BIO 116- A&P Exam 4
1/178
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
179 Terms
Urine Formation
180 L fluid processed daily; only 1.5 L → urine
Glomerular filtration
Tubular reabsorption
Tubular secreation
Glomerular filtration
produces cell and protein-free filtrate
Porous membrane filters the blood
Only water and solutes smaller than proteins can pass
Normally NO CELLS should pass
Refers to the filtration of the blood!!
Tubular reabsorption
returns 99% of substances from filtrate to blood in renal tubules and collecting ducts
Tubular secretion
Selectively moves substances from blood to filtrate in renal tubules and collecting ducts
Function 1 of the Nephron
Glomerular Filtration
Layers of the Filtration Membrane
Fenestrated endothelium of glomerular capillaries
Basement membrane (fused basal laminae of two layers)
Foot processes of podocytes with filtration slits; slit diaphragms repel macromolecules
Pressures that Affect FIltration
Hydrostatic pressure in glomerular capillaries
Hydrostatic pressure in capsular space
Colloid osmotic pressure in capillaries
Hydrostatic pressure in glomerular capillaries
= 55mm Hg
Chief force pushing water out, pushes solutes out of blood
Hydrostatic prssure in capsular space
HPcs Pressure of filtrate in capsule
15 mm Hg
Pushes solutes into the blood
Colloid osmotic pressure in capillaries
OPgc
The “pulling” by proteins in blood
30 mm Hg
Pushes solutes into the blood
Glomerular Filtration Rate (GFR) and regulation of the Blood Pressure
Volume of filtrate formed per minute by both kidneys ( normal = 120-125 ml/min)
Net filtration pressure (NFP) is a major regularor of GFR
GFR affects systemic blood pressure
Kidneys regulate arterial blood pressure
Norepinephrine and Epinephrine → indue systemic vasoconstriction → increased blood pressure
Constriction of afferent arterioles → down GFR → less urine → increased blood volume and pressure
GFR Affects Systemic Blood Pressure
Up GFR → Up urine output → Down blood pressure
Down GFR → Down urine output → Up Blood pressure
How Kidents regulate arterial blood pressure
Direct renal mechanism
The renin-angiotensin-aldosterone mechanism
Norepinephrine
Released by sympathetic nervous system
Epinephrine
Released by adrenal medullea
Renin-Anfiotensin-Aldosterone Mechanism
Main mechanism for increasing blood pressure
Three pathways to RENIN release by granular cells
Three pathways to RENIN release by granular cells
Direct stimulation of granular cells by sympathetic nervous system
Stimulation by activated macula densa cells when filreate NaCl is low
Reduced stretch of Granular cells
Function 2 of the Nephron
Reabsorption
Nephron Reabsorption
Major sites are the tubules and collected ducts
All nutrients, e.g., glucose and amino acids, 65% of Na+ and water, ion, uric acid; ½ urea (which is later secreted back into filtrate)
They move from the tubule back to the blood (they are reabsorbed).
They come back into the blood!!
Reabsorption of Sodium
Activation of the Na+ -K+ ATPase pump
Secondary active transport
Facilitated diffusion (apical)
Secondary active transport
a ion couple with another that is transported actively
Apical Facilited diffusion
Happening through proteins binding in the membrane
It doesn’t require energy
Reabsorption of Water
osmosis, aided by water-filled pores calls aquaporins that could open or close
Reabsorption of water in Descending limb
H2O can leave and solutes cannot
Reabsorption of water in Ascending limb
H2O cannot leave and solutes can
Reabsorption of organic nutrients
water, glucose, amino acids, some ions, and vitamins
Secondary active transport; cotransport with Na+
Water-soluble substances, some ion and urea, follow the water
Lipid-soluble drugs, environmental pollutants are difficult to be reabsorbed because they don’t follow water
Reabsorption is hormonally regulated by:
Antidiuretic hormone (ADH)
Aldosterone
Atrial natriuretic peptide (ANP)
Parathyroid hormone
Antidiuretic hormone (ADH)
increases the reabsorption of water
Aldosterone
Increases the reabsorption of Na+ (therefore water)
Atrial natriuretic peptide (ANP)
Decreases reabsorption of Na+
Parathyroid hormone
Incresase the absorption of Ca2+
Function 3 of the Nephron
Tubular Secretion
Tubular Secretion
K+, H4+, HCO3- creatinine, organic acids and bases move from peritubular capillaries to the tubule cells into the urinary filtrate:
Solutes move INTO the tubules
They go into the urine. They are secreted.
Functions of Tubular Secretion
Disposes of substances (e.g., drugs) bound to plasma proteins
Eliminates undesirable substances passively reabsorbed (e.g., urea and uric acid)
Rids body of excess K+
Controls blood pH by altering amounts of H+ or HCO3- in urine
Regulation of Urine Concentration and Volume
Kidneys maintain osmolality of plasma at ~300 milliosmoles (mOsm) by regulating urine concentration and volume
How to Kidneys Regulate Urine Concentration and Volume
Use a countercurrent mechanism that maintains two compartments with different osmolarities
A low osmolarity area in the outer medulla
A high osmolarity area located in the inner medulla
How do kidneys maintain two areas with different concentrations of solutes in the medulla area?
The permeability for water and solutes changes at different segments fot he nephron loop
Descending Limb
Freely permeable to H2O
H2O leaves attracted by the concentrated medulla → filtrate becomes MORE CONCENTRATED (~1200 mOsm)
Ascending Limb
Impermeable to H2O
Water stays in the tubule Na+ and Cl- are reabsorbed in thick segment; some passively reabsorbed in thin segment → filtrate becomes LESS CONCENTRATED (100 mOsm)
Vasa Recta
Straight capillaries in the medulla running parallel to the loop
Preserve medullary gradient (different concentrations)
Prevent rapid removal of salt from interstitial space
Remove, reabsorbed water, maintaining the high concentrated medulla
How does the Recycling of Urea helps to maintain the Medullary Osmotic Gradient?
Urea is secreted into the ascending limb
Urea is reabsorbed in the collecting ducts
The urea now is in the medulla maintaining the high concentration gradient
Dilution and Concentration of Urine (Overhydration)
Produces large volume of diluted urine
ADH production decreases → urine ~100 mOsm (less concentrated)
If aldosterone present, additional ions (Na+) removed → ~ 50 mOsm (even less concentrated)
Dilution and Concentration of Urine (Dehydration)
Small volume and concentrated urine
When ADH is released (urine ~ 1200 mOsm). The kidney produces less volume and more concentrated urine
In severe dehydration — 99% water is reabsorbed
What is Renal Clearance?
Volume of plasma cleaned by the kidneys of a particular substance in a given time. Ex. Cretinti clearance
Detects glomerular damage and follow up of renal disease
Chronic renal disease
Renal Failure
Chronic renal disease
Defined when GFR < 60 mL/min for 3 months (normal is 120 mL/min)
Renal Failure
GR < 15 mL/min
Causes uremic syndrome
Diuretics
Chemical that enhance urinary output
ADH inhibitors, alcohol
Na+ reabsorption inhibitors, caffeine, drugs for hypertension or edema
Loop diuretics they inhibit medullary gradient formation: furosemide (Lasix)
Osmotic diuretics
Osmotic diuretics
THese substances are not reabsorbed in the tubules and keep and attract water inside tubules (high glucose in diabetic patient, mannitol)
Uremia syndrome
Accumulation of urea and other waste products in the bloodstream, which are normally eliminated by the kidneys
Intracellular fluid (ICF) compartment
Fluid inside cells (2/3 of total body fluid)
Contains more soluble proteins than plasma
Low Na+ and Cl-
Major cation: K+
Major anion HPO42-
Extracellular fluid (ECF) compartment
Fluid in two main ECF compartments outside cells
Plasma: 3L
Interstitial fluid (IF): 12L in spaces between cells
Less proteins than ICF
Major catio: Na+
Major anion: Cl-
Fluid Movement among Compartments
Osmotic and hydrostatic pressures regulate change in solute concentration of any compartment
Increased ECF osmolality → water leaves cell
Decreased ECF osmolality → water enters cell
Osmolality is maintained around 280-300 mOsm
Body Water Content
Infants are 73% or more water (low body fat, low bone mass)
Adult males: ~60% water
Adult females: ~50% water (because higher fat content, less skeletal muscle mass)
adipose tissue is least hydrated of all
Total body water in adults ~40L
Water content declines to ~45% in old age
Regulation of Water Output
Obligatory water losses → explain why we cannot live without water very long
Insensible water loss from lungs (respiration) or skin (evaporation)
Sensible water loss from urine to excrete wastes (60%), obvious sweat (8%), ans feces (4%)
Volume of urine excreted and concentration also depend on fluid intake, diet, and water loss via other avenues
Excessive loss of H2O from ECF
ECF osmotic pressure rises
Cells lose H2O to ECF by osmosis → cells shrink
Hypotonic hydration
Cellular overhydration, or water intoxication
Occurs with renal insufficiency or rapid excess water ingestion
ECF osmolality decreases, causing hyponatremia
Treated with hypertonic saline solution
Hyponatremia
Results in net osmosis of water into tissue cells and swelling of cells
Symptoms: severe metabolic disturbances, nausea, vomiting, muscular cramping, cerebral edema, and possible death
Excessive H2O enters the ECF
ECF osmotic pressure falls
H2O moves into cells by osmosis → cells swells
Central Role of Sodium in Fluid and Electrolyte Balance
Sodium, is most abundant cation in ECF. It is the only cation exerting significant osmotic pressure
Influence of other hormones
Concentration of Na+
Determines osmolality of ECF and excitability of neurons and muscles
Content of Na+
Total body content determines ECF volume and therefore blood pressure
Hormones that Regulate Sodium Balance
Estrogens
Progesterone
Glucocorticoids
Estrogens
Increase NaCl reabsorption (like aldosterone)
Leads to H2O retention during menstrual cycles and pregnancy
Progesterone
Decreases Na+ reabsorption (blocks aldosterone)
Promotes Na+and H2O loss
Glucocorticoids
In
Importance of Potassium ans Regulation of Potassium Balance
Affects resting membrane potential (RMP) in neurons and muscle cells (especially cardiac muscles)
Disruption in [K+] (hyper-or hypokalemia) in heart can interfere with electrical conduction leading to sudden death
K+ is also part of the body’s buffer system
H+ shifts in and out of cells in opposite direction of K+ to maintain cation balance
Hyperkalemia
Increases in ECF [K+]
Cause decreased resting membrane potential, causing depolarization, followed by reduced excitability
Hypokalemia
Decreases in ECF [K+]
Cause hyperpolarization and no responsiveness
H+ shifts in and out of cells in opposite direction of K+ to maintain cation balance, so:
ECF K+ levels rise with acidosis
ECF K+ levels fall with alkalosis
K+ is secreted in the collecting tubes according to the needs of the body
Low K+ diet or accelerated K+ loss reduces its secretion and promotes its limited reabsorption
Increased K+ in adrenal cortex causes release of aldosterone, which increases K+ secretion
Regulation of Calcium
99% of body’s calcium is found in bones as calcium phosphate salts
Calcium balance controlled by parathyroid hormone (PTH)
PTH promotes increase in calcium levels by targeting
Bones
Kidneys
Small intestine
Bones and Calcium
Osteoclasts break down matrix, releasing calcium and phosphate to blood
Kidneys and Calcium
Increases calcium reabsorption
Decreases phosphate ion reabsorption
Small Intertine and Calcium
Increases calcium absorption (indirectly by simulation by vitamin D precursor)
Ca2+ in ECF is important for:
Blood clotting
Cell membrane permeability
Secretory activities
Neuromuscular excitability: most important
Hypocalcemia
Increases neuromuscular excitability and can lead to muscle tetany
Hypercalcemia
Inhibits neurons and muscle cells and may cause heart arrhythmias
Normal pH of body fluids
Arterial blood: pH 7.4
Venous blood and interstitial fluid: pH 7.35
ICF: pH 7.0
Alkalosis or alkalemia
arterial pH > 7.45
Acidosis or acidemia
arterial pH <7.35
Mechanisms of Concentration of Hydrogen Ions
Chemical buffer systems
Brainstem respiratory centers
Renal mechanisms
Chemical buffer systems
Rapid
First line of defense
Brainstem respiratory centers
Acts within 1-3 minutes
Renal mechanisms
Most potent, but require hours to days to effect pH changes
Chemical Buffer Systmes
A system of one or more compounds that act to resist pH changes when stronf acid or base is added
Will bine H+ if pH drops of release H+ if pH rises
There major buffering systems
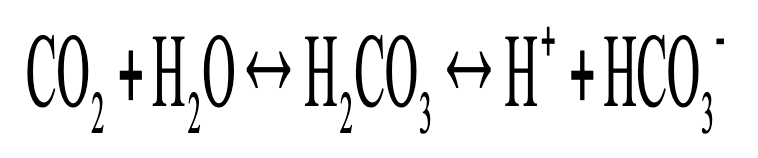
Bicarbonate buffer system
Phosphate buffer system
Protein buffer system
Respiratory and renal systems
physiological buffering systems
Respiratory system
Eliminates CO2 (an acid)
During CO2 unloading (tissues), reaction shifts to left (and H+ is incorporated into H2O)
During CO2 loading (lungs), reaction shifts to right (and H+ is buffered by proteins)
Does hypercapnia or acidosis cause more CO2 to be removed from the blood?
Both (hypercapnia and acidosis) cause more CO2 to be removed from the blood, pushing reaction to left, which reduces H+ concentration
Hypercapnia
PCO2 in blood rises
Activates medullary chemoreceptors
Causes Increased respiratory rate and depth
Acidosis
Rising plasma H+ activates peripheral chemoreceptors
Causes increased respiratory rate and depth
Alkalosis
Depresses respiratory center
Respiratory rate and depth will decrease, causing H+ concentration to increase
Respiratory system impairment that causes acid-base imbalances
Hypoventilation causes respiratory acidosis
Hyperventilation causes respiratory alkalosis
Renal Regulation
Acid-base balance by adjusting amount of bicarbonate in blood by:
Conserving (reabsorbing) or generating new HCO3-
Excreting HCO3-
Excreting H+
Excreting NH4+
Metabolic acidosis
Metabolic alkalosis
Metabolic acidosis
Low blood pH and HCO3-
Rising blood pH and HCO3-
Blood pH below 6.8
Causes depression of CNS, which can lead to coma and death
Blood pH above 7.8
Causes overexcitation of nervous system, leading to muscle tetany, extreme nervousness, convulsions, and death, often from respiratory arrest
Respiratory and Renal Compensations
If acid-base imbalance is due to malfunction of one physiological buffer system, other system tries to compensate
What does Respiratory system attempt to correct?
Metabolic acid-base imbalances
What does Kidneys attempt to correct?
Respiratory acid-base imbalances