative and surgical management
Necrosis of the epiphysis has been reported
Horses with fractures that heal with conservative management have a good prognosis for return to athletic activity
Diaphyseal Fractures of MCIII/MTIII
Most common major long bone fractured in horses is MCIII/MTIII and diaphyseal fractures are encountered most frequently
Chances of success are significantly greater in younger, smaller patients
Diaphyseal MCIII/MTIII fractures probably represent the single most important indication for appropriate external coaptation
Factors Favoring Successful Repair of Diaphyseal MCIII/MTIII Fractures
Access and exposure of the entire diaphysis, making reduction and internal fixation feasible
Strong bone to which screws and plates can be affixed
Possibility of immobilization by external coaptation
Factors that Do Not Favor Repair of Diaphyseal MCIII/MTIII Fractures
Minimal soft tissue coverage, leading to many open fractures
No muscles adjacent to the fracture, resulting in poor extraosseous blood supply to the fracture site
Sparse vascularity of the distal limb
Frequent comminution, especially in older horses
Nonsurgical Management of Diaphyseal MCIII/MTIII Fractures
Cast or splint coaptation as the sole treatment of displaced diaphyseal MCIII/MTIII fractures is rarely an acceptable approach
In young animals, even though fracture healing occurs more quickly, cast coaptation is not the treatment of choice because permanent deformities develop rapidly in the contralateral limb and serious flexor/suspensory weakness occurs in the cast limb
Surgical Management of Diaphyseal MCIII/MTIII Fractures
Internal fixation is the treatment of choice
External skeletal fixation and intramedullary interlocking nails have been used, but optimal treatment remains double plate fixation
Double plating usually necessary in foals and always indicated in larger horses
Dorsolateral surgical approach, splitting the common digital extensor tendon along its course down the bone
Periosteum elevated just enough along the fracture edges to allow visual control of reduction and reconstruction
Reduction maintained with large pointed reduction forceps or by insertion of strategically placed screws inserted in lag fashion
Generally good practice to reconstruct the bone with independent screws before applying the first plate because of the far greater ease to accurately contour and apply plates to an "intact" surface
If the only practical sites for the screws will be under a plate, 3.5 mm screws that are deeply countersunk can be placed to hold the reduction while the plates are applied
Locking plates have major advantages in all types of diaphyseal fractures
Plates are placed dorsolaterally and dorsomedially at 90 degrees to each other unless fracture configuration dictates otherwise
In a large adult horse, two broad plates with 5.5 mm cortex and 5.0 mm locking head screws are used but in a foal one broad, and one narrow plate are adequate
In very small foals, two narrow plates will suffice
Reinforced 3.5 mm plate may be a valuable alternative because it has the same cross section as the narrow 4.5 mm plate, allows the insertion of more screws over the same length of plate, and results in more metal around the plate hole because the holes are smaller
Plates staggered to ensure that screws placed perpendicularly through one plate will not interfere with those from the other
All screw holes in the plate should be used
Both plates should be as long as possible without involving the joints or physis
Autologous cancellous bone graft should always be used if there are any cortical defects
Best to perform surgery as soon as possible after the injury because eburnation of the fragment ends occurs with delays and makes reduction difficult and repaired fracture less stable
Minimally invasive approach can also be used
Decision to place a cast of bandage on the limb depends on the horse's age, postoperative care, apparent stability of the repair, and available special recovery systems
Cast used for recovery but long-term protection of the repair with a cast is often undesirable because of the inevitable flexor weakness that develops
In general, foals younger than 1 year are not cast except for recovery
Casts are used in adult horses when the fixation is considered less than secure
Major complication is infection because of the relatively poor vascularity of the region, poor soft-tissue coverage, a large metal-to-bone ratio, and the frequency of open injury
Aftercare Following Repair of Diaphyseal MCIII/MTIII Fractures
Safest to stage the removal of the two plates
In foals, the first plate (usually the larger/longer of the two) can be removed at around 3 months after implantation and the second plate can be removed 45-60 days later
In neonates times can be shortened more
In adult horses staging is also recommended, although the earliest plate removal is likely to be around 4 months after implantation
Distal Physeal Fractures of MCIII/MTIII
Common injuries in suckling and weanling foals
Nearly all are Salter-Harris fracture type II with a variable length of metaphyseal involvement
Usually heal relatively quickly with minimal surgical management
Foals less than 6 weeks old can be treated with cast coaptation alone for 2-3 weeks, followed by 2-3 additional weeks in a splinted bandage
Because SH II fractures have a soft tissue "hinge" on one side of the fracture with a metaphyseal component, a foal in lateral recumbency should be positioned with that side uppermost resulting in gravity tending to reduce the physeal fracture
In older, heavier foals or those with marked instability, the fracture can be repaired with screws inserted in lag fashion through the metaphyseal component with or without a transphyseal bridge in addition to external coaptation
Foal's return to exercise is carefully graduated over several weeks while the ligamentous and musculotendinous tissues regain strength
Timing for implant removal depends on the age of the foal
If the foal is a neonate with significant remaining potential growth, the implants should be removed as early as possible to minimize risk of a shortened bone, can be as early as 3-4 weeks
In an older foal with negligible growth remaining, the implants can be removed at 2-3 months
Proximal Articular Fractures of MCIII/MTIII
Occur sporadically in racehorses and can be confusing because the lameness associated with them is typically eliminated by local anesthetic injected into the middle carpal or tarsometatarsal joint
Sagittal fractures can be seen in any breed, most occur medial to midline and are best diagnosed on nuclear scintigraphy and DP radiographs
Incomplete sagittal fractures treated conservatively with 3 months of box rest have an excellent prognosis (98%)
Frontal/dorsal plan fractures occur in MCIII or MTIII
In Standardbreds, fracture is most common in young pacers on the dorsomedial aspect of MCIII
Proximal articular fractures have been treated conservatively with good success, but displaced frontal plane fractures are best repaired with internal fixation through cortex screws inserted in lag fashion, implant removal is generally not necessary
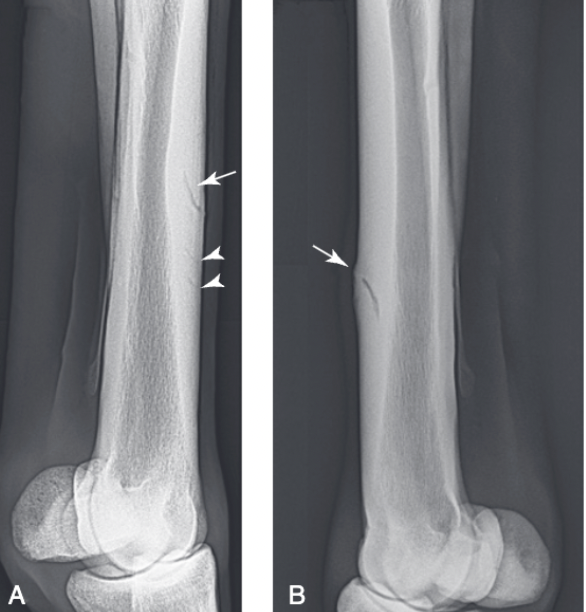
Dorsal Cortical Fractures of MCIII
Some develop one or more oblique radiolucent lines in the dorsal cortex accompanied with focal pain and swelling
Occur most commonly in 3 year old Thoroughbreds after they experience bucked shin problems in their 2 year old season
Most common configuration is a line coursing proximally at a 30-40 degree angle from the surface of the middistal dorsolateral cortex of the left MCIII
Typically the fissure extends approximately 60-70% through the dorsal cortex and disappears, but in some cases the crack curves proximad and courses back to the dorsal cortex, forming a true saucer fracture
Fractures may occur in the opposite configuration (proximodorsal to distopalmar) as well as anywhere along the length of MCIII
Bucked Shins
Pain and lameness associated with the dorsal cortex of MCIII
Nonsurgical Management of Dorsal Cortical Fractures of MCIII
Antiinflammatory agents and rest (stall and paddock) until the fracture is radiographically healed
Many horses heal without surgical intervention, but a significant percentage has no signs of radiographic healing even after several months
Best candidates for conservative treatment are fractures in the distal or proximal metaphyseal regions of MCIII because they develop periosteal bridging callus much more rapidly than the typical intracortical fracture in the diaphysis
Extracorporeal shock wave therapy - little evidence it has beneficial effects on healing and more likely primary effect is local analgesia
Surgical Management of Dorsal Cortical Fractures of MCIII
Osteostixis alone or in combination with an intracortically placed screw
Advantage of osteostixis alone is that it avoids a second operative to remove the screw
More consistent results have been achieved with the combination followed by routine screw removal at 60 days
Surgery performed under GA or under sedation and local anesthesia
Important to locate the exact site of the fracture preoperatively because it can often be very difficult to identify it visually at surgery
Useful technique is to take a radiograph of the limb after surgically preparing the skin and place multiple skin staples in a grid
Screw Placement with Osteostixis for Dorsal Cortical MCIII Fracture
4-6 cm incision made over the fracture site
In typical dorsolateral fracture, incision between the common digital and lateral digital extensor tendons
Periosteum elevated and self-retaining retractors placed to expose the bone surface
Position screw within dorsal cortex placed
In the middiaphysis of MCIII, bending occurs, therefore insertion of a screw engaging both cortices is not recommended
Oblique drill hole made into medullary cavity in estimated correct location and confirmed with radiograph
If hole is correctly positioned it can be used for the screw
If the hole is too proximal or distal an adjustment is made and the first hole just serves as another osteostixis hole
Screw should not be countersunk as it will be removed in 60-80 days
Because it is not countersunk, the screw should not be excessively tightened or it will bend
Easiest error to make is not tapping completely through the distal cortex which will result in a 3.5 mm screw easily breaking during tightening
Most dorsal cortices accommodate a 22 mm screw
Approximately 6 2.5 mm holes are prepared through the dorsal cortex around the screw
All holes must be drilled toward the medullary cavity and separated at least 10 mm
Postoperative Care Following Screw Placement and Osteostixis for Dorsal Cortical Fracture of MCIII
Postoperative care includes stall rest and handwalking for 2-4 weeks followed by 4-6 weeks of stall rest and paddock exercise
At 60 days postoperatively the horse is returned for screw removal which is performed in the standing horse under sedation and local anesthesia
If the screw head cannot be palpated, a grid of sterile skin staples over the area can be placed and a radiograph taken to facilitate localization of the ideal site for a small incision
If the screw strips the head is grasped with locking pliers and removed
After screw removal, the horse is hand walked for another month then begun in a jogging program for about 4-6 weeks before returning to regular race training