Microscopic Anatomy and Physiology of Muscle
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
Type 1 muscle fibers
Stain dark
Contract slowly (Slow twitch)
Can contract for longer periods of time
Type 2 muscle fibers
Stain light
Contract quickly (fast twitch)
Susceptible to fatigue
The speed of contraction is related to what?
myosin ATPase
Endurance relates to content and activity of mitochondria
(Generate ATP for contraction -oxidative/aerobic metabolism)
Sustained contractions
slower twitch
Anti-gravity muscles
I bands
Light zones (thin filaments only)
A Bands
Darker regions (thick and thin filaments)
What is the banding pattern of myofibril composed of?
Alternating A and I bands
What Bisects each I band?
Dense Z line
One end of each filament is attached to Z line
What is the Sarcomere?
Myofibril between Z lines
Fundamental unit of contraction in striated muscle (Skeletal, and Cardiac)
Each muscle fiber has how many myofibrils?
100s to 1000s
Each myofibril:
1500 thick filaments
3000 thin filaments (wrap around the thick)
Thick myofilaments are composed of what?
Myosin = gold club shaped protein
thin myofilaments are composed of what?
Actin= globular protein
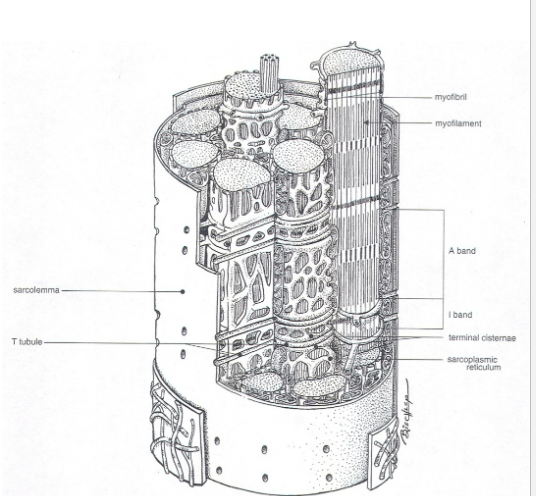
What functions does the sarcoplasmic reticulum (agranular- lack ribosomes) do?
Excitation (contraction) coupling
What is also found in muscle fibers
Golgi apparatus
many mitochondria
Glycogen (liver has lots of glycogen and Skeletal muscle- whole body)
T tubules are continuous with plasma membrane. What do they do?
Extend into the interior of muscle fibers (at right angle). at myofibrils and sarcoplasmic reticulum
Propagates action potentials from sarcolemma (into interior of muscle fibers=initiate contraction)
Number of muscle cells is what?
Set at birth
increase in muscle mass= hypertrophy (increase in myofibrils and vascularization)
If nerve supply to a muscle fiber is destroyed what happens?
Fibers decrease to almost nothing
Denervation or neurogenic atrophy
Ex. Sweeney Shoulder of draft horses - subscapular nerve damaged by collar → Atrophy of supraspinatus and infraspinatus muscle of shoulder
How is a skeletal contraction triggered?
by an action potential
initiated by firing of a motor neuron
Axon branched terminated in a neuromuscular junction (mid-point of muscle)
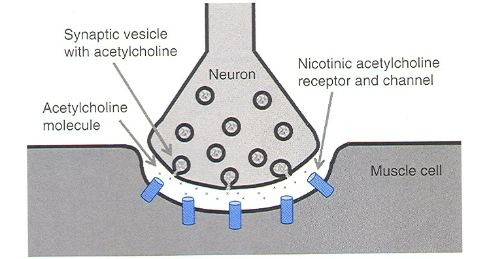
What is a type of excitatory synapse?
Neuromuscular junction
What is the receptor for skeletal muscle contractions?
nicotinic acetycholine receptor
What is resting membrane potential?
-70 mv
What cells are excitable?
neuron and skeletal muscle
Action potential is not propagated directly into muscle cell. explain the steps (look at drawing for help)
Depolarization of motor nerve ending releases acetylcholine (chemical neurotransmitter ACH)
ACH diffuses across the junction binds to Nicotinic receptors (key) located on the muscle fiber
Stimulates opening of ligand-gated (lock and key) NA channels→ leads to Na (+ charge) rush into the cell leading to membrane depolarization.
move 3 sodium out and 2 potassium in
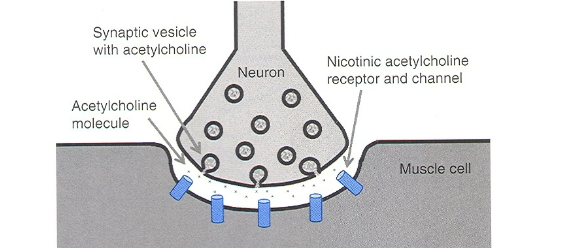
After Ligand gated channels open to start depolarization, what happens next. Explain the steps (look at drawing for help)
End-plate potential =local depolarization of sarcolemma at the neuromuscular junction via ligand-gated channels
depolarization is usually enough to reach threshold potential of electrically gated Na channels (after RMP becomes more positive)
Channels open and more Na rushes in
local current occurs again and other action potentials are generated in adjacent areas
Entire sarcolemma of muscle fibers depolarized
3 step of contractions
T tubules are inward continuations of sarcolemma (action potential travels along tubules throughout fiber)
Some T tubules pass immediately adjacent to SR
Structural link between: Protein in sarcolemma of T tubule (dihydropyridine receptor) and membrane protein channel in SR
Channel becomes permeable to Ca2+ (because of the link between two proteins)
HAVE TO HAVE CALCIUM BEFORE A CONTRACTION
Last step of contractions
Ca2+ concentration in SR is greater than sarcoplasma (100-fold greater)
Ca2+ diffuses into sarcoplasma and into myofibrils
Increase in Ca2+ in myofibrils leads to interaction between thick and thin filaments
Movement (sliding) of thin past thick towards center of sarcomere
Shortens the sarcomere→ Shortens myofibrils→ entire muscle
Hyperkalemic periodic paralysis (HyPP) (Increase in Potassium)
Genetic Disorder of horses
Genetic mutation of transmembrane protein (Electrical gated Na channel is defective) Increase permeability to Na→ depolarization →involuntary muscle contractions
Hyperkalemia is increasing serum K
Clinical sign: muscle spasm, tremors, sweating, and weakness
Thick filaments is a bundle of what?
Myosin and it has two parts:
Filament like part (lies parallel to similar parts of myosin, and makes up the length of filament)
Projects out like an arm from end of filament- enlargement at end is myosin head
Thin filament is made up of three proteins. What are they?
Actin (most prominent, 2 strands wound around each other)
Tropomyosin (2 strands wound around each other, and spiral around actin)
Troponin (bound to tropomyosin at specific sites, together called troponin-tropomyosin complex)
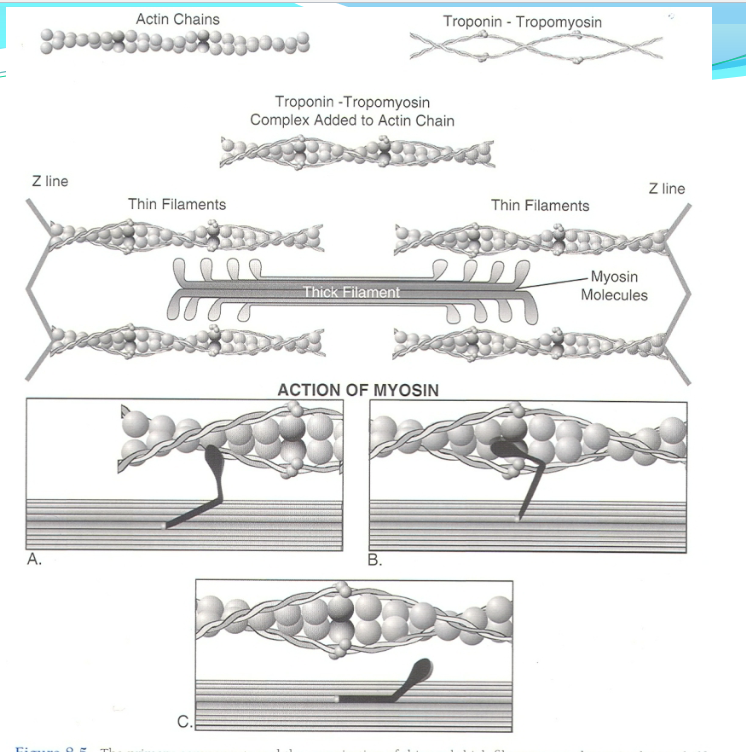
Relaxation
Contractions happen as long as there is excess Ca2+ in the sarcoplasm
When effect of action potential on sarcolemma ends:
Ca2+ goes back into SR
Ion pumps in membrane of SR use ATP to pump Ca2+ (for storage until next action potential) without ATP muscle cannot relax
When most Ca2+ is removed, thick and thin filaments are dissociated
Allows elasticity of muscle to return to resting length (pulls Z lines and thin filaments back to original position)
What is sign of heart attack?
Troponin in bloodstream
Ca2+ binding sites binds to troponin
What is vital for the continuation of contractions?
ATP and Ca2+ level in sarcoplasm
Curarifrom drugs
Bind to ACH receptors so ACH can not bind to them→ no end potential (Stop at step #1 and 2 of contraction)
ACH-ase does not break down curare
Death from asphyxiation
dose dependent
medically used for some surgeries
Drugs that affect skeletal muscle function: Botulinum Toxin
Very early
Prevent release of ACH
→ prevents no action potential= flaccid paralysis
“limberneck” in poultry
Tone
slight tension muscles exhibit when at rest
continuous transmission of impulse at very low frequency
Keeps muscles in partially contracted state
prevents them from become flaccid (flabby)
When an animal gets excited (anxious, fear, etc.) what happens to muscle tone?
Muscle tone intensifies
Animal can respond faster to stimulus
Seen as skittish (jumpy)
Describe muscle tone during sleep.
Tone is low allowing for optimal relaxation
Describe smooth muscle
Involuntary muscle
99% is visceral type (organs)
AKA single unit or unitary smooth muscle
Joined by gap junctions
1% multiunit smooth muscle
Gap junctions not prevalent (pilomotor muscles)
Smooth muscle Structure
Fusiform (spindle shaped)
Central nucleus
Mostly sarcoplasm (no striations, myofibrils, or sarcolemma visible w/light microscope)
filaments with actin and myosin, not orderly arrangement (no shortening of sarcomere)
Increase hypertrophy and hyperplasia (mitotically) Uterine wall during pregnancy
Smooth Muscle Stress-Relaxation (plasticity)
Adjust to stretching w/o increasing final tension
Tension increases with stretching-at first
Relaxes to original tension
Ex. stomach- filling with food, SI- Food moving along, Blood vessel when blood volume increases
Allows expansion w/o pain, and not loose contractility
reverse when stretch is reversed (empty urinary bladder)
Smooth muscle contraction (slower than skeletal)
cause of contraction/relaxation variable
less cell energy
Role of calcium in smooth muscle contraction
contraction/relaxation related to Ca2+ concentration in sarcoplasm
some Ca2+ stored in SR, but also have Ca2+ channels in outer membrane
Voltage gated/ligand-gated channels
respond to hormones
Ca2+ channel blockers (useful for reducing blood pressure)
When Cytoplasmic Ca2+ increases → binds regulatory protein (calmodulin) when bound to calmodulin, activates a kinase—> phosphorylates myosin results in contraction
Relaxation occurs by Unphosporylation by enzymes in cell (occurs when Ca2+ is reduced (Ca2+ Atp-ase)
Sympathetic Epinephrine and norepinephrine bind B2-adrenergic receptors
Effect: relaxation of smooth muscle cells
ex. airways
Sympathetic epinephrine and bind a1-adrenergic receptors
Contraction of smooth muscle cells
ex. blood vessels
Parasympathetic Acetycholine bind muscarinic ACH receptors
Contraction of smooth muscle cells
ex. SM of airways and blood vessels
Cardiac muscle (involuntary striated)
Striations fainter than muscles
Major difference
Heart made up of different cells (than muscles)
muscle cells meet end to end= intercalated disks
Excitation and Contraction of Cardiac muscle
Do not require nerve stimulation
BUT action potentials must occur on cell membrane → 1st occur spontaneously= specialized myocardial pacemaker cells
Cardiac action potential slower than skeletal muscle
Contraction lasts as long as action potential does
Ca2+ binds to regulatory proteins on actin filaments
Cardiac Hypertrophy (increase in cell size)
When heart has excessive work to do
Do NOT regenerate or undergo hyperplasia (similar to skeletal)
Living in high altitude can cause hypertrophy (increase vascular resistance, increase blood pressure in lungs)
Brisket disease (high mountain disease) in cattle
Hypertrophy can NOT compensate for increase in vascular resistance
clinical sign= edema of brisket