AP Exam 3 (done except volumes)
1/152
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
153 Terms
What’s function of respiratory system for
Oxygen intake
CO2 removal
pH regulation
Voice production
Protection + Filtration
(5)
Lungs take o2 from inhaled air to blood and then to tissues
Lungs remove CO2 waste from cells
Resp system mantain blood pH
Larynx creates sound by passing air over vocal cords
MALT, mucus and cilia trap and destroy debris/pathogens
What are the 2 components of the respiratory system?
Conducting division
Respiratory division
What are the functions of the conducting division of resp system? (2)
Provides passageway for air to move
warms, humidifies, and cleanses air
What’s the function of the respiratory division of the resp system?
Site of gas exchange between lungs and blood
What division is the mouth part of in resp system?
Mouth is primarily an organ of the ____ system.
What is the mouth’s role in respiration?
Mouth is especially important when breathing under ____.
Conducting division
Digestive system
Acts with nose as a conduit for air entry/exit
Important when breathing under extertion.
Nares (Nostrils), Bridge, and Root are portions of which division?
Conducting division
Nares are the _____ to the nose and contain ____, and filter _____ ____.
Bridge connects ____ to rest of ____.
Root: Region located between the _____.
Nares/Nostrils = openings to nose, contain hair and filter large particles.
Bridge connects root to rest of nose.
Root is located between the eyebrows.
Nasal Vestibulate, Nasal setpum, S/M/I conchae, and internal nares/choanae, are all portions of the
Internal structures of nose in conducting division
Nasal vestibe, just inside the _____ and leads to the ____ ____.
Nasal septum, divides ____ ____ into ___ and ___ sides.
Superior, middle and inferior conchae - Three pairs of ___-____ bones extending ______ from the nasal septum.
Internal nares (Chonae) - Opening from the ____ ____ into the _____.
Vestibulue- Inside nostrils, leads to nasal cavity
Nasal septum- Divides nasal cavity to L/R sides
Superior, Middle, and Inferior Conchae: 3 pairs of C-shape bones extends laterally from nasal septum
What are Meatuses?
What’s the function of the Eustachian tube opening?
Meatuses: Passageway around conchae allowing air flow
Eustachian tube opening: Drains fluid from middle ear
Where is Olofactory epithielium located, lining, and containing what?
Tissue at top of nasal cavity lining superior nasal conchae containing olofactory cells
Nasopharynx
It’s a ____ for ____ only
____ lie in ____ wall.
Nasopharynx is a conduit for air only
Nasopharynx has adenoids liying on posterior wall
Oropharynx
Conduit for ____ and ____
Has ____ found on its border.
Oropharynx = conduit for digestion/respiration
Has tonxils found on its border
Laryngopharynx
Conduit for ___ and ____.
Opens into ____ and ____.
Laryngopharynx is a conduit for air + food and opens into larynx and esophagus
Larynx is part of which resp division?
Conducting divison
Larynx directs ____ into ____, and food into _____.
What prevents food and drinks from entering trachea?
Large pieces of cartilage keep the larynx from ______.
Larynx directs air into trachea and food into esophagus, and epiglottis prevents food/drinks from entering trachea.
Large pieces of certilage keep larynx from collapsing.
Glottis is part of which division?
Conducting division
Glottis
Glottis is the vocal apparatus of the _____.
Glottis is located inferior to the _____.
Glottis is vocal apparatus of larynx.
Glottis is located inferior to the epiglottis.
What happens when you get a lump in your throat?
Stressors (physical and emotional) trigger the ____.
When ___ or ___ kicks in, glottis is held open to ____ _____ intake.
As this occurs, ____ drain from ____ duct, ____ cavity, and _____ to trigger ____ reflex.
Glottis usually closes during _____, but _____ while ____ ____ system is holding it open feels like a ____ in the throat.
Stressors trigger sympathetic nervous system
When Fight/Flight kicks in, Glottis held open to improve oxygen intake.
As this occurs, tears drain from lacrimal duct, nasal cavity, and throat to trigger swallow reflex.
Glottis usually closes during swallowing, but swallowing while SNS is holding it open feels like lump in the throat.
Trachea is part of the _____ division
Conducting
Trachea
Trachea extends from ____ to its division into ____ and ____ _______.
Trachea contains _____ cartilage (called tracheal cartilages or _____ _____) between fiberous tissue ligaments
The ______ is a ridge of cartilage at the point where the ______ ______ that sense ___ ____ and causes ____ ___ to ____ ____.
Cilitated cells on interior form the ______ ______.
Trachea extends from larynx to its division into L/R bronchi
Trachea contains hyaline cartilage (tracheal cartilage/tracheal rings) between fiberous tissue ligaments
Carina is a ridge of cartilage at point where bronchi branches that senses liquid substances and triggers violent coughing to expel them
Ciliated cells on interior form the mucocilary escalator.
Bronchial tree is part of which division?
Conducting division
Bronchi (singular = bronchus) supported by cartilage, and interior contains ____ _____ cells.
Bronchi (single bronchus) supported by cartilage and interior contains ciliated mucous cells.
Bronchiles lack _____, but have ____ ____ instead, and lack _____ but still have ciliated cells.
Bronchioles lack cartilage, have SM instead, and lack mucous but still have cilaited cells.
What are the branches of the R/L Primary bronchi? (4)
Primary bronchi (R/L) —> Secondary lobar bronchi —> tertiary bronchi —> primary bronchioles —> terminal bronchioles
How is conducting different from resp division?
Conducting moves air in/out
What’s diff between trachea and bronchi?
Trachea is main pathway to get to lungs and bronchi are branches coming off it to get to lungs
Respiratory broncholes and Alveolar sacs are part of what division?
Respiratory division
What are Respiratory bronchioles the final division of, and where do they end?
Alveolar ducts are short conduits of mainly what?
Alveolar sacs are grape like clusters of individual ____ that opened from ____ ducts.
All of the Respiratory bronchioles, Alveolar ducts, and Alveolar sacs are very ____.
Resp broncholes = final division of bronchioles ending at alveoli
Alveolar ducts are short conduits of mainly CT
Alveolar sacs are grape like clusters of individual alveoli that opened from alveolar ducts
Resp Bronchioles, Alevolar ducts, and Alevolar sacs are all very elastic.
Alveoli are part of which division?
Respiratory division
Gas exchange occurs in the ____.
Alveoli have ____ walls with a large ____.
Alveoli provide contact between ____ air and ____ in ____ capillaries around alveolar walls.
Collectively, the alveoli have a surface area of ____, the size of a…
Gas exchange in alveoli
Alveoli have thin walls, large lumen
Alveoli provide contact between inhaled air + blood in pulmonary capillaries around alveolar walls
Collectively, alveoli surface area = 70m², size of singles tennis court
Alveolar cells are structures of the…
Respiratory division
_____ _____ is the site of gas exchange containing squamous cells, basement membrane and capillaries
Respiratory membrane
Type I Alveolar cells are the most _____ alveolar cell type.
____-cells connected to a thin basement membrane
Type 1 = most common alveolar cell
Squamous cells connected to thin basement membrane
Type II Alveolar cells
____-cells aka ____ cells, that make and secrete _____.
_____ reduces ____ ____ between water lining inner alveoli surface
Type II Alveolar cells
Cubodial cells aka septal cells that make/secrete surfactant
Surfactant reduces surface tension between water lining inner alveoli surface
Type III Alveolar cells
Aka _____ _____ or ____ cells; or resident aleveolar ____ cells
These Type III cells scavenge _____ and other ____.
Type III alveolar cells aka alveolar macrophages or dust cells, the resident aleveolar immune cells
Scavaenge microorganisms and other particles
What’s IRDS stand for, and what does it involve
Infant Resp distress syndrome, aka SDD, surfactant deficency syndrome
Surfactants released by Type II cells break H-bonds between H2O molecules making it easier to expand our lungs
What are causes of IRDS? (1)
What’s it common in?
Inadequate surfactant, common in pre-term babies
Symptoms of IRDS? (3)
Can it be fatal?
Difficulty breathing, fast HR, cyanosis
can be fatal
Glucocorticoids to stimulate fetal surfactant production, or O2 via CPAP are treatments for
IRDS
Lungs are part of which division?
Resp division
Lungs
Occupy most of the ____ cavity, surrounded by ___ membrane.
How many lobes do Right lung, and left lung have?
What do the lobes divide into? What does this further divide into?
Lungs
occupy most of thoracic cavity, surrounded by pleural membrane
Right lung has 3 lobes, left lung has 2 lobes
Lobes divide into bronchopulmonary segments, that further divide into pulmonary lobules
What’s the function of the root of the lung, and what does it contain?
What’s the hilum?
Lung root contains arteries, veins, nerves, and bronchi and connects lung to mediastinum
Hilum of lung is where arteries/veins/nerves/bronchi enter/exit
Lung pleura is part of what division
Resp division
Each lung is surrounded by a ____ membrane, with what 2 layers?
Lung has pleural membrane with visceral pleura (tight around lung) and parietal pleura around inner wall of thoracic cavity.
Where’s pleural cavity located, and what does it contain and secrete?
Space between visceral/parietal pleura of pleural membrane with mesothelial cells secreting pleural fluid (lubrication + barrier)
Pleurisy is inflammation of the
Pleura of lungs
What are causes of Pleurisy? (2)
What’s symptom of Pleurisy?
What’s treatment
Pleurisy causes
Infection + certain meds
Symptoms = sharp CP
Treatment: meds, anti-IF, rest.
For Pulmonary blood flow in the lungs, what’s the pathway for Deoxygenated blood, and Oxygenated blood? (8)
Deoxygenated blood —> Pulm trunk on heart —> pulm arteries —> lobar arteries —> capillary beds around alveoli —> oxygenated blood now goes to venules —> small veins —> pulm veins back to heart
For Nitrogen, O2, and CO2, what composition of air?
Nitrogen = 78%
O2 = 20%
CO2 = 0.03%
What’s equation for Flow?
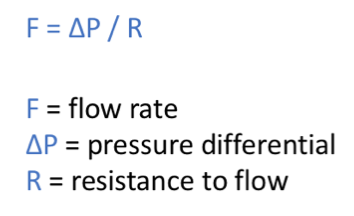
If airways become too narrow, what occurs to flow and oxygen?
Too narrow = increased pressure/resistance, and decreased oxygen
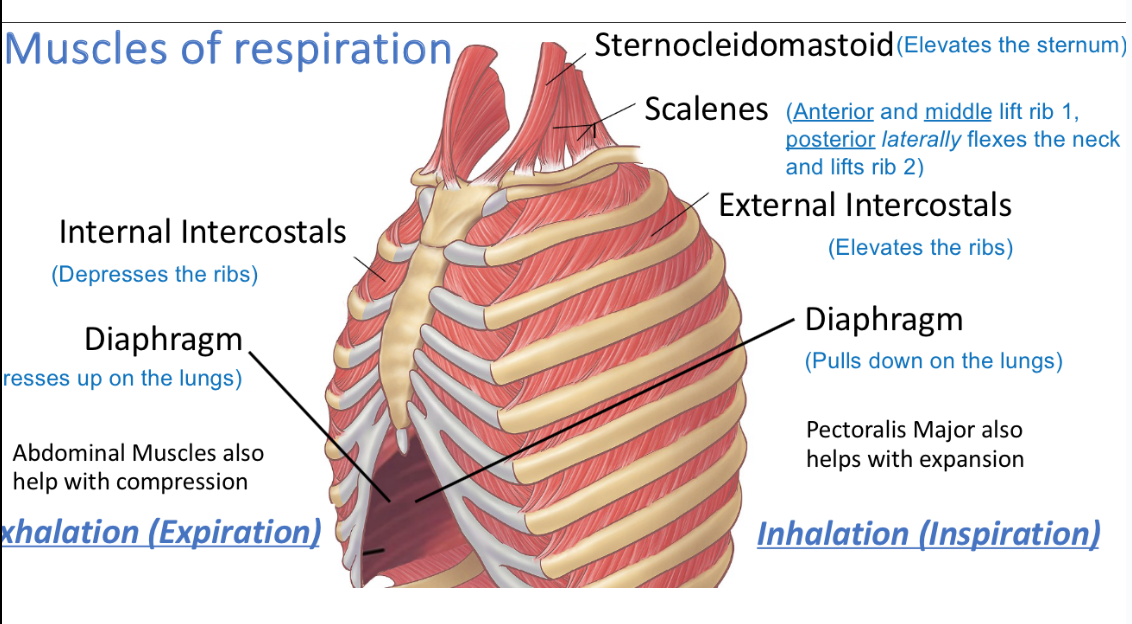
What are the only principle muscles of respiration?
Diaphram and internal/external intercoastals
What’s muscles for Exhalation/Expiration? (3)
What do they do during expiration?
Internal intercostals - Depresses the ribs
Diaphram: Presses up on lungs
Abdominal muscles help with compression
= Expiration!
INT.ic : depress ribs
diaphram: pushes lungs up
Abs: compress
What are the muscles of inspiration (5), and what do they do during inspiration/Inhalation?
(S,S,EI,D,PM)
Sternocliedomastoid - Elevates sternum
Scalenes: Anterior/Middle lift Rib 1, and Posterior laterally flexes neck and lifts Rib 2
External intercostal: Elevates ribs
Diaphram: Pulls down on lungs
Pec major: Helps with inhalation
Respiration: The harder we work to inhale, the more ____ ____ we recruit.
Exhalation is mostly a _____ ____ of muscles used for ____, but ____ ____ will use ____ ____.
Respiration: Harder we work to inhale, more accessory muscles we recruit.
Exhalation is mostly passive relaxation of muscles used for inhalation, but forceful exhalation will use additional muscles.
Describe volume, pressure, and air movement during breathing in, and breathing out.
Breathing in (Inhalation) : Lungs expand (Volume up), Pressure down, air goes in.
Breathing out (Exhalation): Lungs contract( Pressure increases), air is forced out.
Describe each in a sentence
ATM pressure
Transpulm pressure
Intrapleural pressure
Intrapulm/Intra-alveolar pressure
Pressure in ATM around body
TP pressure = Difference between pressures in lungs and intrapleural pressure
IP pressure = Pressure in space between visceral and parietal pleura
Intrapulm/IA pressure = Pressure in alveoli
What’s equation for Boyles Law
P1V1=P2V2
What are determinants of Gas pressure? (determinants of pressure)
# of Gas particles: If # of gas particles (+) = (+) pressure
Temperature: If temp (+) = (+) pressure
Volume of space: If volume decreases = (+) pressure
Pnuemothorax: Collapsed lung
Due to injury/illness, ___, ____, or ____ buildup in pleural space where if intrapleural pressure exceeds ______ pressure, lung collapses.
A pneumothorax due to blood is called a ________.
What’s treatment? (2)
Pnuemothorax
Due to injury/illness, air, blood, or fluid biuldup in pleural space where if intrapleural > intrapulmonary pressure, lung collapses.
Pnuemothorax due to blood is called Hemopnuemothorax.
Treatment = Needle apiration or chest tube to allow air and blood to drain
Pnuemothorax/Collapsed lung = Air/Blood/Fluid buildup in pleural space when Intrapleural pressure > Intrapulm(alveolar) pressure —> causes lung to collapse
Pnuemothorax due to blood is called Hemopnuemothorax
Treatment = Needle apiration or draining blood/air w. chest tube
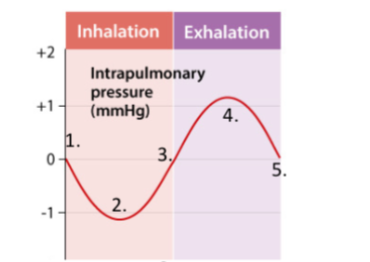
What’s process of ventilation for resting breathing? (5)
Prior to inspiration, ATM pressure = Intrapulm pressure
During inhalation, lungs expand (V+) and intrapulm pressure drops (P-) below ATM pressure and air goes in
Lungs are full and pressure returns to equilibrium
On exhalation, volume decreases, intrapulmonary pressure increases above ATM pressure and air leaves lung
Lungs are empty and pressure equalizes
Nonbreathing Air movements
What’s purpose of coughing and sneezing?
What does a yawn result from?
What’s a hiccup and what does it cause?
What’s Laughing/Crying?
What’s valsava manuever?
Cough/Sneeze: resp system tries to clear irritants from airways
Yawn: Results from deepest possible breath
Hiccup: Diaphram spasm causing burst of air through vocal cords
Laugh/cry: Emotional state drives ventilation pattern
Valsava: Exhaling against closed airway
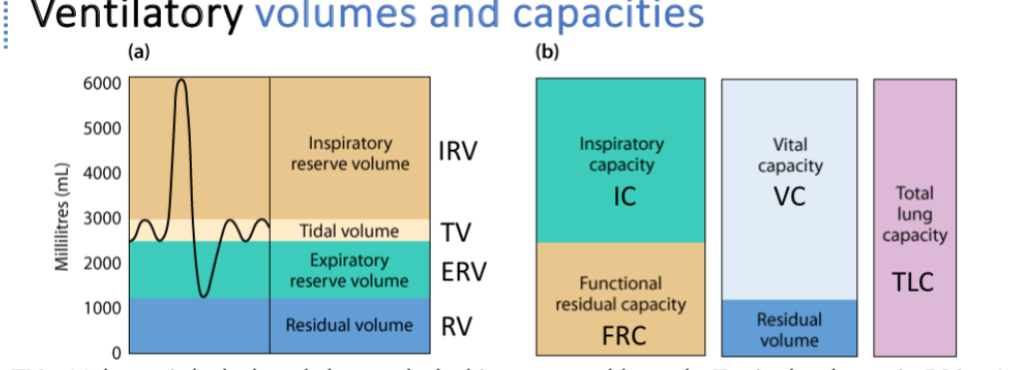
Ventilatory volumes and capacities
What are the following defintiinos, and for TV, IRV, and ERV, and RV, what’s the usual volumes
TV
IRV
ERV
RV
IC
FRC
VC
TV(tidal volume) = Volume inhale/exhale in normal breath, normally 500ml
IRV(insp reserve volume) = # of additional air that can be inhaled in addition to the TV, 2100-3200ml
ERV(exp reserve volume) = # of air that can be force exhaled, after exhaling TV (1000-1200ml)
RV(residual vol) = Air left after a completed ERV (1200ml is lowest lung possible with open alveoli)
IC (inspiratory capacity) = TV + IRV
FRC (funct. residual capacity) = RV + ERV (amount left after a normal exhalation)
VC: Vital capcity: TV + IRV + ERV : amount a person can physically move in and out of their lungs
TV – Tidal Volume
Simple: Air moved in or out during a normal breath.
Example: Quiet breathing while sitting in class.
IRV – Inspiratory Reserve Volume
Simple: Extra air you can inhale after a normal breath in.
Example: Taking a deep breath after a regular inhale.
ERV – Expiratory Reserve Volume
Simple: Extra air you can force out after a normal breath out.
Example: Blowing out hard after breathing out normally.
RV – Residual Volume
Simple: Air that always stays in your lungs, even after forceful exhale.
Example: Air left in lungs after blowing out as hard as possible.
IC – Inspiratory Capacity
Simple: Total air you can inhale after a normal exhale.
Example: Breathing in normally, then taking the deepest breath possible.
FRC – Functional Residual Capacity
Simple: Air left in lungs after a normal exhale.
Example: Air in lungs when you pause after a relaxed breath out.
VC – Vital Capacity
Simple: Maximum air you can move in and out of your lungs.
Example: Taking the deepest breath in possible, then exhaling all the way ou
What do flow rates provide info about?
Resistance of airways
What’s PEF?
FEV?
FVC?
PEF = Peak expiratory flow rate
FEV = Forced expiratory volume (volume that can be forcefully exhaled within a certain time frame)
FVC = forced vital capacity (similar to vital capcity, but measured by exaling as quickly as possible)
What’s Atelectasis?
What determines if Atelectasis is obstructive or nonobstructive?
What’s a general cause of Atelectasis?
What’s treatment? (3)
Collapsed lung from collapsed alveoli
Obstructive Atelectasis if blocked airway, and Nonobstructive if occuring from pressure outside lung
General cause is General anaesthia as a common cause
Treatment: Chest PT, Surgery if obstructive, CPAP
What’s Dalton’s law of partial pressures state?
What’s Partial pressure?
What’s equation of partial pressure?
Total pressure of a mixture of gases is equal to sum of partial pressures of component gasses present
Partial pressure represents the contribution of any gas in a mixture to the mixtures total pressure
Partial pressure = Total pressure x fraction of gas
What does rate of gas diffusion depend on?
What determines the amount of gas dissolved in a liquid?
Rate of gas diffusion depends on solubility coefficent of the gas
Amount of gas dissolved in a liquid = partial pressure x solubility coefficent
V/Q ratios in lungs
For adequate gas exchange to occur, what must occur?
What’s healthy V/Q ratio in lungs? What if it’s above, and below this ratio? (much)
Flow of air (ventilation/V) must match perfusion (flow of blood/Q)
Healthy V/Q ratio = 0.8
If V/Q > 0.8, Ventilation is higher than perfusion, and causes clots, HF, emphysema, capillary damage
If V/Q < 0.8, perfusion is higher than ventilation, and causes aspiration, blockage of bronchi, pnuemonia and asthma or COPD.
Skipped Zones of Blood Flow in lungs
What is diffusion in the lungs and tissues based on?
For the lungs (External respiration): How does O2 move?
For the lungs (External respiration)For CO2, how does it move?
Diffusion in lungs is based on gas partial pressures because fluids travel from high to low pressure areas
In lungs (External respiration): Oxygen (O₂) moves from the air into the blood because its partial pressure is higher in the air than in the blood. As O₂ enters the capillaries, the partial pressure in the blood increases.
Carbon dioxide (CO₂) moves from the blood into the air because its partial pressure is higher in the blood than in the air. As CO₂ leaves the capillaries, its level in the blood decreases.
For the tissues (internal respiration)
How does O2 move?
How does CO2 move?
In tissues (Internal respiration)
Oxygen (O₂) moves from the blood —> tissues because its partial pressure is higher in the blood than in the tissues. As the blood circulates, the partial pressure of O₂ decreases.
Carbon dioxide (CO₂) moves from the tissues —> blood because its partial pressure is higher in the tissues than in the blood. As the blood circulates, the partial pressure of CO₂ increases.
skipped slide for internal and external respiration side by side
Skipped review aerobic cellular respiration
Hemoglobin transports more than __% of blood O2
How many hemoglobin does each RBC carry?
How many o2 molecules can each RBC carry?
98% of blood O2 carried by HG
Each RBC has 250-300m HG molecules
Each RBC can carry up to 1.2B oxygen molecules
skipped CO2 transport in blood mostly except Haldane effect(got that one)
What’s the Haldane effect?
Co2 more readily binds for unoxygenated hemoglobin
skipped slide on gas exchange between blood and body tissues, ALONG WITH CHLORIDE SHIFT PORTION FOR INTERNAL RESPIRATION THATS FUCKING IMPORTANT MAKE SURE YOU GET THAT PART IN THE EXAM REVIEW WHAT THE FUCK ITS BOTH EXTERNAL AND INTERNAL RESPIRATION FUCK
What range must blood pH remain in?
What occurs if it goes above 7.8, or below 6.8?
In the blood buffering system, what is Hydronium H3O and Bicarbonate (HCO3) in equilibrium with? What does this help mantain?
What do additional increases in hydronium H3O stimulate the release of?
Blood pH is mantained between 7.35 and 7.45
Over 7.8 = death
Under 6.8 = death
Blood buffering system (Hydronium H3O) and Bicarbonate (HCO3) are in EQ with Carbonic acid (H2CO3). This balance of acid and base helps mantain pH
(H2CO3 weak acid + H2O) ←- —> H3O + HCO3 (conjguate base)
Additional increases in hyodrinum stimulate more release of O2 from HG
pH regulation
What is the physiological cause of hyperventilation?
What is the general cause of hyperventilation?
Physialogical Hyperventilation: Too much CO2 expelled —> rise in blood pH —> blood vessels narrow to slow BF to brain causing LOC
General Hyperventilation: Breaths that are too fast or deep from anxiety/panic
pH regulation
What is the physialogical cause of hypoventilation?
What is the general cause of hypoventilation?
Physialogical = Rise in CO2 causes drop in blood pH —> O2 levels drop, deprives brain and tissues
General cause = Breaths are slow/shallow from illness or injury
What’s Hypoxia?
Lack of O2
What’s treatment for Hypoxia?
Supp. O2
What are 3 causes of Hypoxia?
Lung diseases, Cyanide poisoning, Heart/Brain problems
Where is partial pressure higher? Blood or body tissues?
Blood
Where is partial pressure of CO2 higher? Blood or alveoli?
Blood
What’s purpose of Chloride shift?
During Internal respiration, Tissues release CO₂, which is converted into bicarbonate in the blood. The bicarbonate leaves the red blood cell and swaps places with chloride to maintain electrical balance.
Overall control of ventilators
What are sensors, and what are 3 things they sense? (3)
What are integrators, and where are they located? (3)
What are effectors (2) and what do they control?
Sensors: Chemoreceptors, detect chem lvls in blood i.e PaCO2 (partial arterial pressure of CO2) PaO2, pH
Integrators: Resp center in brain stem, and neurons in medulla and pons
Effectors: Diapragm and intercostal muscles that control breathing.
What’s the function of the Dorsal Respiratory Group (DRG) of the brainstem for ventilation? (3) (controls, responds to, impacts)
Why don’t we need a control center for exhalation?
Controls inhalation, responds to blood CO2 and O2 levels, and impacts VRG (ventral respiratory group).
Exhalation is generally passive unless forced and doesn’t need a center unless its forced due to exercise or illness.
What’s function of Ventral Respiratory Group (VRG)? (2)
Controls forced exhalation (i.e exercise or sickness) and increases inhalation pressure because if you exhale hard you’ll likely inhale hard.
What’s function of Apnueistic center of brainstem?
Stimulates DRG (Dorsal respiratory group)
What’s function of Pnuemotaxic center? What will it make sure you don’t do underwater?
Inhibits DRG, i.e will make sure you don’t breath while underwater.
What’s function of RTN (Retrotrapezoid nucleus) of Brain stem? (2) (Recieves X from X in X and X ____ to impact X)
Recieves input from chemoreceptors in brain and lung stretch to impact VRG
Sensitivity of ventilation to blood O2, CO2, and pH
What causes us to breath faster, for example when underwater?
The stimuli to breath faster is due to buildup of CO2 and acid rather than O2. So when breathing underwater, it’s not the lack of O2, but rather the buildup of CO2 in blood. O2 has the lowest impact on needing to breathe, while CO2 and pH cause much greater effect on needing to breath faster.
What’s an Obstructive disorder?
Air has trouble flowing due to blockage making air resistance
What’s a restrictive disorder?
Tightness/weakness/stiffness makes it difficult to expand ribs/lungs
What are 6 ways to diagnose Obstructive and Restrictive disorders?
Spirometry: Spirometer with mouthpiece hooked to machine
Plethysomography: Patient sits in air tight box and does stuff
Imaging scan
Pulse oximeter: O2 levels in blood
Biopsy
Bronchscope: Insert scope into mouth down to bronchus
Asthma: Homeostatic imbalances
When airways narrow = higher _____, harder to ____.
What’s the characteristic symptom?
Asthma = narrow airways, high air resistance, hard to breathe.
Characteristic symptom = wheezing and difficulty breathing