Introduction to Communication & Clinical Skills
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
10 Terms
Demonstrate an appreciation of communication skills within the consultation
Communication Skills:
Use of active listening, empathy, and open/closed questioning techniques.
Verbal and non-verbal communication (eye contact, posture, facial expression).
Involving the patient in discussions to build rapport.
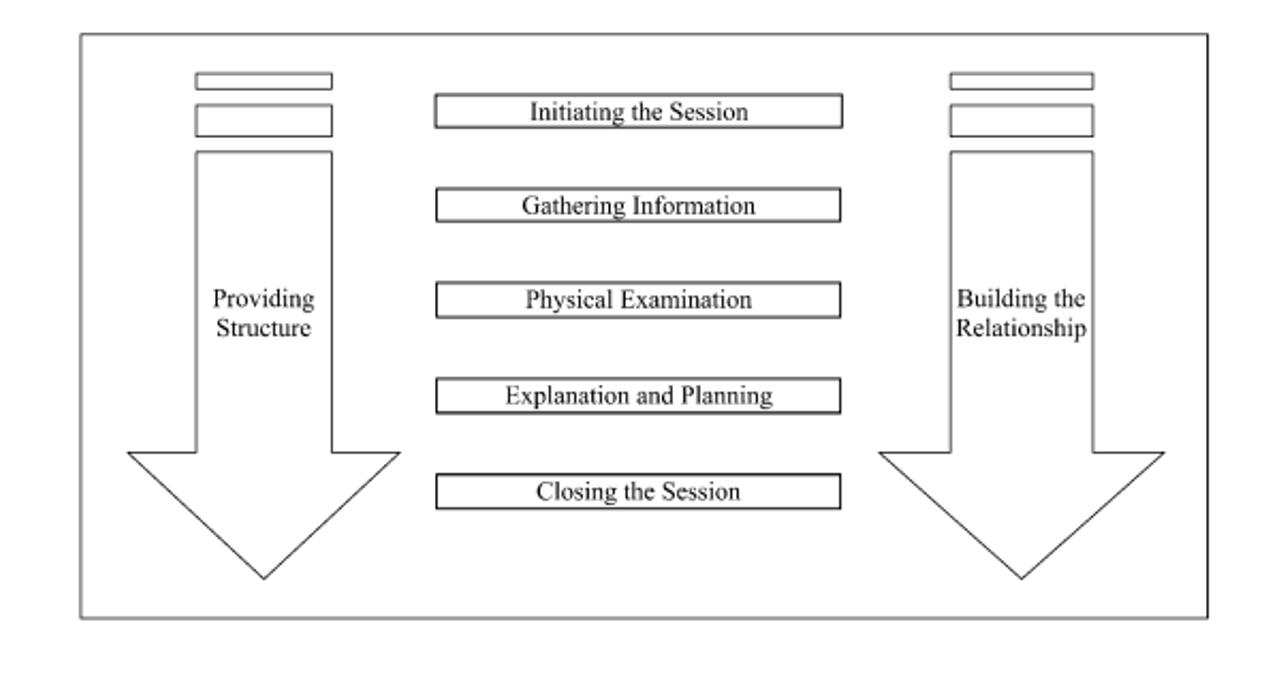
Be aware of the Calgary-Cambridge Consultation Model
Calgary-Cambridge Model:
Initiating the session: Greet patient, introduce yourself, and explain your role.
Gathering information: Open-ended questions, use of SOCRATES for pain.
Building the relationship: Empathy, body language, addressing patient’s ideas, concerns, and expectations (ICE).
Providing structure: Logical flow, signposting, and summarization.
Closing the session: End with a clear plan and check patient’s understanding.
Explain in detail the first 4 headings of the Calgary-Cambridge consultation model
Initiating the Session:
Build rapport, introduce yourself, explain purpose, and seek consent to continue.
Key Question: "Can you tell me why you’re here today?"
listen to patient attentively, without interrupting or directing your patient’s response
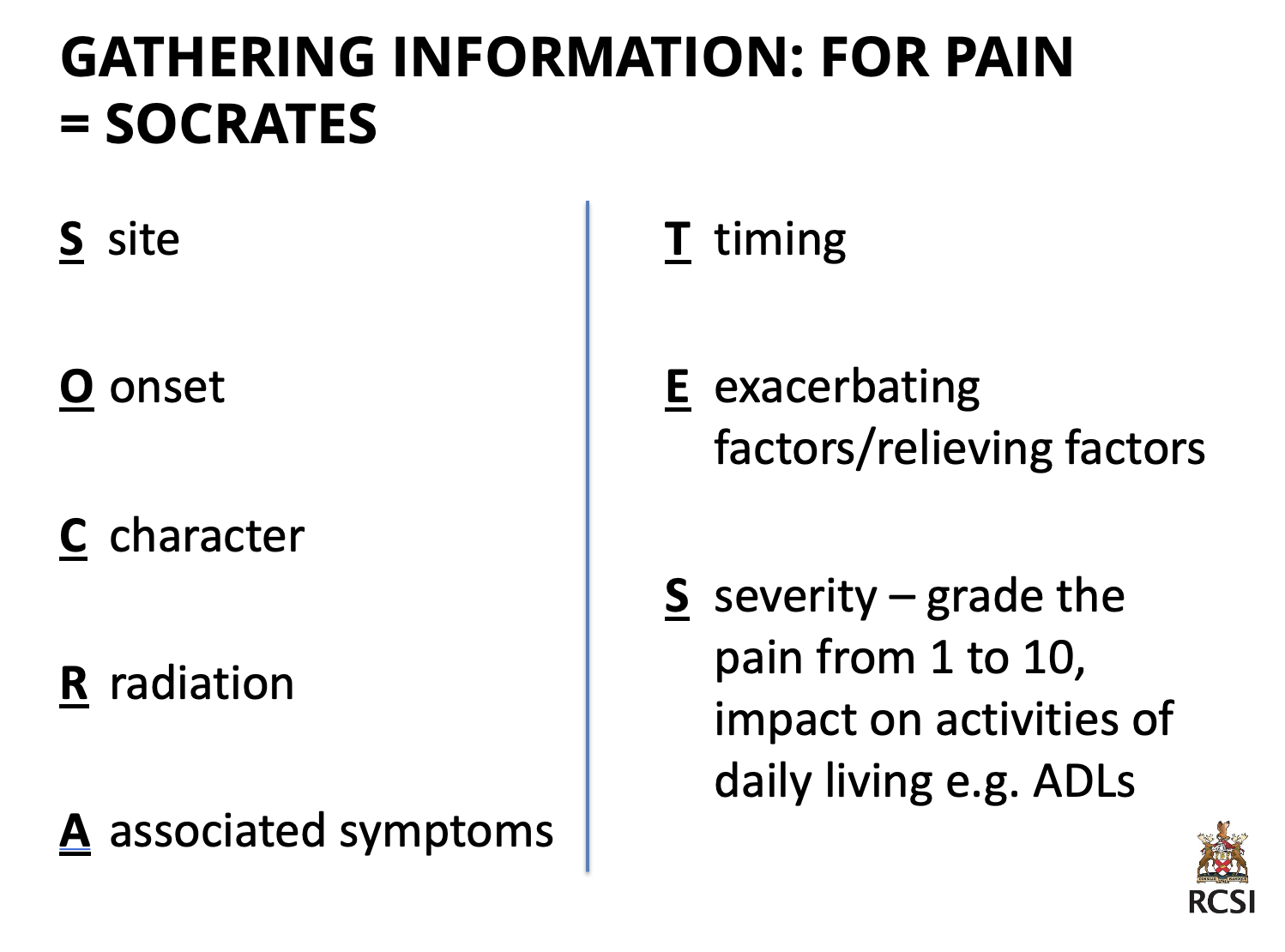
Gathering Information:
Encourage patient to tell the story of the problem(s) ‘Would you like to tell me more about that?’
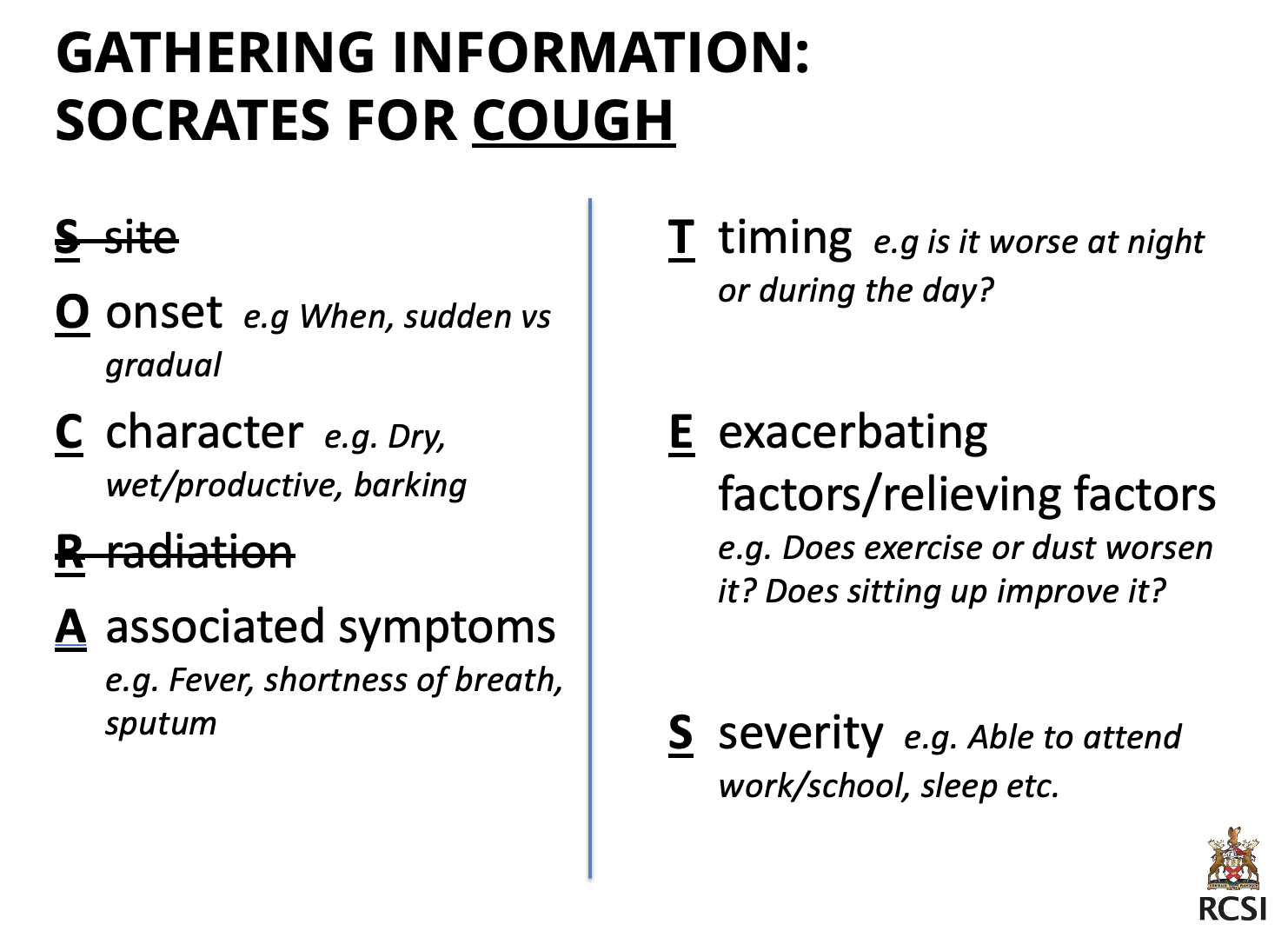
SOCRATES: For pain, assess Site, Onset, Character, Radiation, Associated Symptoms, Timing, Exacerbating/Relieving factors, Severity.
Pick up on cues, expressions and body lanugage.
Use appropriate language ‘Have you experienced any degree of dyspnoea?’ vs ‘Have you felt breathless?’
Establish dates/sequence of events – e.g. when did certain symptoms start
Use both open and closed questions. (Open question: ‘Can you tell me about your cough?’ - Closed question: ‘Does your cough get worse when you exercise?’)
Summarise - to ensure you have interpreted what the patient said correctly AND also shows that you have been listening; that you are attentive to the patient
Providing Structure:
Logical order of questions (flow), signposting, and summaries.
Example: Signposting "Now that we’ve discussed your symptoms, I’d like to ask about your medical history."
Building the Relationship:
Non-verbal behavior: Eye-contact, facial expression, tone/volume/rate of speech posture, position, movement, confidence.
Developing rapport: Use empathy, provide support, acknowledge patient views.
Involving the patient.
Learn the formal structure of history taking and how it relates to the consultation model
Initiating the session:
History Taking Structure:
Introduction & Consent: Introduce yourself and obtain consent.
Presenting Complaint: Use open-ended questions ("What brings you in today?").
Gathering Information:
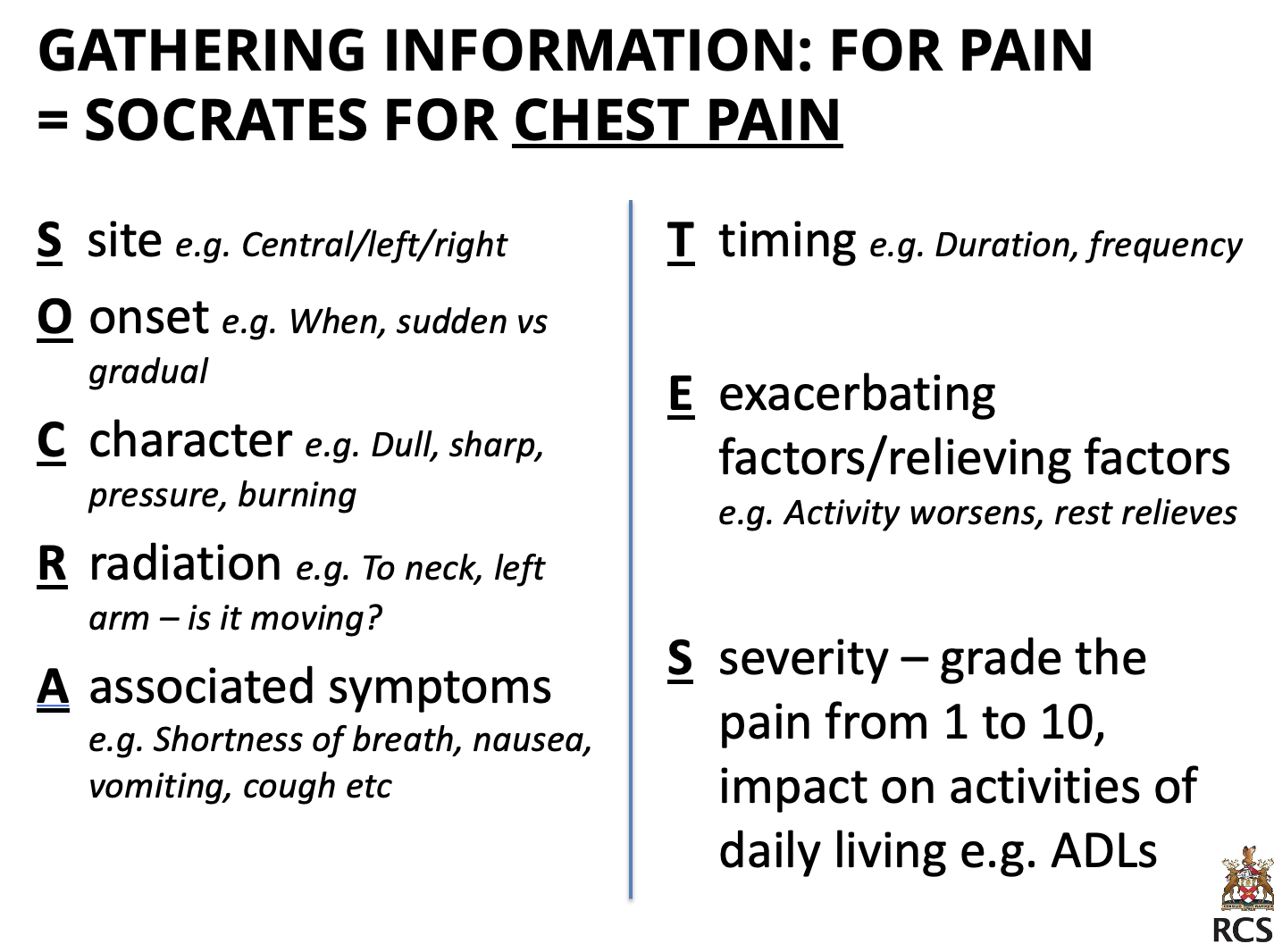
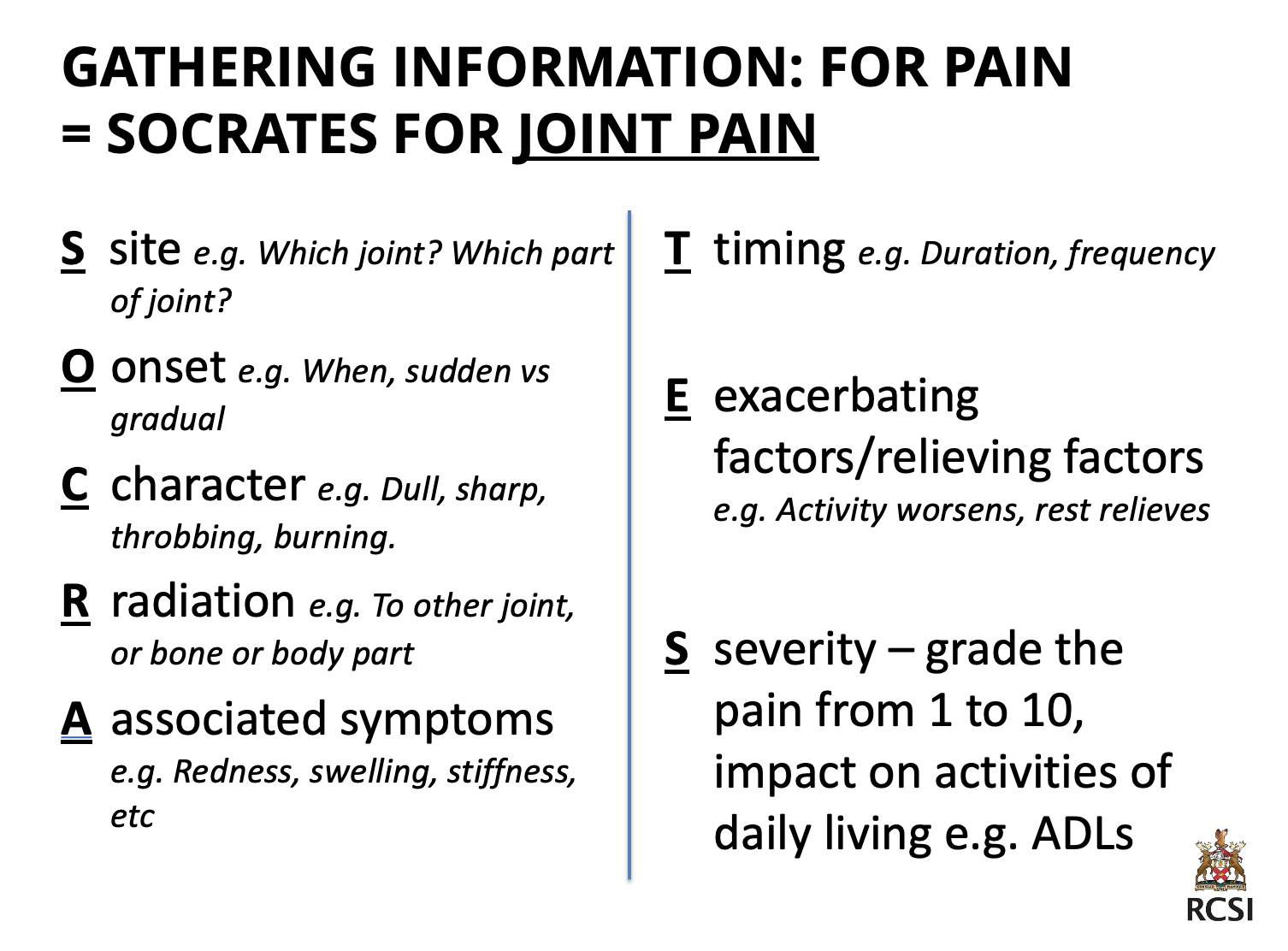
History of Presenting Complaint (HPC): Use SOCRATES for pain or explore cough, chest pain, or joint pain using similar methods.
Past Medical History (PMH): Any previous illnesses, hospitalizations, and ongoing treatments.
Medications & Allergies: Identify prescribed, OTC, and herbal medicines, as well as any allergies.
Social History: Living conditions, work, lifestyle, smoking, and alcohol use.
Family History: Inquire about chronic conditions like diabetes or heart disease in immediate family members.
Systems Review: A quick review of key systems to identify other issues.
Summary, Differential Diagnosis & Management Plan: Summarize key findings and discuss next steps.
Gathering Information: for pain (SOCRATES)
Gathering Information: for chest pain (SOCRATES)
Gathering Information: for joint pain (SOCRATES)
Gathering Information: for cough (SOCRATES)
Be aware of summarizing your findings, forming a differential diagnosis, and management plan
Summary:
Recap key points to ensure the patient’s story is accurately understood.
This shows the patient you are actively listening and allows for clarification.
Differential Diagnosis:
Use the collected information to create a list of possible diagnoses.
Rank possible causes from most likely to least likely.
Management Plan:
Discuss treatment options and check patient’s preferences and understanding.
Ensure the patient is aware of follow-up steps and what to expect.
Identify the patient’s ideas, concerns, and expectations throughout the consultation
Ideas: Patient’s own beliefs about their condition.
Concerns: Fears or worries the patient may have (e.g., "Do I have cancer?").
Expectations: What the patient expects from the consultation (e.g., tests, treatment, reassurance).
Why It’s Important:
Addressing ICE ensures patient-centered care.
Builds trust and helps in creating an effective treatment plan.