Microbial Pathogenesis: Infection, Entry, and Host Defense Mechanisms
1/133
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
134 Terms
What is a pathogen?
A pathogen is an organism that causes disease, including bacteria, viruses, fungi, and parasites.
What are primary pathogens?
Primary pathogens cause disease in healthy hosts.
Give an example of a primary pathogen and its effects.
Enterohemorrhagic Escherichia coli (EHEC) causes severe and bloody diarrhea, inflammation, and renal failure.
What are opportunistic pathogens?
Opportunistic pathogens cause disease only in compromised hosts or after entering unprotected sites.
Provide an example of an opportunistic pathogen.
Staphylococcus aureus, which is normal flora on human skin but can cause infections.
What is pathogenicity?
Pathogenicity refers to an organism's ability to cause disease, measured by infectivity, severity, and genetic makeup.
Define virulence.
Virulence is a measure of the degree or severity of disease caused by a pathogen.
How does the virulence of Ebola virus compare to that of rhinoviruses?
Ebola virus is highly virulent, causing severe hemorrhagic infections with a 50% mortality rate, while rhinoviruses cause the common cold with rare life-threatening complications.
What does infection mean in the context of microbial pathogenesis?
Infection occurs when a pathogen enters or begins to grow on a host, but does not necessarily imply overt disease.
What must microbes do to be considered viable?
Microbes must multiply and be able to spread to new hosts.
What are the two modes of spread for pathogens?
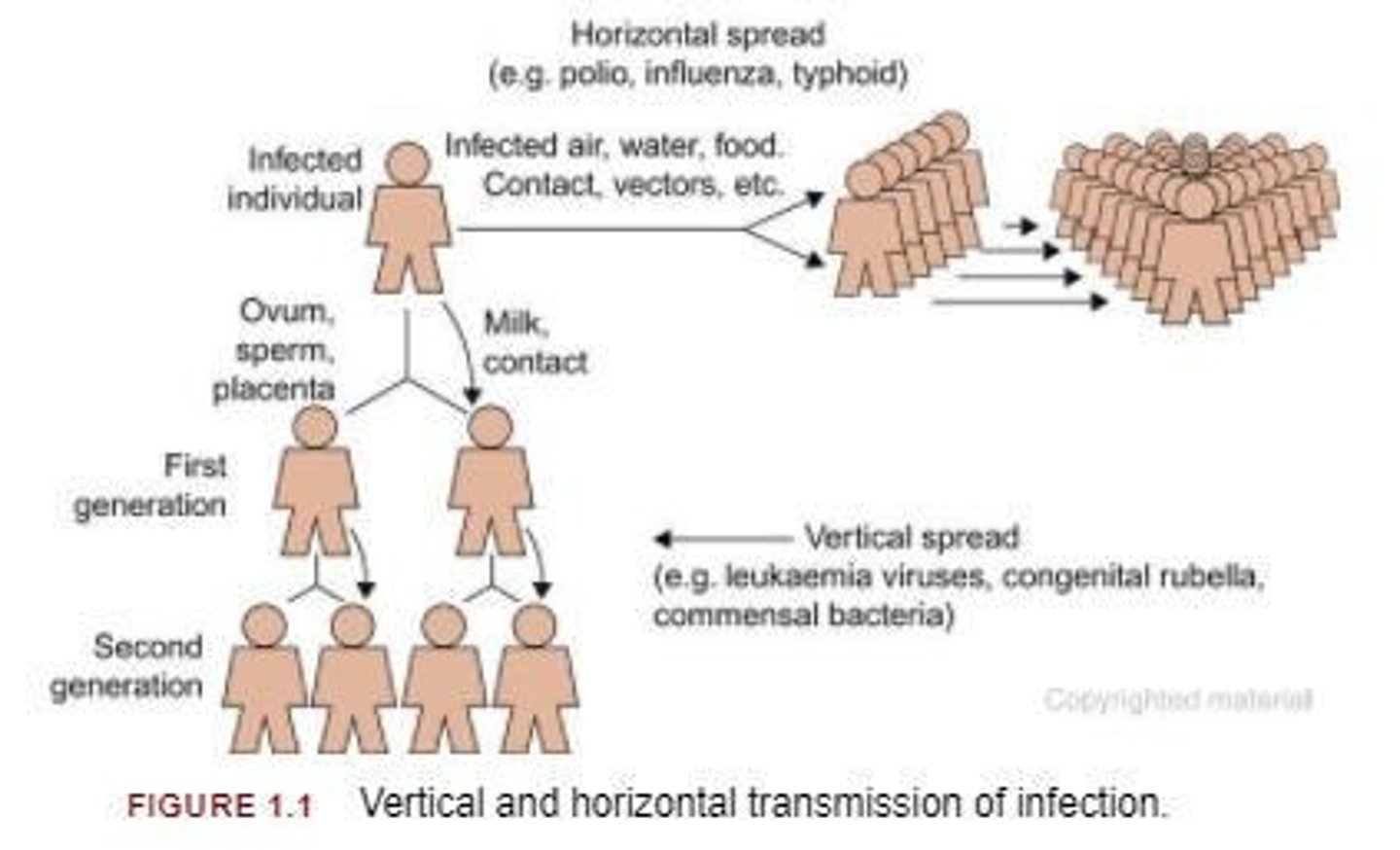
Horizontal spread (contact, air, water, insect vectors) and vertical spread (to offspring via sperm, ovum, placenta, or milk).
What characterizes exogenously acquired diseases?
Exogenously acquired diseases result from encounters with agents in the environment, such as food, water, air, or insect bites.
What are endogenously acquired diseases?
Endogenously acquired diseases are caused by agents present in or on the body, often from normal microbiota that penetrate deeper tissues.
Give an example of an endogenous infection.
Boils caused by Staphylococcus aureus that penetrate through a cut.
What is the challenge in distinguishing between exogenous and endogenous infections?
In some cases, normal microbiota may harbor virulent strains, making it unclear if an infection is endogenous or exogenous.
What role does the microbiota play in human health?
Microbiota are normal microbes on our skin or mucous membranes that can cause disease if they penetrate deeper tissues.
What is the significance of understanding modes of encounter in microbial disease?
The mode of encounter suggests potential modes of prevention for microbial diseases.
What is a nonviable microbe?
A microbe that is unable to replicate and therefore cannot cause infection.
What is the relationship between infectivity and pathogenicity?
Infectivity is a component of pathogenicity, indicating how easily an organism can cause disease.
How does the genetic makeup of a pathogen influence its pathogenicity?
The specific genetic makeup can determine the pathogen's ability to infect hosts and the severity of the disease it causes.
What is the importance of microbial multiplication in the context of infection?
Microbial multiplication is essential for establishing an infection and for the pathogen to spread to new hosts.
How can understanding microbial pathogenesis help in disease prevention?
By understanding how pathogens establish infections and spread, targeted prevention strategies can be developed.
What is the relationship between commensalism and microbial survival?
Commensalism allows organisms to coexist without damage, benefiting microbes by helping them survive, multiply, and leave descendants.
What is balanced pathogenicity in microbes?
Balanced pathogenicity refers to the state where infectious agents cause minimal damage necessary for their entry, multiplication, and discharge from the host.
Why do microbes generally not want to kill their host?
Microbes do not want to kill their host because a reduction in host species limits their ability to multiply.
What are some examples of mild symptoms caused by microbes to facilitate shedding?
Runny nose and diarrhea.
What factors contribute to the achievement of balanced pathogenicity in microbes?
Many organisms have not had time to reach balanced pathogenicity, and virulent variants can emerge, causing extensive disease before reaching balance.
How can the introduction of microbes to new populations affect their pathogenicity?
Microbes introduced to new, more susceptible populations may not have evolved to a less pathogenic form, leading to increased disease.
What is an example of a microbe that has other host species for survival?
Microbes responsible for rabies, anthrax, plague, and tularemia have other host species such as mammals and arthropods.
How do microbes adapt to new species?
Microbes can adapt through evolutionary changes, as revealed by advances in DNA sequencing and phylogenetic analyses.
What is the microbial disease process?
To cause disease, pathogens must enter a host, find their niche, avoid host defenses, multiply, and transmit to a new host.
What are the primary sites of entry for microbes into the body?
Skin, respiratory tract, gut, and urogenital tract.
What role does the skin play in preventing microbial infection?
The skin is the largest organ providing a dry protective surface, but it cannot cover all surfaces.
How do mucosal surfaces facilitate microbial invasion?
Mucosal surfaces provide a pathway for microbial invasion, as they are easier to penetrate than skin.
What are adhesins in the context of microbial infection?
Adhesins are microbial factors that promote attachment to host cells, allowing microbes to colonize or penetrate.
How do viruses and bacteria attach to host cells?
Viruses attach through capsid or envelope proteins, while bacteria use pili, nonpilus proteins, or nonprotein molecules.
What is the importance of multiple adhesin systems in pathogens?
Most pathogens possess more than one adhesin system, which may be necessary to engage multiple receptors for infection.
What are some barriers to infection provided by the body?
The body has skin, mucosal surfaces, and special cleansing systems to prevent microbial attachment and entry.
How do host defenses adapt to microbial threats?
Vertebrates develop efficient recognition systems and immune responses to restrain the growth and spread of microbes.
What is the significance of rapid microbial evolution in relation to host defenses?
Rapid evolution allows microbes to stay ahead of host defenses, exploiting weak points for successful infection.
What is the role of the immune response in microbial infection?
The immune response aims to restrain the growth and spread of microbes, but it is not infallible.
What happens to microbes that have not evolved to a less pathogenic form?
They may cause extensive disease in new host populations before potentially reaching a balanced state.
What is an example of a microbe that has evolved from a related virus in animals?
Measles likely arose from a related virus that infects cattle.
How does the ability to multiply rapidly benefit microbes?
Rapid multiplication allows microbes to evolve faster than their hosts, increasing their chances of survival.
What is a common pathway for acute illnesses caused by microbes?
Most acute illnesses occur via the respiratory or gastrointestinal tract.
How do microbes use specific receptors for attachment?
Some microbes target specific receptors on host cells to facilitate attachment and colonization.
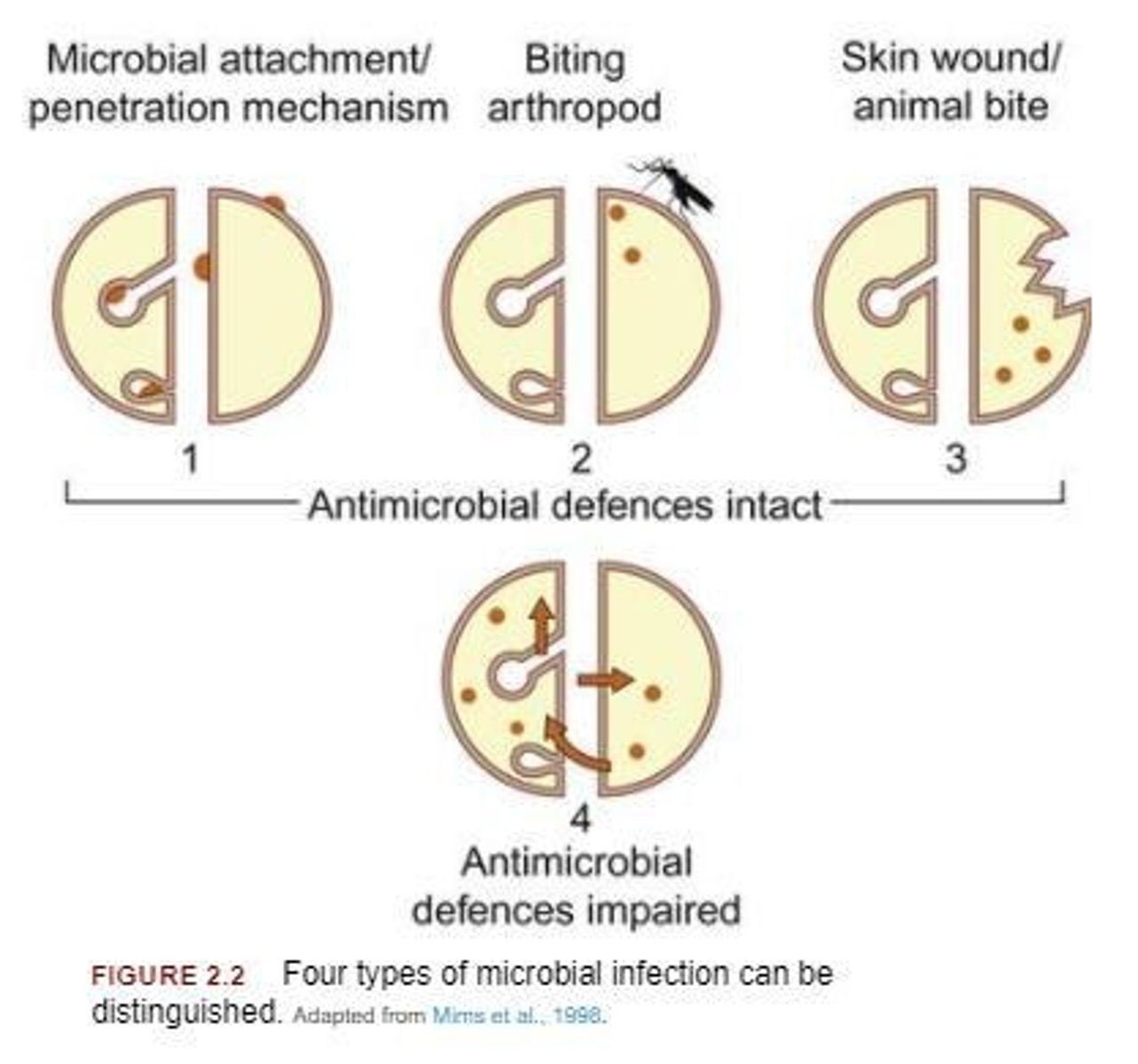
What are the broad classifications of infections based on invasion strategies?
Infections can be classified by mechanisms for attaching to hosts, introduction by arthropods, reproduction and transmission via arthropods, causing disease only with host damage, or requiring immunocompromised hosts.
How do microbes penetrate the skin?
Microbes penetrate the skin at macro or microscopic breaks in continuity, overcoming the skin's natural barrier.
What inactivates microbes on the skin?
Microbes other than commensals are inactivated by fatty acids and materials produced by skin commensals.
What can cause lesions when bacteria enter other orifices?
Bacteria on skin and hair follicles can cause lesions when they enter other orifices.
How can Staphylococcus cause mastitis in cows?
Staphylococcus can cause mastitis when pushed into the bovine teat canal during milking.
What are some obvious routes for infection through the skin?
Large breaks in the skin, such as those caused by needles or shaving, are obvious routes for infection.
How do arthropods introduce pathogens during feeding?
Arthropods like mosquitoes and ticks penetrate the skin and can introduce pathogens either mechanically or biologically.
What is the difference between mechanical and biological transmission of infections by arthropods?
Mechanical transmission involves pathogens contaminating arthropod mouthparts without replication, while biological transmission involves replication in the arthropod and transfer via saliva.
What infections can be transmitted through animal bites?
Rabies can be transmitted through bites from foxes, dogs, wolves, and vampire bats, while bites from cats can transmit Pasteurella multocida.
What is a potential consequence of human bites?
Human bites can inoculate bacteria into the skin, potentially leading to sepsis.
What are the filtration mechanisms of the respiratory tract?
Larger particles are filtered by nostril hair, while particles around 10 µM can be deposited on turbinates and those around 5 µM can reach the lungs.
How many microbes does an average person inhale daily?
An average person inhales about 10,000 microbes per day.
What role does the mucociliary blanket play in the respiratory tract?
The mucociliary blanket traps foreign particles in mucus and moves them up the respiratory tract to be swallowed.

What mechanisms do pathogens use to infect the respiratory tract?
Pathogens must avoid being trapped by mucus, resist phagocytosis, and have mechanisms for attachment to epithelium.
How can cystic fibrosis affect respiratory infections?
Cystic fibrosis leads to abnormally thick mucus that cannot be exported, sequestering microbes and increasing infection risk.
What can impair mucociliary defenses in the respiratory tract?
Smoking and indwelling devices can impair mucociliary defenses, making infections more likely.
What is the role of alveolar macrophages in respiratory infections?
Alveolar macrophages help kill inhaled microbes, and pathogens must resist being killed by them to establish infection.
How does the influenza virus attach to the respiratory epithelium?
The influenza virus uses hemagglutinin, a glycoprotein that binds to neuraminic acid on epithelial cells.
What happens to microbes that lack mechanisms for attachment in the respiratory tract?
Microbes that lack attachment mechanisms only cause infection when mucociliary cleansing is damaged.
What can depress ciliary activity in the respiratory tract?
Certain pathogens can depress ciliary activity, impairing the respiratory tract's ability to clear microbes.
What is the significance of the average mucus production in the respiratory tract?
An average person produces 10-100 mL of mucus daily, which helps trap and remove inhaled particles.
What can cause damage to the respiratory tract that leads to infection?
Defects in cleansing mechanisms, such as those caused by viral infections or physical issues, can lead to respiratory tract infections.
What is the role of nostril hair in the respiratory tract?
Nostril hair filters larger particles from the air.
What size particles are likely to reach the lower respiratory tract (LRT)?
Particles around 5 µM can reach the LRT.
How many organisms are typically present per cubic meter of air in buildings?
400-900 organisms per cubic meter.
How many microbes does an average person inhale per minute?
Approximately 8 microbes per minute, totaling around 10,000 per day.
What is the primary function of the mucociliary blanket in the LRT?
It traps foreign particles in mucus and moves them up the respiratory tract.
What mechanisms can lead to infection in the respiratory tract?
Infection can occur if cleansing mechanisms are defective, allowing microbes to evade mucus trapping and phagocytosis.
Which pathogen is known to attach to epithelial cells and depress ciliary activity?
Bordetella pertussis.
What is the impact of cystic fibrosis on mucus production?
Cystic fibrosis patients produce abnormally thick mucus that cannot be effectively cleared, sequestering microbes.
What type of pathogens can survive in alveolar macrophages in the LRT?
Mycobacterium tuberculosis.
What is a unique characteristic of Helicobacter pylori in the gastrointestinal tract?
It can reside in the stomach and persist for years in the mucus overlay of the epithelial layer.
What happens to bacteria during normal intestinal transit time in the GI tract?
A single E. coli can replicate to 105 cells during the average transit time of 12-18 hours.
What are the exceptions to the lack of distinct cleansing mechanisms in the GI tract?
Vomiting and diarrhea serve as cleansing mechanisms.
How can reduced flow rate in the GI tract affect bacteria?
Reduced flow rate can lead to outgrowth of bacteria, potentially causing nutrient malabsorption.
What is the relationship between commensal bacteria and the intestinal wall?
Commensal bacteria are associated with the intestinal wall, either in mucus layers or attached to the epithelium.
What chronic condition is associated with Helicobacter pylori infection?
Chronic inflammatory response, which can lead to ulcers and cancer.
What is the effect of smoking on mucociliary defenses?
Smoking can impair mucociliary defenses, increasing susceptibility to infections.
What type of microbes typically cause infections when mucociliary cleansing is damaged?
Microbes that lack mechanisms for attachment to epithelium.
What is the significance of temperature for some viruses in the respiratory tract?
Some viruses replicate better at 33°C than at 37°C, leading to infections in the nasal cavity.
How does the presence of pathogens like Pseudomonas aeruginosa affect ciliary activity?
Pseudomonas aeruginosa produces ciliostatic substances that inhibit ciliary activity.
What is the average daily mucus production in the nasal cavity and lung?
An average person produces 10-100 mL of mucus daily.
What is the role of alveolar macrophages in the respiratory tract?
Alveolar macrophages are responsible for phagocytosing inhaled particles and pathogens.
How do pathogens evolve mechanisms for attachment in the respiratory tract?
Pathogens develop specific mechanisms to attach to epithelial cells to resist being cleared by mucus.
What must pathogenic intestinal bacteria do to establish an infection in the GI tract?
They must establish infection and increase in numbers.
What role does mucus play in the GI tract regarding infection?
Mucus protects epithelial cells as a mechanical barrier and contains secretory IgA.
How do motile microbes like Vibrio navigate the mucus in the GI tract?
They can propel themselves through mucus and produce mucinase.
What factors affect the likelihood of infection in the GI tract?
Factors include mucus, motility of microbes, acid, proteolytic enzymes, and bile.
What is the significance of the GI tract's motion in relation to infection?
The GI tract's constant motion allows for frequent encounters between particles in the lumen and host cells.
How do viruses replicate in the GI tract?
Viruses must replicate within host cells and take advantage of encounters with epithelial cells.
What is the role of enteric bacteria in the lumen of the GI tract?
Enteric bacteria can grow in the lumen, enhancing chances of interaction with epithelial cells.
How does Salmonella infect host cells in the GI tract?
Salmonella attaches to microvilli, causing degeneration that allows bacteria to enter the cell.
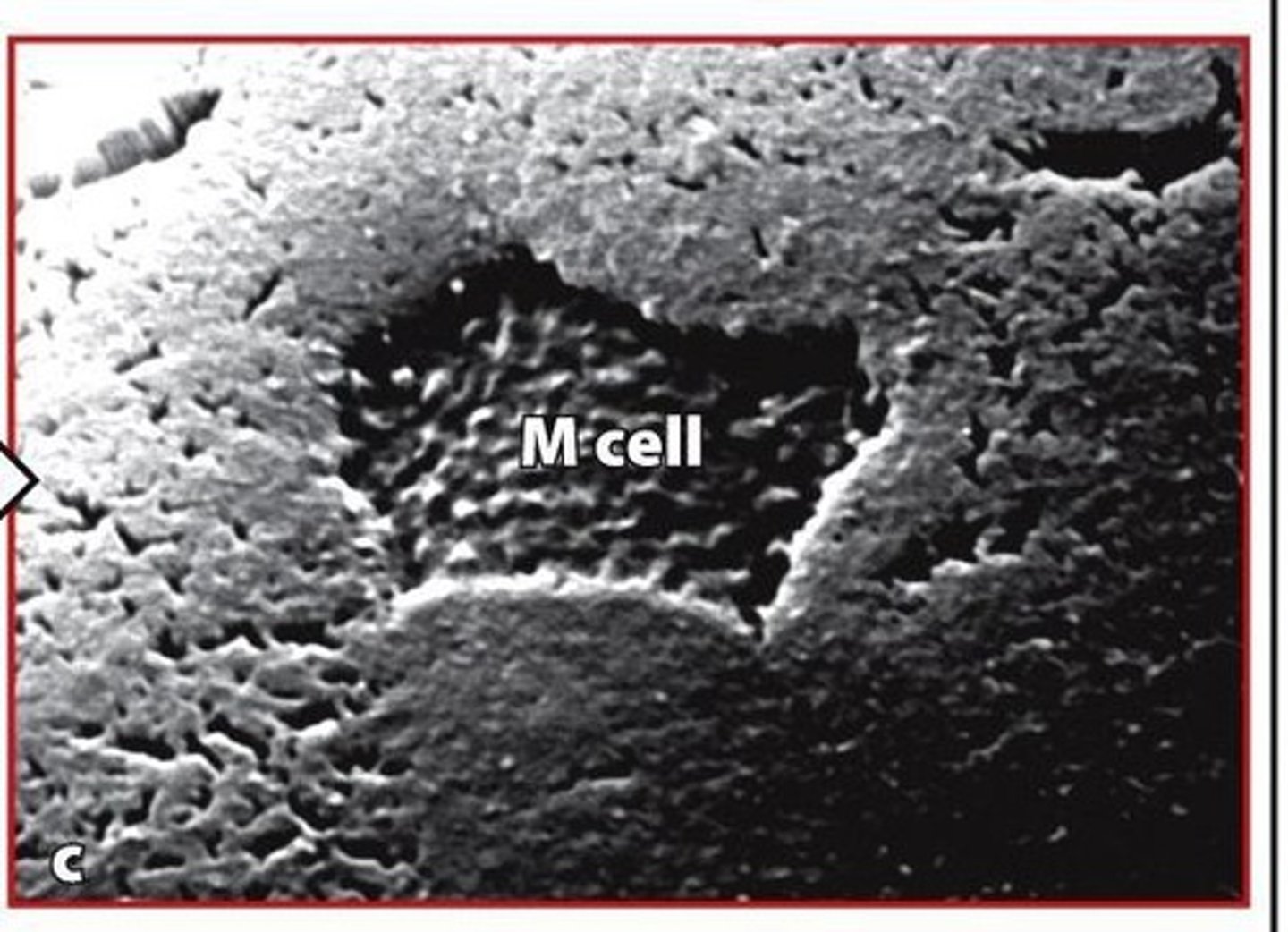
What is the role of Peyer's patches in the intestine?
Peyer's patches are sites of particle uptake, with M cells being specialized epithelial cells involved in this process.
How does the absorption of protein differ in infants compared to adults?
Infants absorb protein more readily and can better absorb maternal antibodies from milk.