41. Antimicrobial Therapy: Antimicrobial Agents 3/4
1/3
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
4 Terms
DNA Gyrase Inhibitors: Fluoroquinolones (Oral)
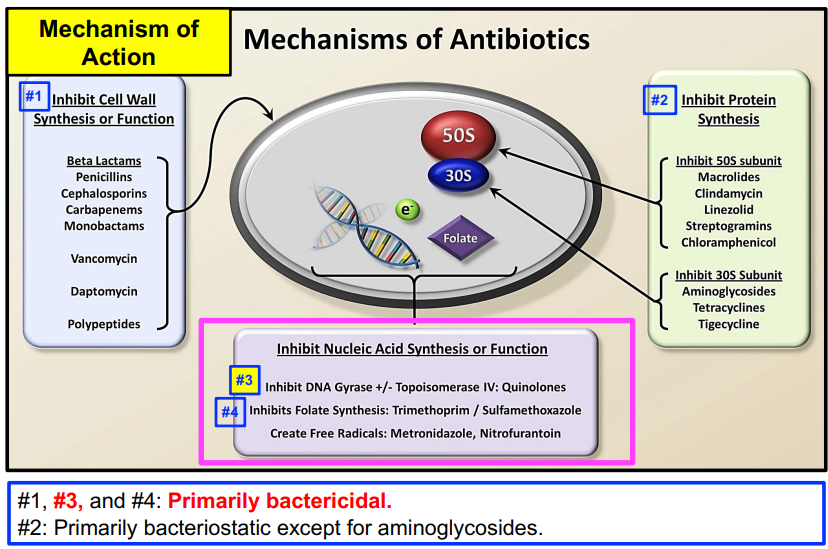
Mechanism of Action: Inhibits DNA gyrase and topoisomerase IV, promotes breakage of double-stranded DNA.
Bactericidal
FQs have broad spectrum of activity, oral administration achieves similar blood levels to IV administration.
Systemic fluoroquinolones are associated with clostridium difficile associated diarrhea (CDAD) and antimicrobial resistance
Levofloxacin and moxifoxacin referred to as “respiratory fluoroquinolones”, because they have excellent activity against S. pneumoniae, which is a common cause of community-acquired pneumonia (CAP).
Fluoroquinolones are commonly considered alternatives for patients with a documented severe β-lactam allergy (similar to macrolides).
Fluoroquinolones may be classified by “generation”
Ciprofloxacin, ofloxacin, levofloxacin, and moxifloxacin
Gatifloxacin and besifloxacin are available only as topical
2nd gen: cipro/oflox; 3rd gen: levo; 4th gen: gati/moxi, ? gen: besi
Indications
Ciprofloxacin: Urinary tract infections, acute uncomplicated cystitis in females, chronic bacterial prostatitis, bone and joint infections, infectious diarrhea, typhoid fever (Salmonella typhi), etc.
Ofloxacin: Urinary tract infections (complicated), cystitis (uncomplicated), prostatitis, chronic bronchitis, community- acquired pneumonia, skin and skin structure infections, etc.
Levofloxacin: Community-acquired pneumonia, chronic bronchitis, acute bacterial rhinosinusitis, prostatitis, urinary tract infection (uncomplicated or complicated); acute pyelonephritis; skin or skin structure infections (uncomplicated or complicated), etc.
Moxifloxacin: Community-acquired pneumonia, chronic bronchitis, skin or skin structure infections, etc.
DNA Gyrase Inhibitors: Fluoroquinolones Multiple BBWs
Tendon inflammation/rupture (BBW)
CNS effects (BBW)
Peripheral neuropathy (BBW)
Myasthenia gravis (BBW)
Adverse Effects: Systemic Administration – Warnings/Precautions
Fluoroquinolones may prolong QTc interval; (similar to macrolides)
Photosensitivity: (similar to tetracyclines)
clostridium difficile associated diarrhea (CDAD) and antimicrobial resistance
Drug interaction: Binding to Mg-Al-Fe-Zn salts in antacids and multi-vitamins may decrease absorption.
Folic Acid Synthesis Inhibitors (Oral): Sulfamethoxazole/Trimethoprim
Sulfa drugs or sulfonamides are considered folate or folic acid synthesis inhibitors.
The addition of trimethoprim to sulfamethoxazole (Bactrim® or Septra®) adds an inhibitor of dihydrofolic acid reduction → bactericidal
Sulfonamide Mechanism of Action: Sulfamethoxazole interferes with bacterial folic acid synthesis
Trimethoprim Mechanism of Action: Trimethoprim inhibits dihydrofolic acid reduction
The addition of trimethoprim to sulfamethoxazole provides for a synergistic effect and is bactericidal; generally sulfa drugs are bacteriostatic.
Indications
urinary tract infections
GI
Adverse Effects: Systemic Administration – Warnings/Precautions
Blood dyscrasias: Severe (agranulocytosis, aplastic anemia, etc.) resulting in fatalities.
Dermatologic reactions: May be severe with fatalities including Stevens-Johnson syndrome and toxic epidermal necrolysis.
Sulfonamide (“sulfa”) allergy: Concerns for cross-reactivity to all sulfa moiety containing compounds (sulfonylureas, thiazide diuretics, loop diuretics except for ethacrynic acid, carbonic anhydrase inhibitors, and celecoxib (SSTLCC).
multiple warnings → not used often